Abstract
The expression and biological role of IL33 in colon cancer is poorly understood. In this study, we show that IL33 is expressed by vascular endothelial cells and tumor cells in the human colon cancer microenvironment. Administration of human IL33 and overexpression of murine IL33 enhanced human and murine colon cancer cell growth in vivo, respectively. IL33 stimulated cell sphere formation and prevented chemotherapy-induced tumor apoptosis. Mechanistically, IL33 activated core stem cell genes NANOG, NOTCH3, and OCT3/4 via the ST2 signaling pathway, and induced phosphorylation of c-Jun N terminal kinase (JNK) activation and enhanced binding of c-Jun to the promoters of the core stem cell genes. Moreover, IL33 recruited macrophages into the cancer microenvironment and stimulated them to produce prostaglandin E2, which supported colon cancer stemness and tumor growth. Clinically, tumor IL33 expression associated with poor survival in patients with metastatic colon cancer. Thus, IL33 dually targets tumor cells and macrophages and endows stem-like qualities to colon cancer cells to promote carcinogenesis. Collectively, our work reveals an immune-associated mechanism that extrinsically confers cancer cell stemness properties. Targeting the IL33 signaling pathway may offer an opportunity to treat patients with metastatic cancer.
Introduction
IL33 is a relatively new member of the IL1 family of cytokines. It is expressed by nonhematopoietic cells (1, 2). IL33 exerts its biological functions through binding and activation of its receptor ST2, a member in the Toll-like receptor superfamily (1, 2). Previous studies have demonstrated that IL33 promotes Th2 immune responses (2–5), regulatory T cell (Treg) development in the intestinal tissue (6), and virus-specific CD8+ T cell function (7) in different murine model systems. Interestingly, it has been reported that IL33 can protect against inflammation-associated atherosclerosis (8) or infection-induced tissue damage (9) and also promote biliary repair (10). Thus, IL33 has a variety of biological activities in different pathologic models. In line with this, the role of IL33 in tumor is under debate. IL33 can promote antitumor CD8+ T-cell responses in experimental mouse tumor models (11, 12). However, IL33 is associated with cancer metastasis in several cancer models (13–15) and facilitates oncogene-induced cholangiocarcinoma (16). Nonetheless, the potential immune-associated biological effect of IL33 on tumorigenesis is poorly understood. Furthermore, the biological role of IL33 in human primary tumor remains unknown.
Cancer cells are phenotypically and functionally heterogeneous in the tumor microenvironment. Cancer cells with stem cell properties may contribute to cancer metastasis and therapeutic resistance (17). In vivo, the stem cell properties are not autonomous to cancer cells, and recent evidence points to a level of external control from the microenvironment that defines the stem cell niche (18–23). It is now clear that cellular and molecular interactions within the tumor microenvironment regulate cancer stem cell properties and play an important role in tumor progression and metastasis (20–23). However, the expression profile of IL33 in human colon cancer and its potential effects on cancer stemness have not been explored in both mouse and human cancers.
In this work, we have investigated the role of IL33 in tumor-bearing mouse models and human primary colon cancer. We have found that IL33 enhances primary human and murine colon cancer cell growth in vivo, stimulates colon cancer cell sphere formation, and prevents chemotherapy-induced tumor apoptosis. Furthermore, we have demonstrated that IL33 activates core stem cell genes via c-Jun signaling activation in tumor cells and recruits and alters macrophages to enhance colon cancer carcinogenesis via PGE2 pathway. We have found that tumor IL33 expression is clinically important in patients with metastatic colon cancer.
Materials and Methods
Colon cancer patients and colon cancer tissues
Patients diagnosed with colon carcinomas were recruited in the study. All usage of human subjects in this study was approved by the local Institutional Review Board. Formalin-fixed, paraffin-embedded colon cancer tissue blocks (n = 176) and metastatic colon cancer tissue blocks (n = 63) were obtained during surgery (Supplementary Table S1). These patients underwent resection of colorectal cancer at the Second Department of General Surgery in the Medical University of Lublin (Lublin, Poland). After pathologic review, a tissue microarray (TMA; ref. 23) was constructed from the most representative area of paraffin-embedded colon cancer tissue. For each tumor, a minimum of two representative tumor areas were selected from a hematoxylin- and eosin-stained section of a donor block. Core cylinders (1 mm) were punched from each of these areas and deposited into a recipient paraffin block. Consecutive 6-μm–thick TMA sections were cut and placed on charged Poly-L-lysine–coated slides for IHC analyses.
Conventional IHC and multiplexed fluorescence staining
The conventional IHC staining (24) was performed on a DAKO Autostainer (DAKO) using DAKO LSAB+ and diaminobenzadine (DAB) as the chromogen. Serial sections of deparaffinized TMA sections were labeled with anti-human IL33 (Enzo; ALX-804-840-C100). Cores from several normal organ tissues were used as staining controls on each slide. The cores were analyzed for the expression of IL33 with an Aperio imaging system (Genetix). The specimens were digitalized with an automated platform (Aperio Technologies), ScanScope XT, and Spectrum Plus using TMA software version 9.1 scanning system. Multiplexed fluorescence staining was performed with Opal 4-plex staining system (PerkinElmer). Tissues were stained with anti-pan-cytokeratin (clone: AE1/AE3, DAKO), anti-CD31 (rabbit polyclonal, Abcam), anti-IL33 (clone: Nessy-1). The tissue slides were loaded into the Vectra slide scanner (PerkinElmer), imported, and analyzed with the relevant software (version 1.4; PerkinElmer). IL33 expression levels were assessed using H-score as we previously described (22, 23, 25). On the basis of the H-scores, we divided the samples into high (H-score > 15) and low (H-score ≤15) groups.
Tumor cell lines
Primary colon cancer cell lines (#1 and #2) were isolated and established from fresh human colon cancer tissues (23). Mouse MC38 colon cancer cell line was tested in 2011 (26) and stood the test of in vivo tumor formation in mice in 2015. Human HT-29 colon cancer cell line was bought from ATCC and did not undergo further testing.
Animal models
Six- to 8-week-old male C57BL/6 IL33 transgenic mice (27) and wild-type C57BL/6 male mice were used for mouse MC38 tumor experiments. Six- to 8-week-old male nude BALB/c mice (Beijing HFK Bioscience Co., Ltd) were used in the human colon cancer experiments. All experiments were conducted according to the Guidelines for the Care and Use of Laboratory Animals and approved by the Ethics Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (HUST, Wuhan, Hubei, China).
Sphere formation assay
The sphere assay was performed as described previously (22). Briefly, colon cancer cells were plated in ultralow attachment plates (Corning) in X-VIVO medium (Lonza) at a density of 1,000–5,000 viable cells/well. Colon cancer cells were treated with recombinant IL33 (PeproTech) or IL33-conditioned macrophages for different time points. The NFκB inhibitor, BAY11-7082; the P38 inhibitor, SB203580; the JNK inhibitor, SP600125; the MEK/ERK inhibitor, PD98059 (Cayman Chemicals), and the iNOS inhibitor, SMT (Aladdin), and anti-human ST2 antibody (R&D Systems) were added in sphere culture for 1 week. Spheres (>20 μm) were counted.
Quantitative real-time PCR analysis
The mRNA was obtained by TRIzol reagent (Invitrogen). Total RNA was reverse transcribed into complementary DNA (cDNA) using First Strand cDNA Synthesis kit (Fermentas) and oligo(dT) 18 primers (TSINGKE). Real-time RT-PCR was performed on an ABI StepOne Plus Detector System (Applied Biosystems) using SYBR Green I Assay (Takara). Relative gene expression levels (the amount of target, normalized to endogenous control gene) were calculated using the comparative Ct method formula 2−ΔΔCt. GAPDH was used as an endogenous control. The primers are listed in Supplementary Table S2.
