Abstract
Context:
Seventy-seven percent of musculoskeletal injuries sustained by United States Army Special Forces Operators are preventable. Identification of predictive characteristics will promote the development of screening methods to augment injury-prevention programs.
Objective:
To determine physical and performance characteristics that predict musculoskeletal injuries.
Setting:
Clinical laboratory.
Patients or Other Participants:
A total of 95 Operators (age = 32.7 ± 5.1 years, height = 179.8 ± 6.9 cm, mass = 89.9 ± 12.7 kg).
Main Outcome Measure(s):
Laboratory testing consisted of body composition, aerobic and anaerobic capacity, upper and lower body strength and flexibility, balance, and biomechanical evaluation. Injury data were captured for 12 months after laboratory testing. Injury frequencies, cross-tabulations, and relative risks (RRs) were calculated to evaluate the relationships between physical characteristics and injury proportions. Between-groups differences (injured versus uninjured) were assessed using appropriate t tests or Mann-Whitney U tests.
Results:
Less shoulder-retraction strength (RR = 1.741 [95% confidence interval = 1.003, 3.021]), knee-extension strength (RR = 2.029 [95% confidence interval = 1.011, 4.075]), and a smaller trunk extension : flexion ratio (RR = 0.533 [95% confidence interval = 0.341, 0.831]) were significant risk factors for injury. Group comparisons showed less trunk strength (extension: P = .036, flexion: P = .048) and smaller right vertical ground reaction forces during landing (P = .025) in injured Operators. Knee strength, aerobic capacity, and body mass index were less in the subgroup of spine-injured versus uninjured Operators (P values = .013−.036).
Conclusions:
Knee-extension and shoulder-retraction strength were risk factors for musculoskeletal injury in Operators. Less trunk-flexion and -extension strength, higher body mass index, lower aerobic capacity, and increased ground reaction forces during landing were characteristics that may also contribute to musculoskeletal injury. Having 2 or more risk factors resulted in a greater injury proportion (χ2 = 13.512, P = .015); however, more research is needed. Athletic trainers working in the military or similar high-demand settings can use these data to augment screening and injury-prevention protocols.
Key Words: military athletes, strength, flexibility, biomechanics
Key Points
Deficits in knee and shoulder strength were risk factors for musculoskeletal injury in Operators.
Having more than 1 risk factor significantly increased the Operators' risk for musculoskeletal injury.
Musculoskeletal injury due to training and recreation is a serious and often underrecognized problem in military populations.1−4 These injuries place a large burden on our military personnel (operational and medical) and can directly affect the readiness of Special Operations Forces (SOF) across various branches of service.4−8 Epidemiologic data4,5 have demonstrated that a large proportion of the musculoskeletal injuries seen in basic military forces and in the SOF community occurred during training and were preventable. These researchers5 have defined preventable injuries as those that can be reduced through the use of injury-prevention programs by modifying the characteristics related to musculoskeletal injury. The leadership has also recognized that these high incidence and recurrence rates of injury may negatively affect the quality of life after service. Athletic trainers and other medical staff within the armed forces have a unique opportunity to combat this problem through screening and prevention initiatives.
Physical training is a critical part of enhancing physical and occupational performance in SOF Operator groups, yet a large proportion of the injuries seen in these groups were directly related to training.7,9,10 A recent epidemiologic evaluation5 of injuries in the US Army Special Forces demonstrated injuries in up to 20.8% of Operators per year, of which 76.9% were preventable musculoskeletal injuries. This highlights the need for an injury-prevention and performance-enhancement training program to combat the large number of musculoskeletal injuries observed during training. Continual evaluation and modification of current injury-prevention and performance-enhancement programming is needed to combat the injuries incurred by military athletes and the subsequent effect on individual and force readiness. Training programs, such as Tactical Human Optimization, Rapid Rehabilitation and Restoration (THOR3), are in place and can be modified for individual needs and to optimize both injury prevention and human performance.
The successful application of an injury-prevention and performance-enhancement initiative has long-term implications for improving the suboptimal characteristics leading to injury, potentially improving the soldier's career longevity.11 Previous reports4,11 have suggested that programs designed to prevent injury and optimize performance in the military are valid and effective. However, before a clinical trial can be conducted, the population-specific modifiable characteristics that are related to a future incidence of injury must first be identified. Therefore, the purpose of our study was to determine the physiological, musculoskeletal, biomechanical, and balance characteristics that may be risk factors for musculoskeletal injuries in US Army SOF Operators. We hypothesized that physiological performance, strength, flexibility, biomechanical, and balance characteristics would be different between injured and uninjured groups. Identifying modifiable risk factors for future injury is critical for developing effective injury-prevention initiatives aimed at reducing avoidable musculoskeletal injuries during service and preserving Operators' career longevity and quality of life after service. In addition to identifying risk factors for injury, we may be able to develop algorithms to screen candidates or cadets who are applying for admission to the SOF community and may be at greater risk of developing injuries.
