Abstract
Objectives
We determined the seroprevalence of chikungunya virus (CHIKV) infection in the adult resident population in Singapore following local outbreaks of chikungunya fever (CHIKF) in 2008–2009.
Methods
Our cross-sectional study involved residual sera from 3,293 adults aged 18–79 years who had participated in the National Health Survey in 2010. Sera were tested for IgG antibodies against CHIKV and dengue virus (DENV) and neutralizing antibodies against CHIKV.
Results
The prevalence of CHIKV-neutralizing antibodies among Singapore residents aged 18–79 years was 1.9% (95% confidence interval: 1.4%– 2.3%). The CHIKV seroprevalence was highest in the elderly aged 70–79 years at 11.5%, followed by those aged 30–39 years at 3.1%. Men had significantly higher CHIKV seroprevalence than women (2.5% versus 1.3%, p = 0.01). Among the three main ethnic groups, Indians had the highest seroprevalence (3.5%) compared to Chinese (1.6%) and Malays (0.7%) (p = 0.02 and p = 0.01, respectively). Multivariable logistic regression identified adults aged 30–39 years and 70–79 years, men, those of Indian ethnicity and ethnic minority groups, and residence on ground floor of public and private housing apartments as factors that were significantly associated with a higher likelihood of exposure to CHIKV. The overall prevalence of anti-DENV IgG antibodies was 56.8% (95% CI: 55.1%– 58.5%), while 1.5% (95% CI: 1.1%– 2.0%) of adults possessed both neutralizing antibodies against CHIKV and IgG antibodies against DENV.
Conclusions
Singapore remains highly susceptible to CHIKV infection. There is a need to maintain a high degree of vigilance through disease surveillance and vector control. Findings from such serological study, when conducted on a regular periodic basis, could supplement surveillance to provide insights on CHIKV circulation in at-risk population.
Author summary
The prevalence of neutralizing antibodies against chikungunya virus (CHIKV) was low at 1.9% among resident adults in Singapore after local outbreaks in 2008–2009. Adults aged 30–39 years and 70–79 years, men, those of Indian ethnicity and ethnic minority groups, and residence on ground floor of public and private housing apartments were significantly associated with a higher likelihood of exposure to CHIKV.
Introduction
Chikungunya fever (CHIKF) has re-emerged as an important mosquito-borne disease caused by the Chikungunya virus (CHIKV), an Alphavirus belonging to the Togaviridae family [1], and transmitted by two main vectors, Aedes aegypti and Aedes albopictus in the urban cycle [2]. It is characterized by fever, joint pain, headache and myalgia [3]. The disease was first described during an outbreak in southern Tanzania in 1952 [3,4]. Since then, CHIKV outbreaks had been identified in countries in Africa, Asia, Europe, and the Indian and Pacific Oceans [5]. In late 2013, the first evidence of local CHIKV transmission in the Americas emerged when France reported two laboratory-confirmed autochthonous cases in the French part of the Caribbean island of St Martin [6]. Subsequently, local transmission has been identified in 45 countries or territories throughout the Americas, and more than 2.9 million suspected and confirmed cases and 296 deaths have been reported to the Pan American Health Organization from affected areas as of late July 2016 [5,7].
In Asia, CHIKV was first isolated in Bangkok, Thailand, in 1958, and outbreaks of CHIKF have been reported since the 1960s [8,9]. More recent reports of CHIKF outbreaks in Southeast Asia include those of Indonesia in 2001–2003 [10], Malaysia in 2006–2009 [11,12], Thailand in 2008–2009 [13] and Singapore in 2008–2009 [14]. While the earlier outbreaks were associated with the Asian genotype, the recent resurgence was associated with the East/Central/South African (ECSA) genotype [15], which had also caused the preceding outbreaks in the Indian Ocean islands in 2005 [16], India in 2006–2008 [17] and Sri Lanka in 2006–2007 [18–20].
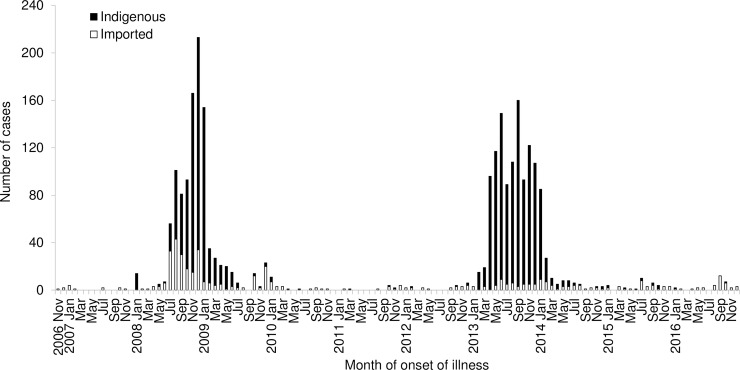
In Singapore, a tropical city-state, dengue is endemic with all four dengue virus (DENV) serotypes in circulation [21,22]. In response to the regional resurgence of CHIKF and to prevent its introduction into the country, an active laboratory-based surveillance system to detect CHIKV infection was established in late 2006 [23]. General practitioners were requested to consider Chikungunya as a diagnosis when dengue was suspected, and blood samples found to be negative for DENV by polymerase chain reaction (PCR) were routinely tested for CHIKV by PCR and serology. Sporadic imported cases were detected in November 2006. The first confirmed indigenous case infected with ECSA genotype was reported in a 13-year-old Taiwanese student who returned home from Singapore on November 20, 2006 [24]. A localized outbreak of 13 cases, which occurred in an Aedes aegypti predominant urban area, was rapidly contained from January to February 2008 (Fig 1) [25]. However, larger outbreaks subsequently occurred from July 2008 to January 2009 in other rural and suburban areas where Aedes albopictus was the predominant vector (Fig 1) [14]. The local transmission was attributed to the introduction of a mutated ECSA CHIKV with A226V substitution in the E1 gene [19,22]. E2-I211T substitution was also observed in CHIKV isolates from CHIKF-suspected sera used for full genome sequencing [19,20]. These two strains have been associated with efficient transmission by Aedes albopictus [26]. With aggressive vector control measures, the outbreak was finally brought under control in 2009. A total of 1,072 laboratory-confirmed CHIKF cases (260 imported and 812 indigenous) were reported between 2006 and 2009. In 2010, only 26 sporadic laboratory-confirmed cases were reported with 76.9% classified as imported cases [27].
