Abstract
Although existing studies have linked high temperature to mortality in a small number of regions, less evidence is available on the variation in the associations between high temperature exposure and cause-specific mortality of multiple regions in China. Our study focused on the use of time series analysis to quantify the association between high temperature and different cause-specific mortalities for susceptible populations for 43 counties in China. Two-stage analyses adopting a distributed lag non-linear model (DLNM) and a meta-analysis allowed us to obtain county-specific estimates and national-scale pooled estimates of the nonlinear temperature-mortality relationship. We also considered different populations stratified by age and sex, causes of death, absolute and relative temperature patterns, and potential confounding from air pollutants. All of the observed cause-specific mortalities are significantly associated with higher temperature. The estimated effects of high temperature on mortality varied by spatial distribution and temperature patterns. Compared with the 90th percentile temperature, the overall relative risk (RR) at the 99th percentile temperature for non-accidental mortality is 1.105 (95%CI: 1.089, 1.122), for circulatory disease is 1.107 (95%CI: 1.081, 1.133), for respiratory disease is 1.095 (95%CI: 1.050, 1.142), for coronary heart disease is 1.073 (95%CI: 1.047, 1.099), for acute myocardial infarction is 1.072 (95%CI: 1.042, 1.104), and for stroke is 1.095 (95%CI: 1.052, 1.138). Based on our findings, we believe that heat-related health effect in China is a significant issue that requires more attention and allocation of existing resources.
Keywords: High temperature, Cause-specific mortality, Multi-counties, Stratified population, DLNM
1. Introduction
High ambient temperature is an important risk factor associated with health effects (Basu, 2009; Hajat and Kosatky, 2010). Many earlier studies have reported increased mortality caused by high temperature in various locations and climates within a single country (Barnett, 2007; Chen et al., 2013; Hajat et al., 2006). Recently, several eco-epidemiological studies have even estimated increased high temperature-induced mortality from multiple countries globally (Gasparrini et al., 2015; Guo et al., 2014). Conclusions from these studies indicate the need for multicenter research, as results from a wide range of locations could be used for the comparison and identification of heterogeneity in heat effects. In addition, studies including multiple locations are helpful for capturing spatial differences and support more target-specific policy making.
Unfortunately, most of the previous work in China on this subject have been focused on single cities. Due to the amplified effects of global climate change in recent years, there are growing public health impacts of exposure to high temperature in China (Committee of National Assessment Report on Climate Change, 2015). In recent years, there have been an increased number of multicenter studies in China. For example: the heat effect on stroke in eight Chinese cities (Chen et al., 2013), the health effect from high temperature on non-accidental mortality in seven Chinese cities (Zeng et al., 2016) and 17 large cities (Ma et al., 2014), and the investigation of heat effects in 66 communities (Huang et al., 2015). However, all of these studies focused on only a single outcome or a couple of main outcomes (cardiovascular and respiratory diseases) and mostly adopted a pre-specified temperature or temperature pattern such as extremely high or moderately high temperatures. Since high temperatures could cause a wide range of diseases through multiple biological pathways (Gasparrini et al., 2012), and different temperature patterns may present different regional estimates (Anderson and Bell, 2009; Medinaramón and Schwartz, 2007), many questions still remain to be explored. There is currently not enough evidence to characterize the cause-specific temperature-mortality relationship under different temperature patterns in multi-locations across China, a country with a wide range of climates, high mortality rates for sensitive diseases, and a highly diverse population. A better understanding of the relationship between high temperature and mortality of different causes and vulnerable subpopulations is not only critical to health risk evaluation in future research work but also to policy makers who plan suitable prevention and intervention strategies under a changing climate (Anderson and Bell, 2009).
This study analyzes cause-specific mortalities in 43 Chinese counties, controlling for different temperature patterns and using subpopulations stratified by age and sex. County-specific and national effects are estimated using advanced statistical modeling. We aim to examine how heat effects estimated for non-accidental and five specific causes of mortality vary across diverse climates in different parts of China.
2. Methods
2.1. Data collections
The study includes 43 counties from 12 cities (city is larger than county in China) distributed from northern to southern China (Fig. 1): Harbin (four counties), Beijing (seven counties), Shijiazhuang (four counties), Taiyuan (two counties), Xi’an (two counties), Nanjing (three counties), Suzhou (one county), Shanghai (seven counties), Chengdu (six counties), Wuhan (three counties), Guangzhou (three counties), and Shenzhen (one county). Of these cities, counties of Harbin are located in a mid-temperate zone; counties from Beijing, Shijiazhuang, Taiyuan, and Xi’an are located in a warm-temperate zone; all other counties are located in a subtropical zone. Daily data from 2013 to 2015 on mortality, weather conditions, and air pollution were obtained for each county (see Table A1 for county-specific information).
Fig. 1.
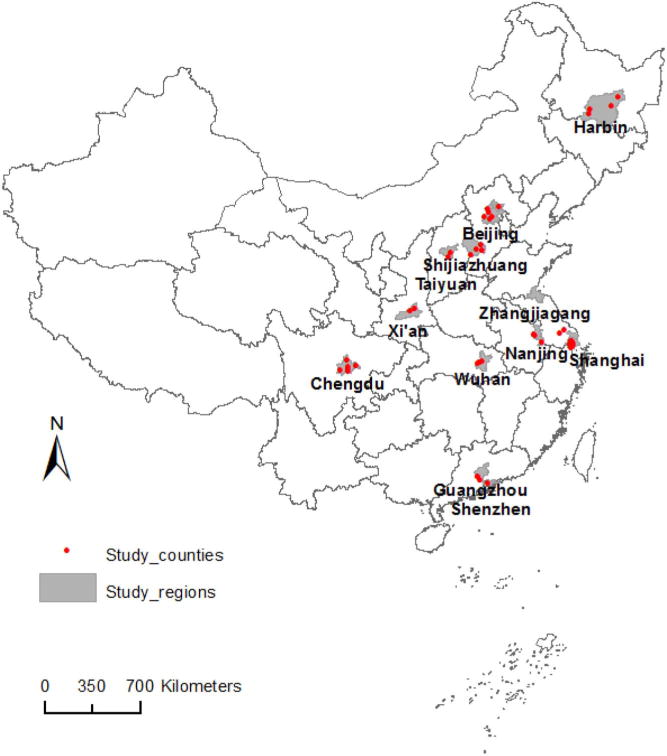
Geographical distribution of the studied counties.
