Abstract
Background:
Traditional total knee implants designs, usually, are not able to reproduce the physiological kinematics of the knee, leaving almost 20% of the patients, those who underwent a total knee arthroplasty (TKA), not fully satisfied. Modern inserts are nowadays designed with a fully congruent medial compartment to reproduce the normal medial pivoting biomechanics of the knee. The aim of this article was to evaluate preliminary clinical improvement using the Medial Congruent (MC) insert as specific level of constraint.
Materials and methods:
A total of 10 consecutive patients have been enrolled in this study and treated using an MC tibial polyethylene insert. The Oxford Knee Score (OKS) and the Knee Society Score (KSS) have been assessed preoperatively and at 3-month, 6-month, and 1-year follow-up (FU) and used as validated measurements to evaluate early clinical improvements. Postoperative radiological examination was reviewed looking for radiolucent lines or loosening of the components.
Results:
Average improvement in OKS was from 19.5 to 41.2, whereas KSS improved with an average score from 64.7 preoperatively to 167.5 at the final FU showing good to excellent results in 95% of the treated knees. Evaluating the range of motion, the average maximum active movement was 124° and none of the patients needing for a revision surgery or manipulation under anesthesia. No complications were observed at the final FU as septic or aseptic loosening or vascular or neurologic injury.
Discussion and conclusions:
Medial Congruent insert showed good to excellent clinical results at 1-year FU. Range of motion and subjective outcomes were satisfying and comparable with results obtained in literature using traditional TKA design.
Keywords: medial pivot insert, Medial Congruent insert, total knee arthroplasty
Introduction
Total knee arthroplasty (TKA) is one of the most effective surgical interventions for pain relief and functional recovery in patients with advanced degenerative arthritis of the knee.1 In 2016, osteoarthritis was the original diagnosis for 87% of knee arthroplasties in the United States with approximately 50% of surgeons preferring posterior-stabilized (PS) implants, which continue to be the most common design used in primary knee arthroplasty. Cruciate retaining (CR) is the second design commonly used, making up nearly 42% of the total procedures.2
Unfortunately, the rate of satisfaction after TKA is reported around 80%, leaving almost 20% of the patients not fully satisfied,3 especially, young patients demanding for high recreational activities such as cycling or trekking after surgery.4
Many patients complain a loss of stability, sometimes referred as an abnormal feeling knee joint, decreased functional outcomes, reduced range of knee motion, and greater difficulty performing daily activities, compared with their age-matched peers.5
An important factor, responsible for these symptoms, is probably an alteration of the normal knee kinematics with an abnormal anterior sliding of the femoral component on the tibial plateau. This characteristic is showed using most of the common traditional TKA designs and is known as “paradoxical motion” in the literature.6
This “paradoxical motion” is more evident using CR design, where during the early flexion of the knee, the weight of the body pushes the femur forward along the tibia until it is stopped by the posterior cruciate ligament (PCL). This concept, called as “mid-flexion instability,” has been accurately described by Vince7 and defined as a condition that exists where a TKA was stable in extension and at 90° of flexion but was unstable between the 2 positions. This phenomenon is also observed using PS implants.8
Several studies adopting fluoroscopically evaluations9 showed a different kinematics of the normal knee. Normally, during the flexion, a posterior sliding of the lateral femoral condyle on the tibial plateau is observed while a pivoting movement is reported on the medial compartment with a quite stable contact point between medial femoral condyle and medial tibial plateau.
These different patterns, associated with a different anatomy (a concave shape on the medial plateau and a convex shape for the lateral) and different loads between the 2 compartments (60% of body weight is transferred through the medial side of the knee), ligaments and tendon, that create a knee that is more stable on the medial side than the lateral, led to the concept of medial pivot kinematics.
A physiological medial pivot pattern on the normal knee is also confirmed by Johal et al10 investigating the kinematics of the knee using open magnetic resonance imaging.
Several modern TKA implants are nowadays designed trying to reproduce the normal kinematics of the knee miming the physiological “medial pivoting” pattern with a greater conformity on the medial compartment between tibial insert and femoral condyle and a less congruency on the lateral side.
