Abstract
Background
Depressive symptoms are common in older adults and associated with increased risk of cognitive impairment. Leisure activities are often promoted for individuals with mood symptoms but few studies compare the effects of different types of leisure activities on reducing depressive symptoms.
Methods
Data were analyzed from participants enrolled from 2008–2009 in the Mental Activity and eXercise (MAX) Trial, which examined the effects of physical plus mental activity over 12 weeks in inactive older adults with cognitive complaints. There were no significant differences between intervention groups on the primary outcome of cognitive function or the secondary outcome of depressive symptoms; therefore, all subjects were combined for the current analyses in which we examined changes in leisure activity engagement (Community Healthy Activities Model Program for Seniors), and changes in depressive symptoms (Geriatric Depression Scale) as a function of changes in leisure activity engagement from baseline to post-intervention.
Results
Participants’ mean age was 73.0 years, 61.6% were female, and 63.6% were non-Hispanic white. There was a significant change in total hours per week engaged in leisure activities from baseline (36.7 hours, SD=12.7) to post-intervention (40.4 hours, SD=15.7; paired t-test p=.02), and mean change in depressive symptoms was significantly inversely correlated with change in leisure activity hours such that increases in total leisure activity were associated with decreases in depressive symptoms (r = −.21, p = .04).
Conclusions
Increasing the total amount of leisure activity levels may help lower depressive symptoms in inactive older adults with cognitive complaints.
Keywords: Leisure Activities, Depressive Symptoms, Mild Cognitive Impairment, aging
INTRODUCTION
Background
Depression is common in older adults. It affects over 15% of people over the age of 65 who live independently in the community (Gallo and Lebowitzh, 1999) and generates an approximate cost of over $40 billion to treat annually (Roberts et al., 1997). When left untreated, depression in older adults can lead to increased risk of mortality (Blake et al., 2009).
Milder depressive symptoms, referred to as subthreshold depression, or the presence of clinical symptoms that do not meet the criteria for a formal mood disorder diagnosis, affect 5 million older adults nationwide (Adams et al., 2010). Depression is correlated with worse cognitive function in older adults (Christensen et al., 1997; Lyketsos et al., 2002), and studies have found that mild depressive symptoms are associated with an increased risk of developing mild cognitive impairment (Barnes et al., 2006; Cabeza et al., 2002), cognitive decline and dementia (Yaffe et al., 1999; Wilson et al., 2002).
Although anti-depressant medications and psychotherapeutic interventions can effectively treat depression in most adults, efficacy is less well established in the elderly, particularly those with cognitive impairment or dementia (Mottram et al., 2006; Wilson et al., 2008; Bains et al., 2002). Therefore, it is critical to investigate alternative approaches for reducing depressive symptoms in vulnerable elders.
Some randomized controlled trials (RCTs) have found that physical activity can be an effective treatment for depression and can slow cognitive decline in older adults with cognitive complaints (McAuley et al., 2000; Lautenschlager et al., 2008). However, most older adults are sedentary, and even those who exercise often have poor adherence (Rosenberg et al., 2010). Observational studies have found that engaging in other types of leisure activities such as utilizing senior centers to engage in social activities, working full time or volunteering are associated with lower depressive symptoms (Fulbright, 2010; Hao, 2008). However, few studies have examined the impact of other types of leisure activities such as those that involve social engagement such as volunteering or attending group meetings, or mental activities such as participating in board games or attending a lecture, as a method for reducing depressive symptoms. Furthermore, to our knowledge, none of these studies have focused specifically on individuals with cognitive complaints who have an increased risk of developing dementia (Busse et al., 2006). Additionally, it is unclear whether leisure activities, which have proven to be effective for healthy older adults, are equally effective in improving mood in older adults experiencing mild cognitive impairment.
We utilized data from the Mental Activity and eXercise (MAX) Trial to examine the impact of leisure activities on depressive symptoms in inactive elders with cognitive complaints. The primary analysis of the MAX Trial compared cognitive function between physical plus mental activity intervention groups (Barnes et al., 2013). Since no significant differences between intervention groups were found for the primary outcome of cognitive function or the secondary outcome of depressive symptoms, subjects were combined in the current analyses to examine changes in depressive symptoms as a function of changes in leisure activities levels from baseline to post-intervention.
