Abstract
Background and Aims
The implications of the rapid rise in electronic cigarette (e-cigarette) use remain unknown. We examined mutual associations between e-cigarette use, conventional cigarette use, and nicotine dependence over time to 1) test the association between e-cigarette use and later conventional smoking (both direct and via nicotine dependence), 2) test the converse associations, and 3) determine the strongest pathways predicting each product’s use.
Design
Data from 4 annual waves of a prospective cohort study were analyzed. Path analysis modeled the bi-directional, longitudinal relationships between past-month smoking frequency, past-month e-cigarette frequency, and nicotine dependence.
Setting
Chicago area, Illinois, USA.
Participants
N=1007 young adult smokers and nonsmokers (ages 19–23).
Measurements
Frequency of 1) cigarettes and 2) e-cigarettes was the number of days in the past 30 on which the product was used. The Nicotine Dependence Syndrome Scale measured nicotine dependence to cigarettes.
Findings
E-cigarette use was not significantly associated with later conventional smoking, either directly (β=0.021, p=.081) or through nicotine dependence (β=0.005, p=.693). Conventional smoking was positively associated with later e-cigarette use, both directly (β=0.118, p<.001) and through nicotine dependence (β=0.139, p<.001). The strongest predictors of each product’s use was prior use of the same product; this pathway was strong for conventional cigarettes (β=0.604, p<.001) but weak for e-cigarettes (β=0.120, p<.001). Nicotine dependence moderately strongly predicted later conventional smoking (β=0.169, p<.001), but was a weak predictor of later e-cigarette use (β=0.069, p=.039).
Conclusions
Nicotine dependence is not a significant mechanism for e-cigarettes’ purported effect on heavier future conventional smoking among young adults. Nicotine dependence may be a mechanism for increases in e-cigarette use among heavier conventional smokers, consistent with e-cigarettes as a smoking reduction tool. Overall, conventional smoking, and to a lesser extent its resulting nicotine dependence, are the strongest drivers or signals of later cigarette and e-cigarette use.
INTRODUCTION
Electronic cigarette (e-cigarette) use has shown a drastic and rapid increase in recent years in the United States, especially among youth, which is accompanied by a decline in conventional cigarette use (1, 2). In fact, e-cigarette use has far surpassed conventional cigarette use among some groups (2), and is perceived as the least risky of all substances (1). The lack of long-term data for this recent trend has led to considerable debate about e-cigarettes’ impact on overall tobacco use and addiction.
In particular, some have raised concerns about e-cigarettes acting as a “gateway” (3) to conventional tobacco use (2, 4–6). For example, 10–40% of adolescent e-cigarette users have never tried a conventional cigarette (2, 7), and adolescents who initiate with e-cigarettes are 2–3 times more likely to use conventional cigarettes in the future (8, 9). Using these and similar statistics, some have concluded that e-cigarettes represent a real public health risk due to subsequent increased tobacco use, possibly via increased nicotine dependence (10–13). However, with limitations of available data, it remains unclear whether e-cigarettes attract distinct, new populations of tobacco users (10, 12, 13), or whether e-cigarette users are already, or would have been, users of conventional cigarettes anyway (14). Another possibility is that e-cigarettes may divert from conventional cigarettes, in (not necessarily successful) attempts to reduce or quit smoking (15, 16), or even for primary prevention of conventional smoking (17).
A vital, yet understudied, element of e-cigarettes’ impact is nicotine dependence. Nicotine dependence remains a primary driver of chronic tobacco use (18, 19), and is assumed to be a mediator between e-cigarette use and conventional smoking in several of these hypotheses. For example, most versions of the “gateway” hypothesis postulate that the development of nicotine dependence via e-cigarettes promotes later conventional smoking (3); and harm reduction hypotheses implicitly assume that nicotine dependence drives consumption of some form of tobacco product (17, 20, 21). However, the common, underlying hypothesis of nicotine dependence as a mediator has not been rigorously tested to our knowledge. A further complicating factor is the mutual dependency among tobacco use and nicotine dependence (22, 23), which makes it difficult to isolate individual pathways (e.g. whether tobacco use drives nicotine dependence more than nicotine dependence drives tobacco use) using conventional analyses.