Fig 1. Number of cases of chikungunya fever (CHIKF) notified by month of onset of illness, Singapore, 2006 to 2016.
There has been limited information on the seroepidemiology of CHIKV in Singapore and in many countries in South-east Asia. In a serosurvey conducted in Singapore among 531 healthy young adults aged 18–29 years in 2002–2003, two (0.4%) tested positive for IgG antibodies against CHIKV [28]. To assess the impact of the introduction into and spread of CHIKV in Singapore, we undertook a comprehensive serological study to determine its prevalence in the adult resident population.
Methods
Study population
We used residual sera from the National Health Survey (NHS) in 2010. The NHS 2010 was a population-based cross-sectional survey conducted by the Ministry of Health to determine the prevalence of major non-communicable diseases and their associated risk factors among Singapore adult residents (Singapore citizens and permanent residents) [29]. Selection of the general population was by a combination of disproportionate stratified sampling and systematic sampling. The survey fieldwork was carried out from 17 March to 13 June 2010 in six sites geographically distributed across the country. A total of 4,337 Singapore residents aged 18–79 years participated in the survey, giving a response rate of 57.7%. Only sera from NHS participants who had given informed consent to allow use of their residual sera for further research were included. Ethical approval was given by the Institutional Review Board Ethics Committee of the Health Promotion Board, Singapore (006/2010).
Residual sera from 3,293 (75.9%) of NHS respondents with sufficient amount leftover were tested. All samples analyzed were anonymized. The socio-demographic profile of these survey respondents in our study and the Singapore resident population aged 18–79 years was found to be similar [30].
Laboratory assays
All residual serum samples were first tested for IgG antibodies against CHIKV and DENV by anti-enzyme-linked immunosorbent assay (ELISA) using commercial test kits (EUROIMMUN, Germany) according to manufacturer's recommended procedure. Titres ≥ 20 RU/mL were considered to be reactive for both tests.
Samples tested positive for CHIKV IgG antibodies were further evaluated for CHIKV-specific neutralizing antibodies using plaque reduction neutralization tests (PRNT). Neutralizing activity of antibodies from human sera samples were tested in duplicates and analyzed by immunofluorescence-based cell infection assay in HEK 293T cells. CHIKV was mixed at a MOI of 10 with diluted (1:1000), heat-inactivated human sera and incubated for two hours at 37°C with gentle agitation (350 rpm). Virus-antibody mixtures were then added to HEK 293T cells seeded in 96-well plates and incubated for 1.5 hours at 37°C. Medium was removed, and cells were replenished with Dulbecco’s modified Eagle’s medium supplied with 10% FBS and incubated for six hours at 37°C. Live cells were determined by staining with a Live/Dead determination dye (Invitrogen) for 20 minutes according to the manufacturer’s protocol, before fixation with 4% paraformaldehyde and immunofluorescence staining. Cells were permeabilized with PBS containing 0.1% Tween-20, 0.1% Triton X-100, 3% BSA, 5% FBS and incubated for 30 minutes at room temperature. Cells were stained with mouse antibody recognizing CHIKV antigen [31] diluted in PBS for one hour at room temperature. This was followed by incubation with goat anti-mouse secondary antibody conjugated to Alexa Fluor 488 (Invitrogen) for one hour at room temperature. Data were acquired using MACSQuant Analyzer (Miltenyi Biotec) and results were analyzed by the FlowJo v10 software (FlowJo, LLC).
Percentage of infection was calculated according to the equation [% infection = 100 x (% infection from neutralization group/% infection from virus infection group)]. In this study, healthy donors lacking anti-CHIKV antibodies were included as negative controls, and infection ≤85% indicated presence of neutralizing activity to CHIKV [32,33]. Strong CHIKV-specific neutralizing activity was defined as ≤50% of 293T cells were infected by CHIKV post-incubation with the sera, moderate as >50% to 75% and weak as >75% to 85%.
Testing of residual sera for IgG antibodies and neutralizing antibodies against CHIKV was approved by National Healthcare Group's Domain Specific Review Board, Singapore (B/2015/01124).
Data analysis
To ensure that the characteristics of the NHS 2010 sample conformed to that of the general population, post-stratification weights were computed based on the age, gender, ethnic group and dwelling type attributes of the Singapore resident population. The overall sample weight was the product of weights for unequal probability of selection and non-response from the household enumeration exercise and survey fieldwork, respectively, and post-stratification weight.
The chi-square test or Fisher’s exact test, where appropriate, was used to test for group differences. Crude odds ratios (cOR) and adjusted odds ratios (aOR) with their 95% confidence intervals (CI) were estimated using univariable and multivariable logistic regression models. Listwise deletion was used for missing data of independent variables in the models. Multivariable logistic regression was used to determine independent factors associated with seropositivity, using forward stepwise selection based on maximum partial likelihood estimation with p < 0.20 for entry of variables and p < 0.05 for removal of variables. All p values reported were two-sided and statistical significance was taken as p < 0.05. Statistical analyses were performed using SPSS software, version 23 (Armonk, NY: IBM Corp., USA).
Results
CHIKV IgG was detected in 71 (2.2%, 95% CI: 1.7%– 2.7%) out of 3,293 survey respondents. Of these 71, 61 had CHIKV-specific neutralizing antibodies–the overall prevalence was 1.9% (95% CI: 1.4%– 2.3%).