A greater medial conformity is provided by a concave surface on the medial compartment of the tibial insert with an anterior lip that stabilizes the knee from full extension through deep flexion confining the anterior sliding with a greater anterior constraint and a subluxation resistance.
In contrast, the lateral condyle is designed to move more freely along an arcuate path. The PCL retention option may further enhance the patient experience providing a proprioceptive feedback and restoring patient confidence during daily activities.
In this way, the femoral implant does not roll back as in PS arthroplasty with post and cam mechanism,11 and quadriceps force is improved especially in early extension.12 Medial pivot implants demonstrate a superior prognosis compared with a PS implant.13
Schmidt et al8 confirmed a clinical improvement using medial pivot implant concluding as patients with different bilateral TKAs feel the medial pivot implant as more stable and more normal, also for highly demanding tasks as rising from a chair without compensation from nonoperated limb: they prefer the medial pivot rather than mobile-bearing, CR, or PS prostheses.
The objective of this prospective study is to evaluate clinical improvement and radiological outcomes of patients at minimum 1-year follow-up (FU) treated for an advanced knee osteoarthritis, undergoing primary TKA, using a Persona (Zimmer Biomet, Warsaw, IN, USA) knee implant with a Medial Congruent (MC) polyethylene insert.
This TKA system is designed with 2 femoral designs (PS and CR) and an anatomical tibial plateau allowing to use 4 different polyethylene inserts: PS, CR, ultracongruent, and MC. The MC insert is fully congruent (1:1 radius) with the medial femoral condyle, and it has been recently designed to reproduce the normal medial pivot kinematics of the knee and it is available at the author institution from April 2016.
Materials and Methods
A total of 10 consecutive patients (7 women and 3 men) scheduled for a total knee replacement (TKR) have been enrolled in this study and treated using a Persona knee implant with an MC tibial polyethylene; this total knee system is routinely used at the author institution to treat advanced knee osteoarthritis and routinely available. Implanting was performed at San Luigi Hospital of Orbassano (Turin, Italy) by the same surgeon from April 2016 to August 2016. The average age of the patients included was 70.5 (from 64 to 81) years with an average body mass index (BMI) of 29.7 (from a minimum of 22.5 to a maximum of 38.3).
A primary advanced knee osteoarthritis leading to a varus deformity or neutral alignment was diagnosed in all patients. Patients with the presence of valgus deformity, previous osteotomies, or previous serious traumatic surgical treatments around the knee were all excluded from the study; rheumatoid or other immunologic arthroplasties were also included in the exclusion criteria.
A standard anterior-posterior and lateral weight-bearing radiographs, a pangonogram of the lower extremities, and a Marchant14 view of patellofemoral joint were performed in all patients preoperatively and at 6-month and final FU.
Intraoperatively, with the patient in supine position and spinal anesthesia, the surgical approach is performed through a standard midline skin incision and a medial parapatellar capsulotomy. Standard bone cuts are made using an intramedullary guide for the femur and an extramedullary guide for the tibial cut checking at this point the extension gap with a 10-mm spacer block and laminar spreader.
Subsequently the femoral sizing guide, anterior reference, was oriented following the surgical transepicondylar axis and trying to avoid an excessive external rotation of the femoral component to prevent, as well is possible, a mid-flexion instability for a laxity of the medial compartment in flexion. Normally, 3° of external rotation is used for the varus knee. The PCL is resected in all cases.
Once the tibial and femoral cuts are completed and all osteophytes are removed, the flexion gap is assessed using laminar spreaders and standard spacer block to obtain a symmetrical and rectangular gap both in flexion and in extension: the current authors prefer to obtain a slightly greater opening on the lateral compartment (no more than 2 mm) during the varus/valgus stress knee maneuver to customize the soft tissue surgical technique according to the design of the medial pivot implant.15
At this point, the femoral component is fitted according to the femoral cuts, the anatomical tibial plateau is oriented following the medial third of the tibial tubercle,16 and the MC insert trial is used evaluating the stability of the knee during the all range of motion (ROM) with the patella relocating on the femoral groove. When a wide ROM with a stable knee is restored, the final tibial insert is introduced. Patella was replaced in all cases (Figure 1).
Figure 1.