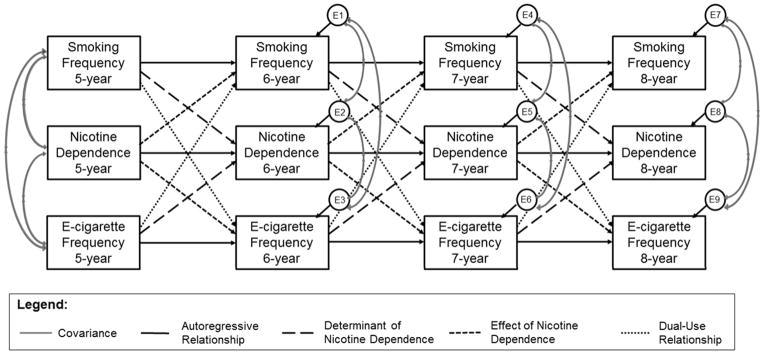
The current study examines the longitudinal relationships between conventional cigarette use, e-cigarette use, and nicotine dependence using a path analysis model, a version of structural equation modeling. All possible autoregressive (same variable predicting itself in the future) and cross-lagged (a variable predicting another variable in the future) relationships among these variables were modeled across 4 time waves (Figure 1), using data from a longitudinal cohort of young adult novice/light smokers and nonsmokers (regular e-cigarette use was rare among this sample). This type of model offers substantial benefits over standard regression analyses in that it parses out different components of a relationship and allows for bi-directional associations, rather than artificially imposing a one-directional relationship. This study aimed to test 1) whether e-cigarette use is associated with (positive or negative) differences in later conventional smoking, either directly or through nicotine dependence as a mediator; 2) whether conventional cigarette use is associated with differences in later e-cigarette use, either directly or via nicotine dependence; and 3) the relative strengths of the pathways predicting e-cigarette and conventional cigarette use.
Figure 1. Full path analysis model.
Observed variables are shown in rectangles and unobserved variables (error terms) are shown in circles. Similar variables are presented in rows, and variables from the same assessment wave are shown in columns. Gray, curved lines represent covariances. Straight lines represent regression relationships, and are organized into categories based on line type.
METHODS
Sample
Data were drawn from the previously described Social and Emotional Contexts of Adolescent Smoking Patterns (SECASP) Study (24). Briefly, 9th and 10th grade students at 16 high schools in the greater Chicago metropolitan area were given a brief screener survey; all novice (<100 cigarettes/lifetime) and current “light smokers” (under ≤5 cigarettes/day), as well as random samples of non-smokers, were invited to participate. Of 3,654 students invited, 1263 provided their own or their parent’s consent, and completed the baseline survey in 2006.
Follow-up surveys were administered approximately annually over 8 years after the baseline survey. Due to questions about e-cigarettes not being present in earlier waves, the current study uses data from the 5-, 6-, 7-, and 8-year follow up surveys (approximate ages 19.6–23.6). Retention at 5 years after baseline was 81.2% (N=1026), and at 8 years was 79.7% (N=1007). Females had higher retention at 8 years than males (86.7% vs. 70.4%, p<.001). Those who were missing at 8 years reported more frequent smoking at baseline (M=4.8 vs. 3.6 days in the past 30, p=.032). Nicotine dependence had a high proportion of missing data which increased over time (approximately 34–47%). Demographic and smoking characteristics for the sample are shown in Table 1.
Table 1.
Demographic and Smoking Characteristics for Analytic Sample (N=1007)
| Characteristic | Summary a | Number of Individuals with Missing Dataa |
|---|---|---|
| Smoking status at baseline | 0 (0.0%) | |
| Nonsmoker | 190 (18.9%) | |
| Experimenter b | 704 (69.9%) | |
| Light smoker c | 113 (11.2%) | |
|
| ||
| Sex | 0 (0.0%) | |
| Female | 621 (61.7%) | |
| Male | 386 (38.3%) | |
|
| ||
| Race/ethnicity | 0 (0.0%) | |
| White | 744 (73.9%) | |
| Non-White | 263 (26.1%) | |
|
| ||
| Age at 8-year follow-up | 23.6 (0.6) | 0 (0.0%) |
|
| ||
| Past-month smoking frequency | ||
| Any smoking in past month | ||
| 5-year follow-up | 504 (54.1%) | 76 (7.5%) |
| 6-year follow-up | 492 (51.3%) | 48 (4.8%) |
| 7-year follow-up | 468 (48.3%) | 38 (3.8%) |
| 8-year follow-up | 402 (39.9%) | 0 (0.0%) |
| Among recent smokers, # days smoked/30 | ||
| 5-year follow-up | 20 (5 – 30) | 76 (7.5%) |
| 6-year follow-up | 24 (5 – 30) | 48 (4.8%) |
| 7-year follow-up | 25 (6 – 30) | 38 (3.8%) |
| 8-year follow-up | 25 (7 – 30) | 0 (0.0%) |
|
| ||
| Past-month e-cig frequency | ||
| Any e-cig use in past month | ||
| 5-year follow-up | 63 (6.8%) | 77 (7.6%) |
| 6-year follow-up | 86 (9.1%) | 62 (6.2%) |
| 7-year follow-up | 170 (17.8%) | 52 (5.2%) |
| 8-year follow-up | 108 (10.7%) | 0 (0.0%) |
| Among recent users, # days used/30 | ||
| 5-year follow-up | 1.5 (1.5 – 1.5) | 77 (7.6%) |
| 6-year follow-up | 1.5 (1.5 – 7.5) | 62 (6.2%) |
| 7-year follow-up | 1.5 (1.5 – 7.5) | 52 (5.2%) |
| 8-year follow-up | 7.5 (1.5 – 7.5) | 0 (0.0%) |
|
| ||
| Nicotine Dependence Syndrome Scale Score | ||
| 5-year follow-up | 1.4 (1 – 2.4) | 341 (33.9%) |
| 6-year follow-up | 1.4 (1 – 2.5) | 370 (36.7%) |
| 7-year follow-up | 1.5 (1.0 – 2.6) | 413 (41.0%) |
| 8-year follow-up | 1.7 (1.0 – 2.7) | 477 (47.3%) |
Categorical variables are summarized as N (valid percentage) and continuous variables are summarized as median (interquartile range).