METHODS
Human subject protections approval for the study procedures and data handling was obtained from the institutional review boards of both the university and the US Army Medical Research and Materiel Command. The demographic information for the Operators who participated in this study are listed in Table 1. Baseline data-collection procedures consisted of physiological, musculoskeletal strength and flexibility, biomechanical, and balance characteristics. Medical records were queried for any injury that occurred during the 12 months after baseline laboratory testing.
Table 1. .
Injury Descriptions
| Description |
n (Proportion, %) |
| Operators | |
| Injured | 48 (50.5) |
| Uninjured | 47 (49.5) |
| Total | 95 (100.0) |
| Location | |
| Upper extremity | 17 (25.8) |
| Spine | 23 (34.8) |
| Lower extremity | 26 (39.4) |
| Total | 66 (100.0) |
Procedures
Physiological Testing.
Body composition was measured using the Bod Pod Body Composition System (Cosmed Inc, Chicago, IL), which applies air-displacement plethysmography to measure body volume and calculate body density based on the Operator's weight. Operators were required to wear spandex or compression shorts and a swim cap while seated in the pod. Appropriate densitometry equations were used with predicted lung volumes.12 Excellent reliability (intraclass correlation coefficient [ICC] = 0.98, standard error of the mean [SEM] = 0.47% body fat) has been demonstrated for this method.13
The Velotron cycling ergometer (RacerMate Inc, Seattle, WA) and Wingate protocol were used to measure peak anaerobic power and capacity during a maximal-effort trial.14 Before a 5-minute, self-paced warmup, we fitted each Operator to the cycle ergometer by adjusting the seat and handlebar position. The Operator began the test by maintaining a pace of 100 revolutions per minute at 125 watts for 15 seconds. After the 15-second preparatory phase, the Operator had 5 seconds to sprint as fast as he could before the electromagnetic brake of 9% of body weight was applied and sustained for 30 seconds. The Operator was instructed to pedal as hard and as fast as he could during the entire braking phase and received oral encouragement throughout the test. Peak anaerobic power and capacity were defined as the maximum wattage and mean wattage, respectively, normalized to body weight, during the 30-second braking phase. This procedure has been previously determined to be both valid and reliable.15
Maximal oxygen consumption was measured during a modified incremental maximal treadmill protocol using a TrueOne metabolic system (Parvo Medics, Sandy, UT).16 Before the test, Operators performed a 5-minute warmup at 75% of their self-reported last 2-mile Army Physical Fitness Test pace. The test was performed at 90% of this pace. The test began at 0% treadmill incline and was increased by 2% every 3 minutes until volitional fatigue occurred. Oral encouragement was given throughout the test. Here, Vॱo2max was calculated as the highest 1-minute average during the test and normalized to body weight (mL·min−1·kg−1). This value has previously been reported17 as reliable and predictive of aerobic fitness in US Army trainees.
Musculoskeletal Assessment.
Isokinetic strength of shoulder internal and external rotation, shoulder protraction and retraction, shoulder elevation, knee flexion and extension, and torso flexion and extension were assessed using the Multi-Joint System 3 Pro (Biodex Medical Systems Inc, Shirley, NY). All measures were completed using the manufacturer's guidelines and collected bilaterally when appropriate. The mean normalized peak torque (Nm/kg) of 5 reciprocal trials was used as the measure of strength. Knee-extension and -flexion strength tested on the Biodex have been previously shown18 to have excellent reliability (ICC = 0.96, SEM = 12.7% body weight [BW] and ICC = 0.98, SEM = 9.3% BW, respectively). Shoulder internal- and external-rotation strength have demonstrated good reliability (ICC = 0.79, SEM = 5.2% BW and ICC = 0.784, SEM = 5.8% BW, respectively).19 Pilot data collected in our research facility demonstrated good to excellent reliability for shoulder protraction-retraction and torso flexion-extension (ICC = 0.83–0.93, SEM = 16.8%–47.2% BW and ICC = 0.92–0.98, SEM = 12.4%–13.5% BW, respectively). Ankle-inversion and -eversion isometric strength was assessed with a handheld dynamometer (Lafayette Instrument Company, Lafayette, IN) using a break protocol. The results of 3 trials were collected and averaged to calculate the mean isometric ankle strength for inversion and eversion (% BW).
Range of motion during flexibility testing was measured using a digital inclinometer (Smart Tool Technologies, M-D Building Products, Oklahoma City, OK). Flexibility of shoulder internal-external rotation and hip extension were assessed using the methods described by Norkin and White,20 which have been shown to have good to excellent reliability (ICC = 0.824–0.935, SEM = 3.25° and ICC = 0.855, SEM = 2.318°, respectively).19 So the examiner could measure posterior shoulder tightness, the Operator assumed the supine position with the shoulder abducted and the elbow flexed to 90°. The examiner blocked movement of the scapula with 1 hand and horizontally adducted the humerus with the other. The excursion of the humerus relative to the trunk (°) was measured. This measure of posterior shoulder tightness has been demonstrated to have excellent reliability (ICC = 0.94, SEM = 1.8°).21 Active knee extension was measured with the Operator in the supine position and the hip and knee bent to 90°. The Operator was then asked to straighten the knee as far as possible while 1 examiner stabilized the thigh and another examiner measured knee flexion (°). This measure of hamstrings flexibility has been shown to have excellent reliability (ICC = 0.901, SEM = 4.208°).19 Three trials were completed for all flexibility measures and the results averaged.