Compared with seronegative adults, a higher proportion of those tested seropositive were of age 70–79 years, men, ethnic minority groups categorized under ‘others’, retirees, and resided on ground floor of public housing apartments, private flats and condominiums (Table 1).
Table 1. Distribution (%) of socio-demographic characteristics according to status of CHIKV-neutralizing antibodies of respondents from National Health Survey, Singapore, 2010.
| Socio-demographic characteristics | Serostatus of CHIKV-neutralizing antibodies | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| Seropositive | Seronegative | |||||||
| No. (%) | No. | (%) | No. | (%) | ||||
| All | 61 | (100) | 3,232 | (100) | 3,293 | (100) | ||
| Age group | ||||||||
| 18–29 | 3 | (4.9) | 661 | (20.5) | 664 | (20.2) | ||
| 30–39 | 21 | (34.4) | 661 | (20.5) | 682 | (20.7) | ||
| 40–49 | 6 | (9.8) | 724 | (22.4) | 730 | (22.2) | ||
| 50–59 | 7 | (11.5) | 677 | (20.9) | 684 | (20.8) | ||
| 60–69 | 2 | (3.3) | 339 | (10.5) | 341 | (10.3) | ||
| 70–79 | 22 | (36.1) | 170 | (5.3) | 192 | (5.8) | ||
| Gender | ||||||||
| Male | 36 | (59.0) | 1,384 | (42.8) | 1,420 | (43.1) | ||
| Female | 25 | (41.0) | 1,848 | (57.2) | 1,873 | (56.9) | ||
| Residency | ||||||||
| Singapore citizens | 47 | (77.0) | 2,783 | (86.3) | 2,830 | (85.9) | ||
| Permanent residents a | 14 | (23.0) | 443 | (13.7) | 457 | (13.9) | ||
| Ethnic Group | ||||||||
| Chinese | 39 | (63.9) | 2,393 | (74.0) | 2,432 | (73.8) | ||
| Malay | 3 | (4.9) | 417 | (12.9) | 420 | (12.8) | ||
| Indian | 11 | (18.0) | 305 | (9.4) | 316 | (9.6) | ||
| Others b | 8 | (13.1) | 117 | (3.6) | 125 | (3.8) | ||
| Main work status over last 12 months * | ||||||||
| Working | 31 | (50.8) | 2177 | (67.4) | 2,208 | (67.1) | ||
| Student / National service | 1 | (1.6) | 221 | (6.8) | 222 | (6.7) | ||
| Homemaker/housewife | 13 | (21.3) | 516 | (16.0) | 529 | (16.1) | ||
| Retired | 16 | (26.2) | 215 | (6.7) | 231 | (7.0) | ||
| Unemployed / Unknown | 0 | (0.0) | 96 | (3.0) | 96 | (2.9) | ||
| Type of residential premises | ||||||||
| Landed residential property c | 4 | (6.6) | 158 | (4.9) | 162 | (4.9) | ||
| Public housing apartment | 54 | (88.5) | 2729 | (84.4) | 2,783 | (84.5) | ||
| Private flat and condominium | 3 | (4.9) | 326 | (10.1) | 329 | (10.0) | ||
| Others d | 0 | (0.0) | 19 | (0.6) | 19 | (0.6) | ||
| Floor level of residential premises | ||||||||
| Landed residential property and others | 4 | (6.6) | 177 | (5.5) | 181 | (5.5) | ||
| Public housing apartment, private flat and condominium | ||||||||
| Ground | 6 | (9.8) | 97 | (3.0) | 103 | (3.1) | ||
| 2nd to 9th floor | 38 | (62.3) | 2022 | (62.6) | 2,060 | (62.6) | ||
| 10th floor or higher | 13 | (21.3) | 936 | (29.0) | 949 | (28.8) | ||
* Numbers do not add up to 3,293 due to non-response, such as refusals. There were missing data for 7 individuals tested negative for CHIKV-neutralizing antibodies.
a Singapore permanent residents refer to non-citizens who have been granted permanent residence in Singapore.
b Ethnic group of “Others” comprises all persons other than Chinese, Malays and Indians. They include Eurasians, Caucasians, Japanese, Filipino, Vietnamese, etc.
c Refers to bungalow/ detached house, semi-detached house and terrace house.
d Refers to temporary residences and dormitories.
The seroprevalence was highest in the elderly aged 70–79 years at 11.5%, followed by those aged 30–39 years at 3.1% (Table 2). Men had significantly higher seroprevalence than women (2.5% versus 1.3%, p = 0.01). Among the three main ethnic groups, those of Indian ethnicity had a higher seroprevalence (3.5%) compared to that of Chinese (1.6%) (p = 0.02) and Malays (0.7%) (p = 0.01). The seroprevalence was highest in the ethnic minority groups categorized as ‘others’ (6.4%), which comprises Eurasians, Caucasians, Japanese, Filipino, Vietnamese, etc. The seroprevalence was also highest among retirees at 6.9%. Adults staying on landed residential properties had the highest seroprevalence at 2.5%. Among the adults living in housing apartments, residents on the ground floor had higher seroprevalence than those residing on second or higher levels (p = 0.002).
Table 2. Seroprevalence (%) and odds ratios for presence of CHIKV-neutralizing antibodies according to socio-demographic characteristics of respondents from National Health Survey, Singapore, 2010.