Western blotting
Western blotting was performed with specific antibodies against human OCT3/4 (sc-5279), Sox-2 (sc-20088), NOTCH3 (sc-5279; Santa Cruz Biotechnology), NANOG (ab21624, Abcam), c-Jun (9165, Cell Signaling Technology), phosphorylated c-Jun (Ser63, 2361, Cell Signaling Technology), phosphorylated c-Jun (Ser73, 3270, Cell Signaling Technology), and β-actin (A5441, Sigma). Specific bands were detected with chemiluminescence assay using ECL detection reagents (Millipore).
Flow cytometry analysis
Tumor cells were first stained with anti-human ST2 antibody (bs-2382, Bioss), then washed and stained with secondary antibody. Immune cells were stained for macrophage and T-cell subset markers. Intracellular staining was used to determine the expression of Foxp3 and cytokines in T cells as described previously (28). Samples were acquired and analyzed on a FACSCalibur flow cytometer (BD Biosciences) or sorted by a high speed sorter (FACSAria II, BD Biosciences).
In vivo tumor formation and macrophage depletion
Primary human colon cancer cells were treated with IL33 and were subcutaneously injected into dorsal tissues of BALB/c nude mice. MC38 and B16F10 cells were subcutaneously injected into dorsal tissues of C57/BL6 IL33 transgenic and wild-type mice. Clodronate liposomes (Formumax) were used to deplete macrophages. Clodronate liposomes (200 μL) were intraperitoneally injected the day after tumor cell inoculation. Clodronate liposomes (100 μL) were intraperitoneally injected every 3 days. Tumor size was measured three times weekly with a Vernier caliper. Tumor volume was calculated on the basis of three perpendicular measurements (29). Tumor incidence and survival were monitored.
Macrophage migration
In vitro migration assay was performed in a Transwell system with a polycarbonate membrane of 6.5-mm diameter with a 3-μm pore size as described previously(29, 30). CD3−CD19−CD14+ macrophages were isolated and sorted from normal blood and fresh colon cancer tissues, and were subjected to the Transwell migration assay. Macrophages were added to the top chamber. IL33 (0–100 ng/mL, R&D Systems) or anti-ST2 (50 ng/mL, R&D Systems) was added to the bottom chamber. After an 8-hour incubation at 37°C, the phenotype and number of migrated cells in the bottom chambers were determined by FACS.
Lentiviral transduction
The lentiviral vectors including pGIPZ lentiviral vector encoding gene-specific shRNAs for c-Jun, IL1RAP, and scrambled shRNA were from the University of Michigan Vector Core. Primary human colon cancer cells were infected with the filtered lentiviral particles in the presence of polybrene and were selected in the presence of puromycin (2 μg/mL) for 1–2 weeks. The knockdown efficiency was determined by RT-PCR and Western blotting.
Chromatin immunoprecipitation
Chromatin immunoprecipitation (ChIP) analysis was performed as described previously (22). Briefly, protein and DNA complex was precipitated with specific antibody against c-Jun (9165, Cell Signaling Technology) and immunoglobulin G control (Millipore). Then, the DNA was suspended in Tris-EDTA buffer and subject to PCR amplification. The PCR products were resolved by gel electrophoresis. The specific primers are listed in Supplementary Table S2.
Tumor and macrophage coculture
Peripheral blood mononuclear cells (PBMC) were obtained from healthy donors. Normal CD3−CD19−CD14+ macrophages were isolated and sorted from PBMCs. Macrophages were treated with IL33 and/or Cox-2 inhibitor celecoxib for 48 hours. PGE2 was measured in the culture supernatants with an ELISA kit (R&D Systems). Primary colon cancer cells were cultured with these macrophages in sphere condition. Sphere numbers were recorded.
Statistical analysis
Unpaired Student t tests were used to compare two groups when appropriate. In cases of multiple groups, statistical analysis was performed through one-way ANOVA analysis with Turkey post test using the SPSS software (SPSS Inc.). Overall patient survival was defined from the date of diagnosis to disease-related death. Survival functions were estimated by Kaplan–Meier methods. Cox proportional hazards regression was performed to model survival after adjusting for gender, stage, grade, and tumor localization. The adequacy of the Cox regression model was assessed using graphical and numerical methods. All analyses were done using SAS 9.3 software. P < 0.05 was considered significant.
Study approval
The use of human samples and animal experiments in this study were conducted according to the principles of the Declaration of Helsinki and approved by the Institutional Review Boards of Tongji Medical College at Huazhong University of Science and Technology (Wuhan, Hubei, China), the University of Michigan School of Medicine (Ann Arbor, MI), and the Medical University in Lublin (Lublin, Poland). All participants gave written informed consent to participate in the study.
Results
IL33 promotes colon tumorigenesis
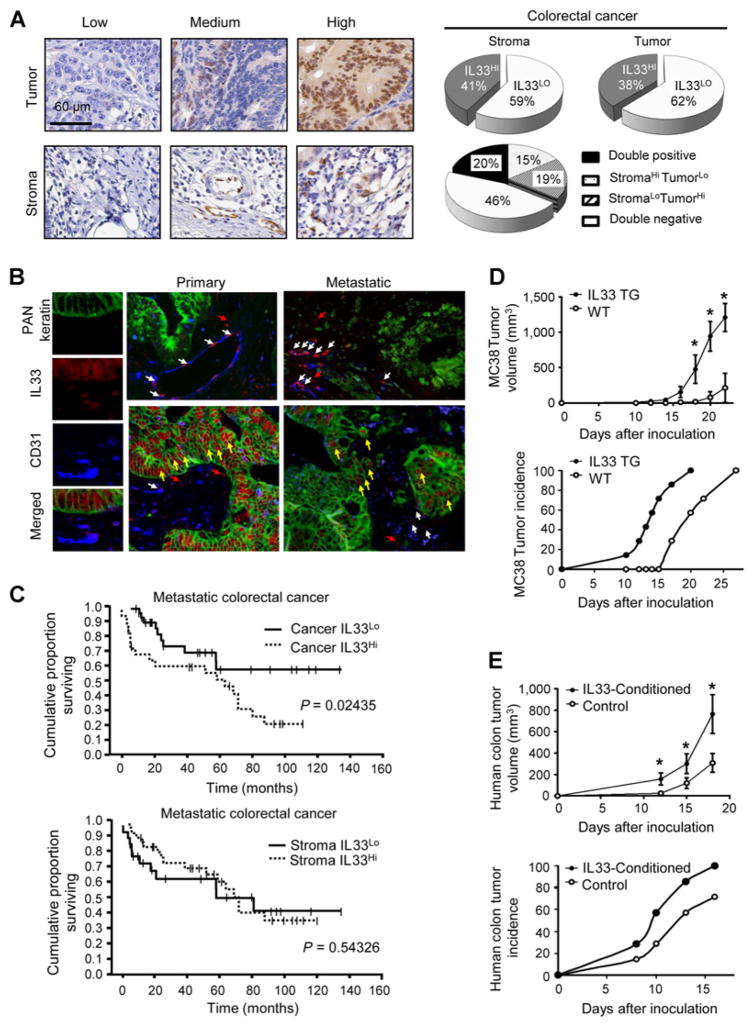
To determine the role of IL33 in colon cancer biology, we initially examined the expression of IL33 in 176 paraffin-fixed human primary colon cancer tissues (Supplementary Table S1). We found that different levels of IL33 were expressed in colon cancer cells and stromal cells in the colon cancer microenvironment (Fig. 1A). Thirty-eight percent of the samples expressed high levels of IL33 (IL33Hi) in colon cancer cells and 41% expressed high levels of IL33 (IL33Hi) in stromal cells (Fig. 1A). Twenty percent of patients were IL33Hi in both tumor cells and stromal cells. Fifteen percent expressed IL33Hi in stromal cells, but IL33Lo in tumor cells, whereas 19% expressed IL33Hi in tumor cells, but IL33Lo in stromal cells (Fig. 1A). Interestingly, when colon cancer cells were IL33+, the adjacent colon epithelial cells were IL33− (Supplementary Fig. S1A). We performed similar analysis in metastatic colon cancer. To specifically define and confirm our findings, we used a multiplexed immunophenotyping microscope to analyze the nature of IL33-expressing cells (Fig. 1B). As expected, PAN-Keratin+ tumor cells and CD31+ vascular endothelial cells expressed IL33 in primary and metastatic colon cancer tissues (Fig. 1B). Thus, IL33 is expressed in the human colon cancer microenvironment.