Daily mortality data in each county were obtained from the national Death Surveillance Point System (DSPs). The International Classification of Diseases, 10th revision (ICD-10) code was adopted to classify non-accidental mortality (A00-R99) and cause-specific mortality for each county, including circulatory disease (Cir., I00-I99), respiratory disease (Resp., J00-J99), coronary heart disease (CHD, I20-I25), acute myocardial infarction (AMI, I21-I22), and stroke (I60-I64). Mortality counts of different causes were also stratified by sex and age (0–65 years, 65–74 years, over 74 years).
Weather data were obtained from the Chinese meteorological data sharing website and include daily mean temperature, maximum temperature, minimum temperature, and relative humidity in each county. We adopted daily mean temperature to evaluate the effects on mortality. We also examined the potential confounding effect from ambient air pollution on mortality by simultaneously considering daily county-specific concentrations of O3 and PM2.5 obtained from the National Air Pollution Monitoring System.
2.2. Data analysis
The temperature-mortality associations were investigated with a two-stage analysis using time series data from the 43 counties. The first-stage analysis at the county-level employed a quasi-Poisson regression model to estimate county-specific relative risks (RRs) for temperature-mortality associations, which included: a natural cubic spline of time with seven degrees of freedom (df) per year to exclude long-term and seasonal trends in mortality; a natural cubic spline of three df for a potential confounder of relative humidity; and days of the week as indicator variables controlling for variations among days of the week. The distributed lag nonlinear model (DLNM) is used to describe the nonlinear associations between high temperature and mortality and lag response (Gasparrini et al., 2015). Specifically, we estimated the temperature-effect with a maximum of a two-day lag, as previous studies indicated that the effects of high temperatures were generally of the short-term (Chen et al., 2013; Guo et al., 2014; Huang et al., 2014); in the cross-basis function, three internal knots were placed at the quartiles, and one internal knot was placed at equally spaced values on the log scale (Gasparrini et al., 2015).
Similar to earlier work in this area (Anderson and Bell, 2009; Chen et al., 2013), we estimated the RRs for the associations between high temperature and disease-specific mortality in each county by considering both relative and absolute temperature changes. For relative temperature changes, we quantified the relative risks (RRs) at extremely high temperatures (99th vs. 90th percentile temperature of each county’s temperature distribution) and moderately high temperatures (90th vs. 75th percentile temperature of each county). For absolute temperature changes, we quantified the RRs at 27.3 °C (90th percentile temperature of all counties) compared to 23.8 °C (75th percentile temperature of all counties). If the temperature data is out of this range, we would expand the temperature-mortality curve to obtain the RR estimates. These temperatures were all calculated based on the daily mean temperature.
In the second-stage analysis, a meta-analysis for each cause and subgroup population was used to obtain nationally pooled estimates of the high temperature effect on mortality, using county-specific effect estimates of different causes from the first-stage models.
We performed sensitivity analyses on the parameters of the county-specific model to test the robustness of the results. We examined models with the inclusion of same-day O3 and same-day PM2.5. In addition, we added a binary variable ‘holiday’ to control the potential influence from public holidays. We also tried extending the lag period to three days. R (version 3.2.2) was used to fit all the models in this study. The dlnm package for DLNMs is used for the first stage analysis, and the metafor package is used for the meta-analysis in the second stage analysis.
3. Results
Table 1 shows the summary of counts of mean daily non-accidental mortality, cause-specific mortality, mean daily temperatures, and air pollution levels in all 43 counties from 2013 to 2015. Mean values, 25th, 50th, 75th, and 95th percentiles for daily death counts as well as the total number of days with data are provided. The dataset includes 531,794 deaths, and the average daily number of non-accidental deaths is 11. Death counts for different causes vary significantly between counties. Further descriptions of the number of total deaths, mean daily temperatures, and air pollution levels in 43 counties are presented in Table A1. Average mortality and temperatures varied greatly by county, which captures the climatic and health variations in China to a large degree. The completeness of the data is good, with only 0.32% of missing data in total and cause-specific mortality, and 0.015% of missing data in daily temperature.
Table 1.
Descriptive data on number of mean daily deaths and exposure during 2013–2015.