Smoked under 100 cigarettes/lifetime, and includes both former experimenters (did not smoke in the past 90 days; N=244) and current experimenters (smoked in the past 90 days; N=460).
Smoked 100 cigarettes/lifetime or more and smoked within the past 30 days, but smoked 5 or fewer cigarettes per day.
Measures
Conventional cigarette use was measured with past-month smoking frequency at each wave (“Now think about the past 30 days. On how many days did you smoke or try cigarettes?”) Original response categories were 0, 1, 2–3, 4–5, 6–7, 8–10, 11–20, 21–29, and all 30 days. This was coded as a numeric variable using the midpoint of each category.
E-cigarette use was also measured with past-month frequency of use at each wave (“During the past 30 days, on how many days did you use e-cigarettes?”). Original response categories were 1–2, 3–5, 6–9, 10–19, 20–29, and all 30 days. This was coded as a numeric variable using the midpoint of each category, and those who did not use e-cigarettes were coded as 0.
Nicotine dependence symptoms were measured using a version of the Nicotine Dependence Syndrome Scale (NDSS) (25) which was psychometrically validated for use in adolescent cigarette smokers (26, 27) and was shortened to 10 items that mainly reflect “drive” and “tolerance” subscales. These 10 items were assessed on a 4-point scale and were averaged into a combined NDSS score. Participants who did not report smoking at least 1 puff in their lifetime were coded as the minimum NDSS score.
Analyses
First, we examined the stability of both e-cigarette use and dual use (e-cigarettes and conventional cigarettes together) by analyzing the proportion of users reporting past-month use across each wave.
A cross-lagged model examining the bi-directional relationships between smoking behavior, e-cigarette use, and nicotine dependence across 4 waves of data collection (5-, 6-, 7-, and 8-year follow-up assessments) was constructed as a path analysis model in AMOS, version 23.0.0. Between each pair of consecutive waves, 3 autoregressive relationships and 6 cross-lagged relationship between each combination of smoking frequency, e-cigarette frequency, and NDSS were modeled (Figure 1). Due to considerations of model parsimony, other risk factors were not included, and all variables were modeled as observed rather than latent variables.
Standardized coefficients were obtained by running models on normalized variables, in order to allow comparison of regression coefficients across different paths. AMOS automatically handles missing data through full-information maximum likelihood (FIML): all information from available variables (e.g. mean, variance) is used to estimate a likelihood function for each participant (28). FIML assumes missing-at-random (MAR) data given all other variables in the model, a correct model, and normally-distributed residuals. Models were analyzed using several fit statistics. Since the χ2 goodness-of-fit index is overly sensitive to sample size, we also considered adjusted χ2 (χ2/d.f.; values under 5 indicate good fit) (29), Tucker-Lewis Index (TLI; values above 0.9 indicate good fit) (30), comparative fit index (CFI; values above 0.95 indicate good fit) (31), and the root-mean-square error of approximation (RMSEA; values under 0.06 indicate good fit (30) and values under 0.08 indicate reasonable fit (32)).
Preliminary analyses (not shown) examined nested models to test whether the regression coefficients in all paths under each category of relationships should be equal or permitted to vary across pairs of time waves, as done elsewhere (23). Based on the fit statistics, the best-fitting model was the one in which each of 9 types of relationships were constrained to be equal across consecutive waves (e.g. the regression coefficient for prior smoking behavior to later NDSS from wave 5 to 6 is equal to the regression coefficients for prior smoking behavior to later NDSS from wave 6 to 7, and wave 7 to 8).
Aim 1 was addressed by examining the cross-lagged paths from e-cigarette use to later conventional smoking and nicotine dependence; Aim 2 by the cross-lagged paths from conventional smoking to later e-cigarette use and nicotine dependence; and Aim 3 by comparing all 3 predictors for both conventional smoking and e-cigarettes.