Figure 1.
IL33 promotes colon tumorigenesis. A, IL33 expression was detected with conventional immunohistochemical staining in the human colon cancer tissues. The representative images of IL33 expression in colon cancer cells (Tumor) and stromal cells (Stroma) are shown. Scale bar, 60 μm. The proportion of IL33 expression in colon cancer cells and stromal cells in the colon cancer microenvironment is depicted (right, pie charts). B, IL33 expression was detected with multiplexed fluorescence staining in the human colon cancer tissues. The representative images show the expression of IL33 (red), CD31 (blue), PAN-Keratin (green). White arrows, nuclear IL33 localization in CD31+ vascular endothelial cells; yellow arrows, nuclear IL33 localization in Keratin+ tumor cells; red arrows, nuclear IL33 localization in CD31−Keratin− stromal cells. C, The association between the survival in patients with metastatic colon cancer and IL33 protein levels in tumor cells (top) and stromal cells (bottom). Survival functions were estimated by Kaplan–Meier methods and analyzed based on the H-score for tumor or stromal cell IL33 expression. D, MC38 cells (106) were subcutaneously injected into wild-type (WT) or IL33 transgenic (IL33 TG) mice. The tumor volume (top) and tumor incidence (bottom) were monitored. Results are expressed as the mean of tumor volume ± SEM; n = 7. *, P < 0.05. E, Human primary colorectal cancer cells (#1) were cultured with or without rhIL33 (0.1 μg/mL) for 24 hours. The cells (106) were subcutaneously injected into nude mice. The tumor volume (top) and tumor incidence (bottom) were monitored. Results are expressed as the mean of tumor volume ± SEM; n = 7, *, P < 0.05.
To evaluate the clinical relevance of IL33, we quantified IL33 expression in patients with colon cancer and metastatic colon cancer (Supplementary Table S1). We found IL33Hi stromal cells were moderately increased, whereas IL33Hi tumor cells were slightly decreased (Fig. 1B; Supplementary Fig. S1B). Interestingly, tumor IL33 expression was negatively associated with survival in patients with metastatic colon cancer (Fig. 1C, top), but not in primary colon cancer (Supplementary Fig. S1C). The association between tumor IL33 expression and survival remained significant in multivariate analysis (Supplementary Table S3). Interestingly, stromal IL33 expression was not associated with patient survival in patients with colon cancer (Supplementary Fig. S1D) and metastatic colon cancer (Fig. 1C, bottom). Thus, tumor IL33 expression is clinically important in colon cancer progression.
To examine the in vivo role of IL33 in colon tumorigenesis, we inoculated MC38 mouse colon cancer cells into IL33 transgenic C57/BL6 (27) and wild-type C57/BL6 mice. We observed an increased MC38 tumor growth (Fig. 1D, top) and incidence (Fig. 1D, bottom) in IL33 transgenic mice compared with normal controls.
Next, we examined the role of IL33 in human primary colon cancer cells in vivo (23). Human primary colon cancer cells were inoculated into nude mice with or without human IL33 treatment. We observed that IL33 promoted human colon cancer growth (Fig. 1E, top) and incidence (Fig. 1E, bottom). Given the importance of cancer stem cells in cancer progression and metastasis (17), we analyzed the mRNA data in colon cancer in the TCGA Data Portal (https://gdc.cancer.gov/). Enrichment plots of GSEA showed that the gene signatures of cancer stem cells (Supplementary Fig. S1E) and metastasis (Supplementary Fig. S1F) were highly correlated with IL33 expression. Thus, our clinical, experimental, and bioinformatics data support the possibility that IL33 affects colon cancer stem-like properties and contributes to cancer metastasis.
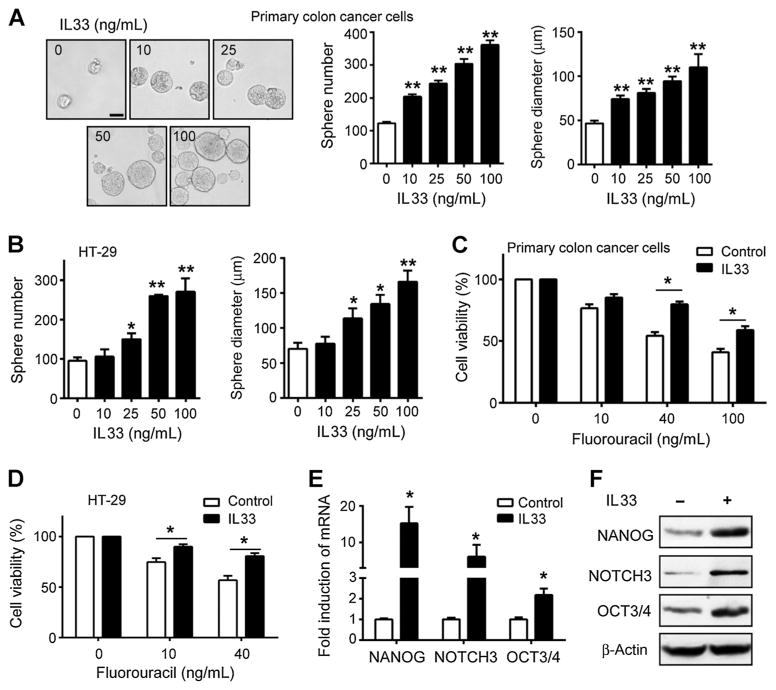
IL33 activates colon cancer stemness
We hypothesized that IL33 targets cancer stem cells and enhances tumorigenesis. To test this hypothesis, we examined the effects of IL33 on colon cancer cell sphere formation, 5-fluorouracil (5-FU) treatment efficacy, and activation on core stem cell genes. We found that IL33 induced sphere formation of human primary colon cancer cells (Fig. 2A) and of HT29 cells (Fig. 2B) in a dose-dependent manner. Furthermore, IL33 reduced primary colon cancer cell (Fig. 2C) and HT29 cell (Fig. 2D) apoptosis induced by 5-FU treatment. In line with this, IL33 activated several core stem cell gene transcripts (Fig. 2E; Supplementary Fig. S2A) and proteins (Fig. 2F; Supplementary Fig. S2B) including NANOG, NOTCH3, OCT3/4, and Lgr5, but not SOX2 and Musashi-1. Thus, IL33 activates core stem cell genes and supports colon cancer stemness.
Figure 2.