| Days with data | Mean ± SD | P25 | P50 | P75 | P95 | |
|---|---|---|---|---|---|---|
| Non-accidental mortality | 46,933 | 11 ± 7 | 6 | 10 | 15 | 24 |
| Male | 46,933 | 6 ± 4 | 3 | 5 | 8 | 13 |
| Female | 46,933 | 6 ± 4 | 3 | 5 | 8 | 13 |
| 0–64 | 46,933 | 3 ± 2 | 1 | 2 | 4 | 7 |
| 65–74 | 46,933 | 2 ± 2 | 1 | 2 | 3 | 5 |
| ≥75 | 46,933 | 7 ± 5 | 3 | 6 | 9 | 16 |
| Cause-specific mortality | ||||||
| Circulatory disease | 46,933 | 5 ± 3 | 2 | 4 | 7 | 12 |
| Respiratory disease | 46,933 | 1 ± 2 | 0 | 1 | 2 | 5 |
| Coronary heart disease | 46,933 | 2 ± 2 | 1 | 1 | 3 | 6 |
| Acute myocardial infarction | 46,933 | 1 ± 1 | 0 | 1 | 1 | 3 |
| Stroke | 46,933 | 2 ± 2 | 0 | 1 | 2 | 4 |
| Meteorological and air pollution data | ||||||
| Daily temperature (°C) | 47,078 | 15.2 ± 10.73 | 7.40 | 17.30 | 23.80 | 29.00 |
| PM2.5(μg/m3) | 44,112 | 72.96 ± 62.4 | 33.20 | 54.86 | 91.52 | 190.25 |
| O3(μg/m3) | 43,625 | 56.39 ± 38.15 | 27.40 | 50.08 | 77.92 | 123.39 |
Fig. 2 shows RRs of non-accidental mortality at lags 0–2 days in each county, with the corresponding relative extremely high temperature (99th vs. 90th), relative moderately high temperature (90th vs. 75th), and absolute temperature (27.3 °C vs. 23.8 °C). In Fig. 2, higher RRs of extremely high temperature show a stronger effect on non-accidental mortality in each county compared to moderately high temperature and absolute temperature. RRs associated with relative moderately high temperature and absolute temperature were similar. Furthermore, RRs of counties in Fig. 2 are ordered by latitude of each corresponding county, so a geographical trend of the heat effects is presented. The RRs are highest in counties in the middle latitudes, compared to counties located in colder areas (higher latitudes) as well as in hotter areas (lower latitudes). However, this trend was not observed in RRs of relative moderately high temperature and absolute temperature.
Fig. 2.
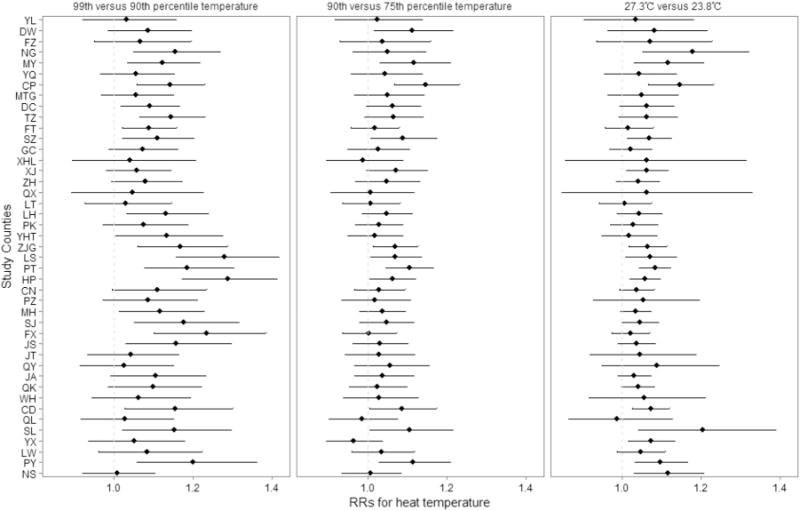
The relative risks (RRs) of heat temperature (99th percentile vs. 90th percentile temperature) on non-accidental mortality cumulated over lags of 0–2 days in each county. The RRs are ordered by geographic latitude of county locations (from north to south). County names are given in Table A1.
Fig. 3 shows the pooled estimates of heat effects on mortality over lags 0–2 days, stratified by age, sex, and different causes. Overall, RRs for extremely high temperature using the 99th percentile versus the 90th percentile temperature are higher than those of moderately high temperature (90th vs. 75th temperature of each county) and absolute temperature (27.3 °C vs. 23.8 °C for all the counties). Mortalities of all diseases are significantly associated with higher temperature. Compared with the 90th percentile temperature for example, the RRs at the 99th percentile temperature for non-accidental mortality is 1.105 (95%CI: 1.089, 1.122), for circulatory disease is 1.107 (95%CI: 1.081, 1.133), for respiratory disease is 1.095 (95%CI: 1.050, 1.142), for coronary heart disease is 1.073 (95%CI: 1.047, 1.099), for acute myocardial infarction is 1.072 (95%CI: 1.042, 1.104), and for stroke is 1.095 (95%CI: 1.052, 1.138). In particular, the non-accidental mortality, circulatory mortality, and respiratory mortality present significant increases corresponding to all patterns of high temperature changes. The 75 years or older age group had the highest RRs for all causes of mortalities; younger groups also presented significant effects for non-accidental mortality, circulatory disease, and respiratory disease. For sex, effects of extremely high temperature on mortality are generally higher in males than in females, except for coronary heart disease. The insignificant CIs may be caused by the small dataset of different population groups (Gasparrini et al., 2015). Results of sensitivity analyses presented in Table A2 also indicate the robustness of county-specific and pooled estimates.
Fig. 3.
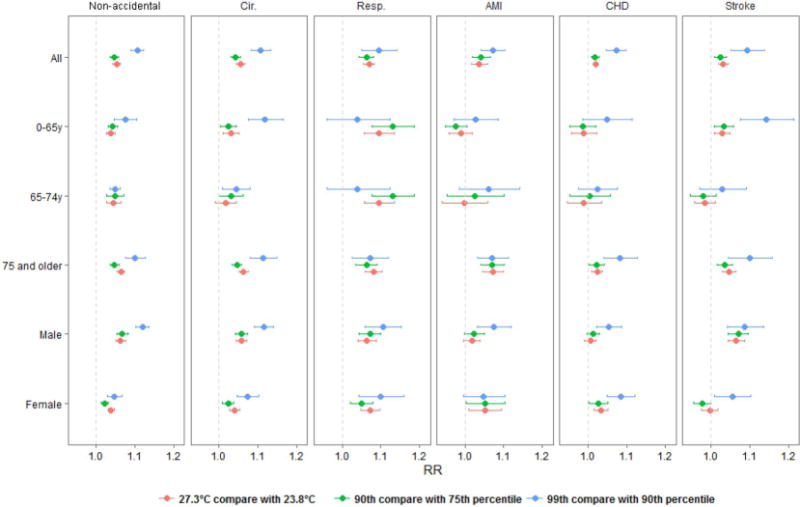
Pooled heat effects on mortality over lags 0–2 days in 43 counties.
