Abstract
OBJECTIVE
Older adults, those aged 65 and older, frequently require emergency care. However, only limited national data describe the Emergency Medical Services (EMS) care provided to older adults. We sought to determine the characteristics of EMS care provide to older adults in the United States.
METHODS
We used data from the 2014 National Emergency Medical Services Information System (NEMSIS), encompassing EMS response data from 46 States and territories. We excluded EMS responses for children <18 years, interfacility transports, intercepts, non-emergency medical transports and standby responses. We defined older adults as age ≥65 years. We compared patient demographics (age, sex, race, primary payer), response characteristics (dispatch time, location type, time intervals) and clinical course (clinical impression, injury, procedures, medications) between older and younger adult EMS emergency “911” responses.
RESULTS
During the study period there were 20,212,245 EMS emergency responses. Among the 16,116,219 adult EMS responses, there were 6,569,064 (40.76%) older and 9,547,155 (59.24%) younger adults. Older EMS patients were more likely to be white and the EMS incident to be located in healthcare facilities (clinic, hospital, nursing home). Compared with younger patients, older EMS patients were more likely to present with syncope (5.68% vs. 3.40%; OR 1.71; CI: 1.71–1.72), cardiac arrest/rhythm disturbance (3.27% vs. 1.69%; OR 1.97; CI: 1.96–1.98), stroke (2.18% vs. 0.74%; OR 2.99; CI: 2.96–3.02) and shock (0.77% vs. 0.38%; OR 2.02; CI: 2.00–2.04). Common EMS interventions performed on older persons included intravenous access (32.02%), 12-lead ECG (14.37%), CPR (0.87%) and intubation (2.00%). The most common EMS drugs administered to older persons included epinephrine, atropine, furosemide, amiodarone, and albuterol or ipratropium.
CONCLUSION
One of every three US EMS emergency responses involves older adults. EMS personnel must be prepared to care for the older patient.
Keywords: Emergency Medical Services, Older Adults, Geriatric, Prehospital intervention
INTRODUCTION
The population of people age over 65 years in the United States is expected to double over the next 25 years to 84 million persons.1 By 2030, older adults will comprise roughly one-fifth of the U.S population. Prior studies suggest that older adults are high users of emergency medical care at rates more than twice that of younger adults.2,3 This observation is not surprising as older patients often have multiple comorbidities and frequently present with acute medical conditions such as cardiac arrest, myocardial infarction, stroke and sepsis.4
An important component of the national emergency care system is prehospital Emergency Medical Services (EMS).5 Originally designed to optimize care of cardiac arrest and major trauma, the current system of EMS care in the United States offers specialized front line care for a range of acute conditions.6 EMS provides an important opportunity for ill and injured individuals to access the healthcare system. In the US, there are currently over 250,000 EMS providers providing care for over 30 million emergency incidents annually.7
EMS frequently provides initial emergency care for older patients. While older patients have unique medical needs, current EMS training curricula offer only limited training in geriatric care.8–11 An important first step in improving the EMS care of older persons is to understand the characteristics of these persons. However, there have been no national descriptions of EMS care provided to older patients; for example, the frequency of these prehospital patient cases, the characteristics of the patients, the nature of the clinical care episodes, the methods of management, and the corresponding outcomes. In this study we sought to determine the national characteristics of EMS care provided to older adults in the United States.
METHODS
Study Design
We analyzed data from the 2014 National Emergency Medical Services Information System (NEMSIS) public research dataset. The Institutional Review Board of the University of Alabama at Birmingham approved the study.
Study Setting and Data Source
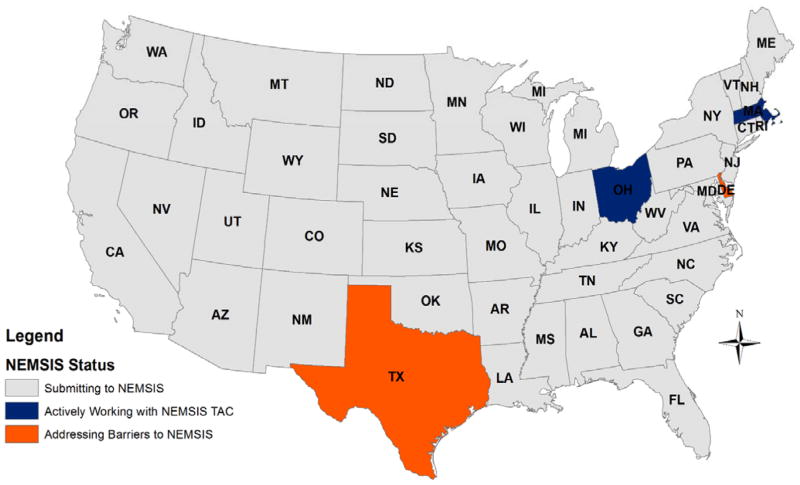
The NEMSIS project is a national effort to standardize EMS data collected by EMS personnel. The database is managed by the NEMSIS Technical Assistance Center (currently located at the University of Utah School of Medicine, Salt Lake City, UT) and supported by the Office of Emergency Medical Services of the National Highway Traffic Safety Administration. Local EMS agencies submit data to their State database for computation, of which a subset of data is then exported to the national database. Greater than 90% of the United States and its territories have a NEMSIS data system implemented. For this study, we used the 2014 NEMSIS Public Release Dataset (Version 2.2.1) which contained data on almost 26 million EMS activations in 46 states and territories. The percentage of EMS agencies providing data ranged between 42–100%, with a few states (Arizona, Kentucky, and Louisiana) providing less than 18%. The requirements for NEMSIS data reporting vary by state (Figure 1).
