Abstract
Objectives:
This research was intended to provide a greater understanding of the context and needs of aged care seating, specifically:
To conduct an audit of typical chairs used in aged care facilities;
To collect data about resident and staff experiences and behaviour around chairs in order to gain a deeper understanding of the exact issues that residents and staff have with the chairs they use at aged care facilities;
To identify positive and negative issues influencing use of chairs in aged care facilities;
To deliver evidence-based recommendations for the design of chairs for aged care facilities.
Methods:
Methods included a chair dimension audit, interviews with residents, experts and carers and observations of aged care residents getting into chairs, sitting in them and getting out.
Results:
Results showed that residents, experts and carers all prefer chairs which are above the recommended height for older people so that they will be able to get out of them more easily. Armrests were essential for ease of entry and egress. However, many residents struggled with chairs which were also too deep in the seat pan so that they could not easily touch the floor or sit comfortably and were forced to slump. Most residents used cushions and pillows to relieve discomfort where possible.
Conclusion:
The implications of these issues for chair design and selection are discussed. Variable height chairs, a range of chairs of different heights in each space and footrests could all address the height problem. Chair designers need to address the seat depth problem by reducing depth in most aged care specific chairs, even when they are higher. Armrests must be provided but could be made easier to grip. Addressing these issues would increase access to comfortable yet easy-to-use chairs for a wider range of the aged care population.
Keywords: Aged care, seating design, ergonomics, anthropometrics, sit-to-stand transfer, occupational therapy
This article reports on a research study intended to provide a greater understanding of the needs of aged care seating users in context. First, we provide the background to the anthropometric issues of seating in aged care and then present the results of an audit, observations and interviews which were carried out across four aged care facilities in Queensland, Australia, to investigate whether or not the available seating met both anthropometric and user requirements for the aged care context. The chair audit (including measurements) was conducted across two facilities and four websites. Interviews were conducted with staff from four facilities and one outside organisation, and observations and interviews with residents were conducted at two facilities. Discussion of the findings and their potential implications follows.
Seating research in relation to older people
An enormous amount of research has been conducted in relation to seating, and particularly the ergonomics of seating and chair design. Much of it has been translated into design guidelines now contained in national and international standards for chair design.1
There are many benefits for older people in using appropriate chairs. As residents of care facilities tend to have reduced functional capacity, with mobility limitations particularly common,2 suitable seating design is imperative. Mobility and independence are maintained if a person is able to get in and out of a chair with relative ease, without having to wait or ask for assistance. Additionally, appropriate seating encourages good postural stability and support while reducing pain, fatigue, venous thrombosis (VT) risk and pressure sores. Good seating may also encourage social interaction, improve respiratory function and intake of food and drink.3,4 Inappropriate seating, however, reduces independence by increasing reliance on others. Poor seating can also simply be uncomfortable, and particularly in older adults with cognitive impairments, discomfort can lead to frustration and behavioural issues.4
However, providing recommendations for older adults in residential aged care environments is complex. Those still independent and mobile require a chair that is easy to get into and out of independently, while encouraging healthy posture but not restricting movement. Those with less mobility and postural control require greater contoured support and safe-assisted transfer.5 So while the ergonomic specifications for seating furniture in office environments are quite explicit, recommendations for aged care seating furniture tend to be more ambiguous. Publicly available information on choosing a chair for older people tends to be directed towards individuals.6,7 In care facilities, physiotherapists and senior staff have made decisions about the most appropriate seating furniture for residents.4 More recently, facilities’ interior designers, rather than carers, physiotherapists or occupational therapists, are liaising with manufacturers in relation to chair design specifications (Tatum, 2015, personal communication).
Sit-to-stand transfer
The act of standing from a seated position is a physical task performed regularly throughout a day and is one of the most important measures of physical function.8 Often referred to as chair-rise, or sit-to-stand (STS) transfer, this ability is key to maintaining mobility and independence and has been identified as the most important factor for older people when choosing a chair.9,10
Biomechanically, rising from a chair is perhaps one of the toughest tasks and involves moving from a static, seated position through an unstable transition phase, to a ‘quasi-static’ (standing) position.11 Successful transition requires significant motor control, momentum and coordination.12 A number of strategies have been observed and classified: momentum transfer (MT), stabilisation (or exaggerated trunk flexion, ETF) and dominant vertical rise (DVR). Strategies differ in the amount of work required by the trunk, the knee and the hip. Some strategies require more strength, some more time, some are used in conjunction with others.10–13
Scarborough et al.12 observed chair-rise strategies in older adults with functional limitations and concluded MT to be the most common, efficient and preferred chair-rise strategy. In another study of older adults, the most common strategy used was leaning forward (MT), the least used strategy was sliding forward (ETF).10 However, older adults employ many strategies and when faced with difficult situations, they will alter their strategies, employ several strategies or avoid certain types of seating altogether.10,14
The results of these studies into STS have been worked into chair design guidelines that can reduce STS difficulties and improve function for older people. Several characteristics of chairs have been found to impact STS performance; the seat height and size, the space underneath the seat,15 the angle of the seat and backrest and whether the chair has armrests are among the most important. Unfortunately, however, some of the factors that make it more difficult to rise from a chair: lowered seat height, increased posterior seat tilt and increased back recline, for example, tend to be the same features that make the chair more comfortable to sit in for extended periods.9
Anthropometrics and chair design guidelines for older people
The information in this section summarises specifications found in the literature on chair design guidelines for chairs used by older people. Where available the recommended values are presented alongside relevant anthropometric and ergonomic data for older members of the population;1,16,17 the crucial elements being seat height, seat size and armrests.
Seat height
Seat height is the most important factor for easy STS6 and is measured as the height of the compressed cushion to the floor.3,5 Higher seat height reduces the motion and strength required by the hips and knees to rise from the chair, and less exertion is required to rise from higher chairs as the distance travelled by the body is smaller.5 Furthermore, those with limited ability to flex the hips, such as after hip replacement or due to the effects of arthritis, will not be able to use lower set chairs. Lower seating also increases pressure on the pelvis rather than distributing it along the thighs.6 Thus, providing seating with a variety of heights is recommended where possible.5,9
However, older adults are not necessarily more comfortable using higher seats. Seats that are too high can compromise stability while seated because a person’s feet will be unable to reach the floor;9 this increases discomfort under thighs and pressure behind the knee,5 which creates a VT risk. Permanently higher seats with footrests are an option for some older people,5,6 and indeed use of footrests is a recommendation for office seating that may need to cater for older employees.16 However, this solution may not be feasible in aged care environments where the footrest could become a trip hazard.5 Motorised chairs that rise up with the person reduce joint stress on rising, but can leave the person unbalanced at the end of rising. Furthermore, as well as being expensive, motorised chairs are generally not viewed favourably as they encourage dependency on the chair rather than on the use of the person’s remaining abilities.5 Thus, although they have their place, they are not discussed further in this article.
