Abstract
Objectives
To assess the technical success, complications, and patients' quality of life (QoL) after treatment of chronic venous disease (CVD) using the 1470 nm radial fiber laser.
Methods
A total of 170 patients with chronic venous disease, classified as C2 to C4 according to CEAP classification, were treated for incompetent greater (GSV) and small (SSV) saphenous veins, using the 1470 nm radial fiber laser and application of tumescent anesthesia. Additional phlebectomies were performed through stab microincisions, while 11 patients further underwent sclerotherapy intraoperatively. Patients' QoL was recorded using a CIVIQ-20 questionnaire pre and post-operatively.
Results
Technical success regarding GSV vein occlusion was recorded at 100% and 98% during 12 and 24 month follow up respectively. SSV occlusion rates were recorded at 100% for the same period. 55% of patients were classified as C2. Mean laser application time was 401.1 ± 92.6 s and 169.4 ± 56.8 s, while an average of 3986.6 ± 934.9 and 1643.5 ± 534.1 J were applied during ablation of GSV and SSV respectively. Three incidents of postoperative pain were recorded. Two patients exhibited partial proximal GSV recanalization, while two patients reported mild post-operative temporal paresthesia. No major complications were observed post-operatively. A significant improvement in patients' QoL was demonstrated through the CIVIQ-20 questionnaires. Mean pre-operative CIVIQ-20 total score was recorded at 77 ± 3.9, with a total score of 32.8 ± 2.8 being observed during 12 month follow-up.
Conclusions
Endovascular laser treatment using the 1470 nm radial fiber laser constitutes an effective and safe modality for treatment of CVD.
Highlights
-
•
Chronic venous disease (CVD) is one of the most commonly encountered health issues regarding venous disorders.
-
•
A paradigm shift has occurred in the 21st century regarding its treatment, offering less invasive treatment options.
-
•
This study was conducted in a series of 170 patients who were treated for CVD the 1470 nm diode laser with radial fiber.
-
•
Technical success rate was excellent with only a few minor incidents of post operative complications.
-
•
Patients' quality of life was drastically improved as it was recorded using a CIVIQ-20 questionnaire.
1. Introduction
Chronic venous disease refers to the peripheral veins' inability of adequate blood regulation. CVD of the lower extremities can present with various clinical signs, the most common being symptomatic varicosities [1]. The etiology, anatomic location, and pathology of the incompetence have led to the development of a classification system known as CEAP [1]. Classification of patients with CVD is essential in decision making regarding treatment management. Duplex colour scan is the basis for the assessment of CVD, with incompetence of the greater and small saphenous veins (GSV – SSV) being the commonest finding [1], [2], [3].
A number of therapeutic modalities have been introduced for treatment of CVD. Non-operative methods include compression therapy and pharmacological products [1], [3], [4] while ligation and stripping of incompetent saphenous veins along with varicosities excision, has been the gold standard surgical approach until the 21st century [5]. In the last 15 years, improvements in knowledge of venous pathology and circulation have led to the introduction of minimal invasive therapeutic options, demonstrating excellent technical success rates, and less complications and discomfort for the patient compared to open surgery. Such modalities include endovascular laser treatment (EVLT), radiofrequency ablation (RFA) and liquid/foam sclerotherapy [1], [6], [7], [8].
This study aims to evaluate the outcome and complications of 170 patients who underwent EVLT for treatment of CVD, using the 1470 nm diode laser and radial fiber.
2. Methods and materials
A retrospective data analysis was performed in our center, concerning patients who underwent EVLT for treatment of CVD of the lower extremities at a private clinic from 2013 to 2015, under the supervision of the main author. Patients eligible for surgery were exhibiting either GSV/SSV incompetence, or both and were classified as C2-C4 according to CEAP classification. Inclusion and exclusion criteria are summarized in table (Table 1).
Table 1.