FIGURE 1.
States contributing data to NEMSIS.
Selection of EMS Responses
We limited the analysis to emergency “911” EMS responses, excluding all EMS intercepts, interfacility transfers, medical transports, mutual aid and standby events. We included only EMS activations responding to adults ≥18 years. We excluded all responses where the age was unknown. We defined older adults as patients of age ≥65 years old. We defined younger adults as patients of age 18–64.
Outcomes and Covariates
We compared characteristics between EMS responses for older and younger adults, including patient’s demographics, EMS response characteristics, primary clinical impression indicated by EMS personnel, procedures performed, and medications given. Demographics included age, sex, race, and primary healthcare payer. EMS responses were categorized with location type where the “911” events occurred and US Census Region. We examined transport destinations, response, scene, and transport time. We determined the variation in number of EMS events during each eight-hour periods (7:00 AM – 2:59 PM, 3:00 PM–10:59 PM, 11:00 PM–6:59 AM). We assessed commonly used EMS interventions, including intubation, intravenous access, CPAP/BiPAP, ECG, CPR, defibrillation, cardiac pacing, and cardiac monitoring. We similarly assessed commonly used medications, including antihypertensive, bronchodilator, and antiarrhythmic drugs.
Data Analysis
We compared patient demographics, EMS characteristics, clinical impressions, procedures, and medications between older and younger adults using t-tests for continuous variables, the Wilcoxon Rank-Sum test for nonparametric variables, and logistic regression for categorical variables. To account for potential confounders, where appropriate we adjusted all estimate for age, sex, race, dispatch time and census region. We analyzed all data using Stata 13.1 (Stata, Inc., College Station, TX).
RESULTS
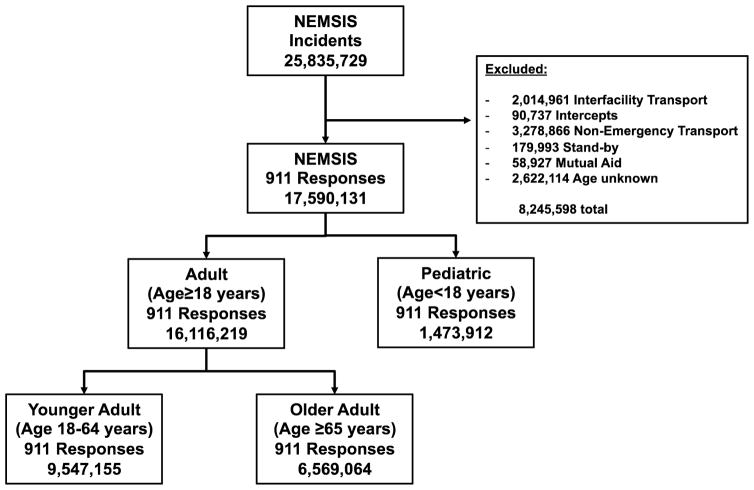
Among 25,835,729 incidents, there were 20,212,245 EMS “911” responses. (Figure 2) Among the 16,116,219 adult EMS responses, 6,569,064 (40.76%) involved older and 9,547,155 (59.24%) involved younger adults. Older adults comprised 32.5% of all EMS “911” responses.
FIGURE 2.
Study population.
Mean patient ages were 79.14 (±SD 8.82) years for older adults and 42.75 (±SD 13.87) for younger adults. (Table 1) Compared to younger adults, EMS responses for older adults were more commonly in health care facility and residential institutions. The largest proportion of EMS responses occurred in the South and the geographic distribution of EMS calls was similar for older and younger adults. The majority of EMS responses for both age group resulted in hospital transport. Median and 90-percent fractile response, on-scene, and transport times were slightly longer for older than younger adults. (Table 2)
TABLE 1.
