Abstract
Objective
Non-suicidal self-injury (NSSI) is prevalent among young adults and associated with negative medical and psychological consequences, necessitating its treatment. However, few treatments have been developed to treat NSSI specifically, or to treat the behavior among individuals without borderline personality disorder. The purpose of this study was to investigate the Treatment for Self-Injurious Behaviors (T-SIB), a brief, behavioral intervention specifically developed to treat NSSI among young adults, in a pilot randomized controlled trial (RCT).
Method
Thirty-three young adults (age: M = 22.36 years, SD = 3.40) meeting inclusion and exclusion criteria were randomly assigned to the treatment (T-SIB; n = 15) or treatment as usual (TAU; n = 18) condition. The sample was 93.9% female, 42.4% Caucasian, and 30.3% Hispanic/Latino.
Results
Feasibility and acceptability of the study and intervention were supported, and medium effects were found for decreased NSSI frequency in the T-SIB group using intent-to-treat analyses.
Conclusion
Results of this study support the further evaluation of T-SIB in a larger RCT.
Keywords: Non-suicidal self-injury, RCT, treatment development, treatment outcome research
Non-suicidal self-injury (NSSI), defined as behaviors involving the deliberate self-inflicted injury of body tissue that are not socially sanctioned and performed without suicidal intent (International Society for the Study of Self-Injury, 2016), is prevalent among young adults, with lifetime rates ranging from 12% to 38% (e.g., Gratz, Conrad, & Roemer, 2002; Muehlenkamp & Gutierrez, 2004). Research investigating criterion A of NSSI disorder, included as a disorder requiring further research in the 5th edition of the Diagnostic and Statistical Manual (DSM; American Psychiatric Association, 2013), suggests that between 11.2% and 37.4% of young adults with NSSI report a clinically-relevant frequency of the behavior (e.g., Andover, 2014; Gratz, Dixon-Gordon, Chapman, & Tull, 2015). The behavior is associated with significant negative consequences, including social isolation, guilt, and shame (Gratz, 2003), physical injury ranging in medical severity, and medical sequelae such as infections and scarring. Further, although NSSI and suicidal behaviors are distinct behaviors distinguished by intent to die, NSSI is a significant risk factor for attempted suicide (e.g., Klonsky, May, & Glenn, 2013). Although the behavior can be difficult to treat (e.g., Muehlenkamp, 2006), NSSI does respond to intervention (Nock, Teper, & Hollander, 2007; Turner, Austin, & Chapman, 2014). The severe nature of NSSI and its consequences mandate its treatment.
Several interventions have been developed to treat self-injurious behaviors, which include both non-suicidal and suicidal self-injury. However, NSSI differs from suicide in several important ways, including intent, frequency, methods used, and severity of injuries (Muehlenkamp, 2005), potentially limiting the effectiveness of interventions for self-injurious behaviors more generally on the specific behavior. Although few interventions have been developed specifically to treat NSSI, several have been applied to the behavior. Dialectical behavior therapy (DBT; Linehan, 1993), developed to treat borderline personality disorder (BPD), includes an emphasis on the treatment of suicidal behaviors and NSSI. Several studies of DBT have evaluated its effect on NSSI specifically, usually among women diagnosed with BPD. These studies have found significant reductions in NSSI behaviors following a 3-month inpatient DBT program (Bohus et al., 2004) and a 12-month outpatient DBT program (van den Bosch, Koeter, Stijnen, Verheul, & van den Brink, 2005; Verheul, van den Bosch, Koeter, De Ridder, Stijnen, & van den Brink, 2003) when compared to treatment as usual (TAU). In addition, brief DBT (B-DBT), a 6-month intervention, was associated with a decrease in NSSI episodes at the end of treatment (Stanley, Brodsky, Nelson, & Dulit, 2007). However, research comparing DBT to treatment by experts found that although NSSI frequency decreased significantly across the sample, there was no difference in rate of decrease between treatment conditions (Linehan et al., 2006). Overall, meta-analyses have indicated small to medium effects for treatment of self-injurious behaviors among individuals with BPD when including both randomized controlled trials (RCTs) and uncontrolled trials (Kliem, Kröger, & Kosfelder, 2010).
Fewer studies have investigated the effect of DBT on decreasing NSSI in samples without a BPD diagnosis, but the intervention continues to appear effective. Among college students with at least three BPD symptoms and current suicidal ideation, greater decreases in NSSI were found among those assigned to DBT than among those assigned to TAU (Pistorello, Fruzzetti, MacLane, Gallop, & Iverson, 2012), and large and medium effect sizes were reported for decreased NSSI at post-treatment and 6-month follow up, respectively, among adolescents with binge eating and self-injurious behaviors (Fischer & Peterson, 2015). Although DBT is a promising intervention in the treatment of NSSI, further research is necessary to investigate its effectiveness when compared with active control conditions (Turner et al., 2014). Further, given that NSSI often occurs among individuals without a BPD diagnosis (e.g., Andover, Pepper, Ryabchenko, Orrico, & Gibb, 2005; Bracken-Minor & McDevitt-Murphy, 2014), additional research on DBT for the treatment of NSSI is necessary among non-BPD samples.
Researchers have suggested the utility of cognitive interventions, which target the maladaptive thoughts and beliefs underlying NSSI, in addressing NSSI behaviors (Muehlenkamp, 2006). In support of this, a meta-analysis of cognitive-behavioral treatments that reported outcomes for suicidal and non-suicidal behaviors among adolescents found a small effect for the reduction of NSSI behaviors (Labelle, Pouliot, & Janelle, 2015). Manual assisted cognitive therapy (MACT), a 6-session adjunctive cognitive-behavioral intervention focusing on problem solving therapy and relapse prevention, was developed for the treatment of both suicidal and non-suicidal self-injury. Studies of the intervention have demonstrated mixed results in the reduction of suicidal and non-suicidal self-injury (Evans et al., 1999; Salkovskis, Atha, & Storer, 1990; Tyrer et al., 2003; Weinberg, Gunderson, Hennen, & Cutter, 2006). However, only one study has investigated NSSI specifically as an outcome, reporting that MACT in addition to TAU was more effective in decreasing NSSI behaviors than TAU alone (Weinberg et al., 2006). Researchers continue to explore cognitive interventions for NSSI, including the adaptation of mindfulness-based cognitive therapy (MBCT) for young adults, which targets emotion regulation, distress tolerance, and attention to negative thoughts in order to decrease NSSI behavior (Rees, Hasking, Breen, Lipp, & Mamotte, 2015).
Research reporting increased emotion dysregulation among individuals with NSSI (e.g., Andover & Morris, 2014), as well as the effectiveness of DBT, which targets emotion regulation skills, in treating the behavior, suggests that interventions focusing on building emotion regulation strategies may be particularly useful in the treatment of NSSI (Gratz, 2007; Turner et al., 2014). Emotion regulation group therapy (ERGT) was specifically developed to address NSSI by targeting emotion regulation and emotional avoidance in a 14-week adjunctive intervention (Gratz & Gunderson, 2006). Researchers have reported decreased NSSI among women with BPD and subclinical BPD assigned to receive ERGT and TAU when compared with those receiving TAU alone at post-treatment (Gratz & Gunderson, 2006; Gratz & Tull, 2011) and at 9-month follow up (Gratz, Tull, & Levy, 2014).
