Abstract
Background:
Colorectal cancer (CRC) is considered a disease of elderly. There has been a steady decrease in the incidence in those aged >50 years, with an alarming increase noted in adults aged <50 years.
Subjects and Methods:
We retrospectively analyzed 89 patients diagnosed with CRC aged <40 years between the years 2010 and 2014. Their clinical profile, treatment, and outcomes were studied.
Results:
The median age was 33 years with a male preponderance (56.2%). Most common symptoms were lower gastrointestinal bleed (48.3%) followed by abdominal pain (46.1%). Most common sites were rectum (50.6%) followed by colon. Histology in all was adenocarcinoma. Most tumors were moderately differentiated (54%) and were stage 4 (36%). Most common sites of metastases were liver (46.9%) followed by peritoneum and ovaries. Majority underwent surgery with adjuvant chemotherapy, with/without radiotherapy. Chemotherapy was administered in 70 patients, majority receiving FOLFOX-4 regimen (88.6%). Median survival was 23 months. Survival in early stage[1],[2] was significantly higher than in advanced stages (3 and above), 34 and 19 months (P = 0.0287), in those aged >40 years compared to <40–35 versus 23 months (P = 0.0029), nonmetastatic compared to metastatic disease – 26 versus 14 months (P = 0.00196), and females compared to males – 26 and 18 months (P = 0.0242). There was no significant difference in survival with respect to tumor grade or site of metastases (hepatic versus extrahepatic).
Conclusions:
Colorectal carcinoma in young seems to be an emerging problem in India. Any young patient presenting with symptoms suggestive of a colonic malignancy should be evaluated promptly and treated aggressively.
Keywords: Colorectal cancer, young patients, age <40
Introduction
Colorectal cancer (CRC) is the third most common cancer in the world and considered mainly as a disease of the elderly. Almost 60% of cases are encountered in developed countries. In India, colon cancer ranks 8th and rectal cancer ranks 9th among men. For women, rectal cancer does not figure in the top 10 cancers, whereas colon cancer ranks 9th.[1] An alarming proportion of adenocarcinoma has been noted in adults aged <50 years in various studies, including few Indian studies, compared to those aged >50 years.[2,3] We review the presentation, treatment, and outcomes of patients with carcinoma colon who were aged <40 years at presentation to our center.
Subjects and Methods
Tumor registry at our hospital was analyzed for cases of CRC. Of the 320 patients studied, those diagnosed with CRC aged <40 years between the years 2010 and 2014 were analyzed in this study. Their clinical details – age, sex, symptoms, grade of the tumor, staging, treatment obtained, and outcomes in terms of survival were noted and analyzed. Survival curves were generated by Kaplan–Meier method and analyzed using the log-rank test and Fisher's exact test.