Demographics of older (age≥65) and younger (age 18–64) EMS patients.
| Patient Characteristic | Older Adults (N=6,569,064) | Younger Adults (N =9,547,155) | Odds Ratio (95% CI) |
|---|---|---|---|
| Age – mean (SD) | 79.14 (±8.82) | 42.75 (±13.87) | |
| Sex | |||
| Male | 2,657,391 (40.5%) | 4,699,329 (49.2%) | Reference |
| Female | 3,849,735 (58.6%) | 4,760,726 (49.9%) | 1.43 (1.43–1.43) |
| Unknown | 61,938 (0.94%) | 87,100 (0.91%) | -- |
| Race | |||
| White | 4,111,229 (62.6%) | 4,459,476 (46.7%) | Reference |
| Black | 702,848 (10.7%) | 2,086,117 (21.9%) | 0.37 (0.36–0.37) |
| American Indian | 25,287 (0.4%) | 94,954 (0.7%) | 0.29 (0.28–.029) |
| Asian | 41,601 (0.6%) | 63,521 (0.7%) | 0.71 (0.70–0.72) |
| Pacific Islander | 8,631 (0.1%) | 19,734 (0.2%) | 0.47 (0.46–0.49) |
| Others | 145,879 (2.2%) | 418,498 (4.4%) | 0.38 (0.38–0.38) |
| Unknown | 1,533,589 (23.4%) | 2,404,855 (25.2%) | -- |
| Primary Payer | |||
| Private Insurance | 450,377 (6.9%) | 813,578 (8.5%) | Reference |
| Medicare | 1,273,617 (19.4%) | 410,050 (4.3%) | 5.61 (5.58–5.64) |
| Medicaid | 124,204 (1.9%) | 671,823 (7.0%) | 0.33 (0.33–0.34) |
| Self Pay | 130,030 (2.0%) | 637,702 (6.7%) | 0.37 (0.37–0.37) |
| Other | 120,630 (1.8%) | 234,112 (2.5%) | 0.93 (0.92–0.94) |
| Location Type | |||
| Home/residence | 3,845,859 (58.6%) | 4,739,541 (49.6%) | Reference |
| Farm/Mine/Quarry/ Industrial Places | 125,730 (1.9%) | 458,674 (4.8%) | 0.34 (0.34–0.34) |
| Recreation facilities/ Bodies of Water | 60,388 (0.9%) | 130,030 (1.4%) | 0.57 (0.57–058) |
| Street or highway | 295,507 (4.5%) | 1,667,183 (17.5%) | 0.22 (0.22–0.22) |
| Public building /Businesses | 256,465 (3.9%) | 1,667,183 (17.5%) | 0.30 (0.30–0.30) |
| Health care facility (clinic, hospital) | 1,051,838 (16.0%) | 668,339 (7.0%) | 1.94 (1.93–1.95) |
| Residential institution (nursing home, jail/prison) | 548,145 (8.3%) | 268,127 (2.8%) | 2.52 (2.51–2.53) |
| Unknown | 385,132 (5.9%) | 561,044 (5.9%) | -- |
| US Census Region | |||
| South | 2,763,366 (42.1%) | 4,053,835 (42.5%) | Reference |
| Midwest | 1,290,721 (19.7%) | 1,819,336 (19.1%) | 1.04 (1.04–1.04) |
| Northeast | 1,657,999 (25.2%) | 2,265,535 (23.7%) | 1.07 (1.07–1.08) |
| West | 851,393 (13.0%) | 1,398,229 (14.7%) | 0.89 (0.89–0.90) |
| Island Areas | 5,585 (0.1%) | 10,220 (0.1%) | 0.80 (0.78–0.83) |
TABLE 2.
Characteristics of EMS responses for older (age≥65) and younger (age 18–64) adult EMS patients.