| Socio-demographics | % sero-positive | Univariable analysis | Multivariable analysis* | |||||
|---|---|---|---|---|---|---|---|---|
| cOR | (95% CI) | p-value | aOR | (95% CI) | p-value | |||
| Age group (years) | <0.0005 | <0.0005 | ||||||
| 18–29 | 0.5 | 1.00 | Referent | 1.00 | Referent | |||
| 30–39 | 3.1 | 7.31 | (2.13–25.08) | 0.002 | 6.58 | (1.90–22.80) | 0.003 | |
| 40–49 | 0.8 | 1.93 | (0.48–7.83) | 0.359 | 1.89 | (0.46–7.73) | 0.374 | |
| 50–59 | 1.0 | 2.34 | (0.59–9.25) | 0.226 | 2.51 | (0.63–10.02) | 0.193 | |
| 60–69 | 0.6 | 1.53 | (0.27–8.72) | 0.633 | 1.68 | (0.29–9.68) | 0.561 | |
| 70–79 | 11.5 | 28.23 | (8.18–97.47) | <0.0005 | 34.28 | (9.74–120.73) | <0.0005 | |
| Gender | 0.011 | 0.008 | ||||||
| Male | 2.5 | 1.96 | (1.17–3.29) | 0.011 | 2.07 | (1.21–3.56) | 0.008 | |
| Female | 1.3 | 1.00 | Referent | 1.00 | Referent | |||
| Residency | 0.039 | |||||||
| Singapore citizen | 1.7 | 1.00 | Referent | |||||
| Permanent resident | 3.1 | 1.89 | (1.03–3.47) | 0.039 | ||||
| Ethnic Group | <0.0005 | 0.001 | ||||||
| Chinese | 1.6 | 1.00 | Referent | 1.00 | Referent | |||
| Malay | 0.7 | 0.39 | (0.11–1.35) | 0.136 | 0.36 | (0.10–1.28) | 0.114 | |
| Indian | 3.5 | 2.10 | (1.05–4.18) | 0.035 | 2.14 | (1.03–4.43) | 0.041 | |
| Others | 6.4 | 4.11 | (1.87–9.00) | <0.0005 | 4.02 | (1.70–9.51) | 0.002 | |
| Main work status over last 12 months | <0.0005 | |||||||
| Working | 1.4 | 1.00 | Referent | |||||
| Student / National serviceman | 0.5 | 0.18 | (0.01–2.48) | 0.200 | ||||
| Homemaker | 2.5 | 1.71 | (0.88–3.30) | 0.113 | ||||
| Retired | 6.9 | 5.19 | (2.80–9.64) | <0.0005 | ||||
| Unemployed / Unknown | 0.0 | 0.13 | (0.001–13.88) | 0.391 | ||||
| Type of residential premises | 0.558 | |||||||
| Landed residential property and others | 2.5 | 1.00 | Referent | |||||
| Public housing apartment | 1.9 | 0.86 | (0.30–2.53) | 0.788 | ||||
| Private flat and condominium | 0.9 | 0.36 | (0.07–1.76) | 0.207 | ||||
| Others | 0.0 | 0.00 | - | 0.998 | ||||
| Floor level of residential premises | 0.011 | 0.006 | ||||||
| Landed residential property | 2.2 | 1.52 | (0.47–4.92) | 0.488 | 1.49 | (0.44–5.09) | 0.521 | |
| Public and private apartment | ||||||||
| Ground | 5.8 | 4.99 | (1.89–13.15) | 0.001 | 6.55 | (2.30–18.72) | <0.0005 | |
| 2nd to 9th floor | 1.8 | 1.38 | (0.73–2.63) | 0.321 | 1.72 | (0.88–3.34) | 0.113 | |
| 10th floor or higher | 1.4 | 1.00 | Referent | 1.00 | Referent | |||
cOR, crude odds ratio; aOR: adjusted odds ratio; CI, confidence interval.
* Adjusted for age group, gender, ethnic group and floor level of residential premises.
In the multivariable regression model, independent factors significantly associated with seropositivity were age group, gender, ethnic group and floor level of residential premises (Table 2). Compared to the age group of 18–29 years, adults in the age group of 30–39 years [adjusted OR (aOR): 6.58, 95% CI 1.90–22.80] and those aged 70–79 years (aOR: 34.28, 95% CI 9.74–120.73) were more likely to be CHIKV seropositive (Table 2). Men were more likely to be seropositive compared to women with an aOR of 2.07 (95% CI 1.21–3.56). Compared to the Chinese, adults of Indian ethnicity (aOR: 2.14, 95% CI 1.03–4.43) and ethnic minority groups categorized as ‘others’ (aOR: 4.02, 95% CI 1.70–9.51) were significantly associated with a higher likelihood of exposure to CHIKV. Compared to adults residing on the 10th floor or higher levels of housing apartments, those who stayed on the ground floor were at higher odds of being CHIKV seropositive (aOR: 6.55, 95% CI 2.30–18.72).
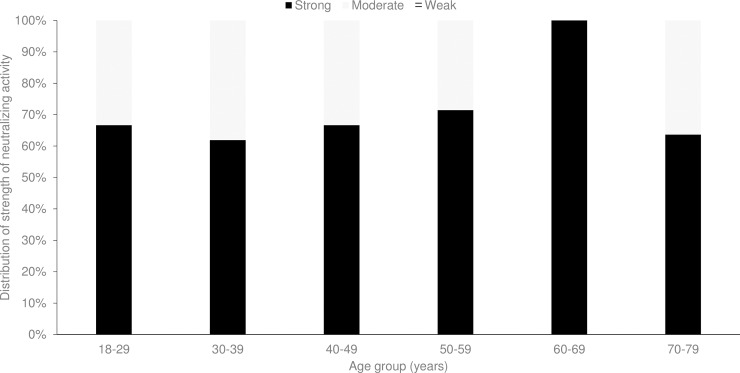
Among the 61 adults with neutralizing activity to CHIKV, 65.6% had strong neutralizing activity while the rest had moderate neutralizing activity and none had weak neutralizing activity. The proportion of CHIKV seropositive respondents having strong neutralizing activity ranged from 61.9% in the age group of 30–39 years to 100% in the age group of 60–69 years (Fig 2).
Fig 2. Distribution of strength of chikungunya virus (CHIKV)-specific neutralizing activity by age group among 61 seropositive respondents from National Health Survey, Singapore, 2010.
The overall prevalence of anti-DENV IgG antibodies was 56.8% (95% CI: 55.1%– 58.5%) [30]. A total of 51 adults (1.5%, 95% CI: 1.1%– 2.0%) had both neutralizing antibodies against CHIKV and IgG antibodies against DENV. Ten adults (0.3%) had neutralizing antibodies against CHIKV only, while 1,821 (55.3%) had IgG antibodies against DENV only.
