Abstract
Bedtime worry, including worrying about incomplete future tasks, is a significant contributor to difficulty falling asleep. Previous research showed that writing about one’s worries can help individuals fall asleep. We investigated whether the temporal focus of bedtime writing—writing a to-do list versus journaling about completed activities—affected sleep onset latency. Fifty-seven healthy young adults (18–30) completed a writing assignment for five minutes prior to overnight polysomnography recording in a controlled sleep laboratory. They were randomly assigned to write about tasks that they needed to remember to complete the next few days (to-do list) or about tasks they had completed the previous few days (completed list). Participants in the to-do list condition fell asleep significantly faster than those in the completed-list condition. The more specifically participants wrote their to-do list, the faster they subsequently fell asleep, whereas the opposite trend was observed when participants wrote about completed activities. Therefore, to facilitate falling asleep, individuals may derive benefit from writing a very specific to-do list for five minutes at bedtime rather than journaling about completed activities.
Keywords: prospection, cognitive arousal, worry, sleep difficulties, prospective memory
Introduction
Forty percent of American adults report difficulty falling asleep at least a few times each month (National Sleep Foundation, 2008). Difficulty falling asleep may relate to socioeconomic factors, personality traits, genetics, pain and medical comorbidities, or environmental factors such as light exposure (Chang, Aeschbach, Duffy, & Czeisler, 2015; Lichstein, Taylor, McCrae, & Petrov, 2017). Perhaps the most common contributor to difficulty falling asleep, however, are cognitive processes operating at bedtime such as worry and rumination (Gross & Borkovec, 1982; Harvey, 2000; Haynes, Adams, & Franzen, 1981).
Traditionally, sleep research and clinical practice have focused on bedtime rumination about past events, but bedtime worry about future events may be at least as important (Borkovec, Robinson, Pruzinsky, & DePree, 1983; Brosschot, 2010). One potential stressor is knowing that one has incomplete tasks, that is, items left on the to-do list. In the cognitive science literature, incomplete tasks are known to remain at a high level of cognitive activation, spurring automatic thoughts about the incomplete tasks (e.g., Bugg & Scullin, 2013; Goschke & Kuhl, 1993; Martin & Tesser, 1996; Syrek & Antoni, 2014; Zeigarnik, 1938). In the sleep literature, a potential analogue is bedtime worry about work-related tasks (Kecklund & Akerstedt, 2004; Söderström, Ekstedt, Akerstedt, Nilsson, & Axelsson, 2004; Syrek, Weigelt, Peifer, & Antoni, 2016), which trigger cognitive arousal, and prolong sleep onset latency (Syrek & Antoni, 2014; Wicklow & Espie, 2000). Therefore, it is unsurprising that difficulty falling asleep is most common at the beginning of the work week (Morin, 1993).
One seemingly counterintuitive solution to bedtime worry and rumination is to write about what is on one’s mind (Pennebaker, 1997). Though one might intuit that writing could reinforce worrying and increase rumination, many studies now show that writing benefits mental health, classroom success, and even physiological markers of autonomic, muscular, and immune function (for review, see Pennebaker & Smyth, 2016). In the sleep field, some argue that writing decreases sleep onset latency (e.g., Harvey & Farrell, 2003, using self-report measures), though other groups have not observed this benefit of writing (e.g., Mooney, Espie, & Broomfield’s, 2009, work using self-report and actigraphy).
The current experiment advances the existing literature in several ways. We used a sample size that was double that used by previous sleep and writing studies (Harvey & Farrell, 2003; Mooney et al., 2009). Moreover, most studies on sleep and writing have measured sleep onset latency using self-report. Here we employ overnight polysomnography. We conducted the writing experiment specifically on the first night in the laboratory because the first night constitutes a psychosocial stressor (e.g., new context, procedures; Agnew, Webb, & Williams, 1966). This psychosocial stressor helps to capture the experience of occasional bedtime stress (National Sleep Foundation, 2008), and is useful to avoiding floor effects in sleep onset latency. For these reasons, the first sleep laboratory night is used as a model of transient insomnia when evaluating sleep aids (Roehrs, Vogel, Sterling, & Roth, 1990; Roth, Roehrs, & Vogel, 1995; Zammit et al., 2009).
Whereas most previous studies focused on writing about past or present worries (or combining past with future worries; e.g., Wicklow & Espie, 2000), the current study focuses on writing about the future; that is, tomorrow’s to-do list. Specifically, we manipulated whether at bedtime participants wrote down everything they needed to remember to do in the next few days versus all the tasks they remembered to complete in the previous few days. We selected the Completed List group over other possible control groups (e.g., no writing at all, writing unrelated lists) for three reasons. First, having participants “journal” about completed activities matches what many people do in naturalistic settings. Second, there are individual differences in busyness (Festini, McDonough, & Park, 2016), and it is possible that individuals who have more activities to complete are those who have more difficulty falling asleep. The Completed List comparison group allowed us to examine the association between the number of tasks/activities reported and difficulty falling asleep, helping to control for busyness as a personality factor. Third, and most importantly, Boot, Simons, Stothart, and Stutts (2013) asserted that the psychological benefits of writing could be explained as placebo effects because the comparison condition in most writing experiments is no activity or a trivial, unrelated writing activity. By having participants in both the To-Do List and Completed List conditions write about the same topic content—activities—the current design is more likely to avoid placebo effects.