METHODS
Participants
A detailed description of the MAX Trial procedures and the primary outcome of cognitive function have been previously published (Barnes et al., 2013). Briefly, the MAX Trial was conducted in the San Francisco Bay Area and participants were recruited through advertisement, medical clinics, or referral from friends or family members. Inclusion criteria were age ≥ 65 years, no/low levels of physical activity (<30 minutes/day, <2 times/week), self-report of a recent decline in memory or thinking, and fluency in English. Exclusion criteria were score lower than 19 on the Telephone Interview for Cognitive Status-modified (de Jager et al., 2003) or self-reported diagnosis of dementia or other major neurological disorder; current major psychiatric diagnosis (e.g., schizophrenia) with active symptoms; brain injury; medical condition that could be exacerbated by exercise (e.g., significant heart or lung disease, joint or hip pain); learning disorder; history of alcohol or substance abuse; severe hearing or visual impairment or tremor; dependence in any basic activities of daily living such as bathing, dressing, toileting, eating, transferring; or lack of physician approval to participate in physical activity. Subjects were enrolled from 2008 to 2009, and data collection was completed in 2009. Data analyses were performed from 2009–2014. The Committee on Human Research at the University of California, San Francisco, and the Research and Development Committee at the San Francisco Veterans Affairs Medical Center approved all study procedures. All subjects provided written informed consent prior to participation in the study.
Intervention
All MAX Trial participants participated in both physical and mental activity interventions (Barnes et al., 2013). The physical activity component involved group exercise (either aerobic or stretching/toning) at the local YMCA, and participants took classes for one hour per day, 3 days a week for twelve weeks. The mental activity component involved computer activities (either games provided by Posit Science Corporation (San Francisco, CA) or educational DVDs) that took place in the participant’s home, and participants were instructed to practice for one hour per day, 3 days a week for twelve weeks.
All participants completed physical and mental activity journals that were used to track weekly attendance and adherence to the interventions. Participants were also contacted by telephone on a biweekly basis throughout the study to monitor potential adverse events and to encourage participant’s compliance with the study procedures.
Measures
All measures were administered at baseline and after the 12-week intervention study period by trained research staff who also were blind to group assignment.
Depressive Symptoms
The 15-item version of the Geriatric Depression Scale (GDS) was used to assess depressive symptoms in this study. The original 30-item GDS is a commonly used measure of depression in older adults (Yesavage et al., 1982). The shorter 15-item version of this scale is widely used in community samples, as well as in medical clinics, and is considered a valid screening measure for detecting depression (Almeida and Almeida, 1999). Participants responded with either a Yes or No to questions such as “Do you feel pretty worthless the way you are now?” or “Do you feel happy most of the time?” Questions that endorsed negative symptoms of depression on this scale were given 1 point each and a sum score was calculated. A higher total sum score represented a higher level of depressive symptoms.
Leisure Activities
The Community Healthy Activities Model Program for Seniors (CHAMPS; Stewart et al., 2001), a 41-item questionnaire, was used to track the type, the number of times per week, and the total number of hours older adults spent performing leisure activities including the activities performed as part of the intervention study. For purposes of the current analyses, the 41 items were analyzed together to represent total number of hours engaged in leisure activities as a whole, as well as categorized as physical, mental or social types of activities. This categorization into three types of leisure activities was an exploratory method developed by the researchers to further identify if certain types of activities were more effective than other types at reducing depressive symptoms. The physical activity category consisted of thirty items, which were deemed physical in nature such as playing tennis, walking for exercise, or performing yoga or tai-chi. The mental activity category consisted of five items, which were considered solitary in nature and required mental acuity such as using a computer, playing a musical instrument, or reading. The social activity category consisted of six items which required participation by both the participant and at least one other party with a main purpose of engaging with others such as visiting with friends and family, going to a senior center, or performing volunteer work. Although some of these items may involve an element of another category (e.g., participation in yoga or tai-chi may include a social and/or mental component in addition to physical activity), the item was categorized based on the description of the activity itself and not its possible components.
Leisure activities were analyzed based on the total number of hours per week reported engaged in all activities, as well as number of hours per week engaged in the physical, social, and mental activities. The CHAMPS questionnaire initially captured this information categorically as “< 1 hour,” “1 – 2 ½ hours,” “3 – 4 ½ hours,” “5 – 6 ½ hours,” “7 – 8 ½ hours,” or “≥ 9 hours” total hours per week. We converted these categories into numeric values using the approximate mid-point of the category, i.e., 0.5, 1.75, 3.75, 5.75, 7.75 and 9.75 total hours per week, respectively. Subjects who did not engage in a given activity were assigned a value of 0. A summary score was created to reflect total hours of leisure activity by summing over all of the individual activities. Summary scores for total hours of physical, mental and social activity were created in a similar manner.