Discussion
This was the first nationally representative study to describe the seroepidemiology of CHIKV and determine the magnitude of exposure in the Singapore resident population. Our study showed that about 1.9% of the adults in Singapore had likely been exposed to CHIKV, which was much lower than that of DENV with a prevalence of 56.8% in the same population studied [30]. This is not surprising as dengue has long been endemic in Singapore since the first outbreak reported in 1960 [34,35].
The CHIKV seroprevalence in adults 18–29 years of age (0.5%) after the 2008–2009 outbreaks was similar to that of a smaller study [28] in the same age group (0.4%) five years before these outbreaks (p = 0.84). However, the findings of these two studies may not be directly comparable due to differences in laboratory methods. In the earlier serological study in 2002–2003, IgG antibodies were detected using CHIKV-infected cells on teflon-coated glass slide as antigen (Ooi EE, Duke-National University of Singapore Medical School, Singapore, personal communication). Nevertheless, this showed that transmission of infection among young adults in the community was relatively low before and during the outbreak.
The post-outbreak seroprevalence in Singapore was lower compared to that of studies in some countries. In north-eastern Italy, the prevalence of IgG antibody against CHIKV by the indirect immunofluorescence method was 10.2% in 325 residents across all ages surveyed after an outbreak in 2007 [36]. In four Malaysian outbreak-free states, 5.9% in 945 healthy adults aged 35–74 years recruited in 2008 tested positive for CHIKV IgG by ELISA [37]. In Cebu City, the Philippines, 22.0% in 150 individuals across all ages were seropositive for CHIKV from a cross-sectional study using neutralization assays in 1973, while a prospective fever cohort study in 2012 found that 28.3% in 853 residents ≥6 months of age had PRNT titers at baseline indicating a history of CHIKV infection [38]. In central and southern Thailand, a study involving serum samples of 835 individuals aged between 6 months and 60 years obtained in 2014 and analyzed by commercial ELISA test kits found that 26.8% were seropositive for CHIKV, while 24.4% possessed both anti-CHIKV and anti-DENV IgG antibodies [39].
In our study, age group, gender and ethnic group were independently associated with CHIKV seropositivity in the multivariable logistic regression analysis. This generally corresponded with demographic characteristics of reported indigenous laboratory-confirmed cases of CHIKF among Singapore residents, with higher incidence rates in adults aged 30–39 years, men, and ethnic minority groups categorized as ‘others’. The incidence rate of indigenous cases was consistently highest in ethnic minority groups at 7.8 and 4.2 per 100,000 Singapore resident population, followed by Chinese at 6.1 and 3.1 per 100,000 population in 2008 and 2009, respectively [14]. In 2013, another outbreak year, ethnic minority groups also had the highest incidence rate of indigenous cases among Singapore residents (26.9 per 100,000) followed by Chinese (9.4 per 100,000) [40].
CHIKF was known to have swept through Southeast Asia in the 1960s and 1970s [8]. Even though CHIKV was not widely tested then, one patient was incidentally tested positive for CHIKV infection by complement fixation tests and neutralization tests in 1960 during an outbreak of dengue hemorrhagic fever in Singapore [41]. Considering that the vector for dengue and chikungunya is the same Aedes mosquitoes, and the Aedes house index (percentage of houses infested with Aedes larvae/pupae) was in the range of 30–50% at that time, it is likely that Singapore was not spared from disease transmission during the regional CHIKF outbreak, which would have contributed to the highest seroprevalence observed among adults aged 70–79 years. The lower proportion of CHIKV seropositive respondents in this age group having strong neutralizing activity (Fig 2) could be due in part to the decline in neutralizing antibody titers over time.
The gender difference for CHIK seroprevalence in our study had also been observed for dengue-specific IgG prevalence [30]. Higher CHIKV seroprevalence in men was also reported in serological studies in Malaysia [37] and the Indian Ocean island of Mayotte [42]. It has been postulated that the gender differential in the risk of CHIKV infection could be attributed to specific behaviour that results in greater exposure to bites by Aedes mosquitoes, and less tendency toward individual protection [36,42,43].
The ethnic difference in seroprevalence could be partly due to exposure during travel to highly endemic countries in the region. The high incidence among Indians corresponded with the highest rate of imported cases among Singapore residents travelling to India during the 2008–2009 outbreaks [14]. Phylogenetic data revealed that the first three reported episodes of local transmission in 2008 were due to three genetically distinct viruses of different geographic origins, suggesting that these episodes may be due to independent importations of CHIKV, most likely from India, Malaysia, and Sri Lanka [22].
The seroprevalence was highest among adults staying on landed residential properties. The incidence rate of indigenous cases of CHIKF and dengue has consistently been the highest for those living on landed residential properties, where there are more potential Aedes breeding habitats.
The proportion of adults aged 18–79 years with both neutralizing antibodies against CHIKV and IgG antibodies against DENV detected was low at 1.5%. Among the 1,872 samples tested positive for IgG antibodies against DENV in our serological study, 51 (2.7%) also had neutralizing antibodies against CHIKV. In Thailand, a seroprevalence study to evaluate evidence of past infection against CHIKV and DENV found that 79.2% (661/835) of individuals aged between 6 months and 60 years were DENV-seropositive, of whom 30.9% (204/661) also had IgG antibodies against CHIKV [39].