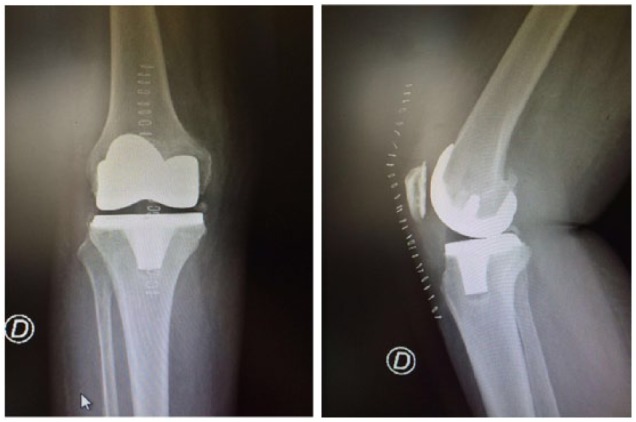
Postoperative X-ray of a 68-year-old female patient: antero-posterior and lateral view.
All patients followed an identical standard postoperative rehabilitation protocol including weight bearing as tolerated with crutches on postoperative day 1, and clinical improvements have been assessed preoperatively and at 3-month, 6-month, and 1-year FU using the Oxford Knee Score (OKS)17 and the Knee Society Score (KSS)18 as patient-reported outcomes measurement system. A radiological evaluation was made by a single physician at 6-month and 1-year FU to detect eventual lines of radiolucency and loosening of the femoral and tibial components.
Results
All patients were available for clinical and radiological evaluation at 1-year minimum FU.
Average improvement in OKS was from 19.5 preoperatively to 41.2 at the final FU, whereas KSS improved with an average score from 64.7 preoperatively to 167.5 showing good to excellent result in 95% of the treated knees. Evaluating the maximum ROM at the final FU, the average maximum active movement was 124° and none of the patients needing for a revision surgery or manipulation under anesthesia. No complications were observed at the final FU as septic or aseptic loosening or vascular or neurological injury.
Postoperative X-ray showing an average femoro-tibial anatomical axis with 4° of valgus (ranging from 7° to 3°) and no radiolucent lines was found in antero-posterior and lateral view; none of the components was found to be radiologically loose. The patellofemoral view showed a correct position of the patellar articular surface on the femoral groove.
Discussion and Conclusions
Medial pivot implants are theoretically designed to better reproduce the physiological kinematics of the normal knee, confining the anterior sliding movement and avoiding the paradoxical anterior roll back of the femoral condyles in TKA. The normal tibial plateau anatomy19 is replicated designing an insert with a deep medial compartment highly congruent and a lateral compartment characterized by less conformity. A “ball-in-socket articulation” with a stable and point is obtained on the medial compartment, whereas a rolling from anterior to posterior occurs in the lateral condyle during the knee motion reproducing a physiological knee biomechanic.20
An interesting analysis has been conducted by Dennis et al21 involving 33 different designs of TKA with the object to evaluate implants variables that affect knee kinematics: the authors observed a medial pivot pattern in 50.6% of the patients with TKA during the gait and in 58% of the patients with TKA during the deep knee bend maneuver, concluding that usually sagittal plan translation patterns after TKA do not duplicate those of the normal knee.
Few studies considering the medial pivot kinematics during the knee motion after TKA are present in literature and unfortunately are already unclear whether these kinematic patterns are related to clinical improvements.
In 2014, Nishio et al,22 using a computed tomography–based navigation system, evaluated the relationship between clinical results, including patient-reported outcomes, and intraoperative knee kinematic patterns after TKA, concluding that functional activities, patient satisfaction, and the knee flexion angle were significantly better in TKA showing intraoperative medial pivot patterns when compared with those of the nonmedial pivot group.
Recently, Warth et al23 published an article with different results. It was also aimed to determine whether intraoperative medial pivot kinematic patterns are associated with improved patient outcomes; however, at minimum 1-year FU, Knee Society objective, satisfaction, function, walking pain, stair pain, and the University of California Los Angeles (UCLA) activity level did not differ based on medial vs nonmedial pivot patterns.