A fifth percentile Australian female over the age of 65 (we’ll refer to her as ‘Jean’) has a popliteal height of 330 mm, while the mean dimension for the same population is 379 mm. Studies of seating for older people have recommend an optimal height of 430 mm,9 or 470 mm with a footrest.18 According to Christenson,15 chair height for older women in care facilities should not exceed 431 mm. However, Christenson also recommended that to best cater for the majority of residents, facilities should provide a variety of lounge chairs with seat heights ranging from 380 to 457 mm. All these recommended seat heights are higher than the mean popliteal height for the age group of 379 mm,16 and suitable only for those elderly females above the 50th percentile, not including ‘Jean’.
Seat size (depth and width)
Seat depth has been identified as an important factor in seating comfort for older people.5 Seats should be able to support the full length of the thighs without the sitter having to slouch or lean to support the back,1,6 and there should be space behind the knees for circulation.4 ‘Jean’ has a buttock to popliteal length of 376 mm and a hip breadth of 277 mm. The mean dimensions for the same population are 440 and 338 mm, respectively.9,18 Kothiyal and Tettey16 recommend 376 mm for both office and bus seating, exactly right for ‘Jean’. The current Australian Standard for fixed height chairs suggests an effective seat depth range of 380–480 mm.1 However, the Standard also notes that to allow for a majority of users to benefit from the backrest, a depth of 440 mm is preferred, which is way too deep for ‘Jean’, or anyone below the mean dimension.
Width of the hips ‘plus a clenched fist on either side’ is recommended to allow for changes in sitting position while in the chair.3,6 Kothiyal and Tettey16 use hip breadth for the 95th percentile female for seat width and recommend a value of 409 mm.
Armrests
Armrests that are high and extend to the edge of the seat have been found to support chair-rise performance by maintaining stability while rising.9 Designs that are lower at the back than the front are preferred,15 and researchers have found that armrests around 250 mm from the seat best facilitate STS performance.19 Holden and Fernie18 recommended that armrests should have a height of 730 mm from the floor at the front and 250 mm from the seat at the back, with a width of 120 mm and a protrusion of 120 mm from the front edge of the seat.
The existing literature shows that guidelines do exist for some aspects of chairs in aged care, but not all of them cater for ‘Jean’ particularly well. The next sections describe our research with residents, and therapists and chairs in aged care facilities.
Aged care seating study
Between December 2015 and March 2016, we conducted an audit of the various types of seating available across two residential aged care facilities. Eight main types of seating were recorded and measured. We also conducted observations and semi-structured interviews with aged care residents, carers (staff) and therapists (experts) in order to understand how the residents and staff related to the chairs available and to video-record the STS processes used by the residents. Participants were from four aged care facilities, and one therapist was from a specialist service for independent living. We also conducted a website audit of published aged care specific chair dimensions in 2017. This research was funded by a commercial client (Lifecare Furniture Pty Ltd) who commissioned this research from the university in order to improve the design of their own offerings in seating for aged care and have given full permission for publication of this material. There is no perceived conflict of interest as their chairs were not assessed as part of this project since none of the facilities visited were clients of theirs.
Participants
Participants were 19 aged care residents (6 male, 13 female), five staff members (3 Facility Managers, 1 Assistant in Nursing (AIN), 1 Clinical Manager) and two experts (1 Occupational Therapist, 1 Physiotherapist). The resident participants were representative of the gender balance of aged care residents in Australia, which is 69% female.20 The staff and experts were representatives from four aged care facilities and one specialist service for independent living and assistive technology. For residents, inclusion criteria were that participants should be living full time in the facility, and participants had to be capable of giving informed consent and were selected by the staff at the facilities. The researchers were not permitted by the facilities to approach potential resident participants resident directly. All data collection was approved by the university Human Research Ethics committee (approval number 1500000968) and by each facility involved. All participants signed a consent form and image release form and received a AUD$25 gift card in return for their participation.
Data collection methods
An audit was conducted on all available communal chairs in two different aged care residences to record context and dimensions. Aged care facilities representing low-end, high-end and mid-range facilities (in terms of cost of care and market position) were invited to participate in order to capture differences across facilities due to level of investment in the facilities’ furniture. The website audit was based on a Google search for Australian-based aged care seating furniture providers in order to provide direct comparisons to chairs encountered in facilities. A total of four websites (overall 54 seats) were audited as they were the ones selling aged care furniture in Australia which included appropriate dimensions on their sites.
The primary research method used with participants was a semi-structured interview accompanied by video-recorded observation. This allowed us to collect opinions and behavioural data simultaneously. During the semi-structured interview, participants (some alone, some in groups or couples) were asked to answer 10–15 questions about their experiences of chairs in aged care (Appendices 1–3). During the observation, aged care residents were also asked to show the researcher how they would normally sit down in a chair. Then, after the interview questions, the residents were asked to show how they would stand up from the chair. Since the whole session was video recorded, we also captured data about how they sat in the chairs, if they moved around, pulled themselves up, slumped and so on, and what other props they used (e.g. walking aids, footrests, cushions and pillows).
The types of chairs varied depending on the location of the observation. Some chairs were high-back lounge chairs and dining chairs available in the communal areas of residential facilities. However, when observations were held in residents’ private rooms, chairs ranged from occasional chairs provided by the facilities to office chairs, lounge chairs and recliners that belonged to the residents and had been brought to the facility when they moved in. The interview questions and structure changed slightly for residents, experts and carers but covered the same information based on their expertise (see Appendices 1–3).
Data analysis
The audio-visual data were imported into Noldus Observer XT software for coding.21 The coding scheme used (Appendix 4) was based on the literature and the initial viewing of the video data, combined with expert input from the research team. It was designed to help us to understand which issues were most important to the residents, experts and carers. The coding scheme included top-level codes from answers to interview questions, such as which is your favourite chair or what do you think of the height and comfort of the chairs. For each code, there were ‘modifiers’ which allowed us to code which chair features were relevant to the particular comment. This allowed us to understand, for example, whether armrests were important for STS or whether seat height and depth were related to comfort.
When coding of video data was complete, the resulting codes were exported to MS Excel to provide quantitative results. These methods were strongly grounded in the approaches we have developed over the past 10–15 years,22 which are focussed on finding out what people actually do in their day-to-day lives rather than simply collecting opinions and beliefs or measuring objects.