The writing manipulation generated the following competing hypotheses (consistent with the principle of equipoise; e.g., Friedman, Furberg, DeMets, Reboussin, & Granger, 2015). One hypothesis is that writing about the future will lead to increased worry over unfinished tasks, thereby increasing sleep onset latency, relative to journaling about completed activities (which, having been completed, should not trigger worry). The alternative hypothesis is that writing a to-do list will “off-load” those thoughts from consciousness (i.e., Pennebaker-like effects), and thereby decrease sleep onset latency, relative to journaling about completed activities (which need not be “off-loaded” because they have already been completed). Though there is anecdotal evidence that writing a bedtime to-do list can help one to fall asleep (Andreessen, 2007; Cooper, 2014), this idea has not been empirically tested. A related possibility, which builds on the idea that the specificity of future simulation (“prospection”) reduces worry about the future (Brown, Macleod, Tata, & Goddard, 2002; Jing, Madore, & Schacter, 2016), is that the number of tasks/activities one reports (hereafter, list specificity) will correlate with decreased sleep onset latency: The more to-do list items that one writes, the faster they will fall asleep.
METHODS
Participants
Healthy adults (N=60, ages 18–30) were recruited using campus flyers at Baylor University.1 Participants were recruited for a multi-night sleep study, and the current manuscript reports data from the first night in which we randomly assigned participants to To-Do List or Completed-List conditions. Participants were pre-screened for self-reported history of sleep disorders (e.g., insomnia, narcolepsy), psychiatric conditions, neurological disorders, and use of any medications that might alter their sleep architecture. We excluded three participants, one for studying textbooks in bed after the writing manipulation, one for accidentally being enrolled after already completing the study the previous year, and one outlier based on reported sleep the night before the experiment (outliers are defined as values that are 1.5 interquartile ranges from the lower or upper quartile). Thus, the final sample size was 57 participants. Based upon the large effect size reported by Harvey and Farrell (2003; d = 1.01), a two-tailed t-test, and alpha set to 0.05, our sample size would allow for .95 power to detect a significant group difference (Faul, Erdfelder, Lang, & Buckner, 2007). Assuming a relatively smaller effect size (.80), we would still have 0.80 power to detect a significant group difference. The Baylor University Institutional Review Board approved this study and individuals received monetary compensation for their participation.
Overnight Polysomnography (PSG)
Overnight PSG took place in a sound-attenuated sleep research laboratory. PSG was measured using the Grass Comet XL Plus system. Following 10–20 measurement, we recorded electroencephalography from 13 channels (Fp1, Fp2, F3, Fz, F4, C3, C4, P3, Pz, P4, O1, Oz, O2) that were referenced to the contralateral mastoids and grounded using Fpz and Cz electrodes. We additionally measured left and right electrooculography and mentalis electromyography. To screen for sleep apnea, we used a nasal pressure transducer, respiratory effort belts, and pulse oximetry. There were no cases of clinical sleep apnea in this young adult sample (i.e., all apnea-hypopnea indexes were fewer than five events per hour). Participants were monitored throughout the night via a low-illumination, infrared video system. Sleep stage scoring was conducted masked to experimental condition by a registered polysomnography technician. Scoring was conducted in 30 second epochs and followed American Academy of Sleep Medicine scoring criteria (Iber, Ancoli-Israel, Chesson, & Quan, 2007).
Writing Condition Manipulation
Participants were randomly assigned to To-Do List and Completed List conditions. In the To-Do List condition, participants were given the following instructions:
“We’d like for you to spend the next five minutes writing down everything you have to remember to do tomorrow and over the next few days. You can write these in paragraph form or in bullet points. Use all five minutes to think and write about tasks you have to complete tomorrow and in the near future, even if few are coming to you.”
In the Completed List condition, the instructions were identical but modified to refer to activities that were completed that day and over the previous few days. Participants wrote their list using pen and paper. Research assistants scored the lists for number of items written (list specificity), and any disagreements were resolved following discussion.
Questionnaires
In addition to basic demographic information (age and gender), we measured stress, enjoyment of cognitive arousal, difficulty remembering future tasks and completed tasks, and self-reported sleep the night before the study.2 The Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1994) is a 10-item scale (response scale of 0 to 4) that assesses stress over the last month (e.g., “how often have you felt that you were on top of things?). The Need for Cognition scale (Cacioppo & Petty, 1982) is an 18-item scale (response scale of 1 to 5) that assesses how much individuals enjoy cognitive activities (e.g., “I like to have the responsibility of handling a situation that requires a lot of thinking,” “I usually end up deliberating about issues even when they do not affect me personally”). The Prospective and Retrospective Memory Questionnaire (PRMQ; Crawford, Smith, Maylor, Della Sala, & Logie, 2003) is a 16-item scale (response scale of 1 to 5) that assesses whether people are more likely to fail to remember a completed event (retrospective scale; “Do you fail to recall things that have happened to you in the last few days?”) or fail to remember to perform a future task (prospective subscale; “Do you forget to buy something you planned to buy, like a birthday card?”). Participants also documented their bedtime, waketime, sleep onset latency, and wake after sleep onset time for the night before the experiment.
Procedure
Participants arrived to the laboratory at 2100 hours on a Monday, Tuesday, Wednesday, or Thursday night (to avoid weekend effects on bedtime, sleep onset latency, and total sleep time; e.g., Crowley, Acebo, & Carskadon, 2007; Roennenberg, 2013). After the participant signed an informed consent document, the research assistants began electrode application. Participants filled out the demographic and other questionnaires during the PSG setup phase. Following PSG setup, participants completed the five-minute writing assignment (To-Do List or Completed List) using paper and pencil. The experimenter returned after five minutes to take the writing sheet. Before and after the writing assignment the experimenter took the participant’s blood pressure (for an association between sleep onset latency and blood pressure see, e.g., Li et al., 2015). Arm-cuff blood pressure was taken with both feet on the ground after the participant had been seated for a minimum of five minutes. We condensed systolic and diastolic blood pressure assessments by using the mean arterial pressure calculation: [(Diastolic × 2) + Systolic)]/2.