Despite the importance of treating NSSI, there are no well-established treatments for NSSI among individuals without a BPD diagnosis. Further, only ERGT has been developed for the treatment of NSSI specifically, rather than self-injurious behaviors more generally. However, it has not yet been evaluated outside of BPD and predominantly BPD samples, an important limitation as NSSI occurs transdiagnostically (Nock, Joiner, Gordon, Lloyd-Richardson, & Prinstein, 2006). Although DBT has the strongest empirical support for decreasing NSSI behaviors to date, evidence for the efficacy of the intervention in treating NSSI outside of BPD samples is limited. Further, DBT is a resource-intensive intervention, and it may be too intensive or not practical for all treatment-seeking individuals (Comtois, 2002; Comtois & Linehan, 2006). Therefore, the field would benefit from the development of a brief intervention designed to treat NSSI behaviors outside of the context of a specific psychiatric diagnosis, especially one that can be administered without intensive training for clinicians.
In order to target the aforementioned limitations of existing treatments, the Treatment for Self-Injurious Behaviors (T-SIB) was developed. This intervention is brief, consisting of 9-sessions, and was specifically developed to treat NSSI behaviors in young adults with and without a BPD diagnosis. In order to increase clinical utility, T-SIB was developed to serve as a stand-alone treatment or an adjunctive intervention. Consistent with recommendations for promising components of NSSI treatment (Nock et al., 2007; Muehlenkamp, 2006; Turner et al., 2014), T-SIB focuses on functional assessments to identify antecedents and reinforcers for NSSI behavior; behavior change is hypothesized to occur through the differential reinforcement of alternative behaviors. Based on antecedents and functions of the behavior identified through functional assessments, one of three individualized modules is selected in the final sessions to begin to address cognitive distortions, or to build skills deficits in interpersonal communication or distress tolerance, that underlie and contribute to NSSI behavior. The feasibility and acceptability of T-SIB were supported in an open pilot trial, and medium to large effect sizes for decreased NSSI at post-treatment and 3-month follow up supported the further study of T-SIB (Reference removed for blind review). The purpose of the current study was to further evaluate the intervention in a pilot RCT comparing T-SIB to TAU in order to examine treatment feasibility and acceptability and to examine change in NSSI behaviors, consistent with Stage I Behavioral Therapies research (Rounsaville, Carroll, & Onken, 2001), using both intent-to-treat and per-protocol approaches.
Method
Participants
The sample consisted of 33 treatment-seeking participants recruited from the community. Inclusion criteria consisted of (a) 18 to 29 years of age; and (b) engaged in NSSI involving direct tissue damage within the past month, or report a history of NSSI and urges to engage in NSSI within the past month. Participants a history of NSSI and urges, but not behaviors, during the past month were included in the study because of ethical concerns that individuals with strong urges to engage in NSSI and a history of the behavior would be excluded from treatment (Reference removed for blind review). Exclusion criteria were (a) active severe suicidal ideation as indicated by a score of 21 or greater on the Modified Scale for Suicidal Ideation (MSSI; Miller, Norman, Bishop, & Dow, 1986); and (b) current psychotic symptoms as indicated on the psychosis module of the Structured Clinical Interview for DSM-IV for Axis I disorders (SCID-I; First, Spitzer, Williams, & Gibbons, 1995). The inclusion and exclusion criteria used in this RCT were identical to those used in the open pilot trial (Andover et al., 2015); these criteria were purposefully kept minimal in order to increase generalizability of findings.
Demographic and clinical characteristics of the sample are provided in Table 2. The majority of the sample (78.8%, n = 26) reported at least one episode of NSSI within the past month; all others reported no NSSI behaviors within the past month, but urges to self-injure. Excluding one statistical outlier, the sample reported a mean lifetime frequency of 1932.27 (SD = 4233.00); among those with urges to self-injure during the past month but no behaviors, mean lifetime frequency was 658.83 (SD = 1018.24). Participants reported a mean of 309.00 NSSI behaviors (NSSI frequency; SD = 590.22) and reported engaging in NSSI on a mean of 9.73 days (NSSI days; SD = 10.77) for the four weeks prior to the baseline assessment; excluding participants with only urges to engage in NSSI during the past month, mean NSSI frequency for the four-week baseline assessment period was 392.23 (SD = 641.84) and mean NSSI days was 12.35 (SD = 10.71). Participants reported using a mean of 5.26 different methods (SD = 2.22); the most commonly reported methods including cutting (81.8%, n = 27), self-hitting (72.7%, n = 24), scratching (60.6%, n = 20), self-biting (57.6%, n = 19), and interfering with wound healing (54.5%, n = 18).
Table 2.
Demographic and Clinical Variables by Treatment Condition
| TAU (n = 18) |
T-SIB (n = 15) |
t/χ2 | df | d/Φ/Cramer’s V | |
|---|---|---|---|---|---|
| Demographic Variables | |||||
| Gender (% women) | 94.4 (n = 17) | 93.3 (n = 14) | 0.02 | 1 | .02 |
| Age | 22.67 (4.06) | 22.00 (2.48) | 0.58 | 28.65 | .20 |
| Race | 0.96 | 3 | .17 | ||
| % Native Hawaiian/Alaskan Native | 5.6 (n = 1) | 0.0 (n = 0) | |||
| % Black/African American | 27.8 (n = 5) | 26.7 (n = 4) | |||
| % White | 38.9 (n = 7) | 46.7 (n = 7) | |||
| % Other | 27.8 (n = 5) | 26.7 (n = 4) | |||
| Ethnicity (% Latino/Hispanic) | 27.8 (n = 5) | 35.7 (n = 5) | 0.23 | 1 | .09 |
| Clinical Variables | |||||
| Axis I Diagnosis (% Yes) | 77.8 (n = 14) | 80.0 (n = 12) | 0.02 | 1 | .03 |
| Number of Axis I Diagnoses | 1.89 (1.53) | 1.94 (1.58) | −0.08 | 31 | .03 |
| Axis I Diagnoses (%Yes) | |||||
| MDD | 50.0 (n = 9) | 33.3 (n = 5) | 0.93 | 1 | .17 |
| Other depressive disorder | 16.7 (n = 3) | 6.7 (n = 1) | 0.77 | 1 | .15 |
| Anxiety disorder | 50.0 (n = 9) | 60.0 (n = 9) | 0.33 | 1 | .10 |
| PTSD | 5.6 (n = 1) | 26.7 (n = 4) | 2.84 | 1 | .29 |
| Substance use disorder | 33.3 (n = 6) | 26.7 (n = 4) | 0.17 | 1 | .07 |
| Eating Disorder | 16.7 (n = 3) | 0.0 (n = 0) | 2.75 | 1 | .29 |
| BPD Diagnosis (% Yes) | 38.9 (n = 7) | 20.0 (n = 3) | 1.38 | 1 | .21 |
| ASPD Diagnosis (% Yes) | 16.7 (n = 3) | 13.3 (n = 2) | 0.07 | 1 | .05 |
| MSSI | 3.39 (6.00) | 3.20 (6.16) | 0.09 | 31 | .03 |
| Other psychotherapy at baseline (% Yes) | 27.8 (n = 5) | 40.0 (n = 6) | 0.55 | 1 | .13 |
| Other psychotherapy at post-treatment (% Yes) | 30.8 (n = 4) | 27.3 (n = 3) | 0.04 | 1 | .04 |
| Other psychotherapy at 3-month follow-up (% Yes) | 26.7 (n = 4) | 36.4 (n = 4) | 0.28 | 1 | .10 |
| Psychotropic medication at baseline (% Yes) | 22.2 (n = 4) | 20.0 (n = 3) | 0.02 | 1 | .03 |
| NSSI Behaviors | |||||
| Lifetime frequency | 2332.25 (4643.34) | 1470.73 (3838.15) | 0.53 | 26 | .20 |
| NSSI at Baseline (% Yes) | 88.9 (n = 16) | 66.7 (n = 10) | 2.42 | 1 | .27 |
| NSSI Frequency, Month | 424.25 (728.82) | 170.77 (337.18) | 1.32 | 24.86 | .43 |
| NSSI Days, Month | 10.94 (10.56) | 8.27 (11.20) | 0.71 | 31 | .25 |
Note. Numbers in parentheses represent standard deviations, unless otherwise noted. BPD = borderline personality disorder. ASPD = Antisocial personality disorder. MSSI = Modified Scale for Suicidal Ideation.