Findings
First, the findings of the seating audit are presented, supported by quotes from resident and staff interviews and relevant images of seating, followed by findings from the website audit. Finally, results from the interviews and observations are presented, supported by quotes, images of seating in use and STS transfer in progress.
Seating audit
The seating audit indicated that aged care facilities provide a variety of seating, particularly in communal and public spaces. Table 1 provides the dimensions for the high-back lounge chair used for observations in one mid-range facility. Table 2 provides dimensions of all communal chairs available in a high-end ‘club’ facility. All of the chairs included in Tables 1 and 2 were provided by a facility-approved aged care seating manufacturer.
Table 1.
High-back lounge chair – mid-range facility.
| Type, location and example | Seat height | Seat width | Seat depth | Armrest height – from floor | Armrest width | Back height – from floor | |
|---|---|---|---|---|---|---|---|
| High-back lounge Recreation hall/lounge room |

|
460 | 485 | 480 | 630 | 100 | 970 |
All measurements are in mm.
Table 2.
Chair audit results from high-end facility.
| Type, location and example | Seat height (sloped backa) | Seat height compressed | Seat width | Seat depth | Armrest height from floor | Armrest width | Back height from floor | |
|---|---|---|---|---|---|---|---|---|
| Wicker chair Waiting areas |

|
460 | 600 | 500 | 610 | 115 | 760–840 | |
| High-back lounge TV area |

|
480 | 455–460 | 510/1025 | 515–530 | 660 | 70 | 1040 |
| Dining casual Communal meals area |

|
475–505a | 490–580 | 485 | 665 | 45 | 915 | |
| Dining Private dining room |

|
440–480a | 460 | 425 | 970 | |||
| Day chair Bedrooms and cinema |

|
480 | 470 | 490 | 520 | 650 | 70 | 910 |
| Woven Outdoors |
|
440 | 400–590 | 460 | 640 | 40 | 910 | |
| Café Coffee shop reception |

|
410–445a | 420 | 390 | 645 | 35 | 815 | |
All measurements are in mm.
signifies that the seat pan is sloped backwards so that it is lower at the back than at the front.
While there was a variety of chair types on offer, and slight changes in size across the range of seating, the chairs used most frequently by residents in the communal areas – the high-back lounge and the dining chair – were quite similar, particularly in terms of seat height and depth. There was no change in size within a particular chair type – all high-back lounges were identical, for example. Space and financial constraints play a role in the provision of seating in aged care contexts. The images below (Figures 1–3) provide a context comparison across three facilities: a four-year old, high-end club facility; a slightly older, mid-range facility; and an older secure dementia facility. All facilities highlighted the need for a home-like environment, however, the style and the need varied depending on the level of care. Some seating, particularly in the dementia secure facility, was simply standard seating available at any major retailer. Facilities relied on advice from in-house physiotherapists or occupational therapists; they used approved suppliers and were guided by recommendations from those suppliers:
‘Who chooses the furniture?’ ‘Our property division. But it’s from a company that are specific to aged care’. (Staff 3)
Figure 1.
Chairs lined up together in a high-end ‘Club’ facility.
Figure 2.
Uniform seating in mid-range facility.
Figure 3.
Seating options in a (low-end) secure dementia facility.
In addition, a review of websites of Australian aged care furniture manufacturers was conducted and seat depth and height for lounge chairs (NOT recliners, automated chairs, two or three seaters or bed chairs) were assessed.
None of the experts or carers was aware of any specific dimensions for appropriate seating for aged care. The occupational therapist and physiotherapist had guidelines they would refer to, but these were general recommendations on fitting a chair to an individual. Facilities were reliant upon manufacturers for appropriate specifications:
As a company we have approved suppliers…whatever specifications they’re making their stuff to we’re pretty much trusting the fact that it’s going to be suitable for the residents. (Staff 1)
In the high-end and mid-range facilities, the seating was relatively fixed and served a dedicated purpose (e.g. for the lounge room, cinema, café or activities areas). In the older secure dementia (low-end) facility, only the dining chair was specifically designed for aged care. Here, the priority was a home-like appearance and cleanliness. By comparison, the high-and mid-range facilities had several communal spaces where maintaining a uniform appearance was a priority. Seating was carefully lined up side by side with a lot of space in front, leaving sufficient room for residents to place wheelie walkers in front of their seats or to manoeuvre through in their wheelchairs.
Websites were identified using a Google search on the term ‘aged care seating.au’ and then searched through for those containing relevant interior dimensions for their seating. Most websites state only the external dimensions but some list seat height and/or depth for some of their chairs. These dimensions (Table 3) suggest that the chairs we audited in situ (Tables 1 and 2) were not out of the ordinary for their context. In fact, we were told by an aged care furniture manufacturer that these are the standard kinds of dimensions in use in the industry and perceived to be in demand by the clients.
Table 3.
Chair audit results from Australian websites.
| Provider | Lounge chairs with dimensions listed | Seat height | Seat depth |
|---|---|---|---|
| Direct Online23 | 3 | Mean 423 | 480 (only one listed) |
| Regency Health Care24 | 2 | Mean 455 | Mean 485 |
| Aidacare25 | 2 | Mean 520 | Mean 485 |
| Healthcraft Furniture26 | 47 | Mean 473Range 420–510 |
No dimensions available |
All measurements are in mm.
Interview and observation results
In this section, first resident and then expert and carer perspectives and examples are presented, with quotes from interviews and images from observations used to illustrate the findings.
Residents’ perspectives
Figure 4 outlines the key features of chairs that were discussed by resident participants in this research. It is an illustration of frequency. For example, the most common feature coded in the analysis was Armrests, followed by Seat height and so on. A list of every incidence of each code was generated. From here, the list was filtered for the most frequently coded modifiers. These key modifiers were then filtered again in a separate analysis that included the other modifiers they were coded with. For example, Armrests featured most frequently with the modifiers STS transitions and positive, meaning that when participants spoke about armrests, it was generally in a positive context and in relation to STS transitions. Quotes and images are provided on the following pages to illustrate the findings relating to armrests and STS, seat height and seat depth.
Figure 4.