| EMS Event Characteristic | Older Adults (N=6,569,064) | Younger Adults (N =9,547,155) | Unadjusted Odds Ratio (95% CI) | Adjusted Odds Ratio** (95% CI) |
|---|---|---|---|---|
| Incident Outcome | ||||
| Treated and transported by EMS | 5,366,969 (81.70%) | 7,442,913 (77.96%) | Reference | Reference |
| Treated and transported by private vehicle or law enforcement | 266,857 (4.06%) | 426,943 (4.47%) | 0.87 (0.86–0.87) | 0.97 (0.97–0.98) |
| Treated and released | 182,592 (2.78%) | 341,371 (3.58) | 0.74 (0.74–0.75) | 0.94 (0.93–0.94) |
| Dead on scene, cancelled, or not found | 140,225 (2.13%) | 161,742 (1.69%) | 1.20 (1.19–1.21) | 1.27 (1.26–1.28) |
| No treatment required | 185,816 (2.83%) | 268,077 (2.81%) | 0.96 (0.96–0.97) | 1.15 (1.14–1.16) |
| Patient refused care | 426,605 (6.49%) | 906,109 (9.49%) | 0.65 (0.65–0.66) | 0.89 (0.88–0.89) |
| Transport Destination | ||||
| Hospital | 5,092,091 (77.52%) | 7,313,187 (76.60%) | Reference | Reference |
| Residential | 150,724 (2.29%) | 70,343 (0.74%) | 3.08 (3.05–3.11) | 3.12 (3.09–3.15) |
| Clinic | 38,343 (0.58%) | 37,960 (0.40%) | 1.45 (1.43–1.47) | 1.62 (1.60–1.65) |
| Morgue | 5,381 (0.08%) | 6,284 (0.07%) | 1.23 (1.19–1.28) | 1.17 (1.13–1.22) |
| Other | 89,022 (1.36%) | 126,054 (1.32%) | 1.01 (1.00–1.02) | 1.01 (1.00–1.02) |
| Unknown | 1,193,503 (18.17%) | 1,993,327 (20.88%) | 0.86 (0.86–0.86) | 0.86 (0.86–0.86) |
| Event Dispatch Time | ||||
| 7AM—2:59PM | 2,614,248 (39.8%) | 3,254,769 (34.1%) | Reference | Reference |
| 3:00PM—10:59PM | 2,543,838 (38.7%) | 3,867,871 (40.5%) | 0.82 (0.82–0.82) | 0.83 (0.83–0.84) |
| 11:00PM—6:59PM | 1,410,978 (21.5%) | 2,424,515 (25.4%) | 0.725 (0.72–0.73) | 0.74 (0.74–0.74) |
| Time Intervals (min) (median, IQR) | ||||
| Response time (Unit en route to arrival on scene | 6 (4–9) | 5 (3–9) | P<0.01* | P<0.01* |
| Scene time (on scene to depart scene) | 16 (12–22) | 13 (9–19) | P<0.01* | P<0.01* |
| Transport time (depart scene to hospital arrival) | 12 (7–19) | 11 (7–18) | P<0.01* | P<0.01* |
| 90% Fractal Time (min) | ||||
| Response time (Unit en route to arrival on scene) | 14 min | 13 min | ||
| Scene time (on scene to depart scene) | 29 min | 26 min | ||
| Transport time (depart scene to hospital arrival) | 29 min | 27 min | ||
Significance determined by Wilcoxon rank-sum test.
Adjusted for race, gender, dispatch time, and US census region
EMS care for older adults more likely involved critical illnesses such as respiratory distress/arrest, syncope, cardiac arrest/rhythm disturbance, stroke, shock, hyper/hypothermia, airway obstruction, and diabetic symptoms. (Table 3) Older adults were more likely to receive resuscitation measures including intravenous access, cardiac monitoring, 12-lead electrocardiogram, cardiopulmonary resuscitation, defibrillation, cardiac pacing, CPAP/BiPAP, bag-valve-mask ventilation, intubation or, supraglottic airway insertion. (Table 4)
TABLE 3.
Clinical impressions of EMS responses for older (age≥65) and younger (age 18–64) adult EMS patients.
| Clinical Impression | Older adults (N=6,569,064) | Younger Adults (N =9,547,155) | Unadjusted Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|---|
| Traumatic Injury | 715,391 (10.9%) | 1,297,932 (13.6%) | Reference | Reference |
| Environmental Toxin (Poison, bite, smoke) | 26,303 (0.40%) | 377,756 (3.96%) | 0.13 (0.13–0.13) | 0.13 (0.13–0.14) |
| Neurological disorders (Altered consciousness, psychiatric disorder, seizure) | 488,294 (7.4%) | 1,213,683 (12.7%) | 0.73 (0.73–0.73) | 0.75 (0.74–0.75) |
| Abdominal pain/problem | 377,292 (5.7%) | 702,687 (7.4%) | 0.97 (0.97–0.98) | 1.00 (0.99–1.00) |
| Cardiovascular Emergency (shock, stroke, syncope, chest pain) | 907,306 (13.81%) | 988,474 (10.35) | 1.67 (1.66–1.67) | 1.68 (1.67–1.69) |
| Cardiac arrest/rhythm | 214,671 (3.3%) | 161,058 (1.7%) | 2.42 (2.40–2.44) | 2.47 (2.45–2.49) |
| Diabetic symptoms | 124,492 (1.9%) | 173,895 (1.8%) | 1.30 (1.29–1.31) | 1.44 (1.43–1.45) |
| Other | 86,323 (1.31%) | 191,690 (2.01%) | 0.82 (0.81–0.82) | 0.85 (0.84–0.85) |
| Airway Emergency (anaphylaxis, respiratory distress, airway obstruction) | 594,081 (9.04%) | 538,151 (5.64%) | 2.00 (1.99–2.01) | 2.04 (2.03–2.05) |
| Unknown | 3,034,911 (46.2%) | 3,901,799 (40.9%) | 1.41 (1.41–1.42) | 1.44 (1.43–1.44) |
Adjusted for race, gender, dispatch time, and US census region
TABLE 4.