Procedure
The procedure for this study was identical to that of the open pilot trial (Reference removed for blind review), with the addition of randomization to the intervention or TAU control condition; a TAU control condition was chosen in order to reflect the community options available to treat NSSI behaviors. Participants were recruited through flyers and online and print advertisements over the course of three years. Individuals calling in response to an advertisement were screened to determine whether inclusion criteria were met. Those meeting inclusion criteria were invited to complete a baseline assessment in person. Written informed consent was obtained at the start of the baseline assessment, and participants completed interviews and self-report questionnaires. At the end of the baseline assessment, participants were randomized to the intervention condition (T-SIB) or the control condition (TAU) using an urn randomization procedure (Stout et al., 1994; Wei & Lachin, 1988) stratified for current use of psychotropic medications or psychotherapy (yes/no), gender (male/female), and self-reported frequency of NSSI in the past month (none/1–5/5+). Study treatment was provided by doctoral students in a clinical psychology program, trained and supervised by the first author. The Modified Scale for Suicidal Ideation (MSSI; Miller et al., 1986) and the Time Line Follow Back (TLFB) interview (Sobell & Sobell, 1992) were administered at baseline, within one week of the final treatment session (9 weeks after the baseline assessment for TAU participants), and at 3-month follow up. The Client Satisfaction Questionnaire (CSQ-8; Attkisson & Zwick, 1982) was administered to participants in the T-SIB condition within one week post-treatment. Post-treatment and follow up assessments were conducted by trained assessors blind to the participants’ baseline assessment and condition. The study was approved by the university’s Institutional Review Board. Participants were provided remuneration for assessments, and the intervention was provided free of charge.
Treatment Conditions
Treatment for Self-Injurious Behaviors (T-SIB)
The intervention consisted of nine hour-long individual weekly sessions. A detailed description of the intervention can be found in Andover et al. (2015), but a brief overview is provided here. Goals for each session are listed in Table 1. The treatment manual is available from the first author.
Table 1.
Topics and Goals by Session
| Session | Topic | Goals for Session |
|---|---|---|
| 1 | Psychoeducation and Addressing Ambivalence |
|
| 2 | Functional Assessment and Differential Reinforcement of Alternative Behaviors |
|
| 3–4 |
|
|
| 5 |
|
|
| 6 |
|
|
| 7–8 | Individualized Modules | Interpersonal Communication
Cognitive Distortions
Distress Tolerance
|
| 9 | Termination |
|
The goals of Session 1 are to provide psychoeducation about NSSI and to orient the participant to the intervention’s conceptualization of NSSI as a coping strategy. Motivational enhancement techniques are used to address ambivalence towards and to build motivation for behavior change.
The goals of Sessions 2 through 6 are two-fold. First, the client is introduced to and taught functional assessment using an informant-based antecedent-behavior-consequence (ABC) chart. This is used in sessions to review any instances of NSSI that occur, and assigned for homework after each session. If NSSI behavior has not occurred, the client may perform a functional assessment on instances when they experienced the urge to self-injure but did not engage in the behavior. The purpose of functional assessments is to identify the environmental, emotional, cognitive, and social antecedents and consequences of NSSI, as well as to provide an ongoing evaluation of the intervention as sessions progress.
The second goal of these sessions is to identify alternative behaviors to NSSI and to implement differential reinforcement procedures to decrease NSSI behavior and increase use of alternative behaviors. Alternative behaviors are identified in Sessions 3 and 4 through collaboration between the therapist and client and by conducting functional assessments of instances when the client experienced antecedents that often lead to self-injury, but did not self-injure. Alternative behaviors should be simple, easily accessible, within the client’s behavior repertoire, consistent with client preferences, and serve a similar function as NSSI. These behaviors are practiced in response to instances of minor distress (i.e., initially not in response to urges to self-injure), analyzed using a functional assessment, and revised before being used to replace NSSI after Session 5. The list of alternative behaviors is again revised during Session 6 based on client experiences, and the client is asked to continue to use the alternative behaviors—and perform functional assessments of these behaviors, which are reviewed at the beginning of session—for the remainder of the intervention. As the alternative behaviors are reinforced by the desired consequences, the likelihood that the alternative behavior will be repeated is increased and the likelihood of NSSI is decreased.
Sessions 7 and 8 are focused on one of three individualized modules: Interpersonal Communication, Cognitive Distortions, and Distress Tolerance. The therapist and client decide on a specific module based on common antecedents to NSSI identified in the functional assessment and coping deficits hypothesized to be contributing to current NSSI. The goal of the Interpersonal Communication module is to increase assertiveness skills in situations that may trigger NSSI; these skills are practiced in session using role play. The goals of the Cognitive Distortions module are to identify cognitive distortions that may contribute to NSSI behavior, and to begin to evaluate these thoughts and generate more realistic cognitions. The goals of the Distress Tolerance module are to discuss the concepts of accepting and tolerating distressing situations and feelings, and to begin to discuss ways to tolerate distress. It is important to note that the purpose of the individualized modules is to give the patient basic tools to begin to address skills deficits that may underlie NSSI behavior; it is not intended to thoroughly address these areas. Patients are encouraged to seek additional treatment to continue the work begun in these modules.
The goal of Session 9 is to prepare the patient for termination by reviewing progress during treatment through a functional assessment framework, reviewing skills that the patient found to be most helpful in decreasing NSSI, and discussing obstacles to maintaining gains after treatment. Any recurrences of NSSI are emphasized as an opportunity to reevaluate the antecedents and consequences of NSSI, as well as the use, function, and effectiveness of alternative behaviors, through a functional assessment.
Therapists for this study were four graduate students from a clinical psychology doctoral program who were trained and supervised by the first author, a licensed psychologist and developer of T-SIB. Training consisted of discussion of the T-SIB treatment manual, review of the techniques used in the intervention, and ongoing supervision. Supervision occurred weekly with the first author to discuss ongoing cases, review the treatment manual, and review recorded treatment sessions as necessary.