Similar results are showed by Menighini et al24 assessing 152 TKA at minimum 1-year FU (average 20.4 months) and using a sensor-guided technology to detect an intraoperative medial pivot kinematic. Controlling for BMI, new Knee Society Scoring System, UCLA activity level score, and pain scores, at latest FU, did not differ in medial knees (40% of the final simple size) and nonmedial pivot, suggesting that a medial pivot kinematic pattern may not be a substantial governor of clinical success.
A number of TKA implants are designed to guide a medial pivot kinematic knee: this new concept of design influences more third-generation prosthesis rather than older implants; consequently, there are not many information about clinical and radiological outcomes at long-term FU.
The ADVANCE Medial-Pivot Knee (AMP) System (MicroPort Orthopedics Inc., Arlington, TN, USA) is one of the older implants (second-generation TKA) designed to replicate normal tibiofemoral joint kinematics. It was introduced in 1998 by Wright Medical Technology, and recently, Macheras et al25 reported results of clinical outcomes with an average FU of 15.2 years. Evaluating 347 knees, which underwent a TKA system using the AMP device, most of the patients (94%) were able to perform age-appropriate activities with a mean knee flexion of 120° (range: 105°-135°) at final FU. Survival analysis showed a cumulative success rate of 98.8% at 17 years.
Recently, Scott et al26 studied the movement patterns of the knee using a modern third-generation TKA designed to reproduce the medial pivot kinematic. The GMK Sphere (Medacta International AG, Castel San Pietro, Switzerland) has been used on 16 knees and evaluated using pulse fluoroscopy during a number of weight-bearing and non–weight-bearing static and dynamic activities. The authors concluded that little or no translation of the medial femoral condyle was observed during flexion, but there was posterior roll back of the lateral femoral condyle, equating to tibiofemoral rotation as showing in the normal knee.
Similar conclusions are reported by Shimmin et al27 in 2015 using a fixed-bearing TKR prosthesis based on a Medial Rotation Knee (MRK) concept. The SAIPH Knee System (MatOrtho; Surrey, UK) is a second-generation medial ball-and-socket knee used in this study. The authors showed, at a fluoroscopic evaluation, a posterior translation of the lateral femoral condyle during knee flexion, with internal rotation of the tibia, and no paradoxical anterior motion in any of the weight-bearing activities analyzed.
As previously reported in the literature, there is no consensus about the relationship between medial pivot kinematic pattern and clinical improvement after TKA; certainly, the prosthetic models have changed extraordinarily in the past decades and several changes have been done also on the insert design looking for a device able to ensure a higher stability with the minimum level of constraint. This study reports our first experience using a third-generation prosthesis system with an MC polyethylene insert recently designed. Good to excellent results using a novel medial pivot design are supported evaluating subjective patient satisfaction in addition to objective clinical and radiological outcomes. To the authors’ knowledge, no further reports are present in literature on the MC Persona polyethylene and no articles are present in literature reporting long-term results about this new device. In this article, excellent clinical and kinematical performance evaluating the active ROM after medial pivot knee arthroplasty has been showed, but a number of limitations are present. First, this is a prospective study enrolling a limited number of patients; second, the FU is short and limited to 1 year. More cases and a long-term FU might be necessary to confirm the value of this new design and eventual clinical improvements. Third, our preliminary clinical result should be confirmed with more objective methods: measurements using fluoroscopic evaluations or a gait analysis study might be more appropriate to better support our preliminary clinical results.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All Authors contributed in preparing the article.