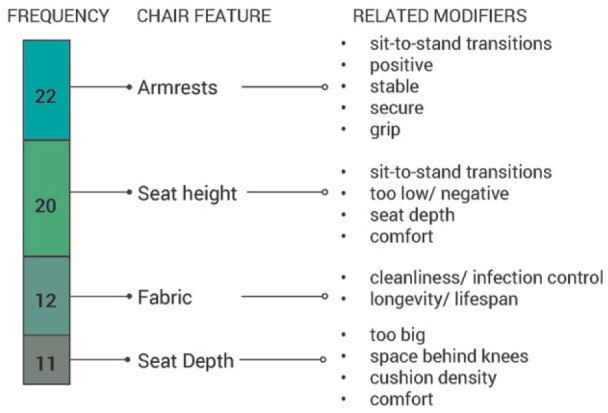
Residents’ perspectives on chair features.
Armrests and STS
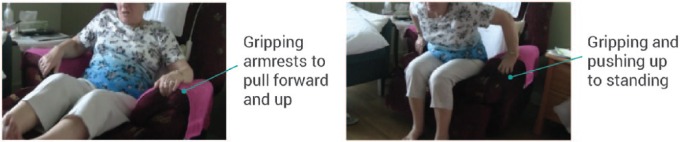
When armrests were available they were used 100% of the time regardless of the resident’s level of mobility (Figures 5 and 6). They were viewed as a tool to aid STS transitions, used to pull forward and push up when standing up, and as guidance and support when sitting down:
…if I have armrests I’ll use them…I hold one arm on the armrest and another on the table…so I can balance myself as I’m standing. (Resident 17)
…if you’ve got the armrests, you’re half-way there [to standing]. (Resident 3)
…unless they’ve got a good arm to push yourself up from, some of them are difficult to get out from because you slip…you’ve just gotta watch if you’re standing up if there’s no arm. (Resident 4)
Figure 5.
Using armrests to pull forward and sit up, then stand up.
Figure 6.
Leaning forward and pushing up on armrests during STS transition.
While armrests provided stability during STS transitions, they also provided security while sitting and a sense of independence as the residents knew they could get up when they wanted to without needing assistance:
It is nice at a restaurant if they have armchairs, it makes all the difference to how you feel… if you’re independent and you’ve got an armchair you feel like anybody else. (Resident 3)
However, there was mention of some armrests being too broad and therefore difficult to grip securely (Figure 5):
… [armrests with] the wooden ends… I find that far better than the padded ones so you can actually get a grip. (Resident 3)
When trying to stand from a chair without armrests, residents would push on other features such as the table, seat back or the seat itself (Figure 7). One resident said having no armrest made her feel very insecure:
I hate this, it’s a real problem for me, I don’t know what I’d do, I’d just panic, I don’t like it. I’m looking for somewhere to push. (Resident 5)
Figure 7.
Standing up using table and chair seat (walker placed behind resident).
Of STS transitions observed, 90% involved careful, considered techniques. All STS transitions involved leaning forward and pushing up on something – armrests when they were available, the seat, the table, a walker or stick. Figures 5–8 illustrate STS transitions using various techniques and aids.
Figure 8.
Multiple attempts at standing from a chair that is too low for the resident, using armrests and walker.
Sometimes residents would make an attempt to get up on their own, before using some assistance, and 90% of those observed during STS needed more than one attempt to stand (Figure 8):
…so I’ll just get up…[several attempts]…eventually [laughs]. (Resident 2)
As the quotes and figures demonstrate, for some residents, a mobility aid played a key role in the success of their STS transitions. For others, it provided security and balance once standing. Walkers or walking sticks are essential for most people in aged care. Figure 9 illustrates the aids used by the residents in this research.
Figure 9.
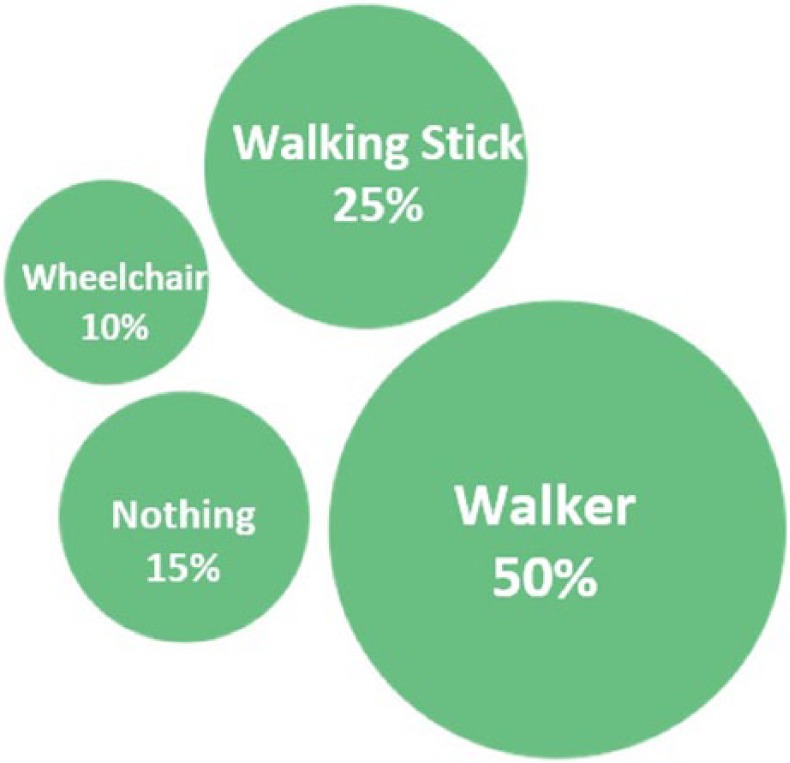
Mobility aids used by residents in the study.
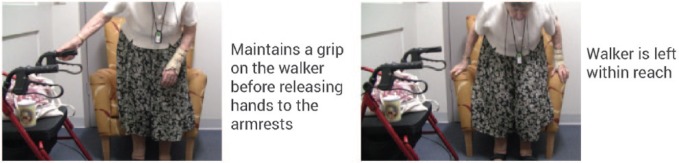
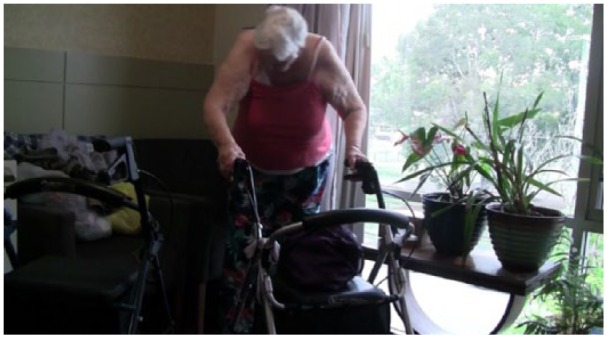
Mobility aids are particularly relevant in STS transitions. Figure 10 illustrates a resident sitting down with the walker to the side, and Figure 11 shows a resident reversing into a chair using her walker. When sitting down, many residents reversed into the chair, and there was a preference for the walker or walking stick to be close-at-hand:
I use my stick or the walker…always have something here. (Resident 14)
I usually take the wheelie walker to the chair, until I feel it on the back of my legs and then I sit right back into it. (Resident 1)
…with the lounge chair in my room I’ve really go to push myself up off it to get out of it. And I need to have the wheelie walker poised so that I can get on the wheelie walker to go where you want to go. (Resident 1)
Figure 10.