Treatment as Usual
In order to make the TAU condition as ecologically valid as possible, participants randomly assigned to this condition were given a list of mental health services in the community and offered assistance in finding a provider and scheduling an intake appointment. When contacted at each assessment point, researchers asked participants whether they were receiving mental health treatment, and if they were not, again offered referrals and assistance in making appointments. Participants in the TAU condition were encouraged, but not required, to receive mental health treatment, and given the scarcity of NSSI treatment providers, NSSI was not required to be a focus of treatment. Participants in the TAU condition were offered the intervention upon completion of the follow up assessment. One participant completed T-SIB after the TAU condition; outcomes following T-SIB for this participant randomized to the TAU condition were not included in the present analyses.
Measures
Structured Clinical Interview for the DSM-IV, Axis I, Non-Patient Version (SCID-I; First et al., 1995)
The SCID-I was used to assess DSM-IV Axis I diagnoses at baseline for mood, substance use, anxiety, and eating disorders, as well as psychotic symptoms. Interrater reliability with trained interviewers for the SCID-I is high (.70 to 1.00; Andover et al., 2015; First et al., 1995).
Structured Clinical Interview for the DSM-IV, Axis II Disorders (SCID-II; First et al., 1997)
The SCID-II was used to assess BPD and ASPD at baseline. The interrater reliability of the SCID-II has been supported in previous research (e.g., Maffei et al., 1997).
Modified Scale for Suicidal Ideation (MSSI; Miller et al., 1986)
The MSSI, an 18-item interview, was used to assess suicidal ideation at baseline. A score of 21 on the MSSI reflects severe levels of suicidal ideation (Miller et al., 1986) and was therefore used as an exclusion criterion for the current study.
Functional Assessment of Self-Mutilation (FASM; Lloyd, Kelly, & Hope, 1997)
The FASM is a self-report measure that assesses specific behavior characteristics and functions of NSSI. For the purpose of this study, the FASM was used to obtain information on characteristics of NSSI behaviors, specifically lifetime frequency and methods used.
Time Line Follow Back (TLFB; Sobell & Sobell, 1992)
The TLFB, a calendar-prompted interview, was used to assess NSSI, which was defined as deliberate injury to the body involving tissue damage performed in the absence of suicidal intent. In the current study, the number of NSSI behaviors (NSSI frequency) and the number of days on which the participant reported that an NSSI behavior occurred (NSSI days) were assessed. The TLFB has demonstrated excellent reliability and validity in alcohol research (Sobell & Sobell, 1992) and has been successfully used to assess NSSI (Andover et al., 2015; Glenn & Klonsky, 2011). The TLFB was administered at baseline (following back four weeks), five weeks after the baseline assessment (following back five weeks), post-treatment (following back four weeks), and at 3-month follow up (following forward 12 weeks from the post-treatment assessment).
Client Satisfaction Questionnaire (CSQ-8; Attkisson & Zwick, 1982)
The CSQ-8 was administered to those in the treatment condition at the post-treatment to assess patient satisfaction with the intervention. Scores on the CSQ-8 range from 8 to 32, with increasing scores indicating increasing satisfaction. Researchers have reported high validity and reliability for the CSQ-8 (Attkisson & Zwick, 1982).
Results
We first investigated differences between the T-SIB and TAU conditions on demographic and clinical variables. As shown in Table 2, there were no significant differences between conditions in demographics, clinical variables assessed at baseline, or NSSI behaviors in the month prior to the baseline assessment. Participants in both conditions were encouraged, but not required, to participate in mental health treatment other than T-SIB; there were no significant differences in receiving other psychotherapy between conditions at any time point.
Feasibility
Recruitment was first examined in order to evaluate the feasibility of the treatment and RCT (See Figure 1.). Ninety individuals responded to advertisements for the research study over the course of three years, 72 of whom completed a telephone screen. Fourteen (19.4%) were not interested in the study after receiving more information (n = 6; 8.3%) or unable to participate due to geographic distance from the treatment site (n = 8; 11.1%). Sixteen (22.2%) did not meet one or more inclusion criteria for the study. Of the 42 individuals scheduled for a baseline assessment, 38 (90.5%) attended this appointment. Four (10.5%) were not eligible to participate (MSSI > 21, n = 3, 7.9%; no NSSI behaviors or urges during the past month, n = 1, 2.6%), and one (2.6%) declined participation without providing a reason. The remaining 33 participants were enrolled in the research study and randomized to T-SIB (n = 15; 45.5%) or TAU (n = 18; 54.5%).
Figure 1.
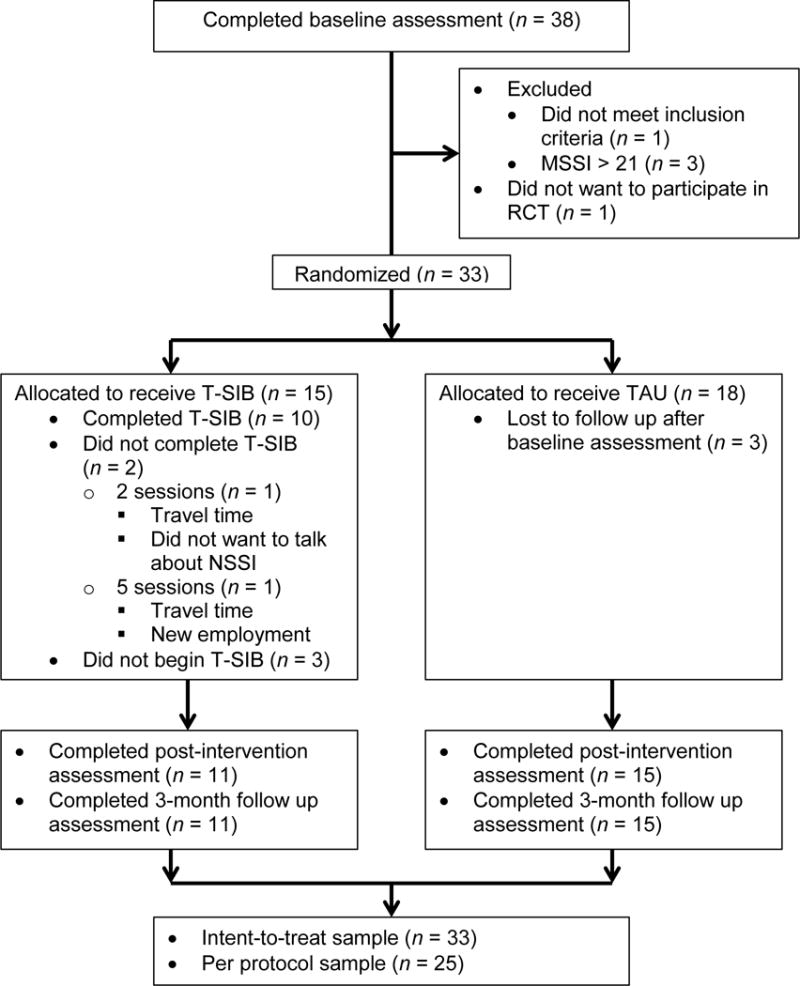
Flowchart of patient enrollment and disposition.