Other Measures
Demographic information was obtained on all subjects based on self-report and included age, gender, race, ethnicity, and education. These data were used for descriptive purposes.
Statistical Methods
Frequency distributions were utilized to describe demographic characteristics of the sample, depressive symptoms, and leisure activities endorsed by subjects. Paired t-tests were utilized to examine change in mean number of depressive symptoms and leisure activity hours from baseline to post-intervention. To determine whether changes in depressive symptoms were associated with changes in leisure activity hours, spearman correlation analyses were performed.
RESULTS
Ninety-nine older adults who completed assessments at baseline and post-intervention were included in this secondary analysis (Table 1). Subjects in our analytic sample had a mean age of 73.0 (SD=5.6) and 60.6% were female. The race/ethnicity distribution was as follows: 63.6% Non-Hispanic White, 16.2% Asian, 11.1% Hispanic or Latino, 7.1% African American, and 2.0% other/unknown. The mean years of education was 16.4 (SD=2.4) and mean global cognition score was 35.7 (SD=4.2).
Table 1.
Baseline Characteristics of 99 Study Participants
| Characteristic | |
|---|---|
| Age, mean (SD), years | 73 (5.6) |
| Gender, female, % | 60.6 |
| Education, mean (SD), years | 16.4 (2.4) |
| Race/ethnicity, Non-Hispanic White, % | 63.6 |
| Global cognition (TICS) score, mean (SD) | 35.7 (4.2) |
Notes: TICS = Telephone Interview for Cognitive Status-modified
The number of depressive symptoms did not change significantly from baseline (mean GDS score=1.7, SD=1.6) to post-intervention (mean GDS score=1.6, SD=1.8, paired t-test, p=0.30). However, there was a significant change in total hours per week subjects engaged in leisure activities from baseline (36.7 hours, SD=12.7) to post-intervention (40.4 hours, SD=15.8; paired t-test p=.01; Figure 1). Specifically, subjects engaged in more hours of physical activities post-intervention (14.2 hours, SD=8.3) compared to baseline (11.3 hours, SD=7.3; paired t-test, p =0.002) and more hours of mental activities post-intervention (19.8 hours, SD=6.2) compared to baseline (16.9 hours, SD=6.3; paired t-test, p <0.001), but there was no significant change in hours per week engaged in social activities from baseline (8.5 hours, SD=6.0) to post-intervention (9.0 hours (SD=6.9); paired t-test, p = .37).
Figure 1. Time spent on leisure activity engagement.
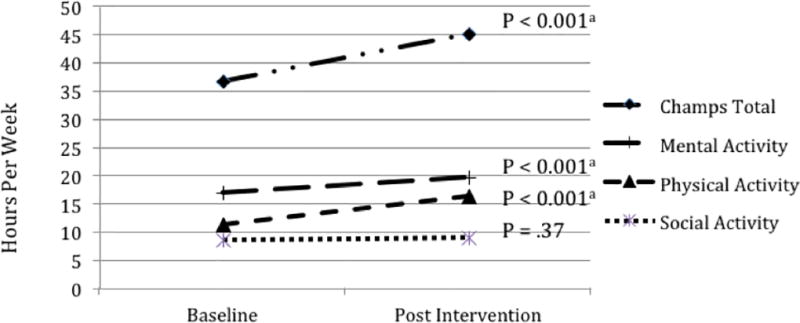
a Number of hours participants engaged in total leisure activities significantly changed from baseline to post-intervention (p < 0.001). Specifically, subjects engaged in more hours of physical activities post-intervention compared to baseline (p < 0.001), and more hours of mental activities post-intervention compared to baseline (p <0.001), but there was no significant change in hours per week engaged in social activities from baseline to post-intervention (p = 0.37).
Notes: CHAMPS Total = Community Healthy Activities Model Program for Seniors scale total hours per week subject engaged in leisure activities; Social Activity = CHAMPS number of hours per week subject engaged in social activities; Mental Activity = CHAMPS number of hours per week subject engaged in mental activities; Physical Activity = number of hours per week subject engaged in physical activities.