4. Discussion
Using data from 43 counties widely ranging from northern to southern China, we have estimated the associations between high ambient temperature and mortality of different causes at the county-level in various climate patterns, including the mid-temperate, warm-temperate and subtropical climate zones. The inclusion of 531,794 deaths provides high statistical power for our analysis and a more accurate description of heat-related effects. Compared to previous studies of multi-cities (Chen et al., 2013; Huang et al., 2015; Ma et al., 2014; Zeng et al., 2016) and global communities (Gasparrini et al., 2015; Guo et al., 2014), another strength of this study is our inclusion of non-accidental death and five different causes, which enables us to understand the responses of cause-specific diseases under exposure to high temperature and characteristics for different population groups. The findings have important public health implications for targeted disease control and prevention.
Based on this large dataset across the country, we found evidence in most counties that high temperature is associated with increased non-accidental mortality risk, and pooled estimates are also significantly associated with high temperature changes in all causes. This result is consistent with earlier multi-center studies in China. In this study, a 1 °C increase of moderately high temperature (90th vs. 75th) is associated with pooled RRs of 1.046 (95% CI: 1.034, 1.058), 1.042 (95%CI: 1.030, 1.054), and 1.063 (95%CI: 1.044, 1.081) in mortality of non-accidental cause, circulatory disease, and respiratory disease, respectively, which is consistent with Ma’s study reporting that a 1 °C increase in temperature (99th vs. 75th) was associated with increases of 2.83% (95% posterior interval (PI): 1.42%, 4.24%) in non-accidental mortality, 3.02% (95% PI: 1.33%, 4.71%) in cardiovascular disease, and 4.64% (95% PI: 1.96%, 7.31%) in respiratory mortality, respectively (Ma et al., 2014), Zeng’s study reporting an increase of 0.33% (95%CI: 0.11%, 0.56%) in non-accidental mortality (Zeng et al., 2016), and Huang’s study reporting a pooled RR of 1.04 (95%CI: 0.90, 1.18) for non-accidental mortality associated with a 1 °C increase above the threshold temperature (Huang et al., 2015). A previous study of 107 US communities reported that increasing temperature (at the 99th versus 90th percentile temperature) was associated with an increase of 3.0% (95%PI: 2.4%, 3.6%) in mortality risk (Anderson and Bell, 2009), compared to a RR of 1.105 (95%CI: 1.089, 1.122) in non-accidental mortality in our study. Percentage increase in acute myocardial infarction at 30 °C was 15.67% (95%CI: −7.54%, 44.71%) (Braga et al., 2002), compared to an increase of 11.8% (95%CI: 8.3%, 15.4%) in this study. The differences may be due to different temperatures, data period, and the application of different models. Our results also indicate that the effects of high temperature are acute at the national level and last for about 2 days. Similar patterns of time lag have been observed in previous studies (Guo et al., 2014). Overall, these results suggest that high temperature is associated with increased mortality risk. Heat- related health effect is a concern that should be better addressed by public health authorities. Implementation of high temperature alert systems and heat-related health risk early warning systems as well as health protection guidelines under extreme heat weather could potentially reduce heat-related health damages.
There are substantial variations in the extent of county-specific relative risks associated with high temperature. On one hand, based on different patterns of effect estimates, we have identified spatial heterogeneity of heat effects in 43 counties. Since we ordered counties in Fig. 2 according to their latitude from north to south, counties located at middle latitudes have a higher mortality increase under exposure to extremely high temperature, including counties from Xi’an (LT, LH), Nanjing (PK, YHT, LS), Suzhou (ZJG), Shanghai (PT, HP, CN, PZ, MH, SJ, FX, JS). While this phenomenon is not observed in heat effects caused by exposure to moderately high temperature, the result signifies counties in central and eastern China with relatively mild temperatures may suffer the most from local extreme temperature compared to counties in northern and southern China. However, this finding is not consistent with the common hypothesis that extremely high temperatures may cause more deaths in cold areas since residents there could not adapt to heat. There are two possible explanations: first, based on a previous study at the global scale (Guo et al., 2014), the degree of risk associated with heat may vary with climate, and the heat threshold temperature in warmer areas may be higher than that of colder areas so that people in southern China may adapt to extreme heat better than people living in central and eastern China. Second, in northern China, although winter temperatures are increasing (Committee of National Assessment Report on Climate Change, 2015), the frequency and strength of extreme heat in the summer is still lower than central and eastern China (Chen et al., 2011). Thus, the health effect due to extreme heat may be milder in northern areas, while people living in central and eastern regions with milder temperature have a higher possibility of suffering from more intense extreme heat due to weaker adaption. Furthermore, rapid urbanization in these counties may exacerbate the heat effect (Anderson and Bell, 2009). A five-city study in China also indicated that cities in subtropical climate zones such as Shanghai and Nanjing suffered more from extremely high temperatures (Sun et al., 2012; Zeng et al., 2016). Investigation in the national climate change report also validated our findings that the central and eastern areas of China have suffered and may be at the forefront for more severe extreme heat in the future (Committee of National Assessment Report on Climate Change, 2015). Our large dataset enable us to capture the spatial characteristic of heat-related mortality in a wide range of locations in China, which could be supportive for the planning of health prevention and adaptation.