Following PSG biocalibrations, participants were instructed that they could fall asleep (lights out) at approximately 2230 hours. Though 2230 hours is earlier than many students’ typical bedtime (though see weekday and weekend differences; Crowley et al., 2007) and earlier than our participants’ reported bedtime the night before coming to the sleep lab, many of the reasons that college students go to bed late are controlled when they are in a laboratory setting (homework, extra-curricular activities, part-time work, watching television, playing video games, using the computer, using smartphones, etc.). These psychosocial factors influence circadian rhythms (e.g., melatonin onset), which have sometimes been mistaken as being immutable (cf. Chang et al., 2015). An alternative design would be to set a later time of lights out (e.g., midnight), but the practical value of showing that writing affects sleep onset latency after midnight would be questionable; that late at night, the drive to sleep is already very high (“Process S” in Borbély et al.’s, 2016, model). There are advantages and disadvantages to using a 2230 bedtime, but this bedtime is congruent with most laboratory polysomnography studies on college students (2200–2300 hours), and controlling for the specific time of lights out and participants’ reported bedtime the previous night did not significantly alter any of the results.3
Statistical Analysis
Study materials and de-identified data are available at Open Science Framework (osf.io/psyjf). Our primary analysis was to use t-tests to determine whether writing condition (to-do list, completed list) differentially affected sleep onset latency (primary dependent variable; Harvey & Farrell, 2003) or other PSG variables (exploratory dependent variables). When necessary, we corrected for unequal variances. Our secondary analysis was to use Pearson product correlations to determine the association between significant PSG measures (from the primary analysis) and list specificity (number of items written). Finally, to determine the impact of the covariates, we conducted a hierarchical linear regression controlling for any demographic or questionnaire variables that were independently associated with the significant PSG measure(s) (from the primary analysis), and then tested for effects of the writing condition and list specificity. We report Cohen’s d, phi, and ΔR2 as measures of effect size.
RESULTS
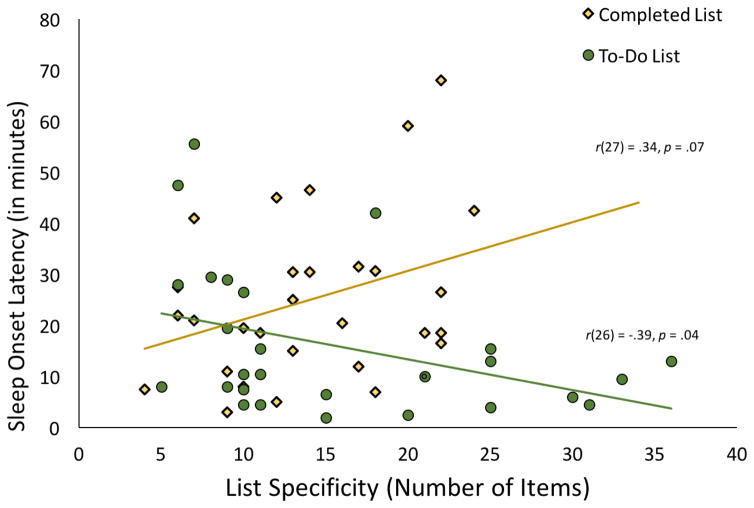
Table 1 demonstrates that the conditions were similar in questionnaire variables, but differed in PSG measures. Participants who wrote a To-Do List fell asleep significantly more quickly than those who wrote a Completed List, t(55) = 2.32, p = 0.02, d = .63. Figure 1 demonstrates that sleep onset latency was further reduced in participants who wrote more specific lists. There was a significant, negative correlation between sleep onset latency and the number of items written on the To-Do List, r(26) = −.39, p = .04. This association does not seem to reflect trait factors (e.g., busyness), because in the Completed List condition, we observed the reverse trend of greater list specificity being positively associated with PSG-defined sleep onset latency, r(27) = .34, p = .07.
Table 1.
Demographic and polysomnography variables across To-Do List and Completed List conditions. Standard deviations are in parentheses. Mean arterial pressure data are missing for one participant and the self-reported sleep data of night before the experiment were missing from three participants.