Sitting down using walker and armrests.
Figure 11.
Reversing into chair using walker.
However, storing the walking aid close to them while sitting so they can easily get up again could be an issue:
…well hopefully it’s at a chair behind you [the walker], but you can’t always do that so beside you or right in front of you. (Resident 4)
…sometimes the walker is over there, B* goes mad if I leave the walker away. (Resident 8)
…there’s not much room in the room, so I’d move it round [wheelie walker] so that it was easily accessible. (Resident 1)
Seat height
Residents approached seat height mostly from the perspective of STS transitions. There was a consistent view that many chairs were too low for easy STS, although we observed many seats that were too high for comfortable sitting. Figure 12 shows examples of chairs which were too high and too low.
Figure 12.
Examples of sitting and chair height.
…it’s too low… I’ve really got to heave to get out… if it’s just that bit higher you can get straight out. (Resident 3)
I find the lounge chair in my room too low. It’s alright to sit down and watch television in, but then it’s hard to get out of. (Resident 1)
…terrible [of high back lounge chairs]… too low to get yourself up and out of them. (Resident 17)
There was also repeated mention of the variety of sizes of residents and that a chair that suited one would not suit another:
The thing the manufacturer should do is make the same chair in four to six sizes. (Resident 3)
I think that they should be adjustable for height, because I’m not the only tall person in this place…. (Resident 11)
It’s quite alright with me, but I don’t know about someone that’s six foot two in height, I’m only five foot two…. (Resident 10)
Seat depth
For residents, seat depth was very much linked to comfort as well as recognition that space behind the knee was important for their circulation. The general perspective was that most of the seating residents had experienced in the aged care setting was too deep. Slumping (posterior pelvic tilt) was consistently observed due to seats being too deep (Figure 13). This meant that residents would shift their feet closer to the floor by tilting their pelvis, creating an unsupported space behind the back, often filled with a cushion or pillow. Pillows and cushions were observed on seats in every private room we accessed. The cushions were used for additional back support to help maintain an upright position while sitting (Figure 14), effectively reducing seat depth:
[takes cushion away from back]… see that takes me back further… I think I prefer the cushion… or I have to push my bottom back into the chair. (Resident 10)
… they stop sometimes the blood circulation [at back of the knee]…You sit far back on them and, it hurts. (Resident 17)
So many arm chairs have deep seats so you’re right in the back. Where I’m personally more comfortable sitting upright in a chair with a shorter seat so that my knees are actually beyond the edge. (Resident 3)
The average chair is too small for me… I like… having a deep seat. (Resident 2) Yes, well, you’ve got longer legs. Our knees get to the end [front of seat] before our bums get to the back. (Resident 3)
Figure 13.

Excess seat depth leading to slumping.
Figure 14.

Using a cushion to sit forward and upright.
Expert and staff perspectives
Figure 15 outlines the key features of chairs that were discussed by experts and staff members. It is again an illustration of frequency. A list of every incidence of each code was generated and the list was filtered for the most frequently coded modifiers. Quotes and images are provided on the following pages to illustrate the findings.
Figure 15.
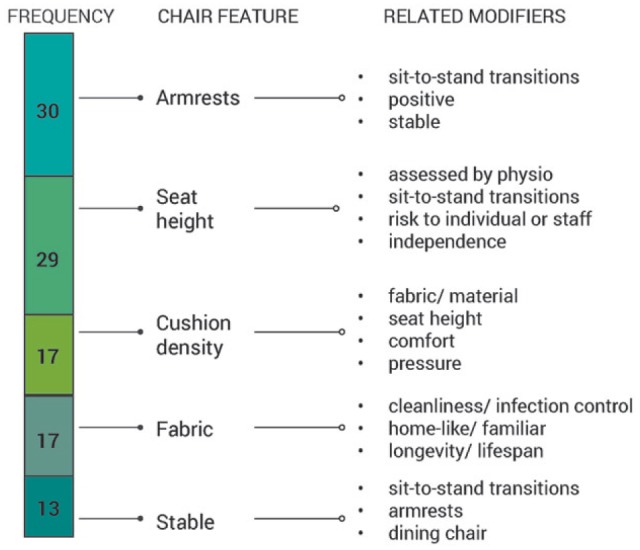
Expert and staff perspectives on chair features.