IL33 promotes colon cancer stemness. A and B, Effects of IL33 on colon cancer sphere formation. Primary colorectal cancer cells (A) and HT-29 cells (B; 4,000 cells) were subject to sphere assay for 7 days. IL33 was added on day 1 and 3. Representative images of spheres of primary colorectal cancer cells are shown (A, left). Scale bar, 50 μm. Results are expressed as the mean numbers of spheres ± SEM and the mean diameters of spheres ± SEM. Each column represents three independent experiments; n = 4; *, P < 0.05; **, P < 0.01. C and D, Effects of IL33 on colon cancer chemotherapy. Primary colorectal cancer cells (C) and HT-29 (D) were cultured with or without IL33 (100 ng/mL) for 24 hours and were subsequently exposed to 5-FU for 24 hours. The cell viability was determined by CCK-8 assay. Results are expressed as the mean ± SEM; n = 7; *, P < 0.05. E and F, Effects of IL33 on core stem cell gene expression in colon cancer cells. Primary colorectal cancer cells were treated with IL33 (100 ng/mL) for 24 hours. The levels of core stem cell gene transcripts (E) and proteins (F) were detected by real-time PCR and Western blotting, respectively. Each column represents three independent experiments. Results are expressed as the mean ± SEM; n = 4; *, P < 0.05.
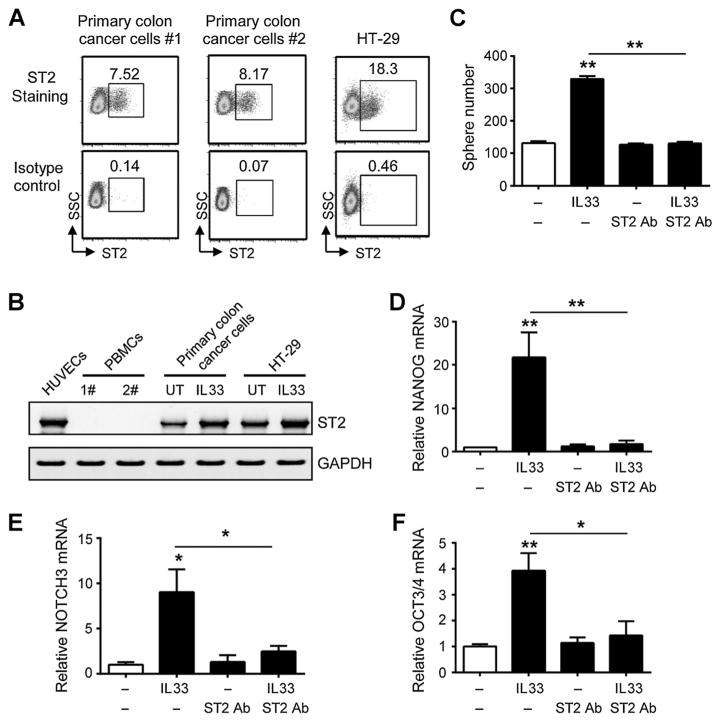
Colon cancer cells express functional IL33 receptor ST2
To further confirm the role of IL33 in colon cancer biology, we detected ST2 expression by flow cytometry analysis (Fig. 3A) and RT-PCR (Fig. 3B) in two primary colon cancer cells. IL33 treatment increased ST2 expression in colon cancer cells (Fig. 3B). Furthermore, neutralizing mAb against ST2 (anti-ST2 mAb) blocked the effects of IL33 in colon cancer sphere formation (Fig. 3C) and core stem cell gene activation (Fig. 3D–F).
Figure 3.
IL33 promotes colon cancer stemness via its receptor ST2. A, Expression of ST2 protein in colon cancer cells. Primary colon cancer cells (#1 and #2) and HT-29 cells were stained with specific rabbit anti-human ST2 Ab and R-PE–conjugated goat anti-rabbit IgG. The expression of ST2 was determined by flow cytometer analyzer and expressed as the percentage of ST2+ cells in total colon cancer cells. One of four experiments is shown. B, Expression of ST2 mRNA in colon cancer cells. ST2 mRNA expression was determined by RT-PCR in human umbilical vascular endothelial cells (HUVEC), peripheral blood mononuclear cells (PBMC), primary colon cancer cells, and HT-29 cells. Primary colon cancer cells and HT-29 cells were cultured with 100 ng/mL IL33 for 24 hours. One of three experiments is shown. C, Effects of anti-ST2 on the role of IL33-mediated colon cancer sphere formation. Primary colorectal cancer cells were subject to sphere assay. IL33 (100 ng/mL) and/or anti-ST2 antibody (1 μg/mL) were added in the sphere culture. Results are expressed as the mean ± SEM; n = 4; **, P < 0.01. D–F, Effects of anti-ST2 on the role of IL33-stimulated colon cancer stem cell gene expression. Primary colorectal cancer cells were cultured with IL33 (100 ng/mL) and/or anti-ST2 antibody (1 μg/mL) for 24 hours. The expression of NANOG (D), NOTCH3 (E), and OCT3/4 (F) transcripts were quantified by real-time PCR. Results are expressed as the mean ± SEM; n = 4; *, P < 0.05; **, P < 0.01.
IL1 receptor, IL1R accessory protein (IL1RAP), forms a heterodimeric receptor complex with ST2 and may mediate IL33 signaling (1, 2). Real-time PCR revealed IL1RAP expression in HT29 and primary colon cancer cells (Supplementary Fig. S3A). IL33 treatment had no effect on IL1RAP expression in these cells (Supplementary Fig. S3A). Knockdown of IL1RAP (Supplementary Fig. S3B) partially impaired IL33-induced sphere formation (Supplementary Fig. S3C). Thus, colon cancer cells express functional IL33 receptor signaling components.