| Completed List (N=29) | To-Do List (N=28) | Condition Main Effect | |
|---|---|---|---|
| Chronological Age | 20.45 (2.35) | 20.00 (1.28) | t(43.47L) = −0.90, p = 0.37, d = 0.24 |
| Gender (% Female) | 75.86% | 57.14% | χ2(1) = 2.25, p = .13, ϕ = 0.20 |
| List Specificity (#of items written) | 14.10 (5.74) | 15.96 (9.14) | t(45.16L) = −0.92, p = 0.36, d = 0.24 |
| Pre-Writing Mean Arterial Pressure | 81.76 (7.78) | 83.95 (9.72) | t(54) = −0.93, p = .36, d = .25 |
| Post-Writing Mean Arterial Pressure | 81.62 (8.17) | 82.06 (7.96) | t(54) = −0.21, p = .84, d = .06 |
| Perceived Stress Scale Score | 16.93 (5.54) | 14.82 (6.10) | t(55) = 1.37, p = .18, d = .37 |
| Need for Cognition Scale Score | 64.55 (10.83) | 68.71 (7.81) | t(50.96L) = −1.67, p = .10, d = .44 |
| PRMQ – Prospective | 2.59 (0.44) | 2.56 (0.41) | t(55) = 0.25, p = .80, d = .07 |
| PRMQ – Retrospective | 2.38 (0.40) | 2.26 (0.44) | t(55) = 1.06, p = .30, d = .29 |
| Total Sleep Time (self-report)a | 414.14 (78.65) | 412.25 (89.51) | t(52) = 0.08, p = 0.93, d = .02 |
| Sleep Onset Time (self-report)a | 16.68 (14.32) | 14.58 (15.15) | t(52) = 0.52, p = 0.60, d = .14 |
| Wake After Sleep Onset (self-report)a | 3.50 (6.57) | 5.87 (13.48) | t(52) = 0.73, p = 0.47, d = .20 |
| Bedtime (self-report)a | 12:41am (1:25) | 12:28am (1:24) | t(52) = 0.55, p = 0.58, d = .16 |
| Wake Time (self-report)a | 7:55am (1:10) | 7:41am (1:19) | t(52) = −0.83, p = 0.41, d = .23 |
| Polysomnography | |||
| Lights Out | 10:24pm (0:21) | 10:28pm (0:21) | t(55) = 0.631, p = .53, d = .17 |
| Sleep Onset Latency (minutes) | 25.09 (15.94) | 15.82 (14.07) | t(55) = 2.32, p = 0.02, d = 0.63 |
| Total Sleep Time (minutes) | 492.40 (45.26) | 498.53 (62.44) | t(55) = −0.43, p = 0.67, d = 0.12 |
| Number of Awakenings | 26.38 (11.54) | 20.93 (10.31) | t(55) = 1.88, p = 0.07, d = 0.51 |
| Wake After Sleep Onset (minutes) | 38.43 (26.82) | 34.08 (41.38) | t(55) = 0.47, p = 0.64, d = 0.13 |
| Sleep Efficiency (percentage) | 88.53 (6.10) | 90.74 (8.87) | t(55) = −1.10, p = 0.28, d = 0.30 |
| N1 (proportion) | .06 (.04) | .05 (.04) | t(55) = 1.21, p = 0.23, d = 0.33 |
| N2 (proportion) | .58 (.07) | .59 (.06) | t(55) = −0.41, p = 0.69, d = 0.11 |
| N3 (proportion) | .16 (.05) | .15 (.04) | t(55) = 0.19, p = 0.85, d = 0.05 |
| REM (proportion) | .20 (.05) | .21 (.05) | t(55) = −0.73, p = 0.47, d = 0.20 |
Abbreviations: PRMQ = Prospective and Retrospective Memory Questionnaire
Indicates that Levene’s test was significant and the degrees of freedom and p values have been corrected accordingly.
The self-reported sleep measures were taken for the night before the experiment.
Figure 1.
Scatterplot illustration of the writing condition by list specificity interaction. When removing the outlier sleep onset latency data point, the correlation in the Completed List condition is r(26) = .25, p = .20. Note that in the To-Do List condition, there were two overlapping data points and we decreased the size of one data point for clarity purposes.
To test for a writing condition by list specificity interaction, we conducted a hierarchical linear regression on PSG-defined sleep onset latency minutes (dependent variable). In Steps 1 and 2 we entered the writing condition, ΔR2 = .09, F(1, 55) = 5.40, p = .02, and then list specificity, ΔR2 < .01, F(1, 54) = 0.31, p = .58. In Step 3, we entered the condition by list specificity interaction term, which explained significant additional variance, ΔR2 = .12, F(1, 53) = 7.75, p = .007. When removing one PSG-defined sleep-onset latency outlier data point, the main effect of writing condition was still significant, ΔR2 = .07, F(1, 54) = 4.29, p = .04, as was the condition by list specificity interaction, ΔR2 = .08, F(1, 52) = 5.08, p = .03. To determine the strength of the writing condition effect when controlling for demographic and questionnaire data, we first tested which of the Table 1 variables were correlated with PSG-defined sleep onset latency.3 Only self-reported sleep onset latency for the night before experiment, r(52) = .37, p = .007, and mean arterial pressure, r(55) = .35, p = .008 (Li et al., 2015), were significantly correlated with PSG-defined sleep onset latency.4 Table 2 illustrates that after including self-reported sleep latency and mean arterial pressure as covariates in Step 1, the writing condition main effect remained statistically significant in Step 2, F(1, 49) = 6.15, p = .02. The condition by list specificity interaction was slightly attenuated, F(1, 47) = 3.64, p = .06.
Table 2.
Results of hierarchical linear regression analysis on sleep onset latency. Mean arterial pressure is collapsed across pre- and post-writing observations.
| Without Covariates | With Covariates | ||||||
|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | Step 1 | Step 2 | Step 3 | Step 4 | |
| Mean Arterial pressure | β = .29* | β = .33* | β = .33* | β = .30* | |||
| Sleep Diary SOL | β = .30* | β = .28* | β = .27* | β = .23† | |||
| Writing List Condition | β = −.30* | β = −.29* | β = .44 | β = −.30* | β = −.29* | β = .20 | |
| List Specificity (number of items written) | β = −.07 | β = .46* | β = −.06 | β = .29 | |||
| Condition x List Specificity Interaction | β = −1.02** | β = −.67† | |||||
| F statistic | F(1,55) = 5.40 | F(1,54) = 0.31 | F(1,53) = 7.75 | F(2,50) = 6.83 | F(1,49) = 6.15 | F(1,48) = 0.23 | F(1,47) = 3.64 |
| ΔR2 | .089* | .005 | .12** | .215** | .088* | .003 | .050† |
Abbreviations: PRMQ = Prospective and Retrospective Memory Questionnaire; SOL: sleep onset latency
indicates p < .10,
indicates p < .05,
indicates p < .01.