Based on Spearman correlation analysis used to assess the relationship between change in depressive symptoms and change in leisure activity hours from baseline to post-intervention, mean change in depressive symptoms was significantly inversely correlated with change in leisure activity hours overall such that increases in total leisure activity were associated with decreases in depressive symptoms (r = −.21, p = .04; Figure 2). However, correlations between changes in depressive symptoms and the specific leisure activity categories were not statistically significant: physical activities (r = −.14, p = .17), mental activities (r = −.15, p = .13), or social activities (r = −.13, p = .22). The correlation between changes in depressive symptoms and leisure activities appeared to be stronger in women (r = −.26, p = .04) than in men (r = −.13, p = 0.44), although these differences were not statistically significant (p-for-interaction = .28).
Figure 2. Relationship between depressive symptoms and leisure activities engagement.
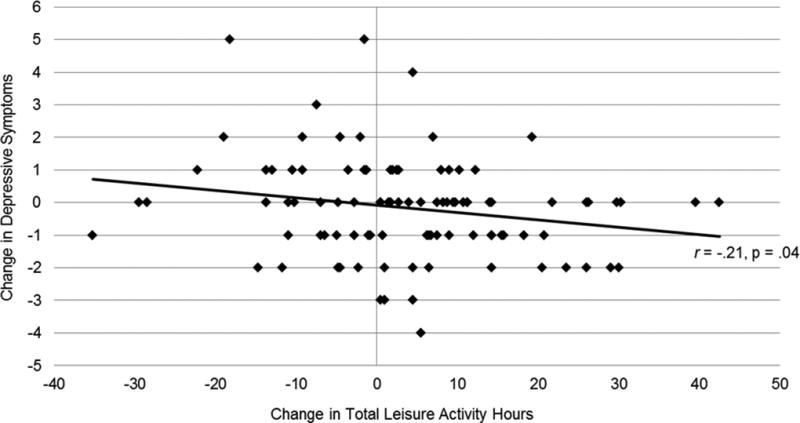
Mean change in depressive symptoms was significantly inversely correlated with change in leisure activity hours overall such that increases in total leisure activity were associated with decreases in depressive symptoms (r = −.21, p = .04).
Notes: Depressive symptoms were assessed with the 15-item Geriatric Depression Scale; Total hours engaged in leisure activities were assessed with the Community Healthy Activities Model Program for Seniors Scale.
DISCUSSION
Our results suggest that increasing engagement in total number of hours of leisure activity may reduce depressive symptoms in inactive older adults with mild cognitive complaints. A handful of studies have found that physical activity helps to reduce depressive symptoms in older adults diagnosed with a formal mood disorder, and improves cognitive performance (Babyak et al., 2000; Baker et al., 2010; Arfken et al., 1999). A meta-analysis of observational studies investigating mental and social activities found that these kinds of leisure interests also may protect against dementia (Fratiglioni et al., 2004). Although the total number of depressive symptoms was not significantly lower after our interventions, the total number of hours older adults dedicated to leisure activities significantly increased from baseline to post-intervention, and these increases in total hours engaged in leisure activity were significantly correlated with decreases in depressive symptoms. It is important to identify strategies for minimizing mild depressive symptoms because prior studies have found that even mild to moderate depressive symptoms are associated with greater risk of adverse health outcomes including cognitive impairment and mortality (Barnes et al., 2006; Arfken et al., 1999). Therefore, identifying the amount and exploring type of leisure activities that can aid in reducing mild depressive symptoms for older adults with cognitive complaints may serve as an important protective factor against developing more severe mood symptoms that could have further adverse effects on cognitive or physical health status.
In addition, a study found that as older adults age, engagement in physical activities decreased while engagement in passive social activities increased. These researchers suggested that reducing one’s investment in social activities might be linked to poor health and functioning and may increase depressive symptoms (Adams et al., 2010). Therefore, engaging in leisure activities with a social aspect, such as attending classes at a local YMCA, may offer opportunities for older adults experiencing mild depressive symptoms to interact or socialize with other people thus reducing depressive symptoms and promoting better health.