The first concurrent isolation of CHIKV and dengue type 2 virus (DENV-2) was from a single blood specimen taken from a patient in the acute phase of a dengue-like illness in southern India in 1964 [44]. Since then, a number of cases of co-infection with DENV and CHIKV have been detected in countries/territories such as Angola, Gabon, India, Madagascar, Malaysia, Myanmar, Nigeria, Saint Martin, Singapore, Sri Lanka, Tanzania, Thailand and Yemen; these constitute only 13 out of the 98 countries/territories where both chikungunya and dengue epidemic/endemic transmission have been reported based on literature search conducted until May 2015 for all relevant articles [45]. This included report of one case of imported co-infection of CHIKV and DENV-2 who had returned to Taiwan from Singapore in 2010 [46]. In Singapore, the active laboratory-based surveillance initiated in late 2006 was confined to DENV-negative blood samples for detection of CHIKV, hence cases co-infected with CHIKV and DENV could be potentially missed out.
The vectors for CHIKF and dengue, Aedes albopictus and Aedes aegypti, are distributed throughout Singapore. Aedes aegypti thrives in urban areas while Aedes albopictus inhabits in higher proportion in less urbanized areas with greenery in Singapore. A well-established nationwide Aedes surveillance and control programme incorporating source reduction, public education, community participation, and law enforcement, has been in place over the last four decades [47]. The overall Aedes house index has been maintained at around 1–2%. Despite the aggressive vector control efforts, CHIKF re-emerged in 2013 with a total of 1,059 laboratory-confirmed cases (95.5% indigenous and 4.5% imported), 1.5 times the 718 laboratory-confirmed cases reported in 2008 (Fig 1) [40]. The recurrence of the outbreak of CHIKF coincided with the largest dengue epidemic in the same year, indicating that similar factors may have facilitated the upsurge in the number of cases of these two mosquito-borne diseases in Singapore [48]. Phylogenetic analysis revealed that while locally transmitted CHIKV strains in 2013 formed a monophyletic group within the ECSA genotype, they possessed a signature of two synonymous substitutions (C639T + C816A) in E1 gene, making them a genetically distinct group [40]. These findings, together with the long-term absence of CHIKV transmission on an outbreak scale in Singapore, supported a viral introduction event prior to the establishment of indigenous transmission during the CHIKV outbreak in 2013. Outbreak strains possessed E1-A226V substitution, which further supported the potential role of Aedes albopictus as a predominant vector in CHIKV transmission in the 2013 outbreak. Imported virus strains belonged to the ECSA and Asian genotypes and did not possess E1-A226V substitution [40]. The ECSA strains all shared an Indian sub-continent ancestry. While imported strains with the ECSA genotype clustered separately from outbreak strains and were sporadically detected during 2009–2013, those with the Asian genotype were mainly from the Philippines and Indonesia [40].
There are a few limitations in our study. Some of the positive tests for CHIKV infection could have cross-reacted with other arboviruses such as O'nyong-nyong virus (ONNV), Ross River virus (RRV) and Barmah Forest virus (BFV) [33,49–51]. However, we have no data on the prevalence of other alphaviruses in our local population. There has been no or limited data comparing the relative sensitivity or specificity of the available CHIKV diagnostic assays [52]. The low seroprevalence in our study was consistent with sporadic detection of clinical cases. To establish past exposure to CHIKV, we used PRNTs which are deemed to be specific for alphaviruses and serve as the gold standard for confirmation of serological test results [53]. As our study was carried out based on residual sera and not specifically for CHIKV infection, clinical signs and travel history were not recorded.
The re-emergence and spread of CHIKF have been attributed to several factors, including vast immunologically naïve human populations, viral adaption, enhanced efficiency of mosquito transmission, drastic increase in international travel, as well as climate and environmental changes [9,48,54]. As Singapore remains highly susceptible to CHIKV infection, there is a need to maintain a high degree of vigilance through disease surveillance and vector control. Findings from such serological study, when conducted on a regular periodic basis, could supplement surveillance to provide insights on CHIKV circulation and profile of at-risk population.
Supporting information
(DOCX)
Data Availability
All relevant data are within the paper. Only staff working on the study are allowed access to the individual records in accordance to data governance and policy of the organization, so as to ensure that subject's privacy is not compromised.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Khan AH, Morita K, Parquet Mdel C Md, Hasebe F, Mathenge EG, Igarashi A. Complete nucleotide sequence of chikungunya virus and evidence for an internal polyadenylation site. J Gen Virol. 2002;83(12):3075–3084. [DOI] [PubMed] [Google Scholar]
- 2.Pialoux G, Gaüzère BA, Jauréguiberry S, Strobel M. Chikungunya, an epidemic arbovirosis. Lancet Infec Dis. 2007;7(5):319–327. [DOI] [PubMed] [Google Scholar]
- 3.Robinson MC. An epidemic of virus disease in Southern Province, Tanganyika territory, in 1952–1953. I. Clinical features. Trans R Soc Trop Med Hyg. 1955;49(1):28–32. [DOI] [PubMed] [Google Scholar]
- 4.Lumbsden WHR. An epidemic of virus disease in southern province of Tanganyika territory, in 1952–1953. II. General description and epidemiology. Trans R Soc Trop Med Hyg. 1955;49(1):33–55. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention, the United States of America. Chikungunya virus–geographical distribution. Available from: https://www.cdc.gov/chikungunya/geo/index.html. Last updated 12 May 2016. Cited 14 November 2017.
- 6.Cassadou S, Boucau S, Petit-Sinturel M, Huc P, Leparc-Goffart I, Ledrans M. Emergence of chikungunya fever on the French side of Saint Martin island, October to December 2013. Euro Surveill. 2014;19(13):20752 [DOI] [PubMed] [Google Scholar]
- 7.Yactayo S, Staples JE, Millot V, Cibrelus L, Ramon-Pardo P. Epidemiology of Chikungunya in the Americas. J Infect Dis. 2016;214(suppl 5):S441–S445. doi: 10.1093/infdis/jiw390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Regional Office for Southeast Asia. Chikungunya. Available from: http://www.searo.who.int/entity/emerging_diseases/topics/Chikungunya/en/index.html. Cited 15 June 2017.
