Dear Sir,
When undertaking surgery for nonunion of scaphoid fractures, appreciation of the three dimensional (3D) anatomy and hence accurate restoration of the original shape of the bone is difficult. Computerised tomography (CT) is regularly used to evaluate scaphoid nonunions slice by slice before surgery. As a potential aid for surgical planning, we have developed a method for producing 3D printed anatomical models of the un-united scaphoid and the intact scaphoid based on the contralateral side. Bilateral CT scans of the wrist were obtained. Virtual 3D CT models of the proximal and distal nonunion fragments and the intact scaphoid, mirrored to the injured side, were created using custom image segmentation software (Dobbe et al., 2011) (Figure 1). Printing was performed using a Blueprinter M2 (Blueprinter®, Copenhagen, Denmark) based on thermoplastic powder with 100 µm resolution.
Figure 1.
(a) Image acquisition: a bilateral CT scan of a unilateral scaphoid nonunion and the normal scaphoid; (b) Image post-processing: virtual 3D models based on the segmented image of the scaphoid nonunion and mirrored image of the contralateral scaphoid.
We evaluated the use of the 3D models in an experimental bench study on palmar plate fixation of the scaphoid, which has been recommended for treatment of some nonunions (Dodds and Halim, 2016). Synthetic printed models were produced from eight patient cases with unilateral scaphoid nonunion with palmar bone loss. Three operators simulated corrective surgery on the synthetic bone fragments using Y-shaped titanium 1 mm thick mini plates (Cibei, Cixi, China). In one group, the plate was bent conventionally using a freehand technique without the use of the anatomic model of the intact scaphoid. In a second group, the plate was prebent onto the model of the intact scaphoid. In total, 48 simulations were performed (three operators × two treatment groups × eight cases). The operators repositioned the fragments without seeing the anatomic model, the plate serving as a guide in the prebent group. The plates were fixed to the fragments using rapid adhesive cyanoacrylate glue (Loctite 545, Henkel, Dusseldorf, Germany) to minimize scattering on subsequent CT scans (Figure 2).
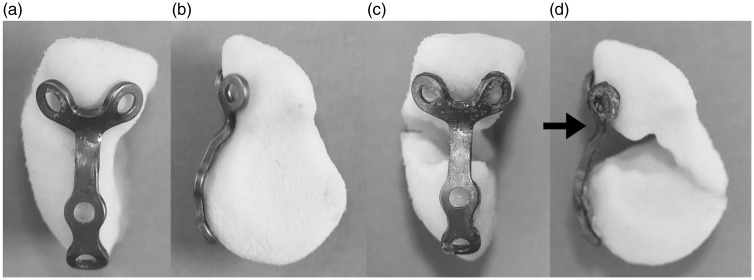
Figure 2.
The 3D printed models with a prebent plate in situ. (a) Palmar view; (b) ulnoradial view of the anatomic model based on the contralateral intact scaphoid; (c) palmar view; (d) ulnoradial view of the repositioned scaphoid nonunion fragments.
CT scans of the reconstructed assembly were obtained, and virtual 3D models of the fragments and plates were created. Displacement of the distal fragment relative to the proximal fragment was quantified in 3D space using the contralateral scaphoid as reference. The intraoperatively bent plate was also virtually superimposed onto the prebent plate, which followed the contours of the anatomical model. The gap between the virtual plates was measured at the level of the waist of the scaphoid. Based on analysis using the Wilcoxon Signed Ranks test, only fragment supination differed significantly between the plating techniques (median difference = 9o; p = 0.02). Compared to prebent plates, intraoperatively bent plates consistently showed malalignment in a palmar direction at the waist of the scaphoid and therefore prominence of the plate at this level. The potential clinical significance of the differences in alignment found is uncertain. A limitation of the study is the use of glue to secure the plates. Screws would press the plate against the bone, possibly giving a better fit, but also might pull the bone fragments out of alignment.
The method of creating synthetic models of the scaphoid may be useful in planning other methods of scaphoid fixation; for example, predicting the size of the bone graft needed to fill the defect at the nonunion site. Currently, medical-grade polyamide, polycarbonate or resin models can be printed in a few hours at low cost, and subsequently used in the operating room after sterilization. Synthetic models could also be used as an education tool for training surgeons and as a communication tool with patients to improve shared decision-making. Additionally, Haefeli et al. (2015) showed promising results with custom-manufactured titanium templates based on the contralateral scaphoid using selective laser melting technology. Further study is needed to evaluate whether clinical outcomes can be improved and the additional costs are justified.
Acknowledgments
We thank the following operators for performing the surgical experiments: Geert A. Buijze, MD, PhD; Simon D. Strackee, MD, PhD; George S. I. Sulkers, MD.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Paul W. L. ten Berg received a PhD grant (2014) from the Academic Medical Center (Amsterdam, The Netherlands) supporting this research.
References
- Dobbe JG, Strackee SD, Schreurs AW, et al. Computer-assisted planning and navigation for corrective distal radius osteotomy, based on pre- and intraoperative imaging. IEEE Trans Biomed Eng. 2011, 58: 182–90. [DOI] [PubMed] [Google Scholar]
- Dodds SD, Halim A. Scaphoid plate fixation and volar carpal artery vascularized bone graft for recalcitrant scaphoid nonunions. J Hand Surg Am. 2016, 41: e191–8. [DOI] [PubMed] [Google Scholar]
- Haefeli M, Schaefer DJ, Schumacher R, Muller-Gerbl M, Honigmann P. Titanium template for scaphoid reconstruction. J Hand Surg Eur. 2015, 40: 526–33. [DOI] [PubMed] [Google Scholar]