Patient's inclusion and exclusion criteria.
| Inclusion Criteria |
|
| Exclusion Criteria |
|
Preoperative workup included physical examination for the evaluation and extent of varicosities. A colour duplex scan was performed in all patients for the assessment of retrograde blood flow in the GSV or SSV and identification of incompetent perforating veins. Venous incompetence was defined as retrograde blood flow >0.5s, after manual compression of the calf, followed by sudden release. Incompetent varicosities and perforator veins were marked with the patient in standing position. Written informed consent was taken from all patients, while they were also given a chronic venous insufficiency questionnaire (CIVIQ), defined as pre-CIVIQ, to complete prior to the operation. Data collection, analysis and calculations were performed using IBM SPSS statistics 23.0.
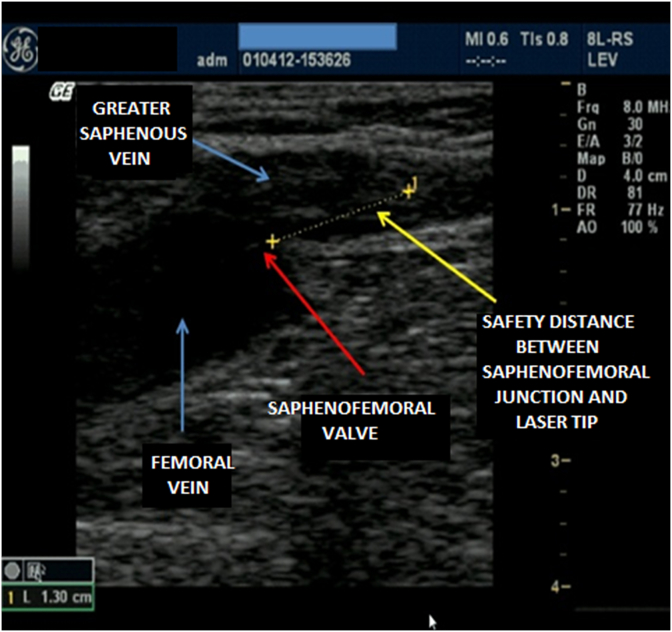
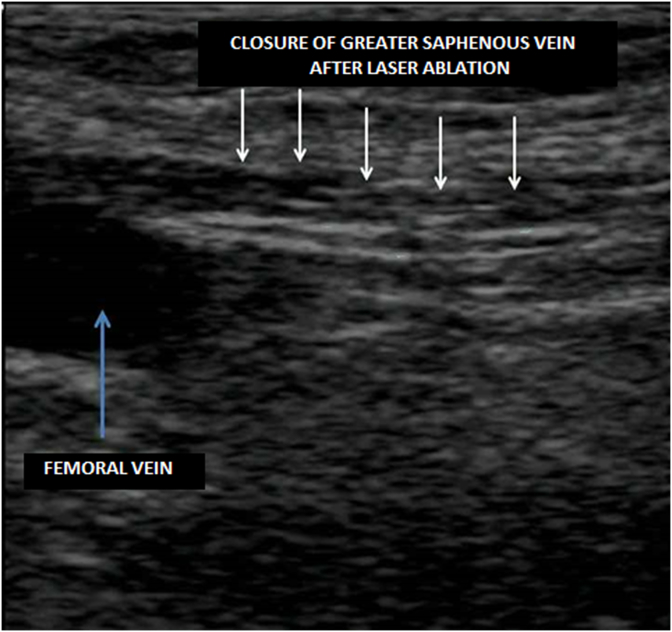
All procedures were performed by the main author, an experienced in simple and complex endoluminal procedures vascular surgeon, with an additional established experience in RF ablation and EVLT. Patients were operated under general or local anesthesia with mild sedation in supine or prone position, depending on GSV or SSV incompetence. With the patient in reverse Trendelenburg position, U/S guided percutaneous access of the GSV was achieved approximately 5–10 cm below the knee according to the Seldinger technique, followed by insertion of a 5 Fr sheath inside the GSV lumen. A 1470 nm radial optic fiber (Laser ELVeS Painless 1470 nm, Biolitec-Endotech, Athens) was inserted through the sheath with its tip advancing 2 cm distal from the safenofemoral junction (SFJ) (Fig. 1). In Trendelenburg position under ultrasound guidance, patients were administered tumescent anesthesia (500 ml N/S 0.9%, 20 ml xylocaine 2%, 10 ml bicarbonate 4%) within the fascial sheath of the GSV. For the SSV, access was obtained in the middle third of the calf, with advancement of the laser fiber as close as 2.5 cm from the safenopopliteal junction (SPJ) and perivenous administration of tumescent anesthetic under ultrasound guidance. With the power set at 9–10 W at thigh level combined with manual compression and 6–7 W at knee level, the laser fiber was withdrawn at a rate of approximately 0.2 cm/s with the help of audio feedback from the laser device. Withdrawal of the sheath was performed as the laser tip came in close proximity, treating the overlapping vein as well (Fig. 2). Ablation stopped approximately 1 cm proximal to the puncture site. Incompetent perforator veins were ligated, and marked varicosities were excised through stab microincisions closed with steri strips. All patients received low molecular weight heparin in a prophylactic dose during the first postoperative week. An elastic compression bandage was applied on the treated extremity and kept for 2 days, after which a class II graduated compression stocking was used for a length of approximately 1 month.