References
- 1. Choi YJ, Ra HJ. Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res. 2016;28:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vaishya R, Agarwal AK, Vijay V. Extensor mechanism disruption after total knee arthroplasty: a case series and review of literature. Cureus. 2016;8:e479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tolk JJ, Van der Steen MC, Janssen RPA, Reijman M. Total knee arthroplasty: what to expect? a survey of the members of the Dutch knee society on long-term recovery after total knee arthroplasty. J Knee Surg. 2017;30:612–616. [DOI] [PubMed] [Google Scholar]
- 4. Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;431:157–165. [DOI] [PubMed] [Google Scholar]
- 5. Varadarajan KM, Zumbrunn T, Rubash HE, Malchau H, Li G, Muratoglu OK. Cruciate retaining implant with biomimetic articular surface to reproduce activity dependent kinematics of the normal knee. J Arthroplasty. 2015;30:2149–2153. [DOI] [PubMed] [Google Scholar]
- 6. Komistek R. In vivo fluoroscopic analyses of the normal human knee. Clin Orthop Relat Res. 2003;410:69–81. [DOI] [PubMed] [Google Scholar]
- 7. Vince K. Mid-flexion instability after total knee arthroplasty: woolly thinking or a real concern? Bone Joint J. 2016;98-B:84–88. [DOI] [PubMed] [Google Scholar]
- 8. Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ. Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res. 2003;410:139–147. [DOI] [PubMed] [Google Scholar]
- 9. Leszko F, Hovinga KR, Lerner AL, Komistek RD, Mahfouz MR. In vivo normal knee kinematics: is ethnicity or gender an influencing factor? Clin Orthop Relat Res. 2011;469:95–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johal P, Williams A, Wragg P, Hunt D, Gedroyc W. Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using “interventional” MRI. J Biomech. 2005;38:269–276. [DOI] [PubMed] [Google Scholar]
- 11. Freeman MA, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38:197–208. [DOI] [PubMed] [Google Scholar]
- 12. Pritchett JW. Patients prefer a bicruciate-retaining or the medial pivot total knee prosthesis. J Arthroplasty. 2011;26:224–228. [DOI] [PubMed] [Google Scholar]
- 13. Hossain F, Patel S, Rhee SJ, et al. Knee arthroplasty with a medially conforming ball-and-socket tibiofemoral articulation provides better function. Clin Orthop Relat Res. 2011;469:55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 15. Risitano S, Indelli PF. Is “symmetric” gap balancing still the gold standard in primary total knee arthroplasty? Ann Transl Med. 2017;5:325. doi: 10.21037/atm.2017.06.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Indelli PF, Graceffa A, Payne B, Baldini A, Pipino G, Marcucci M. Relationship between tibial baseplate design and rotational alignment landmarks in primary total knee arthroplasty. Arthritis. 2015;2015:189294. doi: 10.1155/2015/189294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63–69. [DOI] [PubMed] [Google Scholar]
- 18. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 19. Blaha JD. A medial pivot geometry. Orthopaedics. 2002;25:963. [DOI] [PubMed] [Google Scholar]
- 20. Risitano S, Karamian B., Indelli PF. Intraoperative load-sensing drives the level of constraint in primary total knee arthroplasty: surgical technique and review of the literature. J Clin Orthop Trauma. 2017;8:265–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB. Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:37–57. [DOI] [PubMed] [Google Scholar]
- 22. Nishio Y, Onodera T, Kasahara Y, Takahashi D, Iwasaki N, Majima T. Intraoperative medial pivot affects deep knee flexion angle and patient-reported outcomes after total knee arthroplasty. J Arthroplasty. 2014;29:702–706. [DOI] [PubMed] [Google Scholar]
- 23. Warth LC, Ishmael MK, Deckard ER, Ziemba-Davis M, Meneghini RM. Do medial pivot kinematics correlate with patient-reported outcomes after total knee arthroplasty? J Arthroplasty. 2017;32:2411–2416. [DOI] [PubMed] [Google Scholar]
- 24. Meneghini M, Ishmael MK, Deckard E, Ziemba-Davis M, Warth LC. Are medial pivot kinematics with sensor-guided technology correlated with outcomes after total knee arthroplasty? Bone Joint J. 2017;99:82. [DOI] [PubMed] [Google Scholar]
- 25. Macheras GA, Galanakos SP, Lepetsos P, Anastasopoulos PP, Papadakis SA. A long term clinical outcome of the medial pivot knee arthroplasty system. Knee. 2017;24:447–453. [DOI] [PubMed] [Google Scholar]
- 26. Scott G, Imam MA, Eifert A, et al. Can a total knee arthroplasty be both rotationally unconstrained and anteroposteriorly stabilised? a pulsed fluoroscopic investigation. Bone Joint Res. 2016;5:80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shimmin A, Martinez-Martos S, Owens J, Iorgulescu AD, Banks S. Fluoroscopic motion study confirming the stability of a medial pivot design total knee arthroplasty. Knee. 2015;22:522–526. [DOI] [PubMed] [Google Scholar]