On the other hand, mortality by exposure to extremely high temperature (99th vs. 90th percentile temperature) is consistently higher than by exposure to moderately high temperature (90th vs. 75th percentile temperature) in all 43 counties, which is consistent with Chen’s study on eight Chinese cities (Chen et al., 2013). Both the relative moderately high temperature and the absolute moderately high temperature showed mild influences on non-accidental mortality. Therefore, exposure to extremely high temperatures may be linked to more deaths in all 43 counties. Regardless of different climates, this result suggests that people need to strengthen their adaptation to extreme temperature due to local climate changes. Driving factors of the health effects of extreme temperature should be identified so that public health interventions under our changing climate could effectively target at-risk groups, mitigate health effects, and improve adaptation (Bobb et al., 2014).
Furthermore, we adopted both relative and absolute temperatures because a previous study indicated that effect estimates for these two different temperature patterns may be helpful to explain population adaptation through a wide range of locations (Anderson and Bell, 2009). The effects from relative temperature were estimated according to the distribution of each county’s temperature and allow comparisons despite the differences among climatic ranges, while the effects estimated using absolute temperature changes among all the counties support the comparison of 43 different locations by the same temperature criteria. Since absolute temperatures could have different impacts depending on the location, we hypothesized that larger geographic variances of absolute estimates could be obtained. However, the comparison between RRs of relative temperature (90th vs. 75th percentile temperatures in each county) and absolute temperature (90th vs. 75th percentile temperatures of all counties) did not show large differences. One possible reason for this is that the health effects from moderately high temperature as we defined (90th vs. 75th) in this study may be too mild to capture spatial variances. It is also difficult to find an absolute extremely high temperature value given the wide range of climates in all 43 counties. The same trend of health effects related to the three temperature patterns were also found in the meta-analysis results at the national scale.
The pooled estimates show susceptibility by different causes of death, age, and sex at the national scale. We found that all causes of death could be significantly increased under exposure to high temperature, especially extremely high temperature. This result agrees with many previous findings for single outcomes, including non-accidental mortality (Guo et al., 2014; Zeng et al., 2016), circulatory disease (Anderson and Bell, 2009; Gasparrini et al., 2012; Huang et al., 2014), acute myocardial infarction (Gasparrini et al., 2012; Schwartz et al., 2004), coronary heart disease (Tian et al., 2012), stroke (Chen et al., 2013), and respiratory disease (Anderson and Bell, 2009; Gasparrini et al., 2012; Liu et al., 2011). All causes of deaths generally increase with increasing age, and populations of 75 years or older are associated with a larger heat effect, as reported in previous studies (Anderson and Bell, 2009; Gasparrini et al., 2012). In contrast, other age groups were subject to relatively lower temperature-mortality risks. Males have higher relative risk than females in most causes except AMI and CHD. These vulnerable subpopulations could identify the targets for heat-effects prevention and public health intervention under global warming.
Our dataset including non-accidental and five different causes of death enables us to find substantial variations in cause-specific heat effects that are seldom discussed in other multi-center studies. Among main causes of exposure to extremely high temperature, increased mortality for circulatory disease was slightly higher than that of respiratory disease. However, if we looked at these two causes under exposure to moderately high temperature, the relative risk of respiratory disease was larger compared to that of circulatory diseases, and this was observed in both the total population and stratified subpopulations. Thus, the associations with moderately high temperature are consistent with earlier studies of cardiovascular and respiratory diseases (Gasparrini et al., 2012; Huang et al., 2015). In detail, our findings indicate that increased mortality of respiratory diseases could be higher for populations younger than 75 years of age. The underlying mechanisms for increased respiratory mortality with high temperature are not yet well known (Gasparrini et al., 2015).
Within circulatory causes, increased mortality for acute myocardial infarction (1.7% to 7.5%), coronary heart disease (0.5% to 8.3%) and stroke (2.4% to 14.3%) are all associated with high temperature, in which the highest increased risks appeared for strokes. The relative risks for stroke mortality were similar to the results in a multi-city study (Chen et al., 2013). Increased mortality for populations older than 75 years of age (3.6% to 10.0%) and males (6.5% to 8.8%) are higher than other groups. Physiological mechanisms of increased stroke may be partly due to a thrombotic phenomenon (Bouchama and Knochel, 2002; Chen et al., 2013; Gasparrini et al., 2012). Strokes in China have a higher fatality than that of developed countries (Strong et al., 2007). As a response to the frequent extreme heat weather in this country, high temperature-induced stroke mortality should be addressed and prevented. For acute myocardial infarction and coronary heart disease, population over 75 years old and females indicated relatively higher excess mortality associated with high temperature. This result is consistent with an earlier conclusion that the elderly and females are more sensitive to stroke and heart failure (Gasparrini et al., 2012). Heat vulnerability of the elderly may be due to aging-related physiological changes in thermoregulation and homeostasis (Basu and Samet, 2002a). As high temperature is a potentially avoidable exposure, protective action guidelines should be provided to vulnerable populations to reduce exposure and allow for individual protection in everyday life (Hajat et al., 2010).
Our study has many strengths. First, an analysis of this large dataset across the country increases statistical power to provide reliable evidence for high temperature-related health effects. Second, the DLNMs and meta-analysis enable us to obtain location-specific and national-scale non-linear effects between temperature and mortality risk for non-accidental mortality and five other causes (Gasparrini et al., 2015). In addition, the effects estimated based on both relative and absolute temperature allow comparisons through different climatic patterns. Sensitivity analysis indicated that RRs were slightly changed when PM2.5 and O3 were included in models, which is consistent with the robustness of temperature-mortality results in previous studies (Anderson and Bell, 2009; Basu and Samet, 2002b; Chen et al., 2013).