Follow-up analyses were also performed to test the importance of each type of pathway to the overall model. The main model was compared with nested models in which the coefficients of each of the 6 cross-lagged relationships and the 3 autoregressive relationships were constrained to 0, forcing that specific relationship to be excluded from the model. Results were interpreted in terms of the χ2 difference test, in which a significant difference indicates a worse model fit. Due to the oversensitivity of χ2 to sample size, Cohen’s w effect size, where w<0.10, 0.30, and 0.50 for small, medium and large effects, respectively (33), was also calculated to quantify the effect size of the differences in models:
RESULTS
The sample contained N=299 participants who reported past-month e-cigarette use at any of the four waves. Of these, the majority (N=164, 62.8%) reported past-month use at only one wave; 76 (29.1%) reported past-month use at two waves; 16 (6.1%) reported past-month use at three waves; and only 5 (1.9%) reported past-month use at all four waves. The trends in dual use were similar: of N=254 participants who reported using both cigarettes and e-cigarettes in the past month at least one time during the four assessments, the majority (N=138, 62.1%) reported past-month dual use at only one wave; 68 (30.6%) reported past-month dual use at two waves; 13 (5.89%) reported past-month dual use at three waves; and only 3 reported past-month dual use at all four waves. Together, these trends show that while e-cigarette use increased across time, this primarily represents different users at each assessment wave, with very few consistent users.
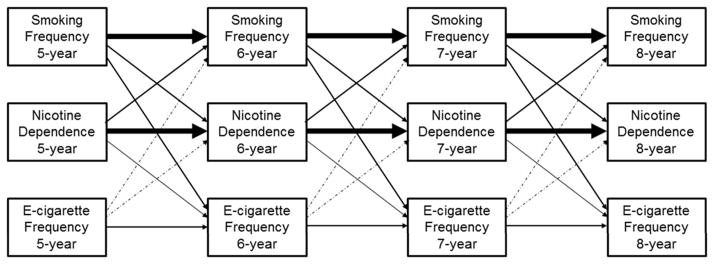
The path model demonstrated a high χ2 goodness-of-fit and adjusted χ2 (χ2(46)=384.8, χ2/d.f.=8.6, both p<.001), but several other fit indices indicated an acceptable fit (TLI=.915, CFI=.951, RMSEA=.077). Figure 2 and Table 2 present the results of the path model by displaying the magnitude of each standardized regression coefficient as line thickness. That is, the thickest lines represent the strongest relationships (prior nicotine dependence to later nicotine dependence; prior smoking frequency to later smoking frequency; and prior nicotine dependence to later smoking frequency), and the thinnest lines represent the weakest relationships (prior e-cigarette frequency to later smoking frequency; prior NDSS to later e-cigarette frequency). All paths except two (prior e-cigarette frequency to later NDSS, and prior e-cigarette frequency to later conventional smoking frequency) had significant regression coefficients (p<.05).
Figure 2. Path analysis results.
Regression coefficients are presented in proportion to line thickness (font size = 10 × β coefficient). Solid lines represent significant regression coefficients (p<.05) and dot-dash lines represent nonsignificant coefficients. For clarity, covariances and error terms are not presented here.
Table 2.
Detailed path analysis results for main modela.
| Path | β | 95% CI | p-value |
|---|---|---|---|
| Autoregressive relationships | |||
| Prior smoking freq. to later smoking freq. | 0.604 | 0.56 – 0.640.58 | <.001 |
| Prior NDSS to later NDSS | 0.629 | −0.67 | <.001 |
| Prior e-cigarette freq. to later e-cigarette freq. | 0.120 | 0.08 – 0.16 | <.001 |
|
| |||
| Determinants of nicotine dependence | |||
| Prior smoking freq. to later NDSS | 0.139 | 0.10 – 0.18 | <.001 |
| Prior e-cigarette freq. to later NDSS | 0.005 | −0.02 – 0.03 | .693 |
|
| |||
| Effects of nicotine dependence | |||
| Prior NDSS to later smoking freq. | 0.169 | 0.13 – 0.21 | <.001 |
| Prior NDSS to later e-cigarette freq. | 0.069 | 0.00 – 0.13 | .039 |
|
| |||
| Dual-use relationship | |||
| Prior smoking freq. to later e-cigarette freq. | 0.118 | 0.06 – 0.18 | <.001 |
| Prior e-cigarette freq. to later smoking freq. | 0.021 | −0.00 – 0.04 | .081 |
For each relationship category (rows) and individual type of path (sub-rows), the standardized coefficient (β), 95% confidence interval (CI), and p-value are shown based on the main model in Figure 2 (all equivalent paths are constrained to be equal across consecutive pairs of time waves). NDSS: Nicotine Dependence Syndrome Scale score. Bold: p<.05
Interpreting these results with respect to the aims of the study, e-cigarette use was weakly and non-significantly associated with later smoking behavior, both directly (β=0.021, p=.081) and mediated through nicotine dependence (β=0.005, p=.693) (Aim 1), as shown by the non-significant coefficient and small effect size for each path. In contrast, conventional smoking was weakly associated with later e-cigarette use, both directly (β=0.118, p<.001) and through nicotine dependence (β=0.139, p<.001) (Aim 2). Finally, conventional smoking was strongly predicted by prior conventional smoking (β=0.604, p<.001), and weakly-to-moderately by prior nicotine dependence (β=0.169, p<.001), while e-cigarette use was weakly predicted by prior e-cigarette use (β=0.120, p<.001), prior conventional smoking (β=0.118, p<.001), and prior nicotine dependence (β=0.069, p=.039) (Aim 3).