Procedures performed on older (age≥65) and younger (age 18–64) adult EMS patients.
| Procedure | Older Adults (N=6,569,064) | Younger Adults (N =9,547,155) | Unadjusted Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|---|
| Cardiac | 2,695,594 (41.0%) | 3,262,088 (34.2%) | 1.34 (1.34–1.34) | 1.33 (1.32–1.33) |
| Cardiac Monitor | 1,332,942 (20.3%) | 1,582,801 (16.6%) | 1.28 (1.28–1.28) | 1.27 (1.26–1.27) |
| ECG (12–Lead) | 943,695 (14.4%) | 909,365 (9.5%) | 1.59 (1.59–1.60) | 1.58 (1.58–1.59) |
| Defibrillation (automated, manual, cardioversion) | 41,888 (0.6%) | 45,188 (0.5%) | 1.35 (1.33–1.37) | 1.40 (1.38–1.42) |
| CPR | 57,273 (0.9%) | 53,980 (0.6%) | 1.55 (1.53–1.57) | 1.65 (1.63–1.67) |
| Cardiac pacing | 4,075 (0.06%) | 1,940 (0.02%) | 3.05 (2.89–3.22) | 3.17 (3.00–3.35) |
| Pulmonary | 999,051 (15.2%) | 1,281,559 (13.4%) | 1.16 (1.15–1.16) | 1.18 (1.18–1.19) |
| Bag-Valve-Mask Ventilation | 24,024 (0.4%) | 29,906 (0.3%) | 1.17 (1.15–1.19) | 1.20 (1.18–1.22) |
| CPAP and BiPAP | 42,959 (0.7%) | 21,130 (0.2%) | 2.97 (2.92–3.02) | 3.08 (3.03–3.13) |
| Intubation | 131,689 (2.0%) | 132,492 (1.4%) | 1.45 (1.44–1.46) | 1.43 (1.42–1.44) |
| Supraglottic Airway | 13,696 (0.2%) | 14,986 (0.2%) | 1.33 (1.30–1.36) | 1.39 (1.36–1.43) |
| Cricothyroidotomy | 113 (0.00%) | 241 (0.00%) | 0.7 (0.5–0.9) | 0.67 (0.53–0.84) |
| Other | ||||
| Intravenous access | 2,103,728 (32.0%) | 2,543,388 (26.6%) | 1.30 (1.30–1.30) | 1.26 (1.25–1.26) |
Adjusted for race, gender, dispatch time, and US census region
Nitroglycerin, epinephrine (1:10,000), and albuterol/ipratropium were the most commonly used medications among older EMS patients. Older adults were more likely than younger patients to receive cardiac and pulmonary medications. (Table 5)
TABLE 5.
Medications given to older (age≥65) and younger (age 18–64) adult EMS patients.
| Medications | Older Adults (N=6,569,064) | Younger Adults (N =9,547,155) | UnadjustedOdds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|---|
| Antiemetic | 139,325 (2.12%) | 242,115 (2.54%) | 0.83 (0.83–0.84) | 0.75 (0.75–0.76) |
| Ondansetron | 134,031 (2.0%) | 231,538 (2.4%) | 0.84 (0.83–0.84) | 0.76 (0.75–0.76) |
| Promethazine | 5,715 (0.09%) | 11,398 (0.12%) | 0.73 (0.71–0.75) | 0.65 (0.63–0.67) |
| Analgesics | 311,771 (4.75%) | 513,953 (5.38%) | 0.88 (0.87–0.88) | 0.85 (0.84–0.85) |
| Fentanyl | 66,912 (1.0%) | 120,242 (1.3%) | 0.81 (0.80–0.81) | 0.73 (0.720.74) |
| Morphine | 45,153 (0.7%) | 81,203 (0.9%) | 0.81 (0.80–0.82) | 0.74 (0.73–0.75) |
| Aspirin | 199,878 (3.0%) | 316,213 (3.3%) | 0.92 (0.91–0.92) | 0.92 (0.92–0.93) |
| Cardiac | 267,259 (4.07%) | 336,323 (2.52%) | 1.16 (1.6–1.17) | 1.18 (1.17–1.18) |
| Nitroglycerine | 182,857 (2.8%) | 264,888 (2.8%) | 1.00 (1.00–1.01) | 1.01 (1.00–1.01) |
| Epinephrine 1:10000 | 50,397 (0.8%) | 46,959 (0.5%) | 1.56 (1.54–1.58) | 1.69 (1.67–1.71) |
| Intravenous Fluids | 515,182 (7.84%) | 621,381 (6.51%) | 1.22 (1.22–1.23) | 1.20 (1.20–1.21) |
| Normal Saline | 434,429 (6.6%) | 531,932(5.6%) | 1.20 (1.19–1.21) | 1.16 (1.16–1.17) |
| Dextrose (50%) | 68,538 (1.0%) | 76,704 (0.8%) | 1.30 (1.29–1.32) | 1.44 (1.42–1.45) |
| Lactated Ringers | 14,691 (0.2%) | 24,802 (0.3%) | 0.86 (0.84–0.88) | 0.88 (0.87–0.90) |
| Pulmonary (DuoNeb) | 1,478,499 (22.51%) | 1,403,404 (14.70%) | 1.69 (1.68–1.69) | 1.67 (1.67–1.67) |
| Paralytics | 5,099 (0.08%) | 9,456 (0.10%) | 0.78 (0.76–0.81) | 0.78 (0.75–0.80) |
| Sedatives | 23,372 (0.36%) | 72,668 (0.76%) | 0.47 (0.46–0.47) | 0.46 (0.46–0.47) |
Adjusted for race, gender, dispatch time, and US census region
DISCUSSION
The provision of care to the growing population of older persons is one of the most important challenges facing the US health care system. Our study affirms that older persons pose similar challenges to the US EMS care system. Older patients comprised 1 of every 3 EMS emergency responses, yet presented more frequently with life threatening conditions. Older patients also more frequently required life-saving interventions and medications. These results illuminate the burden of older patients on the national EMS system and the need for prehospital practitioners to be prepared for the unique needs of these patients.