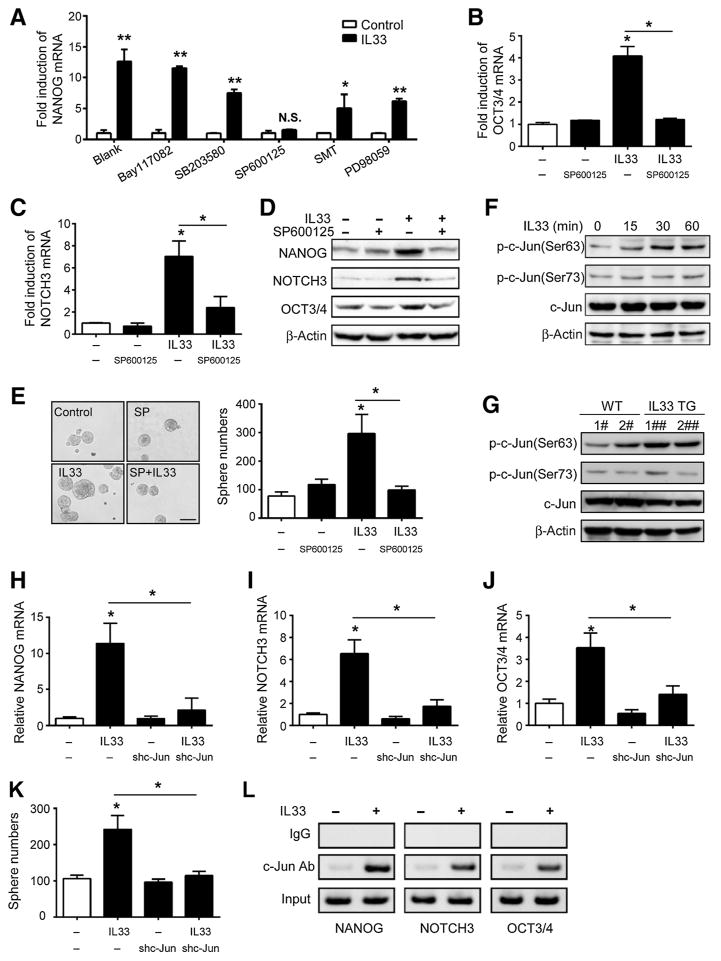
IL33 promotes colon cancer stemness via c-jun activation
Next, we explored the molecular mechanisms by which IL33 promotes colon cancer stemness. It has been reported that IL33 binds ST2 and activates ERK, c-Jun N-terminal kinase (JNK), and p38 MAPK or NFκB nuclear factors in murine cells (31). We examined the effect of several signaling inhibitors on IL33-mediated core stem cell gene expression. We used the NFκB inhibitor, BAY11-7082; the P38 inhibitor, SB203580; the JNK inhibitor, SP600125 (32); the iNOS inhibitor, SMT, and the MEK/ERK inhibitor, PD98059. We found that SP600125, SMT, and PD98059 resulted in moderate decrease of the IL33-stimulated NANOG expression (Fig. 4A). Treatment with JNK-specific inhibitor, SP600125, abolished the effects of IL33 on the transcripts (Fig. 4A–C) and proteins (Fig. 4D) of NANOG, NOTCH3 and OCT3/4. Furthermore, the JNK-specific inhibitor blocked the role of IL33 in colon cancer cell sphere formation (Fig. 4E). In line with this, we observed that IL33 induced c-Jun phosphorylation in colon cancer cells (Fig. 4F). We genetically knocked down c-Jun with specific shRNA (Supplementary Fig. S4A and S4B). We found that shc-Jun blocked stem cell core gene expression (Fig. 4H–J) and decreased colon cancer sphere numbers (Fig. 4K). We reasoned that the activated c-Jun might bind to the promoters of core stem cell gene promoters and subsequently stimulated their activation. In support of this possibility, P-Match prediction suggested several c-Jun–binding sites on the promoter regions of key core stem cell genes (Supplementary Fig. S4C–S4E). ChIP assay demonstrated that IL33 increased c-Jun binding to the promoters of NANOG, NOTCH3, and OCT3/4 (Fig. 4L). In addition, the activity of the NANOG promoter was upregulated by IL33 in colon cancer cells (Supplementary Fig. S4F). Thus, IL33 promotes colon cancer stemness via c-Jun activation.
Figure 4.
IL33 promotes colon cancer stemness via c-Jun activation. A–C, Quantification of NANOG (A), NOTCH3 (B), and OCT3/4 (C) transcripts in primary colorectal cancer cells that were treated with IL33 (100 ng/mL) for 24 hours in the presence of different signaling inhibitors (A) and the JNK inhibitor SP600125 (B and C). Each column represents three independent experiments. Results are expressed as the mean ± SEM; n = 4; *, P < 0.05; **, P < 0.01. D, Effects of the JNK inhibitor SP600125 on NANOG, NOTCH3, and OCT3/4 proteins in primary colorectal cancer cells. The cells were treated with IL33 (100 ng/mL) for 24 hours in the presence of SP600125 (10 μg/mL). NANOG, NOTCH3, and OCT3/4 proteins were detected by Western blotting. One of the three experiments is shown. E, Effects of SP600125 on colon cancer cell sphere formation. Primary colorectal cancer cells were subject to sphere assay in the presence of IL33 (100 ng/mL) and SP600125 (SP, 10 μg/mL). Representative images (left) and the mean numbers (right) of spheres are shown. Scale bar, 100 μm; n = 3; *, P < 0.05. F, Effects of IL33 on c-Jun in primary colorectal cancer cells. The cells were treated with IL33 (100 ng/mL) for different periods of time. The amount of phosphorylated c-Jun and c-Jun protein was detected by Western blotting. One of three experiments is shown. G, Phosphorylated c-Jun and c-Jun protein in MC38 tumors in vivo. MC38 tumor cells were obtained from wild-type and IL33 transgenic mice. The phosphorylated c-Jun and c-Jun proteins were detected by Western blotting. Representative data of two mice/group are shown. H–J, Effects of sh-c-Jun on IL33-stimulated stemness genes in primary colon cancer cells. Sh-c-Jun and scrambled vector expressing primary colorectal cancer cells were cultured with IL33 (100 ng/mL) for 24 hours. The mRNA levels of NANOG, NOTCH3, and OCT3/4 were detected by real-time PCR. Results are expressed as the mean ± SEM; n = 4; *, P < 0.05. K, The effects of sh-c-Jun on IL33-stimulated colon cancer cell sphere formation. Sh-c-Jun and scrambled vector expressing primary colorectal cancer cells were subject to sphere assay in the presence of IL33 (100 ng/mL). Sphere numbers were recorded. Results are expressed as the mean ± SEM; n = 4; *, P < 0.05. L, Effects of IL33 on the c-Jun occupancy in the promoters of core stem cell genes. Primary colorectal cancer cells were cultured with IL33 (100 ng/mL) for 24 hours. c-Jun-ChIP assay was performed. Rabbit IgG was used as a control. One of three experiments is shown.
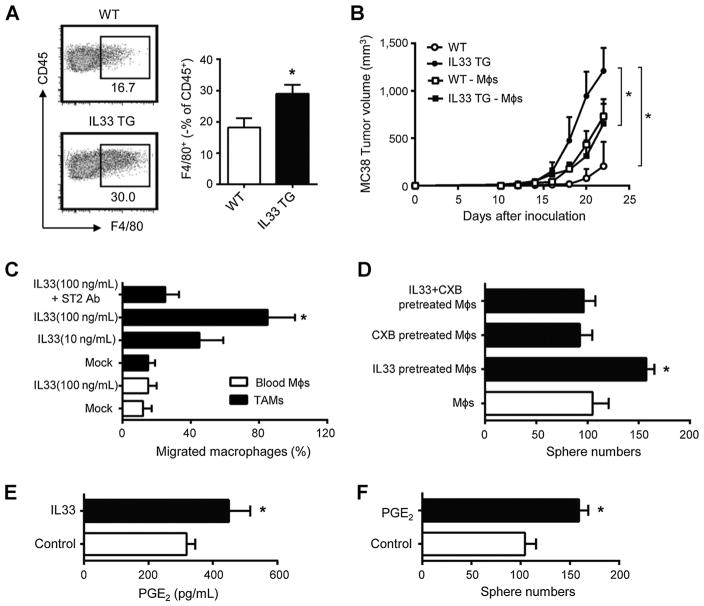
IL33 recruits macrophages and promotes colon cancer stemness
IL33 has been reported to regulate Th2 responses and intestinal regulatory T cells (2, 5, 6). In addition to the direct effect of IL33 on colon cancer cells, we explored whether immune elements are involved in the protumor effects of IL33 on MC38 colon cancer growth in IL33 transgenic mice (Fig. 1D). We found that the numbers of tumor-infiltrating CD4+Foxp3+ T cells (Supplementary Fig. S5A) and IFNγ+ T cells (Supplementary Fig. S5B) were similar in IL33 transgenic and control mice. Interestingly, there were more tumor-infiltrating F4/80+ macrophages in IL33 transgenic mice than control mice at the same time points after tumor inoculation (Fig. 5A). To avoid the potential effect of different tumor volumes on the quantification of tumor-infiltrating macrophages, we additionally analyzed tumor-infiltrating macrophages in the tumors from wild-type mice on day 22 and from IL33 transgenic mice on day 17. The tumor volumes were similar at these time points in these two groups (Supplementary Fig. S5C). Again, there were more tumor-infiltrating macrophages in IL33 transgenic mice than wild-type mice (Supplementary Fig. S5D). To explore the potential role of macrophages in tumor growth, we intraperitoneally injected clodronate liposomes to deplete macrophages. We found that macrophage depletion abolished the protumor effect of IL33 on MC38 growth in IL33 transgenic mice (Fig. 5B). Interestingly, macrophage depletion caused a moderate increase in tumor volume in wild-type mice (Fig. 5B), suggesting a potential immune protective role of macrophages in the absence of potent IL33 signal. In further support of a stimulatory role of IL33 in tumor stem cells, we detected higher levels of multiple core stem cell gene expression in IL33 transgenic mice than wild-type mice (Supplementary Fig. S5E–S5G). Macrophage depletion abolished this effect (Supplementary Fig. S5E–S5G). The data suggest that IL33 may facilitate macrophage tumor migration and function. In support of this possibility, we found that human colon cancer–associated macrophages expressed ST2 (Supplementary Fig. S5H). Human colon cancer–associated macrophages rather than normal macrophages (<15%) efficiently migrated toward IL33 (Fig. 5C). Addition of anti-IL33 receptor, ST2, blocked this migration (Fig. 5C). Furthermore, IL33 conditioned macrophages enhanced colon cancer sphere formation (Fig. 5D) and promoted the expression of NANOG and NOTCH3 in colon cancer cells (Supplementary Fig. S5I). Tumor-associated macrophages may express prostaglandin E2 (PGE2; refs. 33–36), and PGE2 stimulates bladder cancer stem cells (37). We hypothesized that IL33 promoted macrophage PGE2 production and in turn promoted colon cancer stemness. In support of this hypothesis, we detected higher levels of PGE2 in macrophages treated with IL33 compared with controls (Fig. 5E). The effect of IL33-conditioned macrophages on sphere formation was abolished by celecoxib (Fig. 5D), the COX-2–selective inhibitor, which blocks the inducible PGE2 production (38). Exogenous PGE2 promoted primary colorectal cancer sphere formation (Fig. 5F). IL33 had no effect on the expression of CD206 protein (Supplementary Fig. S5J) and IL10, arginase 1, and arginase 2 mRNA (Supplementary Fig. S5K) in macrophages. Altogether, the results indicate that IL33 can directly target tumor stemness program as well as facilitate macrophage recruitment and PGE2 expression, and, in turn, stimulates colon cancer stemness via PGE2 (Supplementary Fig. S5L).