Results
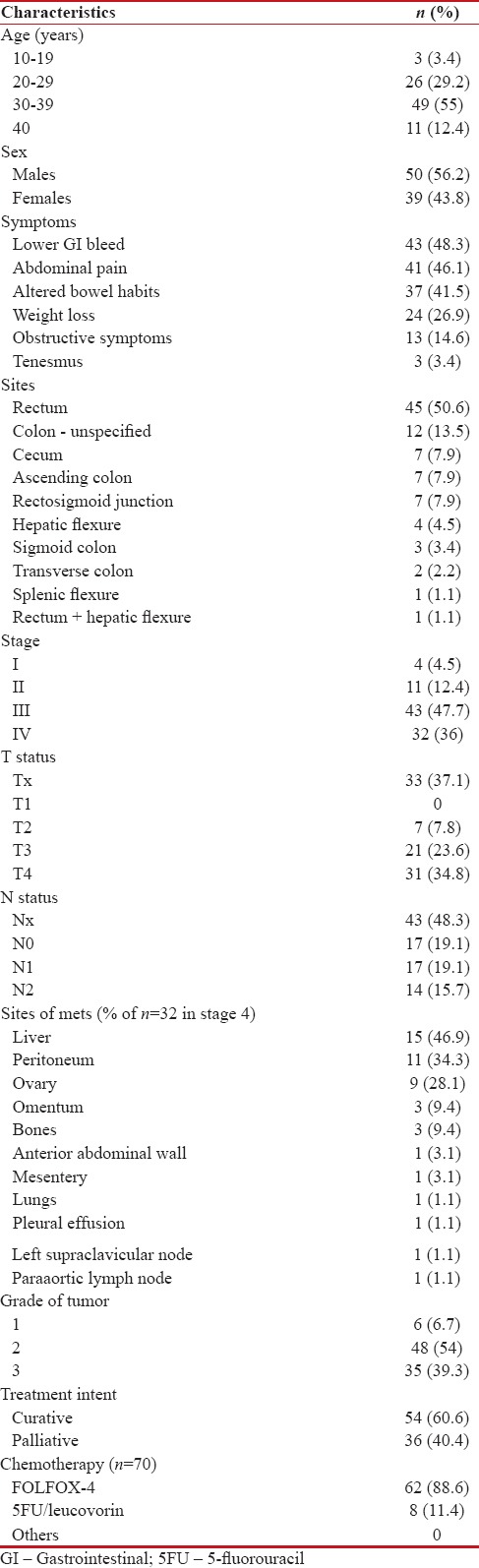
An total of 89 patients diagnosed with CRC and aged <40 years were analyzed. The results are as shown in Table 1. The median age of the study cohort was 33 years (12–40). Majority of the patients belonged to the age group of 30–39 years (n = 49; 55%). There was a male preponderance (56.2%) with the ratio of male to female being 50:39. The most common symptoms at presentation were lower gastrointestinal bleed (n = 43; 48.3%) followed by abdominal pain (n = 41; 46.1%). The other common presenting complaints were change in bowel habits (n = 37; 41.5%), weight loss (n = 24; 26.9%), obstructive symptoms (n = 13; 14.6%), and tenesmus (n = 3;3.4%). The most common sites of disease were the rectum (n = 45; 50.6%) followed by the following sites in the colon namely - unspecified site (n = 12; 13.5%), caecum (n = 7; 7.9%), ascending colon (n = 7; 7.9%), and the rectosigmoid junction (n = 7; 7.9%). There was only one case of a synchronous primary – involving both the rectum and hepatic flexure (each staged separately). The histology in all the cases was adenocarcinoma. Most tumors were either moderately (n = 48; 54%) or poorly differentiated (n = 35; 39.3%). Most tumors presented in higher stage, with stage 3/metastatic disease. The most common sites of metastases were liver (n = 15; 46.9%) followed by metastases in the peritoneum (n = 11; 34.3%) and ovaries (n = 9; 28.1%). The other sites with metastatic involvement were omentum, and uncommon sites were mesentery, anterior abdominal wall, bones, supraclavicular lymph nodes, lung, and pleura.
Table 1.
Clinical profile with treatment details (continued on the next page)
Treatment involved multimodality approaches such as surgery, radiotherapy, and chemotherapy [Table 2]. Surgery was done with either curative or palliative intent. Those that were curative (n = 50) included low anterior resection, abdominoperineal resection, and colectomy with regional lymphadenectomy. Palliative procedure (n = 19) done was diversion colostomy. The most common treatment given involved all the 3 above-mentioned modalities, with the majority of patients undergoing surgery with adjuvant chemotherapy with/without radiotherapy. Chemotherapy was administered in 70 patients, with the majority receiving FOLFOX-4 regimen (n = 62; 88.6%) and 5-fluorouracil/leucovorin in the rest of the 8 (11.4%). Patients who received radiation therapy were administered external beam radiotherapy at a dose of 1.8 Gy per fraction to a cumulative dose of 45 Gy.
Table 2.