It is important to address limitations of this study. The primary objective of the intervention was to examine the effects of physical and mental activity on cognitive function in older adults with cognitive complaints, and individuals with current major depressive disorder were excluded. Therefore, only mild depressive symptoms were detected in this sample. Although research demonstrates that mild depressive symptoms can negatively impact an older adult’s life (Adams et al., 2010), it is important for future studies to consider how the amount of leisure activities (whether physical, mental or social) may be beneficial for individuals meeting formal criteria for a mood disorder diagnosis. Furthermore, a change in GDS score would have been difficult to detect in a sample of older adults reporting few depressive symptoms at baseline. Therefore, it is not surprising that a significant change in total GDS score was not observed. In addition, the education level of our subjects was high; future studies should determine whether our findings generalize to individuals with lower educational attainment.
In addition, a 12-week physical and mental activity intervention could be considered brief. It is unknown whether a longer intervention period would have demonstrated significant reduction in depressive symptoms or shown that a specific type of activity contributed more to a decrease in depressive symptoms. It is also not known whether the increases in leisure activities observed were maintained after the post intervention study assessment. Lastly, this study utilized correlation methods of analysis. Although we found a significant correlation between decreased depressive symptoms and increased leisure activity, we are unable to determine which came first; i.e., it is not clear whether an increase in activity lead to improved depressive symptoms, or an increase in depressive symptoms lead to less engagement in leisure activity. Therefore, studies that incorporate a longer intervention, a longer follow-up period, and causal analysis are warranted.
CONCLUSION
This study suggests that older adults with cognitive complaints who increase their total number of leisure activity hours may experience corresponding decreases in depressive symptoms. These results are important because the primary outcome of the intervention study was cognitive function, and our findings suggest that treatments geared toward improving cognitive functioning may also have an indirect effect on level of depressive symptoms. Furthermore, our results suggest that the amount of leisure activity may be more important than the specific type of leisure activity in reducing depressive symptoms. This is a valuable contribution that has not been well documented in the literature on older adults with cognitive complaints.
Acknowledgments
This study was supported in part by a Career Development Award from the National Institute on Aging (grant K01-AG024069), the Alzheimer’s Association (grant IIRG-06-27306), the University of California School of Medicine, the Institutes of Health/National Center for Research Resources/University of California, San Francisco – Clinical and Translational Science Institute (grant KL2 RR024130) and NIH grant 5-T32-AG000212.
Footnotes
No financial disclosures were reported by the authors of this paper
CONFLICT OF INTEREST
None.
DESCRIPTION OF AUTHORS ROLES
Dr. Barnes had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses. Study concept and design: Barnes, Yaffe, and Poelke. Acquisition: Barnes, Poelke. Analysis and interpretation of data: Barnes, Poelke, Byers, Sudore, Ventura, Yaffe. Drafting of the manuscript: Poelke, Ventura, and Barnes. Revision of the manuscript for important intellectual content: all.
References
- Adams KB, Roberts AR, Cole MB. Changes in activity and interest in the third and fourth age: Associations with health, functioning and depressive symptoms. Occupational Therapy International. 2010 doi: 10.1002/oti.304. [DOI] [PubMed] [Google Scholar]
- Almeida OP, Almeida SA. Short versions of the geriatric depression scale: a study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. International Journal of Geriatric Psychiatry. 1999;14:858–865. doi: 10.1002/(sici)1099-1166(199910)14:10<858::aid-gps35>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- Arfken CL, Lichtenberg PA, Tancer ME. Cognitive impairment and depression predict mortality in medically ill older adults. Journal of Gerontololgy A Biological Science Medical Science. 1999;54:M152–156. doi: 10.1093/gerona/54.3.m152. [DOI] [PubMed] [Google Scholar]
- Babyak M, Blumenthal JA, Herman S, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosomatic Medicine. 2000;62:633–638. doi: 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Bains J, Birks JS, Dening TR. The efficacy of antidepressants in the treatment of depression in dementia. Cochrane Database of Systematic Reviews (Online) 2002:CD003944. doi: 10.1002/14651858.CD003944. [DOI] [PubMed] [Google Scholar]