Our study also has several limitations. First, although a wide range of locations are included, the data only covers the time period of 2013 to 2015, which is shorter than some of the previous studies. Although this limitation might have a slight impact on the significance of the temperature-mortality relationship, the overwhelming large number of cases (531,794) ensures sufficient statistical power in this study. Therefore, this issue would not have a major influence on the overall trend of heat-related effect and on our conclusions. Second, since we conducted a time series analysis, reasons for variation in heat-related effects among different counties and potential confounding factors at the individual level could not be fully explored. Modifications on health effects by socio-economic factors, including aging, education, race, green space, poverty level, AC prevalence, access to health care, etc. are all worth exploring. Therefore, future studies should address the limitations by extending the time scale of datasets and by conducting meta-regression using datasets with location-specific risk factors.
5. Conclusion
This study estimates associations between high temperature and cause-specific mortality in multiple sites across China. In all studied counties, extreme heat is linked to more deaths, and counties in central and eastern areas with mild temperatures should be given more attention for disease prevention. The heterogeneous characteristics across counties indicate the need for location-specific prevention strategies. People with sensitive diseases, including circulatory disease, respiratory disease, CHD, AMI, and stroke, and the elderly population are identified as susceptible subpopulations. Based on these findings, this study provides quantitative evidence of how heat affects health and informs the need for public policies to protect against high temperature-induced mortalities.
Acknowledgments
This study was supported by four foundation: National Natural Science Foundation of China (Grant: 21277135 and 91543111), National High-level Talents Special Support Plan of China for Young Talents, and Environmental Health Development Project of Institute of Environmental Health and Related Product Safety, China CDC.
Table A1.
Summary of air pollution and temperature distributions in 43 counties.
| City | County | Total deaths | N | Mean temperature (°C) | 24 h–average O3 (μg/m3) | Daily PM2.5 (μg/m3) |
|---|---|---|---|---|---|---|
| (Mean ± SD) | (Mean ± SD) | (Mean ± SD) | ||||
| Beijing | Changping (CP) | 13,003 | 1095 | 13.62 ± 10.97 | 63.13 ± 40.34 | 73.57 ± 65.90 |
| Dongcheng (DC) | 16,785 | 1095 | 13.62 ± 10.97 | 55.47 ± 36.84 | 90.27 ± 76.02 | |
| Fengtai (FT) | 25,677 | 1095 | 13.62 ± 10.97 | 40.27 ± 29.27 | 95.61 ± 76.87 | |
| Mentougou (MTG) | 5670 | 1095 | 13.62 ± 10.97 | 54.69 ± 35.97 | 77.07 ± 66.09 | |
| Miyun(MY) | 8064 | 1095 | 13.62 ± 10.97 | 70.59 ± 41.28 | 65.21 ± 58.33 | |
| Tongzhou (TZ) | 14,413 | 1095 | 13.62 ± 10.97 | 49.86 ± 36.19 | 105.66 ± 85.23 | |
| Yanqing (YQ) | 5048 | 1095 | 13.62 ± 10.97 | 58.41 ± 36.44 | 65.47 ± 56.70 | |
| Chengdu | Jintang (JT) | 16,140 | 1095 | 16.59 ± 7.19 | 47.17 ± 33.00 | 78.26 ± 54.97 |
| Pengzhou (PZ) | 15,960 | 1095 | 16.59 ± 7.19 | 71.20 ± 39.48 | 50.70 ± 37.46 | |
| Qingyang (QY) | 11,342 | 1095 | 16.59 ± 7.19 | 53.60 ± 36.45 | 78.85 ± 52.72 | |
| Qionglai (QL) | 12,497 | 1095 | 16.59 ± 7.19 | 45.75 ± 35.03 | 74.65 ± 52.80 | |
| Shuangliu (SL) | 11,706 | 1095 | 16.59 ± 7.19 | 45.75 ± 35.03 | 74.65 ± 52.80 | |
| Wuhou (WH) | 9624 | 1095 | 16.59 ± 7.19 | 45.75 ± 35.03 | 74.65 ± 52.80 | |
| Guangzhou | Liwan (LW) | 17,179 | 1095 | 21.86 ± 6.13 | 46.58 ± 29.30 | 50.83 ± 28.73 |