The nested model comparisons (Table 3) confirm the main findings of the full model. Specifically, the model fit did not suffer from eliminating the contribution of e-cigarettes to either (1) later conventional smoking (Cohen’s w=.05, p=.112) or (2) later nicotine dependence (w=.01, p=.648), indicating that these paths do not significantly contribute to the overall model. These results again fail to show that e-cigarette use is associated with changes in later conventional smoking, either directly or via nicotine dependence (Aim 1).
Table 3.
Nested model comparisons testing the contribution of each cross-lagged relationship to the full model.
| Relationship constrained to 0 | Δd.f. | Δχ2 | p | Cohen’s w |
|---|---|---|---|---|
| Autoregressive relationships | ||||
| Prior smoking freq. to later smoking freq. | 1 | 25.347 | <.001 | 0.16 |
| Prior NDSS to later NDSS | 1 | 7.811 | <.001 | 0.09 |
| Prior e-cigarette freq. to later e-cigarette freq. | 1 | 8.341 | <.001 | 0.09 |
|
| ||||
| Determinants of nicotine dependence | ||||
| Prior smoking freq. to later NDSS | 1 | 48.723 | <.001 | 0.22 |
| Prior e-cigarette freq. to later NDSS | 1 | 0.209 | .648 | 0.01 |
|
| ||||
| Effects of nicotine dependence | ||||
| Prior NDSS to later smoking freq. | 1 | 75.188 | <.001 | 0.27 |
| Prior NDSS to later e-cigarette freq. | 1 | 5.392 | .020 | 0.07 |
|
| ||||
| Dual-use relationship | ||||
| Prior smoking freq. to later e-cigarette freq. | 1 | 15.385 | <.001 | 0.12 |
| Prior e-cigarette freq. to later smoking freq. | 1 | 2.533 | .112 | 0.05 |
Bold: p<.05
Eliminating the direct effect of conventional smoking behavior on later e-cigarette use weakly but significantly worsened the model fit (w=.12, p<.001), and eliminating the mediation path through nicotine dependence yielded a slightly larger reduction in fit (w=.22, p<.001). This indicates that the direct and mediated effects of conventional smoking on later e-cigarette use (Aim 2) are important pathways in the overall model.
Finally, removing the path from prior NDSS to conventional smoking moderately worsened the model fit (w=0.27, p<.001), while removing the autoregressive path from prior smoking more weakly worsened the fit (w=0.16, p<.001). This indicates that prior NDSS and, to a lesser extent prior smoking frequency, were the most important paths predicting conventional smoking (Aim 3). Of the paths to e-cigarette use, the autoregressive path (w=0.09, p<.001) and the path emerging from prior nicotine dependence (w=0.07, p=.020) significantly worsened the model fit when removed, but removing the path from prior conventional smoking (w=0.12, p=.112) did not. This indicates that nicotine dependence and prior e-cigarette use are important pathways predicting e-cigarette use (Aim 3). Also noteworthy is the observation that the path from conventional smoking to later NDSS was important to the model, as indicated by the small-to-medium effect that their removal had on worsening the model fit (w=0.22, p<.001).
DISCUSSION
This study examined the feed-forward and reciprocal relationships of e-cigarette use, conventional smoking, and nicotine dependence across 4 years among a sample of young adult smokers and nonsmokers, with a particular interest in testing nicotine dependence as a mediator of cross-tobacco product associations. E-cigarette use was not signifcantly associated with changes in later conventional smoking, either directly or through nicotine dependence. In contrast, conventional smoking was associated with later e-cigarette use, both directly and via increased nicotine dependence. However, the most dominant relationships in the model were the autoregressive relationships, and to a lesser extent the cross-lagged relationships between conventional smoking and nicotine dependence. Together, these findings suggest that nicotine dependence mediates the transition from conventional cigarettes to e-cigarettes, but not vice versa; and that conventional smoking and nicotine dependence are the dominant pathways signaling future e-cigarette use, rather than vice versa. It is important to note that these relationships cannot be assumed to be causal, due to potential confounding by other risk factors for tobacco use.