Survival outcomes
The median overall survival (OS) of these patients was 23 months (2–66). Seven patients were lost to follow-up and were censored during analysis.
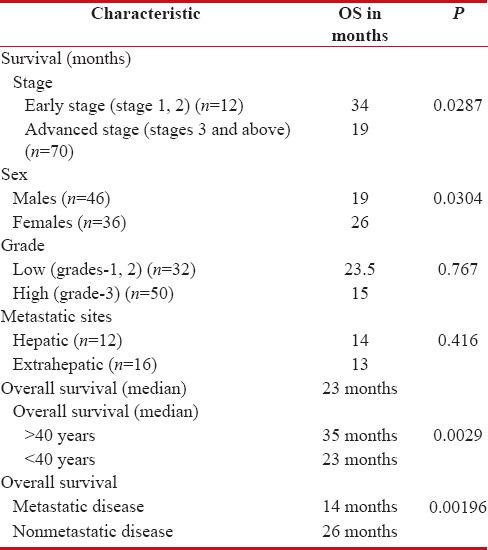
Those with early stage disease (stages 1, 2) had significantly higher survival than those with advanced stages (stage 3 and above), 34 and 19 months, respectively (P = 0.0287) [Figure 1]. Analysis also revealed significantly better survival in females compared to males – 26 and 18 months, respectively (P = 0.0242) [Figure 2]. Furthermore, those aged > 40 years and those with nonmetastatic disease had longer survival [Table 2] [Figures 3 and 4]. There was no significant difference in survival with respect to the grades of the tumor (P = 0.767) or site of metastases (hepatic versus extrahepatic) (P = 0.416).
Figure 1.
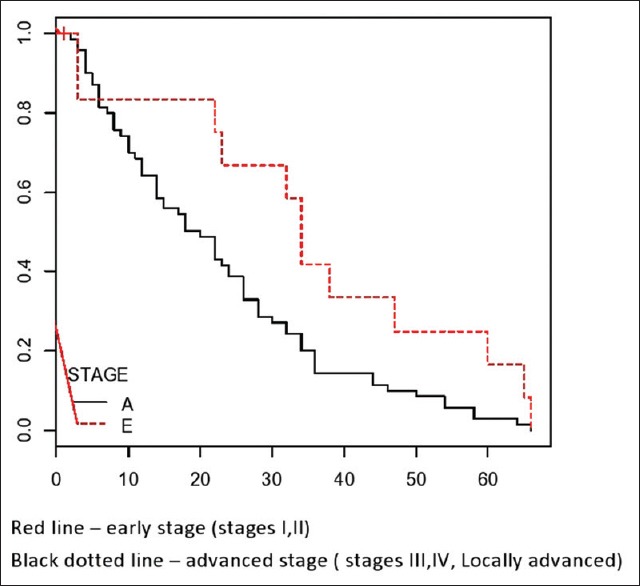
Kaplan–Mein curve comparing the survival between the stages – early and advanced
Figure 2.
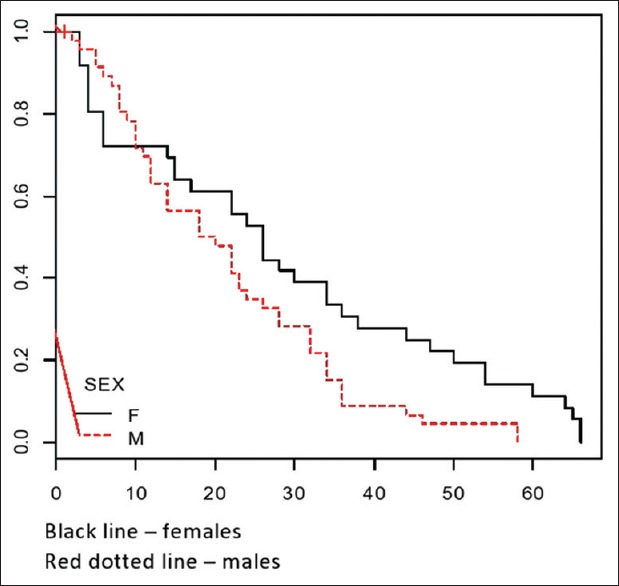
Kaplan–Mein curve comparing the survival between males and females
Figure 3.