Treatment Adherence and Satisfaction
Seven participants were lost to follow up (T-SIB: n = 4, 26.7%; Control: n = 3, 16.7%; χ2 (1, n = 33) = 0.49, p = .48, Φ = .12; see Figure 1). There were no differences in demographic variables, clinical variables, or NSSI frequency or days between those lost to follow up and study completers, all ps > .23. Of the 15 participants randomly assigned to the T-SIB condition, three (20.0%) could not be contacted to schedule the first session. Only two participants (13.3%) withdrew from the intervention after attending the first session. One withdrew after two sessions but completed post-intervention and follow up assessments, and one withdrew after five sessions and did not complete post-intervention or follow up assessments. Reasons for withdrawal from the intervention included travel time to and from the treatment site, scheduling difficulties due to new employment, and not wanting treatment for NSSI behaviors. The remaining 10 participants (66.7%) completed all nine 1-hour sessions. The mean number of sessions attended for all T-SIB participants was 6.47 (SD = 3.39). There were no significant differences between those assigned to T-SIB who completed the intervention and those who did not withdrew or did not begin the intervention in demographic variables, clinical variables, or NSSI frequency or days, all ps > .26. Overall, participants assigned to the T-SIB condition reported high satisfaction with the intervention on the CSQ8 (M = 28.64, SD = 3.98). Participants reported that the most helpful parts of treatment were the functional assessments (n = 2), identification of alternative activities (n = 2), and the non-judgmental approach of the intervention (n = 1).
A measure of therapist adherence to the intervention was developed for three of the nine sessions in the manual, Sessions 1, 2, and 9, selected because they included the most required components of the intervention. This measure consisted of a checklist indicating whether the specific session components and goals were covered. Therapist adherence was assessed on 20.6% of all sessions (n = 20), selected at random. Therapists were found to be 97.5% adherent to the intervention manual.
Statistical Analyses
Data were analyzed using SPSS 22. Intent-to-treat (ITT) analyses were conducted with all participants randomized to intervention and control conditions. Analyses involving differences between groups at baseline were conducted with t-tests and chi-square analyses. Analyses of condition differences over time for each outcome measure were conducted with linear mixed models using restricted maximum likelihood (REML) estimation with a random intercept and slope for subject. In each model, a variance components (CV) structure was specified to model the covariance structure of the random effect, and a heterogeneous first-order autoregressive (ARH1) structure was specified to model the covariance structure of the repeated effect. Cohen’s d effect sizes of the difference between conditions, as well as area under the curve (AUC) effect sizes of the probability that a randomly chosen member of the TAU condition scored higher than a randomly chosen member of the T-SIB condition (e.g., Kraemer, Morgan, Leech, Gliner, Vaske, & Harmon, 2003), were calculated for each week, beginning with one baseline week prior to the start of the study. The main effects of Condition and Week and the Condition × Week interaction were entered as fixed effects. Linear mixed effects models were then repeated using a per-protocol (PP) sample, which included participants who attended all nine intervention sessions, utilizing a maximum likelihood (ML) estimation with a random intercept and slope for subject.
Change in NSSI Behaviors
Although the study was underpowered to detect treatment efficacy, an initial examination of change in NSSI behaviors by condition was conducted. Mixed effects models were used to investigate differences by condition over the last week of baseline and the course of the intervention and follow up period (21 weeks total) using an ITT approach. For NSSI frequency, there were no significant main effects of Condition, F(1, 3399.19) = 0.79, p = .37, Week, F(21, 91.55) = 0.94, p = .54, or their interaction, F(21, 91.55) = 0.99, p = .48 (See Figure 2.). However, medium effect sizes were noted from the sixth week of treatment (when participants are first asked to change behavior) to the last week of follow up (Week 21), all ds = 0.48 – 0.57 (AUCs = .63 – .68). For number of NSSI days, there was a significant main effect for Week, F(21, 75.36) = 2.20, p = .007, but not for Condition, F(1, 40.85) = 0.32, p = .58, or the Condition × Week interaction, F(21, 75.36) = 1.18, p = .29 (See Figure 3.). Small effect sizes were found for Weeks 8 and 9, ds = 0.27 and 0.33, respectively, Weeks 11–13, ds = 0.21 – 0.23, and Weeks 18–21, ds = 0.21–0.30, in the expected direction of fewer NSSI days reported by the T-SIB condition (AUCs for Weeks 6–21 = .53 – .59).
Figure 2.
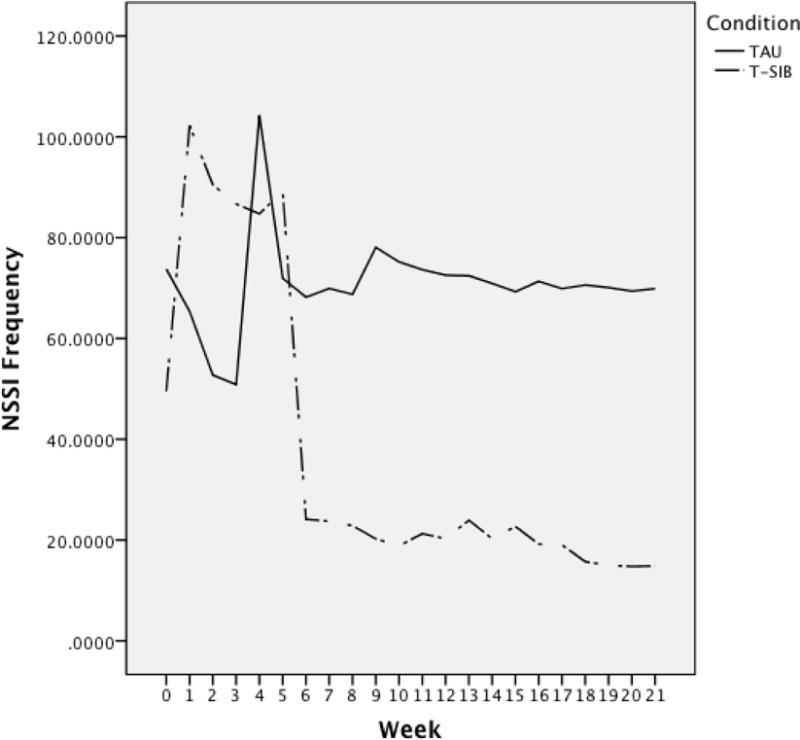
Frequency of NSSI behaviors over baseline (Week 0), treatment (Weeks 1–9), and follow up period (Weeks 10–21).
Figure 3.