Our findings support prior analyses of EMS care of older adults. Platts-Mill, et al showed that EMS usage in North Carolina increased with age; 60.6% of adults over 85 arrived to the ED via EMS transport.12 Ross, et al demonstrated in a 3-year retrospective study in Victoria, Austria that 82.8% response of older adult resulted in a transport to the hospital.13 Dickinson, et al examined 2,712 older EMS patients treated in Colonie, New York, finding that older patients were 2.6 times more likely to be transported for cardiovascular emergencies.4 The authors also found that 54% of older patients required Advanced Life Support interventions, in contrast with 33% of younger patients.4 In a cohort of 930 older patients at an urban university hospital ED, Shah, et al. identified main reasons for EMS use including age ≥85, deficiencies in activities of daily living (ADL), and poor physical or social functioning.2 Shah, et al used 1997–2002 data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) to characterize Emergency Department use by older adults arriving by EMS.3 The authors found that older patients were more likely to have circulatory and respiratory system diagnoses, were more likely to be admitted to the hospital (52.9% vs. 29.1%), admitted to the ICU (7.9% vs. 3.1%) or to die in the ED (3.0% vs. 0.11%). They also found that older adults were more likely to receive ED services including diagnostic services and procedures, and less likely to be given medication.3 Our study supports these finding, with a high rate (93%) of older patients undergoing hospital transport, the common use of advanced procedures, intravenous fluids and medication in the older population.
While not directly addressed by our study, these observations imply the importance of preparing EMS personnel to care for the older patient. Physical examination is difficult in the out-of-hospital environment and may be particularly difficult with older patients, who are known to have atypical physical presentations.14 Older patients often have multiple comorbidities and use multiple medications, heightening the risk of potentially harmful drug interactions; our observations underscore that older persons are more likely to require acute life-saving or medicinal EMS interventions.15,16 The sensitive and frail physique of older patients is important as patient lifting, handling and transportation are important components of EMS care. Communication is commonly difficult in the out-of-hospital environment and may be more challenging with older patients, who may exhibit declines in hearing and cognition, or who may become easily disoriented when taken out of familiar environments and exposed to excessive stimulation.11,17
While the challenges of older patients are well known to healthcare personnel in inpatient and long-term care settings, EMS personnel awareness of these factors is relatively limited. The traditional emergency care model emphasizes diagnostic and therapeutic medical decision-making but fails to address the subtleties that come with geriatric care.16 Prior versions of the national EMS curriculum have presented only limited information on the assessment and care of the geriatric patient.18 Since the 1998 curriculum, the updated 2009 curricula have incorporated information on the physiological change of age, pharmacokinetic, psychosocial, geriatric specific pathological changes and protocols for specific conditions.19 However, the geriatric curriculum for an EMT and EMR are limited to basic age-related variation in assessment, management and physiology. The advanced EMT curriculum has a special section for geriatric care, but only addresses fluid resuscitation.20–22 Additional relevant training may potentially encompass communication techniques with older patients, strategies for managing acute agitation and delirium in the elderly, and the psychosocial aspects of aging. One possibility is requiring all EMS training to incorporate the Advanced Geriatric Education for EMS (GEMS) created by the partnership of National Association of Emergency Medical Technicians and American Geriatric Society. This course builds on the standard GEMS core course by integrating more complex, realistic scenarios and unique technology EMS practitioners are likely to encounter when assessing, treating and transporting older adults.23 EMS providers may also benefit from clinical exposure to geriatric care settings such as nursing homes and long-term care facilities.