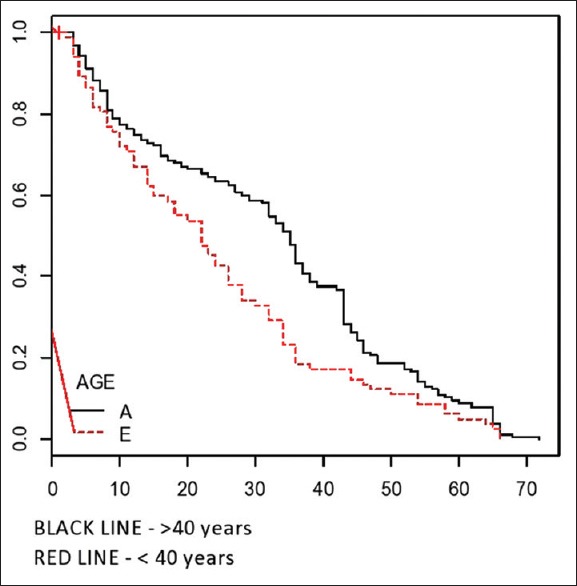
Survival differences between those aged <40 and >40 years
Figure 4.
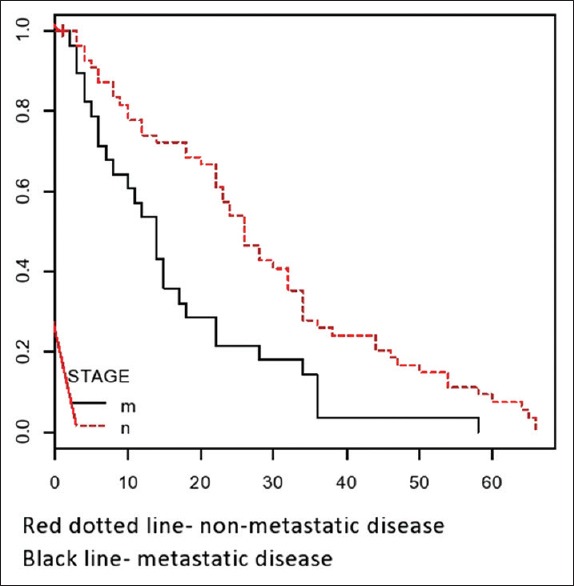
Comparing survival of metastatic versus nonmetastatic stage disease
Discussion
Our study revealed an incidence of 27.8% patients diagnosed with colon cancer in the age group <40 years. This is similar to other studies such as by Sudarshan et al.[2] and Kansakar and Singh.[4] which have documented an incidence of as much as 39.05% and 36%, respectively [Table 3]. The high incidence documented probably reflects the actual increase in incidence or better awareness and diagnostic modalities leading to detection of colon cancer in younger adults.
Table 3.