The finding that e-cigarette use did not predict later conventional smoking and nicotine dependence raises doubts about their hypothesized effects on tobacco use. More specifically, we find no evidence for the key assumption underlying several different (often competing) accounts that nicotine dependence mediates transitions between tobacco products. For example, our findings do not validate the concern that e-cigarettes increase tobacco use via the development of nicotine dependence; nor do they support the idea that e-cigarettes are successful at decreasing conventional smoking via nicotine replacement. However, it is possible that several hypothesized mechanisms are taking place simultaneously in our sample, with some participants becoming tobacco users after becoming nicotine-addicted from e-cigarettes, others diversifying with e-cigarettes in order to reduce or quit conventional cigarettes, and still others using e-cigarettes to prevent conventional smoking altogether. Our findings are unable to test whether the null finding in the combined sample consists of such different subgroups with opposing effects.
In our overall model, conventional smoking was the strongest signal of subsequent smoking, e-cigarette use, and nicotine dependence. Notably, the pathway from conventional smoking to future e-cigarette use was mediated by nicotine dependence. This lends support to the smoking reduction and/or harm reduction hypotheses in which tobacco users transition away from conventional cigarettes to e-cigarettes. However, our findings do not support the success of this method in actually reducing subsequent conventional smoking over the time period examined.
The current study is consistent with prior research showing dual-use of e-cigarettes and conventional cigarettes among young adults (2). Additionally, these findings confirm the limited number of studies that have examined the bi-directional relationships between nicotine dependence and smoking behavior (22, 23), in showing that conventional cigarette use drives later nicotine dependence more than vice versa.
However, these findings fail to support other findings on the risks of e-cigarette use. For example, e-cigarette use has been found to predict increased conventional cigarette use in the future (8–10). One reason for this discrepancy could be that much previous research has looked at smoking initiation among adolescent e-cigarette users, while our study examines relationships between tobacco products among young adults, many of whom were established conventional smokers and did not use e-cigarettes regularly. Limitations of the current sample are further discussed below.
More generally, the current study calls into question the concerns that e-cigarettes pose a risk for later conventional smoking. For example, while those who use e-cigarettes may be more likely to initiate conventional smoking in the future (10, 12, 13), a possible explanation is that adolescents or young adults who use e-cigarettes are already using, or would have gone on to use, conventional cigarettes anyway. In support of this, overall tobacco use has remained constant among youth/late adolescents over the last several years in the U.S., despite the decrease in conventional cigarette use and concurrent increase in e-cigarette use (1). Further, the proportions of actual and potential e-cigarette users are higher among conventional smokers than among non-smokers (6, 34). This explanation is also consistent with the current findings in that the overwhelming majority of e-cigarette users in this sample also smoked conventional cigarettes concurrently. Moreover, we find no evidence that e-cigarettes increase nicotine dependence, raising doubts that e-cigarettes have a causal effect on later tobacco use through this mechanism. Taken together, these findings raise the possibility that adolescent tobacco users are increasingly initiating with e-cigarettes, possibly due to their lower perceived health risks, higher social acceptance, and easier accessibility (5, 35–37). Increased initiation with e-cigarettes may be replacing, rather than adding to, initiation with conventional cigarettes, perhaps even for primary prevention of conventional smoking (17). Further research is needed to rigorously examine this hypothesis using longitudinal data among adolescent users and non-users of tobacco.
This study also furthers the literature in important ways. Many existing studies examining dual use of conventional cigarettes and e-cigarettes fail to explicitly account for nicotine dependence, which is an important driver of future tobacco use (19, 24) and is central to the assumed mechanism underlying various accounts of e-cigarettes’ effect on conventional smoking (10–12, 17, 20, 21). Additionally, there are few longitudinal studies on e-cigarettes to date due to the recency of this trend. The current study adds significantly to this new body of literature by rigorously analyzing the mutual, positive feedback relationships between conventional cigarette use, e-cigarette use, and nicotine dependence over several time points.