| Panyu (PY) | 11,688 | 1095 | 21.86 ± 6.13 | 55.70 ± 35.27 | 49.52 ± 28.72 | |
| Yuexiu (YX) | 21,038 | 1095 | 21.86 ± 6.13 | 44.74 ± 29.33 | 46.83 ± 25.94 | |
| Harbin | Daowai (DW) | 17,350 | 1095 | 5.08 ± 15.60 | 38.34 ± 25.00 | 75.13 ± 78.99 |
| Fangzheng (FZ) | 3751 | 1095 | 5.08 ± 15.60 | 38.34 ± 25.00 | 75.13 ± 78.99 | |
| Nangang (NG) | 21,714 | 1095 | 5.08 ± 15.60 | 38.34 ± 25.00 | 75.13 ± 78.99 | |
| Yilan (YL) | 7255 | 1095 | 5.08 ± 15.60 | 38.34 ± 25.00 | 75.13 ± 78.99 | |
| Nanjing | Lishui (LS) | 8156 | 1095 | 16.62 ± 8.97 | 57.72 ± 35.04 | 66.73 ± 41.10 |
| Pukou (PK) | 9547 | 1095 | 16.62 ± 8.97 | 66.17 ± 33.46 | 69.01 ± 42.36 | |
| Yuhuatai (YHT) | 3962 | 1095 | 16.62 ± 8.97 | 57.72 ± 35.04 | 66.73 ± 41.10 | |
| Shanghai | Changning (CN) | 15,041 | 1095 | 17.24 ± 8.67 | 73.42 ± 32.69 | 57.23 ± 41.39 |
| Fengxian (FX) | 11,662 | 1095 | 17.24 ± 8.67 | 70.43 ± 31.47 | 58.58 ± 43.05 | |
| Huangpu (HP) | 25,371 | 1095 | 17.24 ± 8.67 | 73.89 ± 31.70 | 56.95 ± 39.62 | |
| Jinshan (JS) | 11,337 | 1095 | 17.24 ± 8.67 | 70.43 ± 31.47 | 58.58 ± 43.05 | |
| Minhang (MH) | 22,652 | 1095 | 17.24 ± 8.67 | 70.43 ± 31.47 | 58.58 ± 43.05 | |
| Putuo (PT) | 24,751 | 1095 | 17.24 ± 8.67 | 73.42 ± 32.69 | 57.23 ± 41.39 | |
| Songjiang (SJ) | 12,340 | 1095 | 17.24 ± 8.67 | 70.43 ± 31.47 | 58.58 ± 43.05 | |
| Shenzhen | Nanshan (NS) | 3915 | 1095 | 23.45 ± 5.46 | 55.85 ± 29.08 | 34.62 ± 22.54 |
| Shijiazhuang | Gaocheng (GC) | 12,710 | 1095 | 14.53 ± 10.79 | 40.29 ± 33.29 | 115.79 ± 94.72 |
| Shenze (SZ) | 4632 | 1095 | 14.53 ± 10.79 | 40.29 ± 33.29 | 115.79 ± 94.72 | |
| Xinji (XJ) | 10,821 | 1095 | 14.53 ± 10.79 | 40.29 ± 33.29 | 115.79 ± 94.72 | |
| Zanhuang (ZH) | 4246 | 1095 | 14.53 ± 10.79 | 93.83 ± 46.20 | 88.05 ± 62.84 | |
| Suzhou | Zhangjiagang (ZJG) | 17,579 | 1095 | 16.76 ± 8.94 | 79.39 ± 44.24 | 59.98 ± 41.50 |
| Taiyuan | Qingxu (QX) | 5010 | 1095 | 11.21 ± 10.42 | 46.81 ± 33.55 | 71.80 ± 51.96 |
| Xinghualing (XHL) | 8803 | 1095 | 11.21 ± 10.42 | 42.32 ± 30.72 | 71.26 ± 47.10 | |
| Wuhan | Caidian (CD) | 8254 | 1095 | 16.95 ± 9.10 | 90.77 ± 56.03 | 69.32 ± 48.42 |
| Jiang’an (JA) | 13,212 | 1095 | 16.95 ± 9.10 | 63.00 ± 44.48 | 78.87 ± 55.53 | |
| Qiaokou (QK) | 11,247 | 1095 | 16.95 ± 9.10 | 69.31 ± 55.47 | 85.69 ± 57.92 | |
| Xi’an | Lianhu (LH) | 11,632 | 1095 | 15.25 ± 9.70 | 48.25 ± 33.99 | 81.81 ± 70.76 |
| Lintong (LT) | 9010 | 1095 | 15.25 ± 9.70 | 45.47 ± 30.09 | 78.75 ± 77.82 |
Table A2.
Sensitivity of pooled relative risks to inclusion of pollution variables and different lags in the temperature-non-accidental mortality model.
| 99th versus 90th | RR(95%CI) 90th versus 75th |
27.3 °C versus 23.8 °C | |
|---|---|---|---|
| Main model | 1.105(1.089,1.122) | 1.046(1.034,1.057) | 1.052(1.043,1.062) |
| With air pollution | |||
| With PM2.5 | 1.103(1.087,1.119) | 1.045(1.034,1.057) | 1.051(1.042,1.059) |
| With O3 | 1.100(1.082,1.118) | 1.040(1.029,1.052) | 1.046(1.037,1.054) |
| With PM2.5 and O3 | 1.100(1.082,1.117) | 1.042(1.030,1.053) | 1.046(1.037,1.055) |
| With various lag days | |||
| Lag 0–3, knots = 1 | 1.108(1.089,1.126) | 1.037(1.024,1.051) | 1.044(1.033,1.054) |
| Lag 0–7, knots = 1 | 1.102(1.078,1.128) | 1.033(1.016,1.050) | 1.034(1.022,1.048) |
| Lag 0–7, knots = 3 | 1.098(1.074,1.123) | 1.032(1.016,1.049) | 1.035(1.022,1.048) |
| With public holidays | 1.106(1.090,1.123) | 1.046(1.034,1.058) | 1.052(1.042,1.062) |
Footnotes
Author contribution
J. B. and T. L. designed the study. D.X., W.W., and P.Z. cleaned the data. J.B. and D.X. analyzed data. C.C. and Q.S. checked the data and results. J. B. and M. H. drafted the manuscript. All authors contributed to the interpretation of the results.
Conflict of interest
The authors declare no conflicts of interest.