Biomechanical and Balance Assessment.
Biomechanical characteristics during double- and single-legged landings were measured while Operators performed a double-legged stop-jump task and a single-legged drop-landing task. The double-legged stop-jump task required Operators to perform a forward broad jump over a distance equal to 40% of their body height, land on a 40- × 60-cm force plate, and immediately perform a maximal vertical jump. The single-legged drop-landing task required Operators to begin by standing on 1 leg on top of a 45.7-cm platform, drop off the platform, and land with the same leg on the force plate. This test was completed bilaterally. Retroreflective markers (14 mm) were placed on anatomical landmarks of the Operator's lower extremity (LE) and pelvis according to the Vicon plug-in-gait biomechanical model (Vicon, Centennial, CO). Anthropometric measurements (ie, height, weight, leg length, and knee and ankle widths) were entered into the data-collection software (Nexus version 1.8; Vicon) and used for estimations of joint centers and segment parameters in the biomechanical model. Raw marker trajectory data were collected using a high-speed infrared camera system composed of 6 cameras (model T-Series; Vicon) collecting at a sampling frequency of 200 Hz. Ground reaction forces were measured using 2 force plates (model 9286A; Kistler Instrument Corporation, Amherst, NY) that were flush with the surrounding ground surface and data were collected at a sampling frequency of 1200 Hz. The plug-in-gait biomechanical model was used for kinematic calculations. This model and system have been shown to be a valid and reliable method of 3-dimensional kinematic analysis of the LE (canonical measure of correlation = 0.611–0.983). Maximum and initial-contact knee-joint angles, along with peak vertical ground reaction forces, were averaged across 3 trials using a custom MATLAB script (The MathWorks Inc, Natick, MA). Trials were discarded and repeated if the Operator did not land completely on the force plate.
Dynamic postural stability was assessed during a single-legged landing task as described by Sell.22 Operators were asked to perform a forward double-legged jump from a distance of 40% of their height, land on 1 leg, and achieve balance as quickly as possible. A custom MATLAB script was used to calculate the dynamic postural stability index and medial-lateral stability index as described by Wikstrom et al.23 This method of assessing dynamic postural stability has been shown to have good to excellent reliability (ICC = 0.86, SEM = 0.01). This procedure was completed on both legs. The Sensory Organization Test (SOT) using a NeuroCom Balance Manager system (SMART Balance Master; Natus Medical Inc, San Carlos, CA) was also used to assess standing postural stability under various conditions. Operators were asked to stand on both feet (barefoot), and the examiner aligned their feet on the platform according to the manufacturer's recommendations. This test consisted of 3 trials in each of the 6 conditions in the SOT test battery (SOT1: eyes open, SOT2: eyes closed, SOT3: eyes open–reactive surround, SOT4: eyes open–reactive surface, SOT5: eyes closed–reactive surface, SOT6: eyes open–reactive surface and surround). The SOT had moderate reliability in a young healthy population (ICC = 0.67).24
Prospective Injury Data.
Injury occurrence was reviewed at the end of the 1-year follow-up period from the laboratory data-collection session. The record of musculoskeletal injuries that occurred within that 1-year time period was obtained from the Operators' paper medical charts maintained locally by medical personnel within their respective units. The research team reviewed the medical charts and extracted musculoskeletal injury data using International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes (https://www.cdc.gov/nchs/icd/icd9cm.htm). All data obtained from medical chart review were entered into a customized database. For the purposes of this study, we defined a relevant musculoskeletal injury as an injury to the musculoskeletal system (ie, bones, ligaments, muscles, tendons, or nerves) for which medical treatment was sought and documented. Medical conditions consisted of diagnoses such as sprains, strains, dislocations, and fractures. Contusions, lacerations, open wounds, amputations, and musculoskeletal conditions resulting from traumatic incidences such as motor vehicle accidents, gunshot wounds, or explosives or shrapnel were not included. Independent statistical analyses were conducted for the following outcome variables: all injuries, LE injuries, spine injuries, and upper extremity (UE) injuries.
The ICD-9-CM codes that were identified as relevant to our research were analyzed further; other codes were deleted. The outcome was a relevant ICD-9-CM code (relevant injury) that occurred during the 365 days after laboratory data collection.
Statistical Analysis.
All statistical procedures were performed using SPSS (version 22; IBM Corp, Armonk, NY). Descriptive statistics were calculated for all variables, and normality was assessed using a Shapiro-Wilk test. Frequencies and cross-tabulations were used to examine the proportions of injuries. Between-groups differences (injured group versus uninjured group) were assessed using appropriate t tests or Mann-Whitney U tests. To further evaluate each variable as a potential risk factor for injury, we determined cutoff values for each variable (Table 2). The bottom 25th percentile value of each variable was used for all cutoff values except for body fat percentage; previous researchers13 have demonstrated that general Army Soldiers with greater than 18% body fat displayed decreased physical performance. Relative risks (RRs) and 95% confidence intervals (CIs) were calculated. Relative risk values were considered statistically significant if the 95% CI did not include 1.00. Lastly, a risk factor count score was calculated for each Operator that was the sum of characteristics for which he fell below the 25th percentile. A χ2 test was used to test the dependence of injured participant proportions on risk factor counts with P < .05 considered statistically significant.