- Baker LD, Frank LL, Foster-Schubert K, et al. Effects of aerobic exercise on mild cognitive impairment: a controlled trial. Archives of Neurology. 2010;67:71–79. doi: 10.1001/archneurol.2009.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes DE, Alexopoulos GS, Lopez OL, et al. Depressive symptoms, vascular disease, and mild cognitive impairment: findings from the Cardiovascular Health Study. Archives of General Psychiatry. 2006;63:273–279. doi: 10.1001/archpsyc.63.3.273. [DOI] [PubMed] [Google Scholar]
- Barnes DE, Santos-Modesitt W, Poelke G, et al. The Mental Activity and eXercise (MAX) Trial: A Randomized Controlled Trial to Enhance Cognitive Function in Older Adults. JAMA Internal Medicine. 2013:1–8. doi: 10.1001/jamainternmed.2013.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake H, Mo P, Malik S, et al. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clinical Rehabilitation. 2009;23:873–887. doi: 10.1177/0269215509337449. [DOI] [PubMed] [Google Scholar]
- Busse A, Hensel A, Guhne U, et al. Mild cognitive impairment: long-term course of four clinical subtypes. Neurology. 2006;67:2176–2185. doi: 10.1212/01.wnl.0000249117.23318.e1. [DOI] [PubMed] [Google Scholar]
- Cabeza R, Anderson ND, Locantore JK, et al. Aging gracefully: compensatory brain activity in high-performing older adults. NeuroImage. 2002;17:1394–1402. doi: 10.1006/nimg.2002.1280. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths K, Mackinnon A, et al. A quantitative review of cognitive deficits in depression and Alzheimer-type dementia. Journal of the International Neuropsychology Society. 1997;3:631–651. [PubMed] [Google Scholar]
- de Jager CA, Budge MM, Clarke R. Utility of TICS-M for the assessment of cognitive function in older adults. International Journal of Geriatric Psychiatry. 2003;18:318–324. doi: 10.1002/gps.830. [DOI] [PubMed] [Google Scholar]
- Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurology. 2004;3:343–353. doi: 10.1016/S1474-4422(04)00767-7. [DOI] [PubMed] [Google Scholar]
- Fulbright SA. Rates of depression and participation in senior centre activities in community-dwelling older persons. Journal of Psychiatric and Mental Health Nursing. 2010;17:385–391. doi: 10.1111/j.1365-2850.2009.01535.x. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Lebowitz BD. The epidemiology of common late-life mental disorders in the community: themes for the new century. Psychiatric Services. 1999;50:1158–1166. doi: 10.1176/ps.50.9.1158. [DOI] [PubMed] [Google Scholar]
- Hao Y. Productive activities and psychological well-being among older adults. The Journals of Gerontology. 2008;63:S64–72. doi: 10.1093/geronb/63.2.s64. [DOI] [PubMed] [Google Scholar]
- Lautenschlager NT, Cox KL, Flicker L, et al. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. JAMA. 2008;300:1027–1037. doi: 10.1001/jama.300.9.1027. [DOI] [PubMed] [Google Scholar]
- Lyketsos CG, Lopez O, Jones B, et al. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA. 2002;288:1475–1483. doi: 10.1001/jama.288.12.1475. [DOI] [PubMed] [Google Scholar]
- McAuley E, Blissmer B, Marquez DX, et al. Social relations, physical activity, and well-being in older adults. Preventive Medicine. 2000;31:608–617. doi: 10.1006/pmed.2000.0740. [DOI] [PubMed] [Google Scholar]
- Mottram P, Wilson K, Strobl J. Antidepressants for depressed elderly. Cochrane Database of Systematic Reviews (Online) 2006:CD003491. doi: 10.1002/14651858.CD003491.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Kaplan GA, Shema SJ, et al. Prevalence and correlates of depression in an aging cohort: the Alameda County Study. The Journals of Gerontology. 1997;52:S252–258. doi: 10.1093/geronb/52b.5.s252. [DOI] [PubMed] [Google Scholar]
- Rosenberg D, Depp CA, Vahia IV, et al. Exergames for subsyndromal depression in older adults: a pilot study of a novel intervention. American Journal of Geriatric Psychiatry. 2010;18:221–226. doi: 10.1097/JGP.0b013e3181c534b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, King AC, et al. CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Medicine & Science In Sports & Exercise. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Wilson KC, Mottram PG, Vassilas CA. Psychotherapeutic treatments for older depressed people. Cochrane Database of Systematic Reviews (Online) 2008:CD004853. doi: 10.1002/14651858.CD004853.pub2. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Barnes LL, Mendes de Leon CF, et al. Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology. 2002;59:364–370. doi: 10.1212/wnl.59.3.364. [DOI] [PubMed] [Google Scholar]
- Yaffe K, Blackwell T, Gore R, et al. Depressive symptoms and cognitive decline in nondemented elderly women: a prospective study. Archives General Psychiatry. 1999;56:425–430. doi: 10.1001/archpsyc.56.5.425. [DOI] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research. 1982:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]