Fig. 1.
Placement of the laser tip near the saphenofemoral junction.
Fig. 2.
Intra-operative inspection of vein closure.
All patients had a follow up check at 1, 6, 12 months and then annually. Physical examination and colour duplex scan of the treated extremity were performed for the assessment of recurrent varicosities, GSV/SSV occlusion and possible reflux and recanalization. Patients were asked to complete a CIVIQ questionnaire at 1 and 12 months postoperatively, defined as post-CIVIQ-1 and post-CIVIQ-2 respectively.
The chronic venous insufficiency questionnaire (CIVIQ) is used to assess a person's quality of life (QoL) through 20 items, categorized in four dimensions (pain, physical, psychological, social). Scores range from 1 to 5. Minimum total score is 20, referring to an excellent QoL while maximum score is 100, reflecting a very poor QoL. It is a useful tool for the evaluation of patients' clinical status and symptoms, prior to lower extremity venous surgery [9].
3. Results
A total number of 170 patients underwent EVLT for treatment of CVI, involving 193 lower extremities. 94 (48%) right extremities and 99 (52%) left extremities with incompetence were treated, with bilateral insufficiency being observed in 23 (13%) patients. Ablation was performed in 176 and 24, GSVs and SSVs respectively. Mean age was 52.9 ± 11.2, with a ratio of women to men approximately 2.9. Most patients were CEAP classified as C2, with a percentage of 55%. Preoperative CIVIQ questionnaire showed an average score of 77 ± 3.9, demonstrating a rather low QoL (Table 2).
Table 2.
Patient's demographics and preoperative CEAP classification.
| No of patients | 170 |
| Male/Female ratio | 43 (26%)/127 (74%) |
| Mean patient age (y.o. ± SD) | 52.9 ± 11.2 |
| Extremities involved | 193 |
| Right | 94 (42%) |
| Left | 99 (58%) |
| Patients with bilateral extremities involved | 23 (13%) |
| CEAP Classification (number) | |
| C2 | 106 (62%) |
| C3 | 47 (24%) |
| C4 | 17 (8%) |
General anesthesia was applied only in 8 (5%) procedures as patience preference, while the remaining were performed under local anesthesia and mild sedation. Mean laser application time was 401.1 ± 92.6 s and 169.4 ± 56.8 s, while an average of 3986.6 ± 934.9 and 1643.5 ± 534.1 J were applied during ablation of GSV and SSV respectively. Phlebectomies where performed in all patients, while 11 patients underwent additional intraoperative sclerotherapy using polidocanol for treatment of telangiectasias and reticular veins. All operations have been met with technical success with no intraoperative complications (Table 3).
Table 3.
Operation statistics and perioperative data.