Table 2. .
Strength Measures and Relative Risks of Injury in US Army Special Forces Operatorsa
| Relative Risk (95% Confidence Interval) | ||||
| Variable |
Cutoff |
All Injuries |
Lower Extremity Injuries |
Spine Injuries |
| Strength | ||||
| Left knee extension, % BW | <195.7 | 1.901 (1.029, 3.512) | ||
| Right knee extension, % BW | <202.6 | 2.029 (1.011, 4.075) | ||
| Left shoulder retraction, % BW | <363.1 | 1.741 (1.003, 3.021) | ||
| Trunk extension : flexion ratio | <1.75 | 0.533 (0.341, 0.831) | ||
Abbreviations: % BW, body weight percentage.
Only variables with significant relative risks are reported. No significant relative risk was evident for upper extremity injuries.
RESULTS
Group Comparison
A total of 95 US Army SOFs took part in this study. Of the total participants, 47 (49.5%) went on to sustain an injury during the 12-month period after baseline testing. Lower extremity injuries were most common (39.4%), followed by spine and UE injuries (Table 1). All descriptive statistics and the results of normality testing and between-groups comparisons are reported in Supplemental Tables (available online at http://dx.doi.org/10.4085/1062-6050-52.12.22.S1). Flexibility and balance results failed to show between-groups differences for any injury groups or subgroups. Operators who sustained an injury demonstrated less trunk strength for both extension (273.05% BW versus 321.59% BW, P = .036) and flexion (186.21% BW versus 200.08% BW, P = .048). Landing biomechanics also revealed between-groups differences as Operators who sustained injuries demonstrated less right knee flexion at initial contact (23.6° versus 26.6°, P = .049); however, the left knee data were not significant (24.3° versus 25.1°, P = .623). Despite the smaller right knee-flexion angle at initial contact, Operators who sustained an injury showed smaller right vertical ground reaction forces during single-legged drop landings (559.4% BW versus 610.3% BW, P = .025).
Among the LE injury subgroup, trunk strength and some landing kinematics were different between groups. The Operators who sustained LE injuries had less trunk-flexion strength (181.00% BW versus 197.56% BW, P = .032). Additionally, the right knee varus angles at initial contact during stop jumps (8.0° versus 4.6°, P = .011) and drop landings (1.6° versus −0.3°, P = .006) were greater in Operators who sustained an LE injury.
The UE injury subgroup displayed only 1 significant difference from the uninjured group: age. Operators who went on to develop or sustain an UE injury were older (35.0 versus 30.5 years, P = .039). Lastly, the spine-injured subgroup showed several between-groups differences. Operators who developed a future spine injury had decreased Vॱo2max scores compared with those without spine injuries (44.3 versus 47.6 mL·min−1·kg−1, P = .013). These Operators also had a greater body mass index (BMI) than those who did not have a spine injury (27.84 versus 26.14, P = .013). Left knee-extension strength was also weaker among the spine-injured group than among those without a spine injury (205.57% BW versus 225.28% BW, P = .036).
Risk Factor Analysis
To further assess the measured characteristics of these Operators as potential risk factors for injuries, we calculated RRs for the injured group and for each of the injury subgroups (Table 2). Knee-extension strength, shoulder-retraction strength, and right shoulder internal-rotation range of motion yielded significant RRs ranging from 2.215 to 5.689. Operators who fell into the bottom 25th percentile for knee-extension strength were 2.215 (95% CI = 1.071, 4.582) times more likely to sustain any injury and between 3.263 (95% CI = 1.016, 10.482) and 5.689 (95% CI = 1.657, 19.534) times more likely to sustain an LE injury. Operators in the bottom 25th percentile of left shoulder retraction strength were 4.952 (95% CI = 1.553, 15.788) times more likely to sustain a spine injury, and those in the bottom 25th percentile of right shoulder internal-rotation range of motion were 3.208 (95% CI = 1.193, 8.625) times more likely to sustain a spine injury.
There was a direct relationship between the proportion of injured Operators and the sum of risk factors (Figure). Injury proportions were associated with risk factor counts (χ2 = 13.512, P = .015). The distribution of injured to uninjured Operators with a risk factor count equal to zero was 32% injured and 68% uninjured. However, a greater proportion of Operators in the injured group had a risk factor count of 1 (65% versus 35%), and 100% of those with a risk factor count of 4 were injured.
Figure.