Limitations
These findings should be interpreted within the context of several limitations. First, the data capture the very early years (2011–2015) of the recent rise in e-cigarette use, and the current findings may not reflect stable effects given the increasing popularity of e-cigarettes. Second, although these analysis examine temporality of relationships and impose a causal model, we cannot conclude from this analysis that significant pathways are truly causal. Third, the current study does not include other important signals and/or drivers of tobacco use such as risk-seeking behavior, risk perceptions of substances, mental health comorbidities, and other substance use. Fourth, missing data was associated with heavier prior smoking and nicotine dependence, in violation of the MAR assumption; however, follow-up analyses using multiple imputation showed very similar results (not shown). Finally, the current sample may have limited generalizability: participants were selected based on susceptibility to conventional cigarette use prior to the rise in e-cigarette usage, and are not necessarily representative of e-cigarette users in general. For example, these data contained primarily smokers among whom regular e-cigarette use was rare. Additionally, since this sample was entering early adulthood during the rise in e-cigarette use, it is possible that they were less vulnerable to any possible influences on conventional cigarette use; thus, it is possible that e-cigarettes could pose a stronger risk among younger adolescents whose tobacco use habits have not yet been formed. However, until more up-to-date longitudinal data on e-cigarettes become available, this sample is among the best available which can examine the mutual relationships between e-cigarette use, and conventional cigarette use, and nicotine dependence.
Strengths
This study has a number of strengths. First, considering the lack of existing longitudinal data on e-cigarettes, the SECASP data allow a novel and important examination of these trends among a substantial sample of young adult tobacco users across 4 years. Second, the use of path analysis to examine an autoregressive, cross-lagged model allows a separation of the many mutual relationships between these variables. This approach offers an enormous advantage over conventional analyses, which artificially impose a uni-directional relationship examining a single outcome variable.
Conclusions
This study fails to support a common hypothesis that nicotine dependence mediates the effect of e-cigarettes on future conventional smoking. By extension, this raises doubts about concerns that e-cigarettes either introduce a risk for later cigarette use via nicotine dependence. Similarly, e-cigarettes do not appear to be effective for nicotine replacement and subsequent smoking reduction/cessation, although smokers may be (unsuccessfully) using them for this purpose. Conventional smoking and nicotine dependence are the primary drivers of the overall dynamics of cigarette and e-cigarette use.
Acknowledgments
Austin Blazer for assistance in formatting and preparing the manuscript.
FUNDING
This research was funded by Project Grant P01 CA098262 from the National Cancer Institute, Project L40 DA042431 from the National Institutes on Drug Abuse, and by Center Grant P50 DA038938 awarded to Penn State University. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, NIDA, or NCI.
Footnotes
Declarations of competing interests: None to declare.
COMPETING INTERESTS
None declared.
References
- 1.Johnson LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor: 2016. [Google Scholar]
- 2.Corey CG, Wang B, Johnson SE, Apelberg B, Husten C, King BA, et al. Notes from the field: Electronic cigarette use among middle and high school students -- United States, 2011–2012. CDC; 2013. [Google Scholar]
- 3.Bell K, Keane H. All gates lead to smoking: The ‘gateway theory’, e-cigarettes and the remaking of nicotine. Soc Sci Med. 2014;119:45–52. doi: 10.1016/j.socscimed.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 4.E-cigarette use more than doubles among U.S. middle and high school students from 2011–2012 [press release]. 2013.
- 5.Choi K, Fabian L, Mottey N, Corbett A, Forster J. Young adults’ favorable perceptions of snus, dissolvable tobacco products, and electronic cigarettes: findings from a focus group study. Am J Public Health. 2012;102(11):2088–93. doi: 10.2105/AJPH.2011.300525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pepper JK, Reiter PL, McRee AL, Cameron LD, Gilkey MB, Brewer NT. Adolescent males’ awareness of and willingness to try electronic cigarettes. J Adolesc Health. 2013;52(2):144–50. doi: 10.1016/j.jadohealth.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barrington-Trimis JL, Berhane K, Unger JB, Cruz TB, Huh J, Leventhal AM, et al. Psychosocial Factors Associated With Adolescent Electronic Cigarette and Cigarette Use. Pediatrics. 2015;136(2):308–17. doi: 10.1542/peds.2015-0639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, et al. Association of Electronic Cigarette Use With Initiation of Combustible Tobacco Product Smoking in Early Adolescence. Jama. 2015;314(7):700–7. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sutfin EL, Reboussin BA, Debinski B, Wagoner KG, Spangler J, Wolfson M. The Impact of Trying Electronic Cigarettes on Cigarette Smoking by College Students: A Prospective Analysis. Am J Public Health. 2015;105(8):e83–9. doi: 10.2105/AJPH.2015.302707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, et al. E-Cigarettes and Future Cigarette Use. Pediatrics. 2016;138(1) doi: 10.1542/peds.2016-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cobb CO, Hendricks PS, Eissenberg T. Electronic cigarettes and nicotine dependence: evolving products, evolving problems. BMC medicine. 2015;13:119. doi: 10.1186/s12916-015-0355-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rennie LJ, Bazillier-Bruneau C, Rouesse J. Harm Reduction or Harm Introduction? Prevalence and Correlates of E-Cigarette Use Among French Adolescents. J Adolesc Health. 2016;58(4):440–5. doi: 10.1016/j.jadohealth.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services. E-cigarette use among youth and young adults: A report of the Surgeon General. Atlanta, GA: 2016. [Google Scholar]