Discussion
Participants who wrote a to-do list at bedtime fell asleep faster than those who journaled about completed tasks. This finding is surprising in light of the evidence that unfinished tasks are a significant source of cognitive activation and worry (Bugg & Scullin, 2013; Goshke & Kuhl, 1993; Kecklund & Akerstedt, 2004; Martin & Tesser, 1996; Söderström et al., 2004; Syrek & Antoni, 2014; Syrek et al., 2016; Zeigarnik, 1938). However, the key here seems to be that participants wrote down their to-do list rather than mentally ruminated about their unfinished tasks. Expressive writing has previously been demonstrated to reduce anxiety and depression (Pennebaker & Smyth, 2016), though its impact on sleep onset latency has been a matter of debate (Arigo, & Smyth, 2012; Harvey & Farrell, 2003; Mooney et al., 2009). To the best of our knowledge, the present work constitutes the only sleep and writing study to employ polysomnography, which is considered the gold standard for measuring sleep onset latency. Thus, we can conclude with reasonable confidence that bedtime writing can help some individuals fall asleep, but also that the temporal focus of their writing may be important (i.e., future tasks rather than journaling about completed tasks).
Not only content, but also quantity, of writing was important. There were diverging associations between sleep onset latency and how specifically (detailed) the individual wrote their to-do list versus completed list. The more to-do list items that one wrote, the faster they fell asleep. There is some precedent to the idea that to-do list specificity might be beneficial. For example, one study had first-time pregnant women simulate how future labor would go, and women who showed very specific future simulations showed less worry (Brown et al., 2002). Furthermore, a study in healthy adults found that having participants imagine worrisome future events in a specific/detailed manner decreased anxiety about those events (Jing et al., 2016; see also Jansson-Fröjmark, Lind, & Sunnhed, 2012). In the current study, a pattern (p = .07), was that the more specifically participants journaled about completed tasks/activities, the longer it took for them to fall asleep. If this trend is shown to be reliable in future studies, one possible explanation is that individuals who are busier (either due to personality or due to a busy period of life) experience more sleep disturbances including difficulty falling asleep (e.g., Bootzin, Epstein, & Wood, 1991). A second possible explanation for the diverging correlations across To-Do list and Completed list conditions is that the conditions had slightly different list specificity distributions (i.e., fewer participants wrote ≥20 tasks in the Completed-List condition). A provocative third explanation, however, is that remembering the past may prime some thinking/rumination about future incomplete tasks, which might then prolong sleep onset latency (e.g., see Buckner & Carroll, 2007). Therefore, for sleep onset latency, writing a To-Do List has some benefits, and writing a Completed-Activity List may have some costs.
The writing procedure resembles what has been labeled in behavioral sleep medicine as a “worry list.” Often included in cognitive-behavioral therapy for insomnia (Edinger, Leggett, Carney, & Manber, 2017), worry lists involve having insomnia patients record their worries (while not in bed), with the goal of unburdening their anxieties and concerns and allowing them to later fall asleep more easily (Bootzin & Epstein, 2000; Espie & Lindsay, 1987; Hauri, 1991). The fact that we could identify a similar phenomenon in a group of generally healthy adults argues for generalizability of the writing technique to broader populations who suffer from occasional difficulties falling asleep, a complaint shared by 40% of American adults (National Sleep Foundation, 2008). Indeed, our participants reported no sleep disorders and showed mean sleep onset latencies less than 30 minutes even in the Completed List condition (Table 1). We believe the next logical step is to conduct a randomized controlled trial in individuals with and without sleep-onset insomnia who are asked to write a bedtime to-do list every night. Such a clinical trial would illuminate whether the effectiveness of bedtime writing translates to naturalistic settings (i.e., beyond the first night in a sleep laboratory), as well as whether bedtime writing benefits sleep for multiple nights in healthy and clinical groups.
Control/Comparison Groups for Writing Studies
Future research may consider additional control groups, but should be mindful of the considerable ongoing debate regarding designing appropriate control groups for behavioral studies (e.g., Boot et al., 2013). When researchers use a no-treatment control group (e.g., a no-writing condition) or an “active control” groups (e.g., writing unrelated lists), the study is vulnerable to placebo effects because the “control” participants are engaged in a trivial activity that the experimenters themselves do not expect to affect behavioral outcomes. The alternative is to follow the principle of equipoise in which the comparison group constitutes what participants would normally do and the study is designed such that the experimenters do not know which of two conditions will produce the favorable outcome (e.g., Friedman et al., 2015). This was the guiding framework for contrasting the To-Do List condition with the Completed-List condition. Journaling about completed activities is common near bedtime, the experimenters did not know whether writing the To-Do List would increase or decrease sleep onset latency, and both conditions were engaged in writing about the same topic content (activities/tasks/chores) with only time orientation of the writing differing (future versus past focused). An alternative design that would still be consistent with equipoise is a condition that writes their To-Do List versus one that only thinks about their To-Do List. The challenge here for future studies is to ensure that participants in the think-only condition adhered to those instructions. Returning to the current study’s design, one question that arises is whether the To-Do List improves sleep onset latency or the Completed List impairs sleep onset latency. We expect that both factors play a role, but what the data definitively show is that if an individual is writing about tasks/chores at bedtime it is better to write about future tasks than completed tasks.
Limitations
There were limitations to the current experiment. Though our sample size was appropriate for an experimental, laboratory-based, polysomnography study, it would be too small for a correlational individual differences study. In the current work, the correlational analyses were secondary and used to compliment the experimental finding that writing a to-do list produced different sleep onset latencies than writing a completed list. Additional consideration should also be given to effect moderators. Adherence to the writing intervention is a likely determinant of effect size (e.g., Figure 1 shows that when participants wrote fewer than 10 items there was a smaller condition difference). Furthermore, measures of personality, anxiety, and depression might moderate the effects of writing on sleep onset latency, and could be explored in a larger-sample investigation. We did not include a state-based measure of cognitive arousal or worry because such scales often diverge from objective measurements (e.g., Carney & Waters, 2006). Therefore, the proximal mechanism by which bedtime writing affects sleep onset latency requires additional investigation.