In comparison with other studies (continued on the next page)
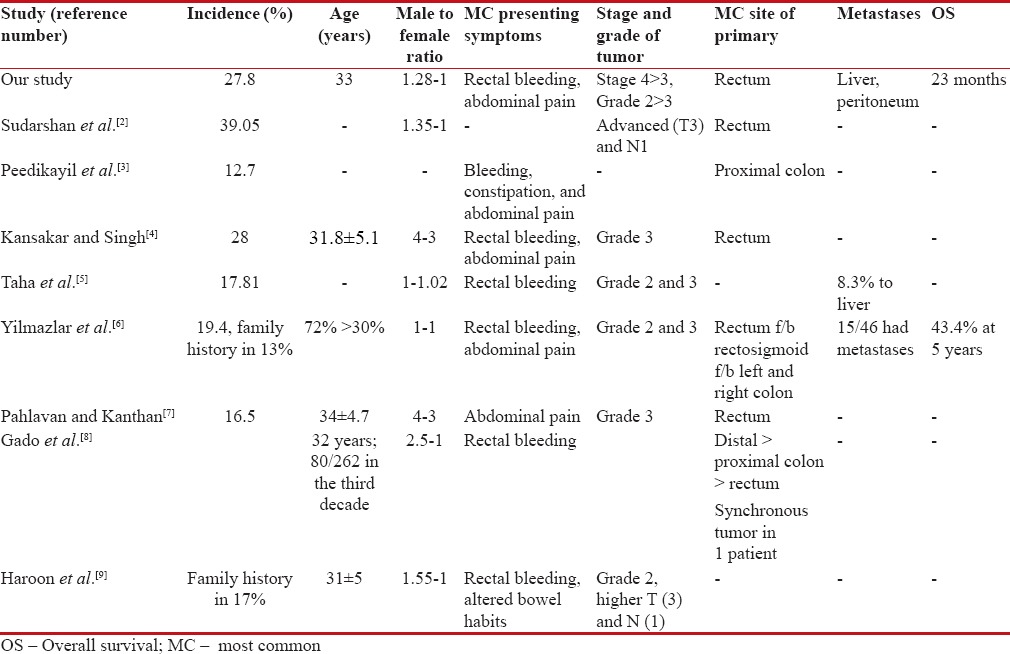
Most were aged between 30 and 39 years with a male preponderance, which is similar to other studies.[2,3,4,5,7,8,9] The most common symptoms in our study were bleeding per rectum and abdominal pain, similar to most studies.[3,4,5,6,7,8,9]
There was no family history of colon cancer in any of our patients. This is unlike some studies that have documented an incidence of >10%.[6,9]
The most common sites involved were the rectum, followed by right-sided colonic cancers. This is similar to various studies where rectum or the proximal colon has been the dominant sites of involvement in young patients.[2,3,6,7,8] Whether the propensity for tumors to occur more in the right colon than left in young patients is indicative of the presence of familial syndromes which are uninvestigated needs to be looked into. We had one case of synchronous primaries – rectum with hepatic flexure. Studies have not documented synchronous primaries, except the study by Gado et al.[8] which had one such case.
The stage of malignancy in our patients was mostly of advanced stage. There were a considerable number of patients with higher T and N status. This is in concordance with other studies which have documented higher stages in younger patients.[2,9] The delay in diagnosis, higher grade of tumor, and lower suspicion of malignancy in younger people due to assumed lack of incidence could be causative factors for an advanced presentation.
The grade of tumor in our series was mostly moderately or poorly differentiated carcinoma, suggesting a more aggressive tumor biology in this subset of patients, which translates to poorer outcomes. A higher grade of tumor has been documented in all studies that have analyzed this subset of patients.[3,6,9]
The most common sites of metastases in our study were liver, followed by intraabdominal sites such as peritoneum, ovary, and mesentery which concur with the fact that the most common presenting site is hepatic in CRC. Three cases had metastases in their appendicular skeleton – the humerus and radius and ulna, which are unusual sites of metastases in carcinoma colon.
Most patients were treated with curative intent, with most receiving the standard multimodality treatment. The most common practiced regimen in our center is FOLFOX-4 which was administered to 88.6% of the patients receiving chemotherapy, followed by 5-fluorouracil/leucovorin which is the regimen in those receiving concurrent chemoradiation. Other regimens commonly used include capecitabine/oxaliplatin and single agent capecitabine, which have not been used in any of the patients in the present study. Although the patients with metastatic disease received palliative chemotherapy, none could be administered targeted therapies.