- 9.Bhatia R, Narain JP. Re-emerging chikungunya fever: some lessons from Asia. Trop Med Int Health. 2009;14(8):940–946. doi: 10.1111/j.1365-3156.2009.02312.x [DOI] [PubMed] [Google Scholar]
- 10.Laras K, Sukri NC, Larasati RP, Bangs MJ, Kosim R, Djauzi, et al. Tracking the re-emergence of epidemic chikungunya virus in Indonesia. Trans R Soc Trop Med Hyg. 2005;99(2):128–141. [DOI] [PubMed] [Google Scholar]
- 11.Noridah O, Paranthaman V, Nayar SK, Masliza M, Ranjit K, Norizah I, et al. Outbreak of chikungunya due to virus of central/east African genotype in Malaysia. Med J Malaysia. 2007;62(4):323–328. [PubMed] [Google Scholar]
- 12.Chua KB. Epidemiology of chikungunya in Malaysia: 2006–2009. Med J Malaysia. 2010;65(4):277–282. [PubMed] [Google Scholar]
- 13.Thavara U, Tawatsin A, Pengsakul T, Bhakdeenuan P, Chanama S, Anantapreecha S, et al. Outbreak of chikungunya fever in Thailand and virus detection in field population of vector mosquitoes, Aedes aegypti (L.) and Aedes albopictus Skuse (Diptera: Culicidae). Southeast Asian J Trop Med Public Health. 2009;40(5):951–962. [PubMed] [Google Scholar]
- 14.Ho K, Ang LW, Tan BH, Tang CS, Ooi PL, James L, et al. Epidemiology and control of chikungunya fever in Singapore. J Infect. 2011;62(4):263–270. doi: 10.1016/j.jinf.2011.02.001 [DOI] [PubMed] [Google Scholar]
- 15.Powers AM, Logue CH. Changing patterns of chikungunya virus: re-emergence of a zoonotic arbovirus. J Gen Virol. 2007;88(9):2363–2377. [DOI] [PubMed] [Google Scholar]
- 16.Renault P, Solet J, Sissoko D, Balleydier E, Larrieu S, Filleul L, et al. A major epidemic of chikungunya virus infection on Reunion Island, France, 2005–2006. J Am Trop Med Hyg. 2007;77(4):727–731. [PubMed] [Google Scholar]
- 17.World Health Organization. Global Alert and Response: Chikungunya in India. Available from: http://www.who.int/csr/don/2006_10_17/en/index.html. Published 17 October 2006. Cited 15 June 2017.
- 18.Ministry of Healthcare and Nutrition, Epidemiology Unit, Sri Lanka. Chikungunya—An update. Weekly Epidemiological Report Sri Lanka. 2009;36:1–2. Available from: http://www.epid.gov.lk/web/pdf/wer_2009/vol_36_no_06_english.pdf. Cited 15 June 2017.
- 19.Hapuarachchi HC, Bandara KB, Sumanadasa SD, Hapugoda MD, Lai YL, Lee KS, et al. Re-emergence of Chikungunya virus in South-east Asia: virological evidence from Sri Lanka and Singapore. J Gen Virol. 2010;91(4):1067–1076. [DOI] [PubMed] [Google Scholar]
- 20.Ng LC, Hapuarachchi HC. Tracing the path of Chikungunya virus—evolution and adaptation. Infect Genet Evol. 2010;10(7):876–885. doi: 10.1016/j.meegid.2010.07.012 [DOI] [PubMed] [Google Scholar]
- 21.Lee KS, Lai YL, Lo S, Barkham T, Aw P, Ooi PL, et al. Dengue virus surveillance for early warning, Singapore. Emerg Infect Dis. 2010;16(5):847–949. doi: 10.3201/eid1605.091006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han HK, Ang LW, Tay J. Review of dengue serotype surveillance programme in Singapore. Epidemiological News Bulletin (Singapore). 2012;38(3):54–62. [Google Scholar]
- 23.Ng LC, Tan LK, Tan CH, Tan SS, Hapuarachchi HC, Pok KY, et al. Entomologic and virologic investigation of Chikungunya, Singapore. Emerg Infect Dis. 2009;15(8):1243–1249. doi: 10.3201/eid1508.081486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shu PY, Yang CF, Su CL, Chen CY, Chang SF, Tsai KH, et al. Two imported chikungunya cases, Taiwan. Emerg Infect Dis. 2008;14(8):1325–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ng LC. Singapore’s first chikungunya outbreak surveillance and response. Epidemiological News Bulletin (Singapore). 2008;34(2):25–28. [Google Scholar]
- 26.Tsetsarkin KA, Vanlandingham DL, McGee CE, Higgs S. A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 2007;3(12):e201 doi: 10.1371/journal.ppat.0030201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ministry of Health Singapore. Communicable Diseases Surveillance in Singapore 2010. Singapore: Ministry of Health; 2011. [Google Scholar]
- 28.Kita Y. Chikungunya virus disease. Epidemiological News Bulletin (Singapore). 2006;32(3):58–61. [Google Scholar]
- 29.Ministry of Health Singapore. National Health Survey 2010. Singapore: Ministry of Health; 2011. [Google Scholar]
- 30.Ang LW, Cutter J, James L, Goh KT. Seroepidemiology of dengue virus infection in the adult population in tropical Singapore. Epidemiol Infect. 2015;143(8):1585–1593. doi: 10.1017/S0950268814002507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Her Z, Malleret B, Chan M, Ong EK, Wong SC, Kwek DJ, et al. Active infection of human blood monocytes by Chikungunya virus triggers an innate immune response. J Immunol. 2010;184(10):5903–5913. doi: 10.4049/jimmunol.0904181 [DOI] [PubMed] [Google Scholar]
- 32.Kam YW, Simarmata D, Chow A, Her Z, Teng TS, Ong EK, et al. Early appearance of neutralizing immunoglobulin G3 antibodies is associated with chikungunya virus clearance and long-term clinical protection. J Infect Dis. 2012;205(7):1147–1154. doi: 10.1093/infdis/jis033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kam YW, Pok KY, Eng KE, Tan LK, Kaur S, Lee WW, et al. Sero-prevalence and cross-reactivity of chikungunya virus specific anti-E2EP3 antibodies in arbovirus-infected patients. PLoS Negl Trop Dis. 2015;9(1):e3445 doi: 10.1371/journal.pntd.0003445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chew A, Ho Y, Lee YK, Gwee AL, Khoo OT, Lim CH, et al. A haemorrhagic fever in Singapore. Lancet. 1961;277(7172):307–310. [DOI] [PubMed] [Google Scholar]