Armrests and STS
Armrests were generally seen as positive by the experts and staff, particularly in relation to the stability of the chair and the ability to complete successful STS transitions. Armrests were considered essential for STS transitions, and STS transitions were identified as vital for maintaining independence. The preferred method was for older adults to be able to achieve STS on their own without being given prompts or assistance:
Sit-to-stand transfer is often rated higher by organisations getting that chair, and for the person, because it allows them to independently transfer – get out of the chair when they want… so that autonomy, which is often lost in aged care. (OT)
Some residents with a more limited mobility may have difficulty getting out of a chair which is why the ones we’ve got with the arms seem to be a lot easier… for them to push down and push themselves up out of the chair. (Staff 5)
‘You would prefer residents to use the arms?’ ‘Most definitely… because it’s easier for them to get a standing transfer and be in a more supported position’. (OT)
…there’s a lot of support with them. Especially with the arms and with the height, allowing residents to maintain that independence. So if they have a wheelie walker in front of them, they have that advantage of being able to get up themselves. (Staff 3)
The experts and staff were able to offer detailed descriptions on both positive and negative aspects of armrests, particularly related to height and width:
…it’s no good having an armrest that’s this wide [gesturing to suggest armrests that are wider than the hands], that the residents can’t [get their hands around], you want something that they can actually grip quite easily. (Staff 1)
…armrests are not great for the shoulder joints sometimes, they bring your shoulders up if they’re too high…. (OT)
Cushion density, although vital for comfort, also had an impact on effective STS transitions, and stability was also a factor for STS:
If you have it too soft then they sink into it and they find it hard to get out of it. If it’s too hard they end up with a sore bottom. (Staff 4)
…the squishability of the chair… if it’s a very squishy chair then it might provide some added comfort for some individuals but then its extra hard to get out of…. (OT)
So how stable is that chair when they go to sit down on it? Does the chair balance? Is it safe for them to be rough with their sitting? (OT)
…they’ve got to be sturdy because people don’t gently sit down. (Staff 2)
Seat height
Seat height was discussed by experts and carers both in terms of independence and STS transitions, but also in relation to reducing risk for staff during manual handling:
The benefit with a higher chair is that it is easier to transfer, it’s easier to do that sit-to-stand… It’s also good for the carers. They like high chairs because it’s not hurting their backs, and back care is one of those big issues with aged care. (OT)
We’ve got to make sure the chair is not too low for the staff to get them up to standing…. (Staff 2)
Chairs that were too low were considered to have a negative impact on STS transitions and also were not suitable for those with hip fractures or replacements:
If you can vary the seat height that would be optimal… any chair that had variable height ability by changing the leg length would be great. (Physio)
too low… especially lounge chairs…When you sit in a lounge chair, because the cushion is comfortable and collapses you go down below that position and so your hips get below your knees. That creates a change in mechanical advantage… needed to get you up. (Physio)
…this chair is too low… especially in the case of fractured hips… then you need over 90 degrees angle at the hip. (OT)
Seat height was also referenced in terms of maintaining the aesthetic of the Club facility. As detailed in the chair audit (Table 2), there was very little variability in seat height overall, and no variation in size within each particular chair type. This consistency seems linked to the ‘club facility’ image, where uniformity in aesthetics was a priority:
We’re a club site so, having uniform chairs, this sort of height… so as you can see, same height same structure the whole way round. (Staff 3)
Seat depth
Although seat depth was not mentioned as frequently by managers and nursing staff as it was by residents, it did feature in interviews with the physiotherapist and occupational therapist, particularly in relation to poor and painful seating positions (Figure 16):
So the depth of the seat is too long for my legs [feet do not touch the floor]… so what’s going to naturally happen if I’m an older person who doesn’t have good postural support, has weakened limbs. They’re just going to gradually tuck under and slide out, looking for a base of support on their feet… the issue with this is not only a falls safety concern, but also of pressure, sheer forces, on their bottom. (OT)
Figure 16.
Occupational therapist demonstrating the impact of a seat that is both too high and too deep.
Discussion
In summary, none of the chairs audited (Tables 1-3) would fit ‘Jean’ – all were too high and too deep. Residents, experts and staff all preferred higher seats to allow for effective STS transfers. Seat height has been identified as the most important factor for easy STS,6 and the literature suggests that older people find it easier to rise from higher seats because the body has to travel a shorter distance, with less effort, to stand.5 A variety of seat heights was observed from 410 to 505 mm in facilities and 423–510 mm in the website audit. Almost all chairs were well over the mean popliteal height for older people (416 mm in males and 379 mm in females); most were above recommended heights for older people and far above ‘Jean’s’ popliteal height of 330 mm. Even so, many residents and staff stated that they would prefer even higher seats, revealing their preoccupation with STS over comfort. These higher chairs may be ideal for STS transfers but not necessarily for comfort, and observations showed that many residents could not touch the floor easily once they were seated. The problem of high seats can also be alleviated with footrests, which are recommended for older people5,6 but in the real world, they are used very little due to perceived risks. Additionally, none of the experts or carers was aware of any specific dimensions regarding appropriate seating for aged care and relied on manufacturers to use appropriate guidelines.
The mean buttock popliteal length for an older Australian female is 440 mm; the Australian Standard recommendation for seat depth for fixed height chairs is 440 mm, but observed seat depths for lounge chairs in our study ranged from 480 to 530 mm in facilities and 470–500 mm in the website audit. This may be because a chair which is over-high but not proportionately deep could look unbalanced and unwelcoming, even though it would probably be more ideal for the residents, so may be less likely to be chosen by facilities and offered by manufacturers. Thus, the combination of the justified and desired excess seat height and unnecessarily generous seat depth can be problematic during sitting if residents are unable to touch the floor. Reducing seat depth on some of the chairs offered would reduce problems of residents having to slump in order to touch the floor, reduce reliance on pillows and increase comfort, while still allowing for easier STS transfers. It should also assist with easier egress from the chair as shuffling forward would not be necessary. This could involve making chairs adjustable or providing a range of seat heights and depths in all spaces.
In the high- and mid-end facilities, the need to maintain a uniform appearance was prioritised over the fit of the chairs to a variety of individuals. Where possible, providing seating with a variety of heights is recommended.5,9 However, the need for a uniform appearance in high- and even mid-range facilities meant that all chairs of the same style had the same finish, fabrics and size, suiting the ‘look’ but not all residents.
The disparity between seat height required for STS and seat height required for comfort while seated, coupled with unnecessary seat depth, becomes an equity issue, whereby shorter residents are being disadvantaged compared with taller ones, suffering discomfort and possible musculoskeletal damage while sitting and being put at risk of deep venous thrombosis (DVT) due to the seating design. In Australia, women comprise 69% of people in permanent aged care20 and of course they are most likely to be the shorter residents. This means that a substantial percentage of the residents in aged care are using chairs which are likely to be uncomfortable and potentially even dangerous for them and are missing out on the benefits that could be gained from good seating discussed earlier (e.g. reduced pain, fatigue, VT risk and pressure sores, increased social interaction, improved respiratory function and intake of food and drink3,4).
Armrests were identified as vital by all participants, were always used for STS when available and were also essential for the feeling of confidence and autonomy from knowing that a transfer could potentially be achieved. Ideally, armrests should be lower at the back than the front; however, only the casual dining chairs were observed to have an angled armrest. Furthermore, with an average of 645 mm across all of the chairs, all of the armrest heights measured were lower than the 730 mm from the floor recommended by Holden and Fernie.18 Holden and Fernie18 also recommended an ideal armrest width of 120 mm. However, participants (residents and experts/carers) mentioned that a slimmer armrest was easier for residents to grip during STS transitions, so chairs which flout Holden and Fernie’s recommendation on armrest width may actually be better suited to this age group.
There was a focus by all experts and carers on fostering and encouraging residents’ remaining abilities and independence. Chairs can help to do this if residents are able to manage STS transitions without assistance; if they are able to reach their walking aid so they can get out of a chair and move away from it as and when they wish; and if they are comfortable enough in the chair that they can sit in it as long as they desire for the activity they are undertaking. The right balance needs to be achieved between assistance from the chair, other aids or other people and the residents’ various abilities, as well as between STS transfer and comfort.