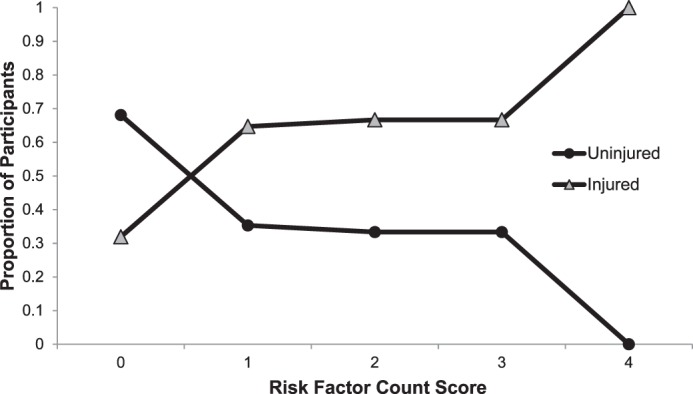
Relationship between proportions of Operators classified in the injured and uninjured groups and the risk factor count score.
DISCUSSION
Identification of population-specific modifiable characteristics is critical to the implementation of an injury-prevention initiative for a unique population such as US Army SOF Operators. The purpose of our study was to determine the physiological, musculoskeletal, and biomechanical characteristics that predicted musculoskeletal injury, which are critical to developing screening procedures in Operators. We hypothesized that these measured characteristics would differ between injured and uninjured groups, and this was partially supported by our results. The comparison between injured and uninjured groups revealed some between-groups differences in strength and landing biomechanics. Relative risk analyses revealed deficits in knee-extension strength, shoulder-retraction strength, and shoulder internal-rotation flexibility to be risk factors for musculoskeletal injury. Comparison of the injured and uninjured groups suggested that reduced knee-extension strength, trunk-flexion strength, and knee-flexion position at initial contact may also be risk factors for injury. Additionally, an inverse relationship was found between the proportion of injured Operators and the risk factor count.
Operators who sustained an injury had significantly less trunk-flexion and -extension strength compared with those who did not sustain an injury. After creating subgroups based on injury type, we found that Operators who sustained an LE injury had significantly less trunk-flexion strength and less knee-extension strength than those who did not sustain an LE injury. Trunk and knee strength were also important in spine injuries. Operators who sustained a spine injury also had significantly less trunk-flexion and knee-extension strength. Although this is the first study to identify a prospective relationship between strength characteristics and injuries in Special Forces Operators, previous researchers25 have noted knee-extension strength was related to overuse injuries in conventional forces. In a meta-analysis, Kollock et al25 suggested that improving knee-extensor strength would help prevent overuse injuries, such as patellofemoral pain syndrome and patellar tendinopathy, in military personnel.25 In an athletic population, strength deficits at the knee have been shown to contribute to more than just overuse injuries and athletic performance.26−28 In the tactical athlete, knee-extensor strength is critical to functional knee-joint stability and tactical performance. Previous investigators29 have also shown that defects in trunk strength were related to injury and back pain in collegiate wrestlers. Maintaining trunk and knee strength is an important component for injury prevention in US Special Forces.
Injured Operators also used less knee flexion at initial contact during landing. Landing with less knee flexion at initial contact has been linked with increased joint loading and is considered a risk factor for some LE injuries, including those affecting the anterior cruciate ligament and meniscus.30 However, we did not detect any group differences in knee-flexion angle at initial contact when examining LE injuries alone. Although differences in knee flexion at initial contact were not significant when we assessed the subgroup with LE injury, the difference in knee-valgus angle at initial contact was significant. Operators who sustained an LE injury landed in more knee varus than those who did not sustain an LE injury. This is in contrast to previous findings31−33 that indicated increased knee-valgus angle was a risk factor for acute LE injuries, such as those to the anterior cruciate ligament, and chronic injuries, such as those associated with anterior knee pain. However, these authors mainly studied a female athletic population, so their results may not be applicable to other populations, which potentially explains why our findings did not agree. Despite this difference, improper frontal-plane knee alignment is an important biomechanical characteristic related to LE injury, and landing in neutral knee alignment protects against LE injury.
Other characteristics such as BMI and Vॱo2max were also different between groups but only for the subgroup of those with spine injuries. Operators who sustained a spine injury had a significantly greater BMI than those who did not. Body mass index has been established as a risk factor for various musculoskeletal injuries, including spine injuries.34−37 Although BMI is not an adequate measure of body composition, it does reflect changes in weight relative to height. In particular, increases in upper body weight, whether originating from fat or lean tissue, would increase loading stress on the spine, perhaps explaining the observed increased risk of spine injury. Additionally, Vॱo2max was less in Operators who sustained a spine injury. Although Vॱo2max may not have a direct physiological link to spine injury, it has been shown to predict athletic performance. United States SOF Operators are required to work at a certain intensity despite a physiological limitation such as Vॱo2max. Operators with higher BMI and lower aerobic capacity may be at an increased risk of injury.