Context of the Research
This research stems from the idea that focusing on the future may affect sleep, or mental processes occurring during sleep. For example, in the memory consolidation literature, there is evidence that only information that is encoded during the day as being relevant in the future will be reactivated and consolidated during sleep (Barner, Seibold, Born, & Diekelmann, 2017; Wilhelm, Diekelmann, Molzow, Ayoub, Mölle, & Born, 2011; see also Bennion, Payne, & Kensinger, 2015). On this topic, our laboratory is currently investigating which aspect of sleep physiology is important to consolidating memories for future goals/intentions (prospective memory; Scullin & McDaniel, 2010), and whether age-related changes in sleep explain age-related changes in prospective memory consolidation (Scullin & Bliwise, 2015). But, we continue to be interested in whether prospection per se (without writing) affects sleep onset latency or other aspects of sleep physiology, with the long-range goal of capitalizing on these basic findings to inform clinical practice.
Conclusions
The present experiment highlights bedtime writing as a potentially beneficial (or potentially costly, depending on past or future focus), easily administered, behavioral sleep aid for young adults who may not present in a clinical setting. Of course, consideration must be given to whether bedtime writing will be ineffective in some individuals due to health, contextual/environmental, or personality characteristics. Nevertheless, in today’s “24/7 society” that emphasizes work productivity, many individuals’ to-do lists are extensive and incur substantial negative affect, anxiety, and rumination (Rajaratnam & Arendt, 2001). Rather than journal about the day’s completed tasks or process tomorrow’s to-do list in one’s mind, the current experiment suggests that individuals spend five minutes near bedtime thoroughly writing a to-do list.
Acknowledgments
M.K.S. was partially supported by NIH AG053161 and the Sleep Research Society Foundation. Portions of this project, including the to-do list specificity findings, were presented at the 2016 Sleep Meeting. We are appreciative of Mericyn Daunis, Cole Rowley, Claudina Tami, Matthew Willis, Sanna Lokhandwala, Ali Villagran, Stacy Nguyen, Mary High, Taylor Terlizzese, and Chenlu Gao for their assistance with data collection and data entry.
Footnotes
Because this was the first polysomnography study conducted at this specific university, we expect that no participant had previously participated in a sleep study.
Some of the present study’s participants (n = 46) returned for additional sessions on prospective memory. When time allowed, the participants filled out questionnaires that may be of interest to the current data. The two groups did not significantly differ on Morningness-Eveningness Questionnaire scores (MCompleted = 51.00, MTo-Do = 50.14, t(41) = 0.31, p = .76; Horne & Ostberg, 1975), Brief COPE scores (MCompleted = 69.60, MTo-Do = 64.75, t(38) = 1.58, p = .12; Carver, 1997), and Rumination Response Scale scores (MCompleted = 40.68, MTo-Do = 36.33, t(35) = 1.29, p = .21; Treynor, Gonzalez, & Nolen-Hoeksema, 2003).
Participants’ self-reported previous-night bedtime and study night lights out were not related to sleep onset latency, ΔR2 < .01, F(2, 51) = 0.005, p > .99. After controlling for these variables, there was still a significant condition main effect, ΔR2 = .08, F(1, 50) = 4.28, p = .04, and condition by list specificity interaction, ΔR2 = .12, F(1, 48) = 7.11, p = .01. Additional analyses in which we subtracted study night lights out from self-reported bedtime showed similar negligible effects, ΔR2 < .01, F(1, 52) = 0.005, p > .94.
During review, the concern was raised that gender may have biased the results. Gender composition was not significantly different across conditions (Table 1) and the assignment to conditions was performed randomly. Even still, we examined our sleep onset latency results by gender and found no evidence for gender effects. Sleep onset latency did not significantly differ across male participants (M = 21.95, SD = 17.28) and female participants (M = 19.83, SD = 14.94), ΔR2 < .01, F(1, 55) = 0.23, p = .64. In a hierarchical linear regression analysis, after statistically controlling for gender, there was still a significant condition main effect, ΔR2 = .10, F(1, 54) = 6.11, p = .02, and condition by list specificity interaction, ΔR2 = .13, F(1, 52) = 8.55, p = .005.
References
- Agnew HW, Webb WB, Williams RL. The first night effect: An EEG study of sleep. Psychophysiology. 1966;2(3):263–266. doi: 10.1111/j.1469-8986.1966.tb02650.x. [DOI] [PubMed] [Google Scholar]
- Andreessen M. Pmarca guide to personal productivity. 2007 Retrieved on February 13, 2017 at http://pmarchive.com/guide_to_personal_productivity.html.