| Veins treated (number) | |
| GSV | 176 (86 R/90 L) |
| SSV | 24 (8 R/16 L) |
| Vein length (cm ±SD) | |
| GSV | 41.2 ± 8.2 |
| SSV | 16.7 ± 5.2 |
| Ablation time (seconds ± SD) | |
| GSV | 401.1 ± 92.6 |
| SSV | 169.4 ± 56.8 |
| Energy used (Joule ± SD) | |
| GSV | 3986.8 ± 934.9 |
| SSV | 1643.5 ± 534.1 |
| Tumescent anesthesia (ml) | 334.5 ± 91.4 |
| Postop complications (incidents) | |
| Bruising | 8 |
| Pain | 3 |
| Paresthesia | 2 |
| Hospital stay (hours ± SD) | 10.6 ± 2.3 |
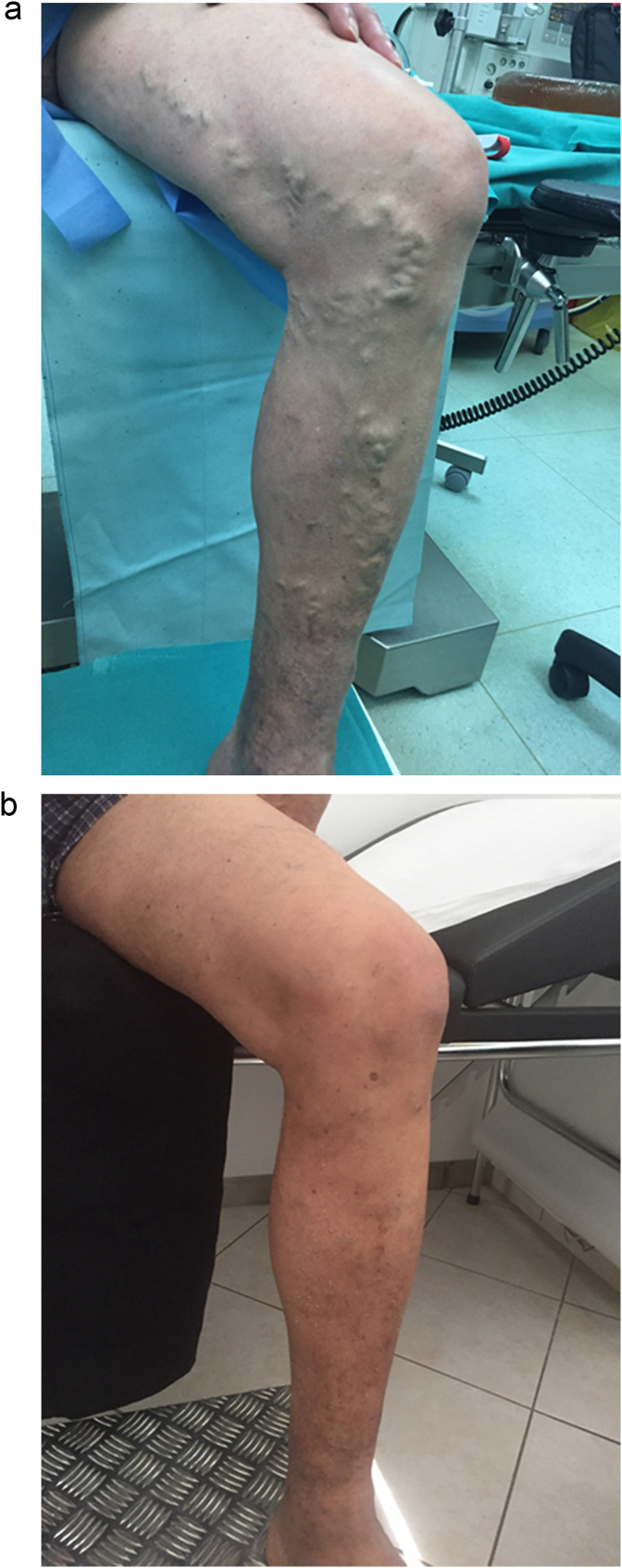
All patients were discharged home the day of operation. No post-surgical complications where observed such as ecchymosis, and skin burn. Eight incidents of local bruising due to phlebectomies or tumescent anesthetic were observed, while three incidents of postoperative pain were recorded. Complete follow up was performed in 160 (94%) patients. At 1 month follow up, three patients reported temporary mild tenderness, while two reported paresthesia. No thrombotic complications were reported throughout the follow up. Complete occlusion of GSV was recorded at 100% during 1, 6 and 12 month follow up and 98% during 24 month follow up respectively, as demonstrated with duplex scan. Two patients had a partial proximal (<20 cm) GSV recanalization and reflux without symptoms. SSV occlusion rate was recorded at 100%, for the same follow up visits. No recurrent varicosities were observed (Fig. 3a and b).