LIMITATIONS
NEMSIS does not include information from all states. However, the version of NEMSIS used in this analysis is national in scope and included EMS calls from 46 states. NEMSIS is an archive of EMS activations and not a data set of individual patients receiving care. Multiple emergency resources may respond to the same call, resulting in different submission by multiple different EMS agencies. Currently, no procedures are in place to link the different reports to the same patient or EMS response. Nevertheless, when considering relationships in the database (e.g., percentages between groups), NEMSIS findings may approximate findings if patient counts were known. For example, if considering the percentage of patients that are “older adults”, there is little reason to believe that the probability of a specific EMS response structure (e.g., single-tier verses dual-tier) would systematically differ, by patient age. Thus, if the bias is unrelated the measure of interest, differences in percentages may be less affected. We did not have information on patient severity. We focused on emergency EMS responses, excluding intercepts, interfacility transfers, non-emergency medical transports, mutual aid and standbys. Data for certain events may have been missing, potentially biasing individual observations. Furthermore, each state has their own rules on what must be reported creating variability in data being reported. This could affect the generalizability of the results.
We defined older age using a defined age cutoff, but the characteristics of aging may vary continuously with age. Measures of functional status and frailty may better characterize the physical capacity of individual patients but were not available. Our study provided insights regarding the EMS care provided to older persons but not their hospital course or outcomes. We also could not ascertain the necessity of the interventions provided to patients. Missing data may have resulted from higher patient severity.
CONCLUSION
In this large, nationally representative sample, we found that older adults comprised one-third of all EMS emergency responses. Older patients were more likely to have serious health outcomes such as stroke, death, and shock. Older adults were more likely to require life-saving interventions and cardiovascular medications. EMS personnel must be prepared to address the unique needs of older patients.
Footnotes
Reprints not available from the authors.
Contributor Information
Hieu V. Duong, University of Alabama School of Medicine.
Lauren Nicholas Herrera, University of Alabama School of Medicine.
Justin Xavier Moore, Department of Emergency Medicine, University of Alabama School of Medicine. Department of Epidemiology, School of Public Health, University of Alabama at Birmingham.
John Donnelly, Department of Emergency Medicine University of Alabama School of Medicine.
Karen E. Jacobson, Department of Pediatrics, University of Utah School of Medicine.
Jestin N. Carlson, Department of Emergency Medicine, University of Pittsburgh. Department of Emergency Medicine, Stain Vincent Health System.
N. Clay Mann, Department of Pediatrics, University of Utah School of Medicine.
Henry E. Wang, Department of Emergency Medicine, University of Alabama School of Medicine.
References
- 1.Ortman JM, Veikoff VA, Hogan H. An Aging Nation: The Older Population in the United States. 2014 [Google Scholar]
- 2.Shah MN, Glushak C, Karrison TG, Mulliken R, Walter J, Friedmann PD, Hayley DC, Chin MH. Predictors of emergency medical services utilization by elders. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2003;10(1):52–58. doi: 10.1111/j.1553-2712.2003.tb01976.x. [DOI] [PubMed] [Google Scholar]
- 3.Shah MN, Bazarian JJ, Lerner EB, Fairbanks RJ, Barker WH, Auinger P, Friedman B. The epidemiology of emergency medical services use by older adults: an analysis of the National Hospital Ambulatory Medical Care Survey. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2007;14(5):441–447. doi: 10.1197/j.aem.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 4.Dickinson ET, Verdile VP, Kostyun CT, Salluzzo RF. Geriatric use of emergency medical services. Annals of emergency medicine. 1996;27(2):199–203. doi: 10.1016/s0196-0644(96)70323-2. [DOI] [PubMed] [Google Scholar]
- 5.Savage SM, Donaldson LA, Cherian S, Chilukuri R, White VA, Sopori ML. Effects of cigarette smoke on the immune response. II. Chronic exposure to cigarette smoke inhibits surface immunoglobulin-mediated responses in B cells. Toxicology and applied pharmacology. 1991;111(3):523–529. doi: 10.1016/0041-008x(91)90256-e. [DOI] [PubMed] [Google Scholar]
- 6.United States Department of Transportation. National Highway Traffic Safety Administration. [Accessed Oct 10, 2016];Education Agenda for the Future: A Systems Approach. 2010 http://www.ems.gov/pdf/education/EMS-Education-for-the-Future-A-Systems-Approach/EMS_Education_Agenda.pdf.