The OS of the cohort was a median of 23 months, with patients in the early stages (34 months) doing significantly better than those in the advanced stage (19 months), i.e., patients who are node positive, locally advanced disease and metastatic disease. A study has documented a low 5-year survival of 23% in their patients of carcinoma colon in young.[10] Furthermore, those with metastatic disease upfront had a significantly inferior survival (14 months) compared to those without metastatic disease (26 months) (P = 0.00196). The median OS between those aged <40 and >40 years in our analysis revealed a significantly inferior outcomes for those with CRC in young, 35 versus 23 months (P = 0.0029). The lower survival noted could be due to higher grade and mere number of patients presenting with advanced stage of disease.
Analysis revealed that there were no variables that significantly affected survival such as age, grade, and site of metastases – hepatic versus extrahepatic. However, univariate analysis for gender revealed a significantly better outcome for females than males.
Conclusions
Colorectal carcinoma seems to be emerging as a major health problem even in developing countries like India. Changing lifestyle, dietary habits, obesity, and lesser physical activity would only become additive risk factors to this subset of patients. Our study revealed that carcinoma colon in young was aggressive and associated with high mortality. There should be a high index of suspicion in any young patient presenting with symptoms suggestive of a colonic malignancy and should be evaluated promptly and treated aggressively.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I thank all the staff and students of the Department of Medical Oncology, Kidwai Memorial Institute of Oncology.
References
- 1.Sirohi B, Shrikhande SV, Perakath B, Raghunandharao D, Julka PK, Lele V, et al. Indian J Med Paediatr Oncol. 2014 Jul-Sep;35(3):192–96. doi: 10.4103/0971-5851.142031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sudarshan V, Hussain N, Gahine R, Mourya J. Colorectal cancer in young adults in a tertiary care hospital in Chhattisgarh, Raipur. Indian J Cancer. 2013;50:337–40. doi: 10.4103/0019-509X.123621. [DOI] [PubMed] [Google Scholar]
- 3.Peedikayil MC, Nair P, Seena SM, Radhakrishnan L, Sadasivan S, Naryanan VA, et al. Colorectal cancer distribution in 220 Indian patients undergoing colonoscopy. Indian J Gastroenterol. 2009;28:212–5. doi: 10.1007/s12664-009-0087-z. [DOI] [PubMed] [Google Scholar]
- 4.Kansakar P, Singh Y. Changing trends of colorectal carcinoma in Nepalese young adults. Asian Pac J Cancer Prev. 2012;13:3209–12. doi: 10.7314/apjcp.2012.13.7.3209. [DOI] [PubMed] [Google Scholar]
- 5.Taha MO, Abdalla AA, Mohamed RS. Pattern and presentation of colorectal cancer in central Sudan, a retrospective descriptive study, 2010-2012. Afr Health Sci. 2015;15:576–80. doi: 10.4314/ahs.v15i2.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yilmazlar T, Zorluoglu A, Ozgüç H, Korun N, Duman H, Kaya E, et al. Colorectal cancer in young adults. Tumori. 1995;81:230–3. doi: 10.1177/030089169508100402. [DOI] [PubMed] [Google Scholar]
- 7.Pahlavan PS, Kanthan R. The epidemiology and clinical findings of colorectal cancer in Iran. J Gastrointestin Liver Dis. 2006;15:15–9. [PubMed] [Google Scholar]
- 8.Gado A, Ebeid B, Abdelmohsen A, Axon A. Colorectal cancer in Egypt is commoner in young people: Is this cause for alarm? Alex J Med. 2014;50:197–201. [Google Scholar]
- 9.Haroon N, Khan S, Alvi R. Rectal carcinoma under 40 years of age: Seven-year post-treatment follow-up at a tertiary care hospital in Pakistan. J Pak Med Assoc. 2013;63:1460–3. [PubMed] [Google Scholar]
- 10.Behbehani A, Sakwa M, Ehrlichman R, Maguire P, Friedman S, Steele GD, Jr, et al. Colorectal carcinoma in patients under age 40. Ann Surg. 1985;202:610–4. doi: 10.1097/00000658-198511000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]