Fig. 3.
a, b. Excision of varicosities (pre and post-operatively).
Average pre-CIVIQ questionnaire score was 77 ± 3.9. Post-CIVIQ-1 average score of 36.3 ± 3, and post-CIVIQ-2 average score of 32.8 ± 2.8, reflect a significant increase in patients QoL after treatment. Most significant score differences were noted in the ‘pain’ dimension, with the pre-CIVQ ‘pain’ score being 17.4 ± 1.3, while the same score was recorded as 6.7 ± 1.2 and 6 ± 1.1 in post-CIVIQ-1 and post-CIVIQ-2 questionnaires respectively (Table 4).
Table 4.
CIVIQ scores as recorded preoperatively and at 1 and 12 month follow up.
| Pre-CIVIQ | Post-CIVIQ-1 | Post-CIVIQ-2 | p-value | |
|---|---|---|---|---|
| Pain Mean ± SD |
17.4 ± 1.3 | 6.7 ± 1.2 | 6 ± 1.1 | 0.001 |
| Physical Mean ± SD |
28.6 ± 2.8 | 14 ± 1.9 | 13 ± 1.6 | 0.001 |
| Psychological Mean ± SD |
18.5 ± 2 | 9 ± 1.5 | 7.8 ± 1.1 | 0.001 |
| Social Mean ± SD |
12.4 ± 1.3 | 6.6 ± 1.5 | 5.8 ± 1.3 | 0.001 |
| Total score Mean ± SD |
77 ± 3.9 | 36.3 ± 3 | 32.8 ± 2.8 | 0.001 |
4. Discussion
EVLT technique for treatment of CVD of the lower extremities is seeing an increasingly application for the past 15 years. Its safety and promising long-term follow up results render it an efficient alternate modality over ligation and stripping of saphenous veins [10], [11]. The aim of endovenous ablation is the occlusion and fibrosis of the vessel lumen, through application of thermal energy on the vessel wall. Technical success of EVLT depends on the amount of energy absorbed by the vein [12]. This process is largely affected by the mechanism of energy application and proper administration and type of tumescent anesthesia [13]. First generation, low wavelength lasers (800–1000 nm) deliver energy on hemoglobin, thus indirectly affecting the vessel. Newly developed, high wavelength diode lasers (1300–1600 nm) have the ability to apply energy in water, causing direct thermal damage on the endothelial cells of the vein wall [12], [14]. Energy required for the ablation of an incompetent vessel segment, depends on its caliber. Reports indicate that high wavelength diode laser such as the 1470 nm require the application of approximately 65–100 J/cm to cause complete occlusion and fibrosis of the vein lumen, with technical success rates reaching approximately 90–100% observed during 1 year follow up [10], [12]. Tumescent anesthesia functions in three different ways: it creates a protective perivenous halo, reducing damage to the soft tissues around the vessel wall; it reduces post-operative pain; finally, it contracts the vessel wall around the laser fiber to allow for an increased surface area, and higher ablation efficacy. Better contact between the vessel wall and the laser fiber can be achieved by promoting vasoconstriction with the application of adrenaline in the tumescent anesthetic [15].
In our study, power was set at 9–10 W in thigh and 7–8 W in knee level, with an average application of 80 J/cm for treatment of incompetent GSV and 68 J/cm for treatment of incompetent SSV. Technical success was 100%, while occlusion rates were recorded at 98% and 100% for GSV/SSV ablation respectively, as demonstrated during 24-month follow up. It is of importance to notice that the correct placement of the laser tip distal from the SFJ or the SPJ is essential in avoiding thrombus propagation in the deep veins, while proper application of tumescent anesthetic helps in elimination of adverse effects, namely skin burn and ecchymosis [12]. No such incidents or thrombotic complications where reported during the follow up period. Tumescent anesthetic also affects postoperative pain, reported only in three occasions as was observed in our study.