- 14.Phillips CV. Gateway Effects: Why the Cited Evidence Does Not Support Their Existence for Low-Risk Tobacco Products (and What Evidence Would) Int J Environ Res Public Health. 2015;12(5):5439–64. doi: 10.3390/ijerph120505439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brose LS, Hitchman SC, Brown J, West R, McNeill A. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction. 2015;110(7):1160–8. doi: 10.1111/add.12917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Czoli CD, Hammond D, White CM. Electronic cigarettes in Canada: prevalence of use and perceptions among youth and young adults. Can J Public Health. 2014;105(2):e97–e102. doi: 10.17269/cjph.105.4119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGraw D. Current and future trends in electronic cigarette use. Int J Psychiatry Med. 2015;48(4):325–32. doi: 10.2190/PM.48.4.g. [DOI] [PubMed] [Google Scholar]
- 18.Dierker L, Hedeker D, Rose J, Selya A, Mermelstein R. Early emerging nicotine dependence symptoms in adolescence predict daily smoking in young adulthood. Drug Alcohol Depend. 2015;151:267–71. doi: 10.1016/j.drugalcdep.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piper ME, Schlam TR, Cook JW, Sheffer MA, Smith SS, Loh WY, et al. Tobacco withdrawal components and their relations with cessation success. Psychopharmacology (Berl) 2011;216(4):569–78. doi: 10.1007/s00213-011-2250-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109(11):1801–10. doi: 10.1111/add.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Le Houezec J, McNeill A, Britton J. Tobacco, nicotine and harm reduction. Drug Alcohol Rev. 2011;30(2):119–23. doi: 10.1111/j.1465-3362.2010.00264.x. [DOI] [PubMed] [Google Scholar]
- 22.Doubeni CA, Reed G, Difranza JR. Early course of nicotine dependence in adolescent smokers. Pediatrics. 2010;125(6):1127–33. doi: 10.1542/peds.2009-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Song TM, An JY, Hayman LL, Kim GS, Lee JY, Jang HL. A three-year autoregressive cross-lagged panel analysis on nicotine dependence and average smoking. Healthc Inform Res. 2012;18(2):115–24. doi: 10.4258/hir.2012.18.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dierker L, Mermelstein R. Early emerging nicotine-dependence symptoms: a signal of propensity for chronic smoking behavior in adolescents. J Pediatr. 2010;156(5):818–22. doi: 10.1016/j.jpeds.2009.11.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shiffman S, Waters A, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6(2):327–48. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- 26.Clark DB, Wood DS, Martin CS, Cornelius JR, Lynch KG, Shiffman S. Multidimensional assessment of nicotine dependence in adolescents. Drug Alcohol Depend. 2005;77(3):235–42. doi: 10.1016/j.drugalcdep.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 27.Sterling KL, Mermelstein R, Turner L, Diviak K, Flay B, Shiffman S. Examining the psychometric properties and predictive validity of a youth-specific version of the Nicotine Dependence Syndrome Scale (NDSS) among teens with varying levels of smoking. Addict Behav. 2009;34(6–7):616–9. doi: 10.1016/j.addbeh.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Modeling longitudinal and multilevel data: Practical uses, applied approaches, and specific examples. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 29.Wheaton B, Muthen B, Alwin DF, Summers GF. Assessing reliability and stability in panel models. Sociol Methodol. 1977;8:84–136. [Google Scholar]
- 30.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 31.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. [Google Scholar]
- 32.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–62. [Google Scholar]
- 33.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–9. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 34.Pearson JL, Richardson A, Niaura RS, Vallone DM, Abrams DB. e-Cigarette Awareness, Use, and Harm Perceptions in US Adults. Am J Public Health. 2012;102(9):1758–66. doi: 10.2105/AJPH.2011.300526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schneider S, Diehl K. Vaping as a Catalyst for Smoking? An Initial Model on the Initiation of Electronic Cigarette Use and the Transition to Tobacco Smoking Among Adolescents. Nicotine Tob Res. 2016;18(5):647–53. doi: 10.1093/ntr/ntv193. [DOI] [PubMed] [Google Scholar]
- 36.Peters RJ, Jr, Meshack A, Lin MT, Hill M, Abughosh S. The social norms and beliefs of teenage male electronic cigarette use. J Ethn Subst Abuse. 2013;12(4):300–7. doi: 10.1080/15332640.2013.819310. [DOI] [PubMed] [Google Scholar]
- 37.Marynak K, Baker Holmes C, King BA, Promoff G, Bunnell R, McAfee T. State laws prohibiting sales to minors and indoor use of electronic nicotine delivery systems -- United States, November 2014. CDC; 2014. [PMC free article] [PubMed] [Google Scholar]