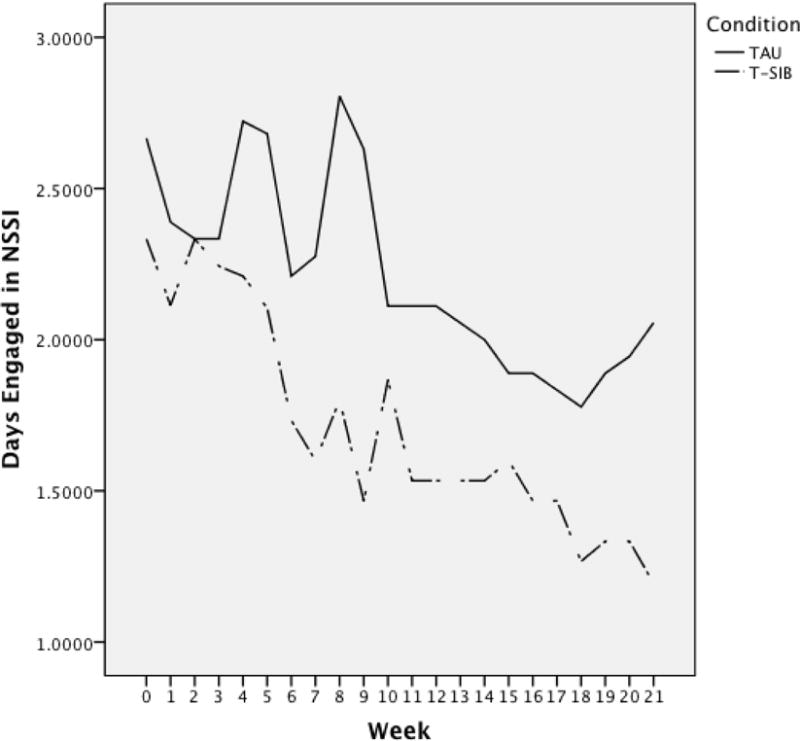
NSSI days over baseline (Week 0), treatment (Weeks 1–9), and follow up period (Weeks 10–21).
We also completed per protocol analyses, including only those participants who completed the full nine sessions of the T-SIB intervention (n = 10). Maximum likelihood (ML) estimates were used given the exploratory nature of these analyses. For NSSI frequency, a significant Condition × Week interaction was found, F(21, 3231.47) = 1.64, p = .03. A non-significant trend was noted for Week, F(21, 3231.47) = 1.49, p = .07, and no main effect for Condition was found, F(1, 8.73) = 0.01, p = .92. Effect sizes were small to medium from Week 6 of the intervention throughout the follow up period, ds = 0.27–0.48 (AUCs = .58 – .63). For number of NSSI days, the main effect of Week was significant, F(21, 16.32) = 3.77, p = .004, but neither the main effect of Condition, F(1, 32.05) = 1.15, p = .29, nor the Condition × Week interaction, F(21, 16.32) = 1.19, p = .36, were significant. However, effect sizes from Week 7 throughout the follow up period were small to medium, ds = 0.23–0.64 (AUCs = .57 – .67).
Discussion
The prevalence of NSSI among young adults is significant, and the behavior is associated with medical, psychological, and social consequences ranging in severity. However, no treatments specific to NSSI have been developed outside the context of BPD, and research on the effectiveness of these interventions in a non-BPD sample is limited. The purpose of this study was to further investigate the feasibility and acceptability, as well as an initial investigation of change in NSSI behavior, in a pilot RCT of the Treatment of Self-Injurious Behavior (T-SIB), a brief intervention specifically developed to treat NSSI behaviors in a transdiagnostic sample. Thirty-three participants were assigned to receive T-SIB or TAU using an urn randomization procedure. Feasibility of the study was supported; over the course of three years, nearly 60% of individuals responding to advertisements for the study met inclusion criteria upon initial screening, and nearly 90% of those completing a baseline assessment were eligible to participate in the study. The acceptability of the study and the treatment were also supported by the numbers of participants who were lost to follow up and who withdrew from the T-SIB intervention. The remaining participants assigned to T-SIB were adherent with the intervention, completing all nine one-hour sessions. Participants who completed the intervention reported high levels of satisfaction. In addition, they reported the main components of the intervention (i.e., functional assessments and identification of alternative behaviors) as the most helpful aspects of treatment.
Although sample sizes were likely too small to detect significant differences between conditions, changes in NSSI frequency and number of days the participant reported engaging in NSSI over the course of the intervention and follow up period were examined between the T-SIB and TAU conditions using ITT analyses. Although there were no significant differences between conditions in weekly reported NSSI frequency or days, medium or “typical” effect sizes (Kraemer et al., 2003; p. 1525) for differences in NSSI frequency were found between conditions beginning in week 6 of the intervention, the importance of which is discussed below. Small effect sizes between conditions were found for number of NSSI days, but overall the number of NSSI days significantly decreased over time for both conditions. In addition to Cohen’s d, AUC was calculated as a measure of effect size, as it is considered to be a more direct indicator of clinical significance (Kraemer et al., 2003). Results of the AUC with ITT analyses suggest that on average over the 3-month follow up period, a participant in the T-SIB condition would report less NSSI frequency than a participant in the TAU condition 65% of the time, and fewer NSSI days 56% of the time. Results with the per protocol sample were similar, with a significant decrease in NSSI frequency for the T-SIB group over time, and small to medium effects beginning at the sixth week of the intervention. Although the number of NSSI days decreased over time for both groups, small to medium effects in favor of the T-SIB condition were noted. Using the per protocol sample, a participant in the T-SIB condition would report less NSSI frequency and fewer NSSI days than a participant in the TAU condition an average of 61% of the time over the 3-month follow up period.
We first detected medium effect sizes for decreased NSSI behavior among the T-SIB condition in Week 6 of the intervention; these effect sizes then continued until the end of the follow up period. The timing of the initial detection of this medium effect is notable, as Week 6 is the first week of the intervention where patients are asked to change their NSSI behaviors. The first five weeks of the intervention consist of functional assessments to identify NSSI antecedents and consequences, as well as identifying and testing alternative behaviors in response to minor stressors in preparation for behavior change; participants are not asked to change their NSSI behavior during this time. The detection of a medium effect at Week 6 is consistent with the intervention and supports the role of T-SIB in behavior change.
It is important to note that a significant main effect for Week was found for number of NSSI days in both the ITT and per protocol analyses; for NSSI frequency, a non-significant trend was found in the per protocol sample only. This indicates that number of days the participant reported engaging in NSSI each week decreased over time for all participants, regardless of condition. There are several potential reasons for this finding. First, participants in both conditions were motivated for treatment, as they responded to recruitment materials advertising an intervention for NSSI. Regardless of condition, participants may have actively attempted to decrease their NSSI behaviors. Second, ongoing assessment and monitoring of NSSI behaviors in the TAU condition may have led to a decrease in NSSI as awareness of the behavior or perceived accountability increased. Finally, participants in the TAU condition were given mental health referrals at their initial assessment and encouraged to seek treatment. Half of participants in the TAU condition received outpatient treatment at some point during the study period, and 27.8% reported that NSSI was discussed at some point during treatment; this treatment may have led to a decrease in NSSI.
The authors of this study chose a TAU condition as the study’s control group. Half of participants in the TAU condition received outside outpatient therapy at some point during the study period; NSSI was addressed in some way during this therapy in a quarter of participants in the TAU condition. The type or quality of treatment or emphasis on NSSI in the treatment was not controlled. Reasons for the decision to use a TAU control condition were twofold. First, exclusion criteria for the study only included severe suicidal ideation and active psychosis. Participants therefore ranged in severity of mental health symptoms, which indicated that a TAU condition would be preferable to a no-treatment or waitlist condition. Second, given that empirically supported treatments for NSSI are limited, a TAU condition would reflect the treatments currently available to individuals seeking treatment for the behavior. However, future studies may choose to utilize an active control condition consisting of a treatment that has shown promise in decreasing NSSI behavior, such as DBT or ERGT. Similarly, 53.3% of participants in the T-SIB condition received other outpatient therapy at some point during the study period; NSSI was addressed in some way during this therapy in 13.3% of participants. As T-SIB was designed as either a stand-alone or adjunctive intervention, the proportion of participants in other outpatient therapy reflects the intended purpose of the intervention. However, studies may wish to restrict other psychotherapy among participants in the experimental condition in the future to determine the specific contribution of T-SIB relative to other psychotherapy in the reduction of NSSI behavior.