To our knowledge, we are the first to prospectively evaluate differences between injured and uninjured military personnel as well as to establish musculoskeletal characteristics as risk factors for musculoskeletal injury in US SOF Operators. Sell et al4 established risk factors for musculoskeletal injury in US 101st Airborne Air Assault Army soldiers by comparing baseline data with those of healthy, elite-level triathletes. They found that 101st soldiers had strength deficits at the knee, shoulder, and ankle; flexibility deficits in the shoulder; and physiological deficits in BMI, body fat percentage, anaerobic power, anaerobic capacity, and aerobic capacity. Although Sell et al4 provided a unique analysis and comparison that demonstrated suboptimal performance in this military cohort, we were also able to highlight prospective differences between Operators who went on to become injured and those who did not. Dvorak et al38 conducted a similar study investigating risk factors for injury in football athletes but did not include measures of strength, flexibility, balance, or biomechanics. They found that individuals who were injured had lower percentages of body fat.38
We identified 3 modifiable characteristics that demonstrate how Operators with deficits in these areas had a higher likelihood of becoming injured. Operators in the bottom 25th percentile for knee-extension strength, shoulder-retraction strength, and shoulder internal-rotation range of motion had 2.215 to 5.689 times the risk of becoming injured compared with Operators above the bottom 25th percentile. However, no physiological, strength, flexibility, balance, or biomechanical characteristics demonstrated higher odds of an UE injury for those who fell in the bottom 25th percentile. We expected to observe more relationships between characteristics and injury; however, this lack may be due to the fact that we used ICD-9-CM codes for LE musculoskeletal injuries. Also, we grouped injuries by gross location because further separation into specific injuries or sublocations did not provide large enough sample sizes for appropriate analyses.
As the risk factor count increased, there was a greater proportion of injured than uninjured Operators. This finding suggests that Operators who fell in the bottom 25th percentile in multiple characteristics were at greater risk of sustaining an injury. A previous study39 in US Army Rangers also determined that multiple risk factors increased the likelihood of sustaining an injury. Dvorak et al38 found a similar relationship in elite-level football players: the greater the number of risk factors, the greater the proportion of injured players. This result is important for athletic training and other medical and human performance staffs as it suggests the need to consider and assess individualized training and rehabilitation to target deficits related to peer performance. Also, these findings help justify the use of screening methods in the military to identify individuals at increased risk of sustaining a musculoskeletal injury, thereby providing the opportunity to implement a specific prevention intervention.
Earlier researchers34,36 who aimed to identify risk factors for musculoskeletal injuries in military populations have commonly found body composition measures such as a high BMI to be risk factors for injury. However, we did not find that body fat percentage was a risk factor for injury and only observed a BMI difference in the spine-injury group. Teyhen et al39 performed a similar prospective risk factor analysis using BMI in US Army Rangers and demonstrated no difference between soldiers who sustained an injury and those who did not. This discrepancy may be due to the observed population. Soldiers required to perform at a higher level of physical standard, such as SOF Operators, may be less susceptible to injuries related to a larger BMI or body fat percentage due to their training. However, an increased percentage of body fat was related to decreased performance, and therefore, optimization is still recommended in future efforts to maximize force effectiveness.13
LIMITATIONS
Limitations were associated with this study. We tracked musculoskeletal injuries over a 12-month period using the ICD-9-CM codes reported in each Operator's medical chart. Although this method of injury and disease tracking is widely used and accepted, causes and mechanisms of injuries are often not reported.1,3,9,40,41 Because of this, we were not able to report or categorize injuries based on specific mechanisms. Despite the use of ICD-9-CM diagnosis codes and large groupings of injuries, RR values were still significant. Furthermore, the sample size, particularly within the multiple risk factor counts analysis, reduced the potential for detecting a true association and repeating the findings despite significant χ2 values. Further research is warranted to expand upon and validate this concept and to assess the effect of multiple risk factors on the risk of sustaining musculoskeletal injury in the military. In addition, these data were collected from US Army SOF Operators; therefore, the generalizability of these findings may be limited to this population and may not align well with other military forces. Military groups with different injury patterns and demands may have different risk factors, potentially due to different injury mechanisms or exposures. Additionally, different SOF groups throughout different military branches and even within the Army may display different injury characteristics and exposures due to different operation specialties and deployment patterns. Population- and demand-specific training and injury prevention are critical considerations for human performance and rehabilitation in the military and need to be considered in future studies. Lastly, we reported large CIs for some RR values. Some characteristics were not normally distributed (ie, rightward skewed), which may have contributed to the wider CIs for these characteristics. However, some variables that were normally distributed also displayed wide CIs, possibly due to the smaller sample sizes relative to the injury occurrences. Outlier analyses did not identify any significantly influential points. Despite these wider CIs, significant RR ratios were still seen.
CONCLUSIONS
The findings of this study demonstrate the importance of optimizing knee-extension strength, trunk strength, and knee position on landing to prevent musculoskeletal injuries in US Army SOF Operators. Operators with a deficit in knee-extensor strength were more likely to sustain an LE injury. We also found that shoulder-retraction strength and shoulder internal-rotation deficits contributed to a higher likelihood of sustaining an injury. Additionally, the accumulation of risk factors seemed to compound the risk of sustaining injuries. Athletic trainers and military staff within the armed forces are in a unique position to develop and implement injury-prevention initiatives to minimize training-related musculoskeletal injuries. The findings from this study also highlight the need for individualized screening and training that focus on identifying and correcting musculoskeletal and performance deficits relative to peers. Future studies are needed to validate such training interventions in this population.
Supplementary Material
ACKNOWLEDGMENTS
This study was supported by USAAMRE/TATRC #W81XWH-11-2-0020.
DISCLAIMER
The opinions expressed in this document are solely those of the authors and do not represent an endorsement by or the views of the US Army or the US Army Special Operations Command.