Figure 5.
IL33 promotes colon cancer stemness via recruiting and stimulating macrophages. A, Tumor-associated macrophages in IL33 transgenic mice. MC38 cells (106) were subcutaneously injected into wild type and IL33 transgenic mice. Tumor-infiltrating immune cells were stained for CD45 and F4/80 and were analyzed by FACS. Results are shown as the mean of F4/80+ macrophages ± SEM in CD45+ cells in day 28 tumor tissues; n = 4; *, P < 0.05. B, Effects of macrophage depletion on MC38 tumor growth. MC38 cells (106) were subcutaneously injected into wild type or IL33 transgenic mice. Clodronate liposomes were intraperitoneally injected into the mice. Tumor growth was monitored. Results are expressed as the mean of tumor volume ± SEM. – Møs, macrophage depletion; n = 4 per group; *, P < 0.05. C, Macrophage migration toward IL33. CD14+CD45+ macrophages were enriched and sorted from colon cancer tissues or normal blood and subjected to the migration assay in the presence of IL33 and/or anti-ST2. Results are expressed as the mean percentage of migrated cells ± SEM. Møs, macrophages. TAM, tumor associated macrophages; n = 4; *, P < 0.05. D, Effects of IL33-treated macrophages on colon cancer sphere formation. Normal blood CD14+ macrophages were treated with IL33 in the presence or absence of celecoxib for 72 hours. Primary colon cancer cells were subject to sphere formation in the presence of these treated macrophages. Results are expressed as the mean of sphere numbers ± SEM; n = 4 per group; *, P < 0.05. E, Effects of IL33 on macrophage-derived PGE2.Normal blood CD14+ macrophages were treated with IL33 for 48 hours. PGE2 was detected in the culture supernatants by ELISA. Results are expressed as the mean values ± SEM; n = 4 per group; *, P < 0.05. F, Effects of PGE2 on colon cancer sphere formation. Primary colon cancer cells were subject to sphere assay in the presence of PGE2 (50 ng/mL). Results are expressed as the mean of sphere numbers ± SEM; n = 4 per group; *, P < 0.01.
Discussion
In this work, we demonstrate that IL33 promotes colon cancer stemness via two novel mechanisms: (i) IL33 directly targets cancer stem cell genes via c-Jun activation; (ii) IL33 facilitates macrophage recruitment and activation and stimulates cancer stem cell gene activation via PGE2.
IL33 has been implicated in Th2 responses (2, 5), intestinal Treg cell development (6), and virus-specific CD8+ T-cell responses (7) in murine models. However, the role of IL33 and the underlying molecular mechanisms in human colon cancer are poorly understood. We demonstrate that IL33 directly targets and stimulates primary and established colon cancer cell sphere formation, prevents 5-FU–induced tumor cell apoptosis, and activates core stem cell genes via c-Jun activation. High levels of IL33 are expressed in tumor stromal cells and/or tumor cells in the colon cancer microenvironment. Blockade of IL33 and ST2 signaling pathway abolishes the protumor activities of IL33. The protumor role of IL33 is validated in the in vivo models with IL33 overexpression and IL33 treatment. Thus, we reason that IL33 and ST2 signaling may be functionally operative in the cancer microenvironment in patients with colon cancer. In support of this notion, IL33 administration promotes tumorigenesis (10, 16), and soluble ST2 is correlated with tumor burden (14, 39). IL33 predicts poor prognosis, promotes ovarian cancer cell growth and metastasis (40), and activates tumor stroma to promote intestinal polyposis (41). Our bioinformatics and pathologic analyses have demonstrated that the expression of tumor IL33 is associated with poor survival in patients with metastatic colon cancer. Thus, we suggest that the IL33 and ST2 signaling pathways play a direct protumor role in patients with cancer.
Interestingly, the immunologic involvement of IL33 has been applied in several murine models (3, 7, 11). Although we cannot rule out the direct immunologic role of IL33 in T cells, we have found that T-cell subsets are numerically and functionally similar in the tumor microenvironment in the IL33 transgenic model and control mice. To our surprise, IL33 recruits macrophages, and stimulates their production of PGE2, and, in turn, macrophage-derived PGE2 stimulates colon cancer stem cell properties. In support of this notion, in vivo macrophage depletion abolishes the protumor effects of IL33 in vivo. Macrophages (21, 42) and macrophage-derived factors including PGE2 (37) contribute to cancer invasiveness and stemness. We add a novel layer of the mechanistic interaction between IL33 expressing cells, macrophages, and tumor cells, and provide previously unappreciated insight into IL33 biology.
Notably, our experiments have shown that macrophage depletion largely subverts the protumor role of IL33 in the established colon cancer model. It suggests that the direct effect of IL33 on tumor cells may potentially be predominant at an early stage of cancer progression, whereas the role of IL33-educated macrophages may be more effective at a late stage. Further kinetic studies will elucidate this possibility. Nonetheless, we suggest a dual mode of action of IL33 in the context of tumor. IL33 may initially engage ST2 in tumor cells, resulting in JNK activation and the expression of stem cell core genes. In addition, IL33 subsequently recruits macrophages into the tumor microenvironment and educates them to produce PGE2, which enhances and maintains tumor stemness. It is worth stressing that IL33 may exhibit multiple regulatory functions in vivo and control cancer immunologic and biological processes (2, 5–7). Furthermore, the plasticity of macrophages and multifaceted roles of PGE2 in cancer have been tested in tumor (38). Thus, the polyfunctional nature of IL33 may depend on its receptor expression profile and different cellular targets (tumor cells, macrophages, stromal cells, Tregs, and T cells). In addition, the release and activation of nuclear IL33 remain mechanistically unclear. The active form of IL33 may be released into the extracellular space after cell necrosis or mechanical injury (43). We have detected IL33 expression in tumor cells and tumor stromal cells in the human colon cancer microenvironment, and analyzed its clinical significance. However, in our human system, we are not able to thoroughly explore how IL33 is kinetically activated and released by different types of cells in the human tumor microenvironment, and how IL33 derived from different cells dynamically affects tumor immunity and biology. Nonetheless, our in vivo and in vitro experiments support a novel notion that IL33 may enhance colon cancer stemness by directly targeting tumor cells and by recruiting and activating macrophages. Our work suggests that targeting IL33 and ST2 signaling may be potentially applicable in treating patients with colon cancer.