- Arigo D, Smyth JM. The benefits of expressive writing on sleep difficulty and appearance concerns for college women. Psychology & Health. 2012;27(2):210–226. doi: 10.1080/08870446.2011.558196. [DOI] [PubMed] [Google Scholar]
- Barner C, Seibold M, Born J, Diekelmann S. Consolidation of prospective memory: Effects of sleep on completed and reinstated intentions. Frontiers in Psychology. 2016;7 doi: 10.3389/fpsyg.2016.02025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennion KA, Payne JD, Kensinger EA. Selective effects of sleep on emotional memory: What mechanisms are responsible? Translational Issues in Psychological Science. 2015;1(1):79–88. [Google Scholar]
- Boot WR, Simons DJ, Stothart C, Stutts C. The pervasive problem with placebos in psychology: Why active control groups are not sufficient to rule out placebo effects. Perspectives on Psychological Science. 2013;8(4):445–454. doi: 10.1177/1745691613491271. [DOI] [PubMed] [Google Scholar]
- Bootzin RR, Epstein DR. Stimulus control. In: Lichstein KL, Morin CM, editors. Treatment of late-life insomnia. Sage Publications; Thousand Oaks, CA: 2000. pp. 167–184. [Google Scholar]
- Bootzin RR, Epstein D, Wood JM. Case studies in insomnia. Springer; US: 1991. Stimulus control instructions; pp. 19–28. [Google Scholar]
- Borbély AA, Daan S, Wirz-Justice A, Deboer T. The two-process model of sleep regulation: a reappraisal. Journal of Sleep Research. 2016;25(2):131–143. doi: 10.1111/jsr.12371. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Robinson E, Pruzinsky T, DePree JA. Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy. 1983;21(1):9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- Brosschot JF. Markers of chronic stress: Prolonged physiological activation and (un) conscious perseverative cognition. Neuroscience & Biobehavioral Reviews. 2010;35(1):46–50. doi: 10.1016/j.neubiorev.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Brown GP, Macleod AK, Tata P, Goddard L. Worry and the simulation of future outcomes. Anxiety, Stress & Coping. 2002;15(1):1–17. [Google Scholar]
- Bugg JM, Scullin MK. Controlling intentions: The surprising ease of stopping after going relative to stopping after never having gone. Psychological Science. 2013;24:2463–2471. doi: 10.1177/0956797613494850. [DOI] [PubMed] [Google Scholar]
- Buckner RL, Carroll DC. Self-projection and the brain. Trends in Cognitive Sciences. 2007;11(2):49–57. doi: 10.1016/j.tics.2006.11.004. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Petty RE. The need for cognition. Journal of Personality and Social Psychology. 1982;42(1):116–131. [Google Scholar]
- Carney CE, Waters WF. Effects of a structured problem-solving procedure on pre-sleep cognitive arousal in college students with insomnia. Behavioral Sleep Medicine. 2006;4(1):13–28. doi: 10.1207/s15402010bsm0401_2. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chang AM, Aeschbach D, Duffy JF, Czeisler CA. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Sciences. 2015;112(4):1232–1237. doi: 10.1073/pnas.1418490112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. Measuring stress: A guide for health and social scientists. 1994. Perceived stress scale. [Google Scholar]
- Cooper BB. Five unexpected ways to work smarter, not harder. 2014 Retrieved February 13, 2017 at https://blog.bufferapp.com/5-more-ways-to-work-smarter-not-harder.
- Crawford J, Smith G, Maylor E, Della Sala S, Logie R. The Prospective and Retrospective Memory Questionnaire (PRMQ): Normative data and latent structure in a large non-clinical sample. Memory. 2003;11(3):261–275. doi: 10.1080/09658210244000027. [DOI] [PubMed] [Google Scholar]
- Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Medicine. 2007;8(6):602–612. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Leggett MK, Carney CE, Manber R. Psychological and behavioral treatments for insomnia II: Implementation and specific populations. In: Kryger M, Roth T, editors. Principles and Practice of Sleep Medicine. 6. Elsevier; 2017. [Google Scholar]
- Espie CA, Lindsay WR. Cognitive strategies for the management of severe sleep-maintenance insomnia: A preliminary investigation. Behavioural Psychotherapy. 1987;15(04):388–395. [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Festini SB, McDonough IM, Park DC. The busier the better: Greater busyness is associated with better cognition. Frontiers in Aging Neuroscience. 2016;8 doi: 10.3389/fnagi.2016.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman LM, Furberg CD, DeMets DL, Reboussin DM, Granger CB. Fundamentals of clinical trials. 5. New York: Springer; 2015. [Google Scholar]
- Goschke T, Kuhl J. Representation of intentions: Persisting activation in memory. Journal of Experimental Psychology: Learning, Memory, and Cognition. 1993;19(5):1211–1226. [Google Scholar]
- Gross RT, Borkovec TD. Effects of a cognitive intrusion manipulation on the sleep-onset latency of good sleepers. Behavior Therapy. 1982;13(1):112–116. [Google Scholar]
- Harvey AG. Pre-sleep cognitive activity: A comparison of sleep-onset insomniacs and good sleepers. British Journal of Clinical Psychology. 2000;39(3):275–286. doi: 10.1348/014466500163284. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Farrell C. The efficacy of a Pennebaker-like writing intervention for poor sleepers. Behavioral Sleep Medicine. 2003;1(2):115–124. doi: 10.1207/S15402010BSM0102_4. [DOI] [PubMed] [Google Scholar]
- Hauri PJ. Case studies in insomnia. Springer; US: 1991. Sleep hygiene, relaxation therapy, and cognitive interventions; pp. 65–84. [Google Scholar]