Results of this study must be interpreted in light of the study’s limitations. First, the study was underpowered to detect group differences in NSSI behaviors. However, the small sample size was consistent with the study’s aim of conducting a Stage I pilot RCT to determine the feasibility and acceptability of such a study in order to inform a larger RCT consistent with Stage II behavioral therapies research (Rounsaville, Carroll, & Onken, 2001). The results of the current study support the further investigation of T-SIB in a larger RCT based on effect sizes, as well as feasibility and acceptability. Future RCTs should also investigate potential moderators of the treatment effect, such as NSSI characteristics, severity of emotion dysregulation, or concurrent engagement in T-SIB and other outpatient psychotherapy, which were beyond the scope of the current paper. Second, there was considerable variability in reported NSSI frequency among participants. This was expected given that severity and frequency of NSSI were not specified as inclusion criteria for the study, and some participants will report greater frequency NSSI behaviors compared with others; however, the large variance may have affected the results of this study. Although the randomization procedure was designed to stratify based on NSSI frequency, the frequency chosen a priori was relatively low given the actual frequency reported by the sample. A future RCT may choose to stratify randomization based on an NSSI frequency that is more reflective of the sample of interest or based on severity of NSSI behaviors.
The purpose of this study was to further investigate T-SIB, a brief intervention designed specifically to address NSSI behaviors among young adults. An experimental condition was compared to a TAU condition in a small pilot RCT with the aims of examining study and intervention feasibility and acceptability and providing a preliminary investigation of change in NSSI behaviors between conditions. Inclusion and exclusion criteria were kept purposefully broad in order to enhance generalizability of the findings. The data support the feasibility and acceptability of the study. Medium effect sizes for decreased NSSI frequency in the T-SIB condition were found using ITT analyses, and using the per protocol sample, NSSI frequency significantly decreased over time in the T-SIB condition compared with the TAU condition. Adherence to the intervention manual was high among therapists in the study, who were students in a clinical psychology doctoral program. Although it is necessary to further investigate the use of T-SIB by other service providers, this suggests that clinicians, even those who may be relatively inexperienced or not familiar with NSSI, can be trained in the intervention. Given the prevalence of NSSI in both clinical and community samples, as well as the transdiagnostic nature of the behavior, a brief, non-resource-intensive intervention that is specific to NSSI but not specific to diagnosis is necessary but currently lacking. Together, this study supports investigating the T-SIB intervention in a larger RCT that is adequately powered to detect significant differences between conditions.
Public Health Significance.
A novel intervention for non-suicidal self-injury was compared to treatment as usual in a pilot randomized controlled trial (RCT). The feasibility and acceptability of the treatment and study design were supported. Medium effect sizes for decreased NSSI behaviors among the T-SIB condition add support for a larger RCT to further evaluate the intervention.
Acknowledgments
Author’s Note: This research was supported by National Institute of Mental Health Grant K23MH082824.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Author; Arlington, VA: 2013. [Google Scholar]
- Andover MS. Non-suicidal self-injury disorder in a community sample of adults. Psychiatry Research. 2014;219:305–310. doi: 10.1016/j.psychres.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andover MS, Morris BW. Expanding and clarifying the role of emotion regulation in nonsuicidal self-injury. Canadian Journal of Psychiatry. 2014;59:569–575. doi: 10.1037/t01029-000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andover MS, Pepper CM, Ryabchenko KA, Orrico EG, Gibb BE. Self-mutilation and symptoms of depression, anxiety, and borderline personality disorder. Suicide & Life-Threatening Behavior. 2005;35:581–591. doi: 10.1521/suli.2005.35.5.581. [DOI] [PubMed] [Google Scholar]
- Andover MS, Schatten HT, Morris BW, Miller IW. Development of an intervention for nonsuicidal self-injury in young adults: An open pilot trial. Cognitive and Behavioral Practice. 2015;22:491–503. doi: 10.1016/j.cbpra.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attkisson CC, Zwick R. The Client Satisfaction Questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning. 1982;5:233–237. doi: 10.1016/0149-7189(82)90074-X. [DOI] [PubMed] [Google Scholar]
- Bracken-Minor KL, McDevitt-Murphy ME. Differences in features of non-suicidal self-injury according to borderline personality disorder screening status. Archives of Suicide Research. 2014;18:88–103. doi: 10.1080/13811118.2013.809040. [DOI] [PubMed] [Google Scholar]
- Bohus M, Haaf B, Simms T, Limberger MF, Schmahl C, Unckel C, Linehan M. Effectiveness of inpatient dialectical behavioral therapy for borderline personality disorder: A controlled trial. Behaviour Research and Therapy. 2004;42:487–499. doi: 10.1016/S0005-7967(03)00174-8. [DOI] [PubMed] [Google Scholar]
- Comtois KA. A review of interventions to reduce the prevalence of parasuicide. Psychiatric Services. 2002;53:1138–1144. doi: 10.1176/appi.ps.53.9.1138. [DOI] [PubMed] [Google Scholar]
- Comtois KA, Linehan MM. Psychosocial treatments of suicidal behaviors: A practice-friendly review. Journal of Clinical Psychology. 2006;62:161–170. doi: 10.1002/jclp.20220. [DOI] [PubMed] [Google Scholar]
- Evans K, Tyrer P, Catalan J, Schmidt U, Davidson K, Dent J, Thompson S. Manual-assisted cognitive-behaviour therapy (MACT): A randomized controlled trial of a brief intervention with bibliotherapy in the treatment of recurrent deliberate self-harm. Psychological Medicine. 1999;29:19–25. doi: 10.1017/S003329179800765X. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbons M, Spitzer RL, Williams J. User’s Guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington DC: American Psychiatric Press; 1997. [Google Scholar]
- First M, Spitzer R, Williams J, Gibbons M. Structured Clinical Interview for DSM-IV–Patient version. New York: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- Fischer S, Peterson C. Dialectical behavior therapy for adolescent binge eating, purging, suicidal behavior, and non-suicidal self-injury: A pilot study. Psychotherapy. 2015;52:78–92. doi: 10.1037/a0036065. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. Prospective prediction of nonsuicidal self-injury: A 1-year longitudinal study in young adults. Behavior Therapy. 2011;42:751–762. doi: 10.1016/j.beth.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL. Risk factors for and functions of deliberate self-harm: An empirical and conceptual review. Clinical Psychology: Science and Practice. 2003;10:192–205. doi: 10.1093/clipsy/bpg022. [DOI] [Google Scholar]