Some measures that could be taken by furniture manufacturers in order to find this balance include developing chairs which easily and simply increase in height for STS transition but lower for prolonged sitting (not fully automated recliners as these already exist but are very costly and bulky and do not encourage users to make the most of their remaining abilities) and reducing seat depth on almost all chairs for aged care contexts. Meanwhile, aged care facilities could help by allowing footrests to be used in facilities, allowing residents to bring cushions and pillows from their rooms into communal areas in order to customise the seating and providing a better variety of seat heights in each of the various contexts within facilities.
Limitations
This study used a convenience sample to investigate a variety of aged care seating with residents, staff and experts based around Brisbane, Australia. Australia is a multi-cultural society but even so this does not make this sample representative of all aged care residents and staff in terms of anthropometrics, abilities or attitudes. In addition, the seating audited was limited to that available in Australia and is not necessarily representative of aged care seating available elsewhere in the world.
The study was qualitative and collected subjective opinions of participants. It did not include objective measures of strain, pressure or movement but aimed more at discovering subjective perceptions about what was working and not working for aged care residents on a day-to-day basis. Studies employing more objective measures may be required to evaluate particular seating solutions developed based on our recommendations. However, by focusing on subjective perceptions of comfort and observing actual STS and sitting activity within the aged care environment, this study has begun an important conversation about the specific seating needs of older people within the residential aged care context.
Conclusion
In this article, we have discussed the extant literature about seating in aged care and the recommended anthropometric and design guidelines relevant for aged care seating. Furthermore, we have described an investigation of current seating furniture available online and in use in aged care facilities in Queensland (Australia). Taking the importance of STS transfers into account, suitability of most chair dimensions (including excess height) was justifiable apart from seat depth in many cases. As a result of increased seat height for STS purposes and unnecessary excess depth of seat pans, chairs were too high and/or deep for many residents to sit comfortably. There was almost no use of footrests to offset these issues and very little variety in seat heights throughout facilities. This research suggests that a balance needs to be found between ease of egress, independence and comfort for all residents regardless of their size. This disconnection between comfort, STS and function is an area in need of further attention in seating design for the aged care context.
Appendix 1
Interview questions residents
What would be your ideal lounge chair?
- Are you happy with the height of the chairs you use?
- a. When you are sitting;
- b. When you are getting up and down.
- 3. Do you use footrests?
- a. If so, what do you think of them?
- b. Which type do you prefer and why?
4. Which parts of the lounge chair do you find most/least comfortable?
- 5. Are you happy with the comfort of the chairs, when you are sitting for a long time?
- a. If not, why?
- 6. Do you have a favourite and least favourite chair?
- a. Please show us and explain why.
7. Do you prefer a firm or soft lounge chair?
8. If you fall asleep in the chair, does that cause pain or discomfort?
9. What would be the most number of hours you spend sitting in the same chair?
10. What makes you feel stable when sitting down into a chair?
11. What makes you feel unstable when sitting down into a chair?
12. What are the key grab points or hand supports you look for when sitting in a chair?
13. If your chair could recline how far back would you prefer it to go?
14. If you could adjust the pressure in any part of the chair – seat, lumber, neck support – which would you think most critical?
15. What kinds of things do you do while sitting in lounge chairs, that is, activities such as reading, knitting, watching telly, playing games?
16. Do you have any comments about other types of chairs?
Appendix 2
Interview questions experts
From your experience, could you describe or show us some of the chairs most frequently used by older people at your workplace?
In your opinion, are there any clear positive or negative aspects about these most frequently used chairs?
What issues do you face in moving residents in and out of these frequently used chairs?
How does the design of the frequently used chairs impact your work?
What would be your ideal lounge chair for aged care?
- Are you happy with the height of the chairs?
- a. When residents are sitting;
- b. When they are getting up and down (STS transfer).
- 7. Do you use footrests?
- a. If so, what do you think of them?
- b. Which type do you prefer and why?
8. Which parts of the chair do you think residents find most/least comfortable?
- 9. Are you happy with the comfort of the chairs, when residents are sitting for a long time?
- a. If not, why not?
10. If residents fall asleep in the chair, does that cause pain or discomfort?
11. Do you use or see any need for additional neck support?
12. What would be the most number of hours residents spend sitting in the same chair?
- 13. Is there a specific chair per resident?
- a. Is it then adapted for them?
- b. If so how?
14. Do you have any comments about lounge chairs or other types of chairs?
Appendix 3
Interview questions carers
From your experience, could you describe or show us some of the chairs most frequently used by older people?
In your opinion, are there any clear positive or negative aspects about these frequently used chairs?
What issues do you face while using these frequently used chairs to care for residents?
What issues do the people you care for experience while using these frequently used chairs?
How does the design of the frequently used chairs impact your work?
What would be your ideal lounge chair for aged care?
- Are you happy with the height of the chairs:
- a. When residents are sitting;
- b. When they are getting up and down (STS transfer)?
- 8. Do you use footrests?
- a. If so, what do you think of them?
- b. Which type do you prefer and why?
9. Which parts of the chair do you think residents find most/least comfortable?
- 10. Are you happy with the comfort of the chairs, when residents are sitting for a long time?
- a. If not, why not?
11. If residents fall asleep in the chair, does that cause pain or discomfort?
12. Do you use or see any need for additional neck support?
13. What would be the most number of hours residents spend sitting in the same chair?
- 14. Is there a specific chair per resident?
- a. Is it then adapted for them? If so how?
15. What types of activities do you perform for residents while they are in the chairs – for example, serving refreshments, applying or checking dressings and moving around?
16. What kinds of things do residents do while sitting in lounge chairs – that is, activities such as reading, knitting, watching telly, playing games?
17. Do you have any comments about lounge chairs or other types of chairs – for example, dining chairs?
Appendix 4
Full coding scheme.