- 35.Lim KA, Chan YC, Phoon WO, Hanam E. Dengue-type viruses isolated in Singapore. Bull World Health Organ. 1964;30(2):227–240. [PMC free article] [PubMed] [Google Scholar]
- 36.Moro ML, Gagliotti C, Silvi G, Angelini R, Sambri V, Rezza G, et al. Chikungunya virus in North-Eastern Italy: a seroprevalence survey. Am J Trop Med Hyg. 2010;82(3):508–511. doi: 10.4269/ajtmh.2010.09-0322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Azami NA, Salleh SA, Shah SA, Neoh HM, Othman Z, Zakaria SZ, et al. Emergence of chikungunya seropositivity in healthy Malaysian adults residing in outbreak-free locations: chikungunya seroprevalence results from the Malaysian Cohort. BMC Infect Dis. 2013;13:67 doi: 10.1186/1471-2334-13-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salje H, Cauchemez S, Alera MT, Rodriguez-Barraquer I, Thaisomboonsuk B, Srikiatkhachorn A, et al. Reconstruction of 60 years of Chikungunya epidemiology in the Philippines demonstrates episodic and focal transmission. J Infect Dis. 2016;213(4):604–610. doi: 10.1093/infdis/jiv470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vongpunsawad S, Intharasongkroh D, Thongmee T, Poovorawan Y. Seroprevalence of antibodies to dengue and chikungunya viruses in Thailand. PLoS One. 2017;12(6):e0180560 doi: 10.1371/journal.pone.0180560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ministry of Health Singapore. Communicable Diseases Surveillance in Singapore 2013. Singapore: Ministry of Health; 2014. [Google Scholar]
- 41.Lim KA, Rudnick A, Chan YC. Recent studies of haemorrhagic fevers in Singapore. Singapore Med J. 1961;2:158–61. [PubMed] [Google Scholar]
- 42.Sissoko D, Moendandze A, Malvy D, Giry C, Ezzedine K, Solet JL, et al. Seroprevalence and risk factors of chikungunya virus infection in Mayotte, Indian Ocean, 2005–2006: a population-based survey. PLoS One. 2008;3(8):e3066 doi: 10.1371/journal.pone.0003066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakkhara P, Chongsuvivatwong V, Thammapalo S. Risk factors for symptomatic and asymptomatic chikungunya infection. Trans R Soc Trop Med Hyg. 2013;107(12):789–796. doi: 10.1093/trstmh/trt083 [DOI] [PubMed] [Google Scholar]
- 44.Myers RM, Carey DE. Concurrent isolation from patient of two arboviruses, Chikungunya and dengue type 2. Science. 1967;157:1307–1308. [DOI] [PubMed] [Google Scholar]
- 45.Furuya-Kanamori L, Liang S, Milinovich G, Magalhaes RJS, Clements ACA, Hu W, et al. Co-distribution and co-infection of chikungunya and dengue viruses. BMC Infect Dis. 2016;16:84 doi: 10.1186/s12879-016-1417-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chang SF, Su CL, Shu PY, Yang CF, Liao TL, Cheng CH, et al. Concurrent isolation of Chikungunya virus and Dengue virus from a patient with coinfection resulting from a trip to Singapore. J. Clin. Microbiol. 2010;48(12):4586–4589. doi: 10.1128/JCM.01228-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ooi EE, Goh KT, Gubler DJ. Dengue prevention and 35 years of vector control in Singapore. Emerg Infect Dis. 2006;12(6):887–93. doi: 10.3201/10.3201/eid1206.051210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oon LL, Ng LC. Chikungunya in Singapore—the Battle Continues. Ann Acad Med Singapore. 2014;43(6):325–327. [PubMed] [Google Scholar]
- 49.Blackburn NK, Besselaar TG, Gibson G. Antigenic relationship between chikungunya virus strains and o’nyong nyong virus using monoclonal antibodies. Res Virol. 1995;146(1):69–73. [DOI] [PubMed] [Google Scholar]
- 50.Chanas AC, Hubalek Z, Johnson BK, Simpson DI. A comparative study of O’nyong nyong virus with Chikungunya virus and plaque variants. Arch Virol. 1979;59(3):231–238. [DOI] [PubMed] [Google Scholar]
- 51.Mease L, Coldren R, Musila L, Prosser T, Ogolla F, Ofula V, et al. Seroprevalence and distribution of arboviral infections among rural Kenyan adults: A cross-sectional study. Virol J. 2011;8:371 doi: 10.1186/1743-422X-8-371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gibney KB, Fischer M, Prince HE, Kramer LD, St George K, Kosoy OL, et al. Chikungunya fever in the United States: a fifteen year review of cases. Clin Infect Dis. 2011;52(11):e121–126. [DOI] [PubMed] [Google Scholar]
- 53.Staples JE, Breiman RF, Powers AM. Chikungunya fever: an epidemiological review of a re-emerging infectious disease. Clin Infect Dis. 2009;49(6):942–948. doi: 10.1086/605496 [DOI] [PubMed] [Google Scholar]
- 54.Shragai T, Tesla B, Murdock C, Harrington LC. Zika and chikungunya: mosquito-borne viruses in a changing world. Ann N Y Acad Sci. 2017;1399(1):61–77. doi: 10.1111/nyas.13306 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper. Only staff working on the study are allowed access to the individual records in accordance to data governance and policy of the organization, so as to ensure that subject's privacy is not compromised.