SUPPLEMENTAL MATERIAL
Supplemental Tables.
Found at DOI: http://dx.doi.org/10.4085/1062-6050-52.12.22.S1
REFERENCES
- 1. Hauret KG, Jones BH, Bullock SH, Canham-Chervak M, Canada S. . Musculoskeletal injuries: description of an under-recognized injury problem among military personnel. Am J Prev Med. 2010; 38 suppl 1: S61– S70. [DOI] [PubMed] [Google Scholar]
- 2. Jones BH, Bovee MW, Harris JM III, Cowan DN. . Intrinsic risk factors for exercise-related injuries among male and female army trainees. Am J Sports Med. 1993; 21 5: 705– 710. [DOI] [PubMed] [Google Scholar]
- 3. Jones BH, Cowan DN, Tomlinson JP, Robinson JR, Polly DW, Frykman PN. . Epidemiology of injuries associated with physical training among young men in the army. Med Sci Sports Exerc. 1993; 25 2: 197– 203. [PubMed] [Google Scholar]
- 4. Sell TC, Abt JP, Crawford K, et al. Warrior Model for human performance and injury prevention: Eagle Tactical Athlete Program (ETAP) Part I. J Spec Oper Med. 2010; 10 4: 2– 21. [DOI] [PubMed] [Google Scholar]
- 5. Abt JP, Sell TC, Lovalekar MT, et al. Injury epidemiology of U.S. Army Special Operations Forces. Mil Med. 2014; 179 10: 1106– 1112. [DOI] [PubMed] [Google Scholar]
- 6. Hollingsworth DJ. . The prevalence and impact of musculoskeletal injuries during a pre-deployment workup cycle: survey of a Marine Corps special operations company. J Spec Oper Med. 2009; 9 4: 11– 15. [DOI] [PubMed] [Google Scholar]
- 7. Lovalekar M, Abt JP, Sell TC, Keenan K, Zimmer A, Lephart SM. . Descriptive epidemiology of musculoskeletal injuries in naval special warfare personnel. Med Sci Sports Exerc. 2013; 45 suppl 5: 63– 66. [Google Scholar]
- 8. Shaffer RA, Brodine SK, Ito SI, Le AT. . Epidemiology of illness and injury among U.S. Navy and Marine Corps female training populations. Mil Med. 1999; 164 1: 17– 21. [PubMed] [Google Scholar]
- 9. Lynch JH, Pallis MP. . Clinical diagnoses in a Special Forces group: the musculoskeletal burden. J Spec Oper Med. 2008; 8 2: 76– 80. [Google Scholar]
- 10. Peterson SN, Call MH, Wood DE, Unger DV, Sekiya JK. . Injuries in Naval Special Warfare Sea, Air, and Land personnel: epidemiology and surgical management. Oper Techniques Sports Med. 2005; 13 3: 131– 135. [Google Scholar]
- 11. Sell TC, Abt JP, Crawford K, et al. Warrior Model for human performance and injury prevention: Eagle Tactical Athlete Program (ETAP) Part II. J Spec Oper Med. 2010; 10 4: 22– 33. [DOI] [PubMed] [Google Scholar]
- 12. Siri WE. . Body composition from fluid spaces and density: analysis of methods. 1961. Nutrition. 1993; 9 5: 480– 491; discussion 480, 492. [PubMed] [Google Scholar]
- 13. Crawford K, Fleishman K, Abt JP, et al. Less body fat improves physical and physiological performance in army soldiers. Mil Med. 2011; 176 1: 35– 43. [DOI] [PubMed] [Google Scholar]
- 14. Smith JC, Hill DW. . Contribution of energy systems during a Wingate power test. Br J Sports Med. 1991; 25 4: 196– 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bar-Or O. . The Wingate anaerobic test. An update on methodology, reliability and validity. Sports Med. 1987; 4 6: 381– 394. [DOI] [PubMed] [Google Scholar]
- 16. Kang J, Chaloupka EC, Mastrangelo MA, Biren GB, Robertson RJ. . Physiological comparisons among three maximal treadmill exercise protocols in trained and untrained individuals. Eur J Appl Physiol. 2001; 84 4: 291– 295. [DOI] [PubMed] [Google Scholar]
- 17. Sharp MA, Patton JF, Knapik JJ, et al. Comparison of the physical fitness of men and women entering the U.S. Army: 1978−1998. Med Sci Sports Exerc. 2002; 34 2: 356– 363. [DOI] [PubMed] [Google Scholar]
- 18. Keskula DR, Dowling JS, Davis VL, Finley PW, Dell'omo DL. . Interrater reliability of isokinetic measures of knee flexion and extension. J Athl Train. 1995; 30 2: 167– 170. [PMC free article] [PubMed] [Google Scholar]
- 19. Sell TC, Tsai YS, Smoliga JM, Myers JB, Lephart SM. . Strength, flexibility, and balance characteristics of highly proficient golfers. J Strength Cond Res. 2007; 21 4: 1166– 1171. [DOI] [PubMed] [Google Scholar]
- 20. Norkin CC, White DJ. . Measurement of Joint Motion: A Guide to Goniometry. 2nd ed. Philadelphia, PA: FA Davis Company; 1995. [Google Scholar]
- 21. Myers JB, Oyama S, Wassinger CA, et al. Reliability, precision, accuracy, and validity of posterior shoulder tightness assessment in overhead athletes. Am J Sports Med. 2007; 35 11: 1922– 1930. [DOI] [PubMed] [Google Scholar]