- Haynes SN, Adams A, Franzen M. The effects of presleep stress on sleep-onset insomnia. Journal of Abnormal Psychology. 1981;90(6):601–606. doi: 10.1037//0021-843x.90.6.601. [DOI] [PubMed] [Google Scholar]
- Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. International Journal of Chronobiology. 1975;4(2):97–110. [PubMed] [Google Scholar]
- Iber C, Ancoli-Israel S, Chesson A, Quan SF. The AASM manual for the scoring of sleep and associated events: Rules, terminology and technical specifications. Vol. 1. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- Jansson-Fröjmark M, Lind M, Sunnhed R. Don’t worry, be constructive: A randomized controlled feasibility study comparing behaviour therapy singly and combined with constructive worry for insomnia. British Journal of Clinical Psychology. 2012;51(2):142–157. doi: 10.1111/j.2044-8260.2011.02018.x. [DOI] [PubMed] [Google Scholar]
- Jing HG, Madore KP, Schacter DL. Worrying about the future: An episodic specificity induction impacts problem solving, reappraisal, and well-being. Journal of Experimental Psychology: General. 2016;145(4):402. doi: 10.1037/xge0000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Vgontzas AN, Fernandez-Mendoza J, Bixler EO, Sun Y, Zhou J, … Tang X. Insomnia with physiological hyperarousal is associated with hypertension. Hypertension. 2015;65(3):644–650. doi: 10.1161/HYPERTENSIONAHA.114.04604. [DOI] [PubMed] [Google Scholar]
- Lichstein KL, Taylor DJ, McCrae CS, Petrov ME. Insomnia: Epidemiology and risk factors. In: Kryger M, Roth T, editors. Principles and Practice of Sleep Medicine. 6. Elsevier; 2017. [Google Scholar]
- Kecklund G, Åkerstedt T. Apprehension of the subsequent working day is associated with a low amount of slow wave sleep. Biological Psychology. 2004;66:169–176. doi: 10.1016/j.biopsycho.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Martin LL, Tesser A. Some ruminative thoughts. Advances in Social Cognition. 1996;9:1–47. [Google Scholar]
- Mooney P, Espie CA, Broomfield NM. An experimental assessment of a Pennebaker writing intervention in primary insomnia. Behavioral Sleep Medicine. 2009;7(2):99–105. doi: 10.1080/15402000902762386. [DOI] [PubMed] [Google Scholar]
- Morin CM. Insomnia: Psychological assessment and management. Guilford Press; New York: 1993. [Google Scholar]
- National Sleep Foundation. 2008 Sleep in America poll. Washington, DC: 2008. [Google Scholar]
- Pennebaker JW. Writing about emotional experiences as a therapeutic process. Psychological Science. 1997;8(3):162–166. [Google Scholar]
- Pennebaker JW, Smyth JM. Opening up by writing it down: How expressive writing improves health and eases emotional pain. Guilford Publications; 2016. [Google Scholar]
- Rajaratnam SM, Arendt J. Health in a 24-h society. The Lancet. 2001;358(9286):999–1005. doi: 10.1016/S0140-6736(01)06108-6. [DOI] [PubMed] [Google Scholar]
- Roehrs T, Vogel G, Sterling W, Roth T. Dose effects of temazepam in transient insomnia. Arzneimittel-Forschung. 1990;40(8):859–862. [PubMed] [Google Scholar]
- Roenneberg T. Chronobiology: the human sleep project. Nature. 2013;498(7455):427–428. doi: 10.1038/498427a. [DOI] [PubMed] [Google Scholar]
- Roth T, Roehrs T, Vogel G. Zolpidem in the treatment of transient insomnia: a double-blind, randomized comparison with placebo. Sleep. 1995;18(4):246–251. doi: 10.1093/sleep/18.4.246. [DOI] [PubMed] [Google Scholar]
- Scullin MK, McDaniel MA. Remembering to execute a goal: Sleep on it! Psychological Science. 2010;21(7):1028–1035. doi: 10.1177/0956797610373373. [DOI] [PubMed] [Google Scholar]
- Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: Integrating a half-century of multidisciplinary research. Perspectives on Psychological Science. 2015;10:97–137. doi: 10.1177/1745691614556680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Söderström M, Ekstedt M, Akerstedt T, Nilsson J, Axelsson J. Sleep and sleepiness in young individuals with high burnout scores. Sleep. 2004;27:1369–1378. doi: 10.1093/sleep/27.7.1369. [DOI] [PubMed] [Google Scholar]
- Syrek CJ, Antoni CH. Unfinished tasks foster rumination and impair sleeping—Particularly if leaders have high performance expectations. Journal of Occupational Health Psychology. 2014;19(4):490–499. doi: 10.1037/a0037127. [DOI] [PubMed] [Google Scholar]
- Syrek CJ, Weigelt O, Peifer C, Antoni CH. Zeigarnik’s sleepless nights: how unfinished tasks at the end of the week impair employee sleep on the weekend through rumination. Journal of Occupational Health Psychology. 2016 doi: 10.1037/ocp0000031. http://dx.doi.org/10.1037/ocp0000031. [DOI] [PubMed]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27(3):247–259. [Google Scholar]
- Wicklow A, Espie CA. Intrusive thoughts and their relationship to actigraphic measurement of sleep: Towards a cognitive model of insomnia. Behaviour Research and Therapy. 2000;38(7):679–693. doi: 10.1016/s0005-7967(99)00136-9. [DOI] [PubMed] [Google Scholar]
- Wilhelm I, Diekelmann S, Molzow I, Ayoub A, Mölle M, Born J. Sleep selectively enhances memory expected to be of future relevance. Journal of Neuroscience. 2011;31(5):1563–1569. doi: 10.1523/JNEUROSCI.3575-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zammit G, Schwartz H, Roth T, Wang-Weigand S, Sainati S, Zhang J. The effects of ramelteon in a first-night model of transient insomnia. Sleep Medicine. 2009;10(1):55–59. doi: 10.1016/j.sleep.2008.04.010. [DOI] [PubMed] [Google Scholar]
- Zeigarnik B. On finished and unfinished tasks. In: Ellis WD, editor. A source book of Gestalt psychology. London, England: Harcourt, Brace and Co; 1938. pp. 300–314. [Google Scholar]