Supplementary Material
Acknowledgments
We thank Dr. Zhanguo Li (Beijing University Medical School People’s Hospital, Beijing, China) and Dr. Lianfeng Zhang (Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China) for generously providing IL33 transgenic mice.
Grant Support
This work was supported by National Natural Science Foundation of China Programs 81272559, 81441077, 81502572, 81671904, and 81572866; the Major State Basic Research Development Program of China (973 Program, 2015CB554007); the Thousand Talents Program of China (L. Wang); the International Science and Technology Corporation Program of Chinese Ministry of Science and Technology S2014ZR0340; the Science and Technology Program of Chinese Ministry of Education 113044A; the Frontier Exploration Program of Huazhong University of Science and Technology 2015TS153; the Natural Science Foundation Program of Hubei Province 2015CFA049; the Hundred Talents Program of Hubei, China (Z. Wang); the Integrated Innovative Team for Major Human Diseases Program of Tongji Medical College, HUST (G. Wang); and the Research Fund of Public Welfare in Health Industry (No.201402015) from the Health and Family Plan Committee of China.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Note: Supplementary data for this article are available at Cancer Research Online (http://cancerres.aacrjournals.org/).
Authors’ Contributions
Conception and design: Y. Li, Z. Wang, W. Zou, L. Wang
Development of methodology: M. Fang, K. Huang, N. Nagarsheth, I. Kryczek, Z. Wang, L. Wang
Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): M. Fang, Y. Li, S. Qi, J. Zhang, W. Zgodzinski, M. Majewski, G. Wallner, S. Gozdz, P. Macek, A. Kowalik, M. Pasiarski, E. Grywalska, L. Vatan, N. Nagarsheth, Z. Wang
Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): M. Fang, Y. Li, K. Huang, S. Qi, J. Zhang, L. Zhao, I. Kryczek, Z. Wang, L. Wang
Writing, review, and/or revision of the manuscript: Y. Li, W. Zgodzinski, M. Majewski, G. Wallner, S. Gozdz, A. Kowalik, Z. Wang, W. Zou, L. Wang
Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): K. Huang, S. Qi, W. Zgodzinski, M. Majewski, P. Macek, M. Pasiarski, E. Grywalska, W. Li, Z. Wang, L. Wang
Study supervision: Z. Wang, L. Wang
References
- 1.Dinarello CA. An IL-1 family member requires caspase-1 processing and signals through the ST2 receptor. Immunity. 2005;23:461–2. doi: 10.1016/j.immuni.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Schmitz J, Owyang A, Oldham E, Song Y, Murphy E, McClanahan TK, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23:479–90. doi: 10.1016/j.immuni.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 3.Kurowska-Stolarska M, Kewin P, Murphy G, Russo RC, Stolarski B, Garcia CC, et al. IL-33 induces antigen-specific IL-5+ T cells and promotes allergic-induced airway inflammation independent of IL-4. J Immunol. 2008;181:4780–90. doi: 10.4049/jimmunol.181.7.4780. [DOI] [PubMed] [Google Scholar]
- 4.Savinko T, Matikainen S, Saarialho-Kere U, Lehto M, Wang G, Lehtimaki S, et al. IL-33 and ST2 in atopic dermatitis: expression profiles and modulation by triggering factors. J Invest Dermatol. 2012;132:1392–400. doi: 10.1038/jid.2011.446. [DOI] [PubMed] [Google Scholar]
- 5.Tordesillas L, Goswami R, Benede S, Grishina G, Dunkin D, Jarvinen KM, et al. Skin exposure promotes a Th2-dependent sensitization to peanut allergens. J Clin Invest. 2014;124:4965–75. doi: 10.1172/JCI75660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schiering C, Krausgruber T, Chomka A, Frohlich A, Adelmann K, Wohlfert EA, et al. The alarmin IL-33 promotes regulatory T-cell function in the intestine. Nature. 2014;513:564–8. doi: 10.1038/nature13577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonilla WV, Frohlich A, Senn K, Kallert S, Fernandez M, Johnson S, et al. The alarmin interleukin-33 drives protective antiviral CD8(+) T cell responses. Science. 2012;335:984–9. doi: 10.1126/science.1215418. [DOI] [PubMed] [Google Scholar]
- 8.Miller AM, Xu D, Asquith DL, Denby L, Li Y, Sattar N, et al. IL-33 reduces the development of atherosclerosis. J Exp Med. 2008;205:339–46. doi: 10.1084/jem.20071868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones LA, Roberts F, Nickdel MB, Brombacher F, McKenzie AN, Henriquez FL, et al. IL-33 receptor (T1/ST2) signalling is necessary to prevent the development of encephalitis in mice infected with Toxoplasma gondii. Eur J Immunol. 2010;40:426–36. doi: 10.1002/eji.200939705. [DOI] [PubMed] [Google Scholar]
- 10.Li J, Razumilava N, Gores GJ, Walters S, Mizuochi T, Mourya R, et al. Biliary repair and carcinogenesis are mediated by IL-33-dependent cholangiocyte proliferation. J Clin Invest. 2014;124:3241–51. doi: 10.1172/JCI73742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Villarreal DO, Wise MC, Walters JN, Reuschel EL, Choi MJ, Obeng-Adjei N, et al. Alarmin IL-33 acts as an immunoadjuvant to enhance antigen-specific tumor immunity. Cancer Res. 2014;74:1789–800. doi: 10.1158/0008-5472.CAN-13-2729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gao X, Wang X, Yang Q, Zhao X, Wen W, Li G, et al. Tumoral expression of IL-33 inhibits tumor growth and modifies the tumor microenvironment through CD8+ T and NK cells. J Immunol. 2015;194:438–45. doi: 10.4049/jimmunol.1401344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jovanovic IP, Pejnovic NN, Radosavljevic GD, Pantic JM, Milovanovic MZ, Arsenijevic NN, et al. Interleukin-33/ST2 axis promotes breast cancer growth and metastases by facilitating intratumoral accumulation of immunosuppressive and innate lymphoid cells. Int J Cancer. 2014;134:1669–82. doi: 10.1002/ijc.28481. [DOI] [PubMed] [Google Scholar]
- 14.Gillibert-Duplantier J, Duthey B, Sisirak V, Salaun D, Gargi T, Tredan O, et al. Gene expression profiling identifies sST2 as an effector of ErbB2-driven breast carcinoma cell motility, associated with metastasis. Oncogene. 2012;31:3516–24. doi: 10.1038/onc.2011.525. [DOI] [PubMed] [Google Scholar]
- 15.Liu X, Zhu L, Lu X, Bian H, Wu X, Yang W, et al. IL-33/ST2 pathway contributes to metastasis of human colorectal cancer. Biochem Biophys Res Commun. 2014;453:486–92. doi: 10.1016/j.bbrc.2014.09.106. [DOI] [PubMed] [Google Scholar]
- 16.Yamada D, Rizvi S, Razumilava N, Bronk SF, Davila JI, Champion MD, et al. IL-33 facilitates oncogene-induced cholangiocarcinoma in mice by an interleukin-6-sensitive mechanism. Hepatology. 2015;61:1627–42. doi: 10.1002/hep.27687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wicha MS, Liu S, Dontu G. Cancer stem cells: an old idea–a paradigm shift. Cancer Res. 2006;66:1883–90. doi: 10.1158/0008-5472.CAN-05-3153. [DOI] [PubMed] [Google Scholar]