EVLT using the 1470 nm diode laser and radial fiber to be a safe and efficient method regarding treatment of chronic venous disease. Compared to open surgery, there are various analyses reporting no difference in technical success or recurrence rate, but much lower episodes of intraoperative or post-surgical complications [10], [11], [16]. Cases of hematoma and wound infection are significant lower after EVLT, with patients resuming earlier their normal activities. Postoperative paresthesia incidents after EVLT where similar compared to open surgery; still during EVLT this can be avoided with proper application of tumescent anesthetic [10]. In two cases from our series paresthesia was temporal and completely resolved after 5–6 weeks.
In a recently published report, Hirokawa M et al. compared a 1470 nm radial 2ring fiber with a 980 nm bare tip fiber for ablation of saphenous veins. His study indicates a significant difference between bruising and postoperative pain incidents. 14 patients who underwent ablation with the 980 nm bare tip laser experienced postoperative pain, compared to zero from the 1470 nm radial 2ring group. 32 events of bruising compared to 4 were recorded among the two groups respectively [17]. Both the mechanism of thermal energy application on the vein wall, and the type of the laser tip account for incidents of postoperative ecchymosis and pain. Lower wavelength lasers have a higher chance of perforating the vein wall, thus more cases of postoperative bruising and pain are recorded. The same applies for the laser tip, with bare tip fibers causing more damage on the vein endothelium and more incidents of wall perforation [18].
Compared to radiofrequency ablation (RFA), EVLT seems to have the same technical success and recurrence rate. Lower wavelength lasers account again for higher postoperative incidents of ecchymosis and tenderness, while there are reports of higher incidents of superficial thrombophlebitis following treatment with RFA [10], [19].
In conclusion, EVLT offers an excellent modality for treatment of chronic venous disease. While its efficacy demonstrates similar results compared to other treatment options such as open surgery and RFA, its intraoperative safety and lower rates of postoperative complications render it a viable treatment option. Higher wavelength lasers such as the 1470 nm should be preferred over first generation, low wavelength lasers, while bare tip fibers should be avoided, since they account for a number of postoperative complications. Tumescent anesthesia is also of major importance regarding technical success and avoidance of adverse effects, with its application depending solely on surgical experience and expertise. Further studies should be conducted with different wavelength lasers and laser tips in order to evaluate and compare their outcome.
Ethical approval
This was a retrospective data analysis, so ethical approval was not required.
Funding
Nothing to declare.
Conflicts of interest
All authors declare that they have no conflict of interest.
Consent
Written consent was obtained from all patients prior to the operation.
Acknowledgements
This work has been reported in line with the PROCESS criteria.
Agha RA, Fowler AJ, Rammohan S, Barai I, Orgill DP and the PROCESS Group. The PROCESS Statement: Preferred Reporting of Case Series in Surgery. International Journal of Surgery 2016; 36 (Pt A): 319–323 [20].
References
- 1.Eberhardt R.T., Raffetto J.D. Chronic venous insufficiency. Circulation. 2014;130(4):333–346. doi: 10.1161/CIRCULATIONAHA.113.006898. [DOI] [PubMed] [Google Scholar]
- 2.Marston W.A. PPG, APG, duplex: which noninvasive tests are most appropriate for the management of patients with chronic venous insufficiency? Semin. Vasc. Surg. 2002;15(1):13–20. [PubMed] [Google Scholar]
- 3.Gloviczki P., Comerota A.J., Dalsing M.C. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J. Vasc. Surg. 2011;53(5 Suppl):2S–48S. doi: 10.1016/j.jvs.2011.01.079. [DOI] [PubMed] [Google Scholar]
- 4.Nicolaides A.N. From symptoms to leg edema: efficacy of Daflon 500 mg. Angiology. 2003;54(Suppl 1):S33–S44. doi: 10.1177/0003319703054001S05. [DOI] [PubMed] [Google Scholar]