- Gratz KL. Targeting emotion dysregulation in the treatment of self-injury. Journal of Clinical Psychology: In Session. 2007;63:1091–1103. doi: 10.1002/jclp.20417. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Conrad SD, Roemer L. Risk factors for deliberate self-harm among college students. American Journal of Orthopsychiatry. 2002;72:128–140. doi: 10.1037/0002-9432.72.1.128. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Gunderson JG. Preliminary data on an acceptance-based emotion regulation group intervention for deliberate self-harm among women with borderline personality disorder. Behavior Therapy. 2006;37:25–35. doi: 10.1016/j.beth.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT. Extending research on the utility of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality pathology. Personality Disorders: Theory, Research, and Treatment. 2011;2:316–326. doi: 10.1037/a0022144. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Levy R. Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychological Medicine. 2014;44:2099–2112. doi: 10.1017/S0033291713002134. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Dixon-Gordon KL, Chapman AL, Tull MT. Diagnosis and characterization of DSM-5 nonsuicidal self-injury disorder using the Clinician-Administered Nonsuicidal Self-Injury Disorder Index. Assessment. 2015;22:527–539. doi: 10.1177/1073191114565878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Society for the Study of Self-Injury. Fast facts. 2016 Retrieved from http://itriples.org/redesadmin15/fast-facts/
- Kliem S, Kröger C, Kosfelder J. Dialectical behavior therapy for borderline personality disorder: A meta-analysis using mixed-effects modeling. Journal of Consulting and Clinical Psychology. 2010;78:936–951. doi: 10.1037/a0021015. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. Journal of Abnormal Psychology. 2013;122:231–237. doi: 10.1037/a0030278. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Morgan GA, Leech NL, Gliner JA, Vaske JJ, Harmon RJ. Measures of clinical significance. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:1524–1529. doi: 10.1097/00004583-200312000-00022. [DOI] [PubMed] [Google Scholar]
- Labelle R, Pouliot L, Janelle A. A systematic review and meta-analysis of cognitive behavioral treatments for suicidal and self-harm behaviours in adolescents. Canadian Psychology. 2015;56:368–378. doi: 10.1037/a0039159. [DOI] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, Lindenboim N. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006 doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Lloyd EE, Kelley ML, Hope T. Self-mutilation in a community sample of adolescents: Descriptive characteristics and provisional prevalence rates. Poster presented at the annual meeting of the Society for Behavioral Medicine; New Orleans, LA: 1997. [Google Scholar]
- Maffei C, Fossati A, Agostoni I, Barraco A, Bagnato M, Deborah D, Petrachi M. Interrater reliability and internal consistency of the Structured Clinical Interview for DSM-IV Axis II personality disorders (SCID-II), version 2.0. Journal of Personality Disorders. 1997;11:279–284. doi: 10.1521/pedi.1997.11.3.279. [DOI] [PubMed] [Google Scholar]
- Miller IW, Norman WH, Bishop SB, Dow MG. The Modified Scale for Suicidal Ideation: Reliability and validity. Journal of Consulting and Clinical Psychology. 1986;54:724–725. doi: 10.1037/0022-006X.54.5.724. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ. Self-injurious behavior as a separate clinical syndrome. American Journal of Orthopsychiatry. 2005;75:324–333. doi: 10.1037/0002-9432.75.2.324. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ. Empirically supported treatments and general therapy guidelines for non-suicidal self-injury. Journal of Mental Health Counseling. 2006;28:166–185. [Google Scholar]
- Muehlenkamp JJ, Gutierrez PM. An investigation of differences between self-injurious behavior and suicide attempts in a sample of adolescents. Suicide and Life-Threatening Behavior. 2004;34:12–23. doi: 10.1521/suli.34.1.12.27769. [DOI] [PubMed] [Google Scholar]
- Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiatry Research. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Nock MK, Teper R, Hollander M. Psychological treatment of self-injury among adolescents. Journal of Clinical Psychology: In Session. 2007;63:1081–1089. doi: 10.1002/jclp.20415. [DOI] [PubMed] [Google Scholar]
- Pasieczny N, Connor J. The effectiveness of dialectical behavior therapy in routine public mental health settings: An Australian controlled trial. Behavior Research and Therapy. 2011;49:4–10. doi: 10.1016/j.brat.2010.09.006. [DOI] [PubMed] [Google Scholar]
- Pistorello J, Fruzzetti AE, MacLane C, Gallop R, Iverson KM. Dialectical behavior therapy (DBT) applied to college students: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2012 doi: 10.1037/a0029096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees CS, Hasking P, Breen LJ, Lipp OV, Mamotte C. Group mindfulness based cognitive therapy vs group support for self-injury among young people: study protocol for a randomised controlled trial. BMC Psychiatry. 2015;15:154–161. doi: 10.1186/s12888-015-0527-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from Stage I. Clinical Psychology: Science and Practice. 2001;8:133–142. doi: 10.1093/clipsy/8.2.133. [DOI] [Google Scholar]
- Salkovskis PM, Atha C, Storer D. Cognitive-behavioural problem solving in the treatment of patients who repeatedly attempt suicide: A controlled trial. British Journal of Psychiatry. 1990;157:871–876. doi: 10.1192/bjp.157.6.871. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-Back: A technique for assessing self-reported alcohol consumption. In: Allen RJ, editor. Measuring Alcohol Consumption. New Jersey: Humana Press Inc; 1992. [Google Scholar]
- Stanley B, Brodsky B, Nelson JD, Dulit R. Brief dialectical behavior therapy (DBT-B) for suicidal behavior and non-suicidal self-injury. Archives of Suicide Research. 2007;11:337–341. doi: 10.1080/13811110701542069. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distributions of prognostic factors in treatment outcome research. Journal of Studies on Alcohol. 1994;(Suppl 12):70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Turner BJ, Austin SB, Chapman AL. Treating nonsuicidal self-injury: A systematic review of psychological and pharmacological interventions. The Canadian Journal of Psychiatry. 2014;59:576–585. doi: 10.1177/070674371405901103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrer P, Thompson S, Schmidt U, Jones V, Knapp M, Davidson K, Wessely S. Randomized controlled trial of brief cognitive behavior therapy versus treatment as usual in recurrent deliberate self-harm: The POPMACT study. Psychological Medicine. 2003;33:969–976. doi: 10.1017/S0033291703008171. [DOI] [PubMed] [Google Scholar]
- van den Bosch LMC, Koeter MWJ, Stijnen T, Verheul R, van den Brink W. Sustained efficacy of dialectical behavior therapy for borderline personality disorder. Behaviour Research and Therapy. 2005;43:1231–1241. doi: 10.1016/j.brat.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Verheul R, van den Bosch LMC, Koeter MWJ, de Ridder MAJ, Stijnen T, van den Brink W. Dialectical behaviour therapy for women with borderline personality disorder: 12-month, randomized clinical trial in the Netherlands. British Journal of Psychiatry. 2003;182:135–140. doi: 10.1192/bjp.182.2.135. [DOI] [PubMed] [Google Scholar]
- Wei LJ, Lachin JM. Properties of the urn randomization in clinical trials. Controlled Clinical Trials. 1988;9:345–364. doi: 10.1016/0197-2456(88)90048-7. [DOI] [PubMed] [Google Scholar]
- Weinberg I, Gunderson JG, Hennen J, Cutter CJ. Manual assisted cognitive treatment for deliberate self-harm in borderline personality disorder patients. Journal of Personality Disorders. 2006;20:482–492. doi: 10.1521/pedi.2006.20.5.482. [DOI] [PubMed] [Google Scholar]