| Behaviour | Behaviour |
|---|---|
| OBSERVED | DISCUSSED |
| Bed - Lying Down | Activity |
| Bed - Sitting | Care |
| Leaning | Chair |
| Pushing Up | Environment |
| Reaching | Feature |
| Reposition | Time |
| Sit Down | |
| Sitting | |
| Stand Up | |
| Standing |
| Modifier | Modifier | Modifier |
|---|---|---|
| Type of Chair | Body positions | USING |
| 2/3 seater couches | back | footrest |
| bench seat | feet not flat on floor | handle |
| cafe chair | knee(s) | hoist |
| dining chair | legs | nothing |
| facility chair/ supplied/ communal | looking for something to push on/hold/grip | person/staff help |
| high back lounge | multiple attempts | pillow/ cushion |
| lift-chair | neck | pressure cushion |
| occasional/ day | not holding/ pushing anything | railing |
| office chair | one arm | table |
| own chair/ personal/ private | one hand at a time | towel |
| recliner | perched | walker |
| toilet | posterior tilt- pelvic tuck - | walking stick |
| wheel chair | pushing | |
| wing chair | put feet up _ in recliner | |
| reclined |
| Modifier | Modifier |
|---|---|
| Features - Chair or Room | Impact and Considerations |
| convenient position | activities of daily living |
| controls/ button for recliner | assessed by physio |
| comfort | cognition - cognitive decline |
| cluttered | home- like |
| cushion density | independence |
| dirty - easy to clean - stain resistant - infection control | maintaining/ improving |
| chair against wall | mental health |
| adjustable | mobility |
| back support/back rest | model of care |
| armrests | negative |
| easily moved | not used |
| fabric/ material | physical health |
| familiarity - used to it | positive |
| grip - armrest | pressure |
| head rest | quality of life |
| lifespan – longevity- durability | risk - to individual or staff |
| modified - customised - personalised | skin conditions/ abrasions |
| multi-functional | sliding forward/ sliding out of chair |
| no armrests | technique |
| removable | used regularly/ frequently |
| safety | |
| seat | |
| seat depth | |
| seat height | |
| seat width | |
| softness | |
| space behind knee | |
| stable/ strong | |
| too big | |
| too low | |
| too small | |
| uncomfortable | |
| variety | |
| water resistant |
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from QUT University Ethics Committee Approval number 1500000968.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by a commercial client (Lifecare Furniture Pty Ltd) who commissioned this research from the university and has given full permission for publication of this material.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iD: Alethea Blackler  https://orcid.org/0000-0002-9406-2645
https://orcid.org/0000-0002-9406-2645
Marianella Chamorro-Koc  https://orcid.org/0000-0001-7982-1626
https://orcid.org/0000-0001-7982-1626
References
- 1. AS/NZS 4688.1:2000. Furniture-fixed height chairs – part 1: ergonomic and general requirements (Standards Australia/Standards New Zealand). [Google Scholar]
- 2. O’Reilly M, Courtney M, Edwards H, et al. Clinical outcomes in residential care: setting benchmarks for quality. Australas J Ageing 2011; 30: 63–69. [DOI] [PubMed] [Google Scholar]
- 3. Thirugnanachandran T, Bateson A. Seating for improving function in older people. Eur Geriatr Med 2012; 3: 67–72. [Google Scholar]
- 4. Nitz JC. The seating dilemma in aged care. Aust J Physiother 2000; 46: 53–58. [DOI] [PubMed] [Google Scholar]
- 5. Holden J, Fernie G, Lunau K. Chairs for the elderly – design considerations. Appl Ergon 1988; 19: 281–288. [DOI] [PubMed] [Google Scholar]
- 6. Disabled Living Foundation, 2005, http://www.dlf.org.uk/factsheets/chairs.
- 7.Center of Design for an Aging Society. Ease of access: solutions for seating, n.d., http://www.centerofdesign.org/pages/easeaccessability.htm
- 8. Rodosky MW, Andriacchi TP, Andersson GB. The influence of chair height on lower limb mechanics during rising. J Orthop Res 1989; 7: 266–271. [DOI] [PubMed] [Google Scholar]
- 9. Alexander NB, Koester DJ, Grunawalt JA. Chair design affects how older adults rise from a chair. J Am Geriatr Soc 1996; 44: 356–362. [DOI] [PubMed] [Google Scholar]
- 10. Dolecka UE, Ownsworth T, Kuys SS. Comparison of sit-to-stand strategies used by older adults and people living with dementia. Arch Gerontol Geriat 2015; 60: 528–534. [DOI] [PubMed] [Google Scholar]
- 11. Hughes Myers BS, Schenkman ML. The role of strength in rising from a chair in the functionally impaired elderly. J Biomech 1996; 29: 1509–1513. [PubMed] [Google Scholar]
- 12. Scarborough DM, McGibbon CA, Krebs DE. Chair rise strategies in older adults with functional limitations. J Rehabil Res Dev 2007; 44: 33. [DOI] [PubMed] [Google Scholar]
- 13. Hughes Weiner D, Schenkman M, Long R, et al. Chair rise strategies in the elderly. Clin Biomech 1994; 9: 187–192. [DOI] [PubMed] [Google Scholar]
- 14. Alexander NB, Gross MM, Medell JL, et al. Effects of functional ability and training on chair-rise biomechanics in older adults. J Gerontol A: Biol 2001; 56: M538–M547. [DOI] [PubMed] [Google Scholar]
- 15. Christenson MA. Chair design and selection for older adults. Phys Occup Ther Geriatr 1990; 8: 67–85. [Google Scholar]
- 16. Kothiyal K, Tettey S. Anthropometry for Design for the Elderly. Int J Occup Saf Ergo 2001; 7: 15–34. [DOI] [PubMed] [Google Scholar]
- 17. National Occupational Health Safety Commission. Ergonomic Principles and Checklists for the Selection of Office Furniture and Equipment, 1991, https://www.safeworkaustralia.gov.au/doc/ergonomic-principles-and-checklists-selection-office-furniture
- 18. Holden J, Fernie G. Specifications for a mass producible static lounge chair for the elderly. Appl Ergo 1989; 20: 39–45. [DOI] [PubMed] [Google Scholar]
- 19. Finlay O, Bayles T, Rosen C, et al. Effects of chair design, age and cognitive status on mobility. Age Ageing 1983; 12: 329–335. [DOI] [PubMed] [Google Scholar]
- 20. Australian Institute of Health Welfare, 2017, Older Australia at a Glance, https://www.aihw.gov.au/reports/older-people/older-australia-at-a-glance/contents/health-and-aged-care-service-use/aged-care
- 21. Noldus. Noldus the observer XT, 2017, http://www.noldus.com/human-behavior-research/products/the-observer-xt
- 22. Blackler A, Popovic V, Lawry S, et al. Researching Intuitive Interaction. In: Roozenburg NFM, Chen LL, Stappers PJ. (eds) IASDR2011, the 4th world conference on design research Delft: TU Delft, 2011 [Google Scholar]
- 23. Buy Direct Online com.au, 2017, https://buydirectonline.com.au/commercial-equipment/healthcare-equipment/aged-care-chairs
- 24. Regency Health Care, 2017, http://www.regencyhealthcare.com.au/shop/products/
- 25. Aidacare, 2017, https://www.aidacare.com.au/aidacare/products/chairs—therapeutic/couches-facility-chairs/
- 26. Healthcraft Furniture, 2017, https://healthcraft.com.au/.