- 7.National EMS Information System. 2014 National Emergency Medical Services Information System. 2014. Salt Lake City, UT: 2014. [Google Scholar]
- 8.Shah MN, Rajasekaran K, Sheahan WD, 3rd, Wimbush T, Karuza J. The effect of the geriatrics education for emergency medical services training program in a rural community. Journal of the American Geriatrics Society. 2008;56(6):1134–1139. doi: 10.1111/j.1532-5415.2008.01738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah MN, Caprio TV, Swanson P, Rajasekaran K, Ellison JH, Smith K, Frame P, Cypher P, Karuza J, Katz P. A novel emergency medical services-based program to identify and assist older adults in a rural community. Journal of the American Geriatrics Society. 2010;58(11):2205–2211. doi: 10.1111/j.1532-5415.2010.03137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shah MN, Swanson PA, Nobay F, Peterson LK, Caprio TV, Karuza J. A novel internet-based geriatric education program for emergency medical services providers. Journal of the American Geriatrics Society. 2012;60(9):1749–1754. doi: 10.1111/j.1532-5415.2012.04112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peterson LK, Fairbanks RJ, Hettinger AZ, Shah MN. Emergency medical service attitudes toward geriatric prehospital care and continuing medical education in geriatrics. Journal of the American Geriatrics Society. 2009;57(3):530–535. doi: 10.1111/j.1532-5415.2008.02108.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Platts-Mills TF, Leacock B, Cabañas JG, Shofer FS, McLean SA. Emergency Medical Services Use by the Elderly: Analysis of a Statewide Database. Prehospital Emergency Care. 2010;14(3):329–333. doi: 10.3109/10903127.2010.481759. [DOI] [PubMed] [Google Scholar]
- 13.Ross L, Jennings PA, Smith K, Williams B. Paramedic Attendance to Older Patients in Australia, and the Prevalence and Implications of Psychosocial Issues. Prehospital Emergency Care. 2017;21(1):32–38. doi: 10.1080/10903127.2016.1204037. [DOI] [PubMed] [Google Scholar]
- 14.Esmer E, Derst P, Lefering R, Schulz M, Siekmann H, Delank KS. Prehospital assessment of injury type and severity in severely injured patients by emergency physicians : An analysis of the TraumaRegister DGU(R) Der Unfallchirurg. 2016 doi: 10.1007/s00113-015-0127-3. [DOI] [PubMed] [Google Scholar]
- 15.Carpenter CR, Shah MN, Hustey FM, Heard K, Gerson LW, Miller DK. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. The journals of gerontology. Series A, Biological sciences and medical sciences. 2011;66(7):775–783. doi: 10.1093/gerona/glr040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carpenter CR, Platts-Mills TF. Evolving prehospital, emergency department, and “inpatient” management models for geriatric emergencies. Clinics in geriatric medicine. 2013;29(1):31–47. doi: 10.1016/j.cger.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yorkston KM, Bourgeois MS, Baylor CR. Communication and aging. Physical medicine and rehabilitation clinics of North America. 2010;21(2):309–319. doi: 10.1016/j.pmr.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.United States Department of Transportation. National Highway Traffic Safety Administration. [Accessed Oct 10, 2016];EMT-Paramedic: National Standard Curriculum. 1998 https://www.ems.gov/pdf/education/Emergency-Medical-Technician-Paramedic/Paramedic_1998.pdf.
- 19.United States Department of Transportation. National Highway Traffic Safety Administration. [Accessed Oct 10, 2016];National Emergency Medical Services Education Standards: Paramedic Instructional Guidelines. 2009 http://www.ems.gov/pdf/education/National-EMS-Education-Standards-and-Instructional-Guidelines/Paramedic_Instructional_Guidelines.pdf.
- 20.United States Department of Transportation. National Highway Traffic Safety Administration. National Emergency Medical Services Education Standards: Advanced Emergency Medical Technician Instructional Guidelines. 2009 http://www.ems.gov/pdf/education/National-EMS-Education-Standards-and-Instructional-Guidelines/ADV_EMT_Instructional_Guidelines.pdf.
- 21.United States Department of Transportation. National Highway Traffic Safety Administration. National Emergency Medical Services Education Standards: Emergency Medical Responder Instructional Guidelines. 2009 http://www.ems.gov/pdf/education/National-EMS-Education-Standards-and-Instructional-Guidelines/EMR_Instructional_Guidelines.pdf.
- 22.Myles PR, Hubbard RB, Gibson JE, Pogson Z, Smith CJ, McKeever TM. The impact of statins, ACE inhibitors and gastric acid suppressants on pneumonia mortality in a UK general practice population cohort. Pharmacoepidemiology and drug safety. 2009;18(8):697–703. doi: 10.1002/pds.1769. [DOI] [PubMed] [Google Scholar]
- 23.Education N. Geriatric Education for EMS (GEMS) 2017;2017 https://www.naemt.org/docs/default-source/education-documents/gems/gems-and-gems-advanced_2016.pdf?sfvrsn=0. [Google Scholar]