- 5.MacKenzie R.K., Allan P.L., Ruckley C.V. The effect of long saphenous vein stripping on deep venous reflux. Eur. J. Vasc. Endovasc. Surg. 2004;28(1):104–107. doi: 10.1016/j.ejvs.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 6.Kahle B., Leng K. Efficacy of sclerotherapy in varicose veins– prospective, blinded, placebo-controlled study. Dermatol. Surg. 2004;30(5):723–728. doi: 10.1111/j.1524-4725.2004.30207.x. [DOI] [PubMed] [Google Scholar]
- 7.Merchant R.F., DePalma R.G., Kabnick L.S. Endovascular obliteration of saphenous reflux: a multicenter study. J. Vasc. Surg. 2002;35(6):1190–1196. doi: 10.1067/mva.2002.124231. [DOI] [PubMed] [Google Scholar]
- 8.Lurie F., Creton D., Eklof B. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Eur. J. Vasc. Endovasc. Surg. 2005;29(1):67–73. doi: 10.1016/j.ejvs.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 9.Launois R., Mansilha A., Jantet G. International psychometric validation of the chronic venous disease quality of life questionnaire (CIVIQ-20) Eur. J. Vasc. Endovasc. Surg. 2010;40(6):783–789. doi: 10.1016/j.ejvs.2010.03.034. [DOI] [PubMed] [Google Scholar]
- 10.Siribumrungwong B., Noorit P., Wilasrusmee C. A systematic review and meta-analysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Eur. J. Vasc. Endovasc. Surg. 2012;44(2):214–223. doi: 10.1016/j.ejvs.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 11.Disselhoff B.C., Der Kinderen D.J., Kelder J.C. Five-year results of a randomised clinical trial of endovenous laser ablation of the great saphenous vein with and without ligation of the saphenofemoral junction. Eur. J. Vasc. Endovasc. Surg. 2011;41(5):685–690. doi: 10.1016/j.ejvs.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Galanopoulos G., Lambidis C. Minimally invasive treatment of varicose veins: endovenous laser ablation (EVLA) Int. J. Surg. 2012;10(3):134–139. doi: 10.1016/j.ijsu.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 13.Almeida J.I., Raines J.K. Laser ablation of cutaneous leg veins. Perspect. Vasc. Surg. Endovasc. Ther. 2008;20(4):358–366. doi: 10.1177/1531003508325055. [DOI] [PubMed] [Google Scholar]
- 14.Van Den Bos R.R., Van Ruijven P.W., Van Der Geld C.W. Endovenous simulated laser experiments at 940 nm and 1470 nm suggest wavelength-independent temperature profiles. Eur. J. Vasc. Endovasc. Surg. 2012;44(1):77–81. doi: 10.1016/j.ejvs.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 15.Saha S., Tiwari A., Hunns C., Refson J., Abidia A. Efficacy of topical local anaesthesia to reduce perioperative pain for endovenous laser ablation of varicose veins: a double-blind randomized controlled trial. Ther. Adv. Cardiovasc. Dis. 2016;10(4):251–255. doi: 10.1177/1753944716644140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Groenendael L., Van Der Vliet J.A., Flinkenflogel L. Treatment of recurrent varicose veins of the great saphenous vein by conventional surgery and endovenous laser ablation. J. Vasc. Surg. 2009;50(5):1106–1113. doi: 10.1016/j.jvs.2009.06.057. [DOI] [PubMed] [Google Scholar]
- 17.Hirokawa M., Ogawa T., Sugawara H. Comparison of 1470 nm laser and radial 2ring fiber with 980 nm laser and bare-tip fiber in endovenous laser ablation of saphenous varicose veins: a multicenter, prospective, randomized, non-blind study. Ann. Vasc. Dis. 2015;8(4):282–289. doi: 10.3400/avd.oa.15-00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vuylsteke M.E., Thomis S., Mahieu P. Endovenous laser ablation of the great saphenous vein using a bare fibre versus a tulip fibre: a randomised clinical trial. Eur. J. Vasc. Endovasc. Surg. 2012;44(6):587–592. doi: 10.1016/j.ejvs.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Goode S.D., Chowdhury A., Crockett M. Laser and radiofrequency ablation study (LARA study): a randomised study comparing radiofrequency ablation and endovenous laser ablation (810 nm) Eur. J. Vasc. Endovasc. Surg. 2010;40(2):246–253. doi: 10.1016/j.ejvs.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 20.Agha R.A., Fowler A.J., Rammohan S., Barai I. Orgill DP and the process group. The process statement: preferred reporting of case series in surgery. Int. J. Surg. 2016;36(Pt A):319–323. doi: 10.1016/j.ijsu.2016.10.025. [DOI] [PubMed] [Google Scholar]