- 22. Sell TC. . An examination, correlation, and comparison of static and dynamic measures of postural stability in healthy, physically active adults. Phys Ther Sport. 2012; 13 2: 80– 86. [DOI] [PubMed] [Google Scholar]
- 23. Wikstrom EA, Tillman MD, Smith AN, Borsa PA. . A new force-plate technology measure of dynamic postural stability: the dynamic postural stability index. J Athl Train. 2005; 40 4: 305– 309. [PMC free article] [PubMed] [Google Scholar]
- 24. Wrisley DM, Stephens MJ, Mosley S, Wojnowski A, Duffy J, Burkard R. . Learning effects of repetitive administrations of the sensory organization test in healthy young adults. Arch Phys Med Rehabil. 2007; 88 8: 1049– 1054. [DOI] [PubMed] [Google Scholar]
- 25. Kollock RO, Andrews C, Johnston A, et al. A meta-analysis to determine if lower extremity muscle strengthening should be included in military knee overuse injury-prevention programs. J Athl Train. 2016; 51 11: 919– 926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Alemdaroğlu U. . The relationship between muscle strength, anaerobic performance, agility, sprint ability and vertical jump performance in professional basketball players. J Hum Kinet. 2012; 31: 149– 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Milgrom C, Finestone A, Eldad A, Shlamkovitch N. . Patellofemoral pain caused by overactivity. A prospective study of risk factors in infantry recruits. J Bone Joint Surg Am. 1991; 73 7: 1041– 1043. [PubMed] [Google Scholar]
- 28. Palmieri-Smith RM, Lepley LK. . Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med. 2015; 43 7: 1662– 1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Iwai K, Nakazato K, Irie K, Fujimoto H, Nakajima H. . Trunk muscle strength and disability level of low back pain in collegiate wrestlers. Med Sci Sports Exerc. 2004; 36 8: 1296– 1300. [DOI] [PubMed] [Google Scholar]
- 30. Chu Y, Sell TC, Abt JP, et al. Air assault soldiers demonstrate more dangerous landing biomechanics when visual input is removed. Mil Med. 2012; 177 1: 41– 47. [DOI] [PubMed] [Google Scholar]
- 31. Weiss K, Whatman C. . Biomechanics associated with patellofemoral pain and ACL injuries in sports. Sports Med. 2015; 45 9: 1325– 1337. [DOI] [PubMed] [Google Scholar]
- 32. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005; 33 4: 492– 501. [DOI] [PubMed] [Google Scholar]
- 33. Munro A, Herrington L, Comfort P. . Comparison of landing knee valgus angle between female basketball and football athletes: possible implications for anterior cruciate ligament and patellofemoral joint injury rates. Phys Ther Sport. 2012; 13 4: 259– 264. [DOI] [PubMed] [Google Scholar]
- 34. Anderson MK, Grier T, Canham-Chervak M, Bushman TT, Jones BH. . Occupation and other risk factors for injury among enlisted U.S. Army Soldiers. Public Health. 2015; 129 5: 531– 538. [DOI] [PubMed] [Google Scholar]
- 35. Evans KN, Kilcoyne KG, Dickens JF, et al. Predisposing risk factors for non-contact ACL injuries in military subjects. Knee Surg Sports Traumatol Arthrosc. 2012; 20 8: 1554– 1559. [DOI] [PubMed] [Google Scholar]
- 36. Taanila H, Suni JH, Kannus P, et al. Risk factors of acute and overuse musculoskeletal injuries among young conscripts: a population-based cohort study. BMC Musculoskelet Disord. 2015; 16: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. George SZ, Childs JD, Teyhen DS, et al. Predictors of occurrence and severity of first time low back pain episodes: findings from a military inception cohort. PLoS One. 2012; 7 2: e30597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dvorak J, Junge A, Chomiak J, et al. Risk factor analysis for injuries in football players. Possibilities for a prevention program. Am J Sports Med. 2000; 28 suppl 5: S69– S74. [DOI] [PubMed] [Google Scholar]
- 39. Teyhen DS, Shaffer SW, Butler RJ, et al. What risk factors are associated with musculoskeletal injury in US Army Rangers? A prospective prognostic study. Clin Orthop Relat Res. 2015; 473 9: 2948– 2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jones BH, Canham-Chervak M, Canada S, Mitchener TA, Moore S. . Medical surveillance of injuries in the U.S. Military descriptive epidemiology and recommendations for improvement. Am J Prev Med. 2010; 38 suppl 1: S42– S60. [DOI] [PubMed] [Google Scholar]
- 41. Jones BH, Knapik JJ. . Physical training and exercise-related injuries. Surveillance, research and injury prevention in military populations. Sports Med. 1999; 27 2: 111– 125. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