References
- Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20:205–213. doi: 10.1097/EDE.0b013e318190ee08. http://dx.doi.org/10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett AG. Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology. 2007;18:369–372. doi: 10.1097/01.ede.0000257515.34445.a0. http://dx.doi.org/10.1097/01.ede.0000257515.34445.a0. [DOI] [PubMed] [Google Scholar]
- Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. http://dx.doi.org/10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R, Samet JM. An exposure assessment study of ambient heat exposure in an elderly population in Baltimore, Maryland. Environ Health Perspect. 2002a;110:1219–1224. doi: 10.1289/ehp.021101219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002b;24:190–202. doi: 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- Bobb JF, Peng RD, Bell M, Dominici Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect. 2014;122:811–816. doi: 10.1289/ehp.1307392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346:1978–1988. doi: 10.1056/NEJMra011089. http://dx.doi.org/10.1056/NEJMra011089. [DOI] [PubMed] [Google Scholar]
- Braga ALF, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities Environ Health Perspect. 2002;110:859–863. doi: 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Jiang Z, Li L, Yiou P. Simulation of regional climate change under the IPCC A2 scenario in southeast China. Clim Dyn. 2011;36:491–507. http://dx.doi.org/10.1007/s00382-010-0910-3. [Google Scholar]
- Chen R, Wang C, Meng X, Chen H, Thach TQ, Wong CM, Kan H. Both low and high temperature may increase the risk of stroke mortality. Neurology. 2013;81:1064–1070. doi: 10.1212/WNL.0b013e3182a4a43c. http://dx.doi.org/10.1212/WNL.0b013e3182a4a43c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee of National Assessment Report on Climate Change. The Third National Assessment Report on Climate Change. Committee of National Assessment Report on Climate Change; Beijing: 2015. [Google Scholar]
- Gasparrini A, Armstrong B, Kovats S, Wilkinson P. The effect of high temperatures on cause-specific mortality in England and Wales. Occup Environ Med. 2012;69:56–61. doi: 10.1136/oem.2010.059782. http://dx.doi.org/10.1136/oem.2010.059782. [DOI] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369–375. doi: 10.1016/S0140-6736(14)62114-0. http://dx.doi.org/10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Gasparrini A, Armstrong B, et al. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology. 2014;25:781–789. doi: 10.1097/EDE.0000000000000165. http://dx.doi.org/10.1097/EDE.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat S, Kosatky T. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health. 2010;64:753–760. doi: 10.1136/jech.2009.087999. http://dx.doi.org/10.1136/jech.2009.087999. [DOI] [PubMed] [Google Scholar]
- Hajat S, Armstrong B, Baccini M, Biggeri A, Bisanti L, Russo A, Paldy A, Menne B, Kosatsky T. Impact of high temperatures on mortality: is there an added heat wave effect? Epidemiology. 2006;17:632–638. doi: 10.1097/01.ede.0000239688.70829.63. http://dx.doi.org/10.1097/01.ede.0000239688.70829.63. [DOI] [PubMed] [Google Scholar]
- Hajat S, O’Connor M, Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet. 2010;375:856–863. doi: 10.1016/S0140-6736(09)61711-6. http://dx.doi.org/10.1016/S0140-6736(09)61711-6. [DOI] [PubMed] [Google Scholar]
- Huang J, Wang J, Yu W. The lag effects and vulnerabilities of temperature effects on cardiovascular disease mortality in a subtropical climate zone in China. Int J Environ Res Public Health. 2014;11:3982–3994. doi: 10.3390/ijerph110403982. http://dx.doi.org/10.3390/ijerph110403982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z, Lin H, Liu Y, Zhou M, Liu T, Xiao J, Zeng W, Li X, Zhang Y, Ebi KL, Tong S, Ma W, Wang L. Individual-level and community-level effect modifiers of the temperature-mortality relationship in 66 Chinese communities. BMJ Open. 2015;5:e009172. doi: 10.1136/bmjopen-2015-009172. http://dx.doi.org/10.1136/bmjopen-2015-009172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Breitner S, Pan X, Franck U, Leitte AM, Wiedensohler A, von Klot S, Wichmann HE, Peters A, Schneider A. Associations between air temperature and cardio-respiratory mortality in the urban area of Beijing, China: a time-series analysis. Environ Health. 2011;10:51. doi: 10.1186/1476-069X-10-51. http://dx.doi.org/10.1186/1476-069X-10-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma W, Chen R, Kan H. Temperature-related mortality in 17 large Chinese cities: how heat and cold affect mortality in China. Environ Res. 2014;134:127–133. doi: 10.1016/j.envres.2014.07.007. http://dx.doi.org/10.1016/j.envres.2014.07.007. [DOI] [PubMed] [Google Scholar]
- Medinaramón M, Schwartz J. Temperature, temperature extremes, and mortality: a study of acclimatization and effect modification in 50 United States cities. Occup Environ Med. 2007;64:827–833. doi: 10.1136/oem.2007.033175. http://dx.doi.org/10.1136/oem.2007.033175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J, Samet JM, Patz JA. Hospital admissions for heart disease: the effects of temperature and humidity. Epidemiology. 2004;15:755–761. doi: 10.1097/01.ede.0000134875.15919.0f. [DOI] [PubMed] [Google Scholar]
- Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6:182–187. doi: 10.1016/S1474-4422(07)70031-5. http://dx.doi.org/10.1016/S1474-4422(07)70031-5. [DOI] [PubMed] [Google Scholar]
- Sun Y, Li L, Zhou M. Analysis of the lag-effects of temperature on the five cities’ mortality in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2012;46:1015–1019. [PubMed] [Google Scholar]
- Tian Z, Li S, Zhang J, Jaakkola JJK, Guo Y. Ambient temperature and coronary heart disease mortality in Beijing, China: a time series study. Environ Health. 2012;11:56. doi: 10.1186/1476-069X-11-56. http://dx.doi.org/10.1186/1476-069X-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Q, Li G, Cui Y, Jiang G, Pan X. Estimating temperature-mortality exposure-response relationships and optimum ambient temperature at the multi-city level of China. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13030279. http://dx.doi.org/10.3390/ijerph13030279. [DOI] [PMC free article] [PubMed] [Google Scholar]