- 18.Bendall SC, Stewart MH, Menendez P, George D, Vijayaragavan K, Werbowetski-Ogilvie T, et al. IGF and FGF cooperatively establish the regulatory stem cell niche of pluripotent human cells in vitro. Nature. 2007;448:1015–21. doi: 10.1038/nature06027. [DOI] [PubMed] [Google Scholar]
- 19.Scadden DT. The stem-cell niche as an entity of action. Nature. 2006;441:1075–9. doi: 10.1038/nature04957. [DOI] [PubMed] [Google Scholar]
- 20.Nagarsheth N, Peng D, Kryczek I, Wu K, Li W, Zhao E, et al. PRC2 epigenetically silences Th1-Type chemokines to suppress effector T-Cell trafficking in colon cancer. Cancer Res. 2016;76:275–82. doi: 10.1158/0008-5472.CAN-15-1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wan S, Zhao E, Kryczek I, Vatan L, Sadovskaya A, Ludema G, et al. Tumor-associated macrophages produce interleukin 6 and signal via STAT3 to promote expansion of human hepatocellular carcinoma stem cells. Gastroenterology. 2014;147:1393–404. doi: 10.1053/j.gastro.2014.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cui TX, Kryczek I, Zhao L, Zhao E, Kuick R, Roh MH, et al. Myeloid-derived suppressor cells enhance stemness of cancer cells by inducing micro-RNA101 and suppressing the corepressor CtBP2. Immunity. 2013;39:611–21. doi: 10.1016/j.immuni.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kryczek I, Lin Y, Nagarsheth N, Peng D, Zhao L, Zhao E, et al. IL-22(+)CD4 (+) T cells promote colorectal cancer stemness via STAT3 transcription factor activation and induction of the methyltransferase DOT1L. Immunity. 2014;40:772–84. doi: 10.1016/j.immuni.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moussion C, Ortega N, Girard JP. The IL-1-like cytokine IL-33 is constitutively expressed in the nucleus of endothelial cells and epithelial cells in vivo: a novel ‘alarmin’? PLoS One. 2008;3:e3331. doi: 10.1371/journal.pone.0003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peng D, Kryczek I, Nagarsheth N, Zhao L, Wei S, Wang W, et al. Epigenetic silencing of TH1-type chemokines shapes tumour immunity and immunotherapy. Nature. 2015;527:249–53. doi: 10.1038/nature15520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tanikawa T, Wilke CM, Kryczek I, Chen GY, Kao J, Nunez G, et al. Interleukin-10 ablation promotes tumor development, growth, and metastasis. Cancer Res. 2012;72:420–9. doi: 10.1158/0008-5472.CAN-10-4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhiguang X, Wei C, Steven R, Wei D, Wei Z, Rong M, et al. Over-expression of IL-33 leads to spontaneous pulmonary inflammation in mIL-33 transgenic mice. Immunol Lett. 2010;131:159–65. doi: 10.1016/j.imlet.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 28.Li Y, Fang M, Zhang J, Wang J, Song Y, Shi J, et al. Hydrogel dual delivered celecoxib and anti-PD-1 synergistically improve antitumor immunity. OncoImmunology. 2016;5:e1074374. doi: 10.1080/2162402X.2015.1074374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P, Mottram P, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10:942–9. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 30.Curiel TJ, Wei S, Dong H, Alvarez X, Cheng P, Mottram P, et al. Blockade of B7-H1 improves myeloid dendritic cell-mediated antitumor immunity. Nat Med. 2003;9:562–7. doi: 10.1038/nm863. [DOI] [PubMed] [Google Scholar]
- 31.Mirchandani AS, Salmond RJ, Liew FY. Interleukin-33 and the function of innate lymphoid cells. Trends Immunol. 2012;33:389–96. doi: 10.1016/j.it.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Bennett BL, Sasaki DT, Murray BW, O’Leary EC, Sakata ST, Xu W, et al. SP600125, an anthrapyrazolone inhibitor of Jun N-terminal kinase. Proc Natl Acad Sci U S A. 2001;98:13681–6. doi: 10.1073/pnas.251194298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hull MA, Booth JK, Tisbury A, Scott N, Bonifer C, Markham AF, et al. Cyclooxygenase 2 is up-regulated and localized to macrophages in the intestine of Min mice. Br J Cancer. 1999;79:1399–405. doi: 10.1038/sj.bjc.6690224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bamba H, Ota S, Kato A, Adachi A, Itoyama S, Matsuzaki F. High expression of cyclooxygenase-2 in macrophages of human colonic adenoma. Int J Cancer. 1999;83:470–5. doi: 10.1002/(sici)1097-0215(19991112)83:4<470::aid-ijc6>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 35.Williams CS, Tsujii M, Reese J, Dey SK, DuBois RN. Host cyclooxygenase-2 modulates carcinoma growth. J Clin Invest. 2000;105:1589–94. doi: 10.1172/JCI9621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feng Y, Renshaw S, Martin P. Live imaging of tumor initiation in zebrafish larvae reveals a trophic role for leukocyte-derived PGE2. Curr Biol. 2012;22:1253–9. doi: 10.1016/j.cub.2012.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kurtova AV, Xiao J, Mo Q, Pazhanisamy S, Krasnow R, Lerner SP, et al. Blocking PGE2-induced tumour repopulation abrogates bladder cancer chemoresistance. Nature. 2015;517:209–13. doi: 10.1038/nature14034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakanishi M, Rosenberg DW. Multifaceted roles of PGE2 in inflammation and cancer. Semin Immunopathol. 2013;35:123–37. doi: 10.1007/s00281-012-0342-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bergis D, Kassis V, Ranglack A, Koeberle V, Piiper A, Kronenberger B, et al. High serum levels of the interleukin-33 receptor soluble ST2 as a negative prognostic factor in hepatocellular carcinoma. Transl Oncol. 2013;6:311–8. doi: 10.1593/tlo.12418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tong X, Barbour M, Hou K, Gao C, Cao S, Zheng J, et al. Interleukin-33 predicts poor prognosis and promotes ovarian cancer cell growth and metastasis through regulating ERK and JNK signaling pathways. Mol Oncol. 2016;10:113–25. doi: 10.1016/j.molonc.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maywald RL, Doerner SK, Pastorelli L, De Salvo C, Benton SM, Dawson EP, et al. IL-33 activates tumor stroma to promote intestinal polyposis. Proc Natl Acad Sci U S A. 2015;112:E2487–96. doi: 10.1073/pnas.1422445112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu H, Clauser KR, Tam WL, Frose J, Ye X, Eaton EN, et al. A breast cancer stem cell niche supported by juxtacrine signalling from monocytes and macrophages. Nat Cell Biol. 2014;16:1105–17. doi: 10.1038/ncb3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cayrol C, Girard JP. The IL-1-like cytokine IL-33 is inactivated after maturation by caspase-1. Proc Natl Acad Sci U S A. 2009;106:9021–6. doi: 10.1073/pnas.0812690106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.