Abstract
The literature suggests that women of different races are more or less likely to use certain contraceptive methods and patient race can influence which contraceptive recommendations a provider makes. To explore whether health care providers treat individuals of different races differently, we conducted a preliminary investigation on whether medical students recommended different contraceptive methods for hypothetical patients presenting with the same clinical features who only varied by race. Third- and fourth-year medical students (n=103) at the University of Hawai‘i completed an online survey. Students read case studies about a 23-year-old and 36-year-old patient and then made contraceptive recommendations. All students reviewed the same scenarios, with the exception of the patient's name which was randomly assigned to represent one of five racial/ethnic groups (White, Chinese, Filipina, Native Hawaiian, and Micronesian). Recommendations were analyzed using χ2 tests and bivariate logistic regressions. For the younger patient, students were most likely to recommend intrauterine devices (IUDs), followed by the contraceptive pill and Etonogestrel implant; recommendations did not differ by race/ethnicity (P = .91). For the older patient, students were most likely to recommend IUDs or sterilization, and Micronesian women were more likely to receive sterilization recommendations compared to White women (60% versus 27%, P = .04). In summary, contraceptive recommendations, specifically the frequency of recommending sterilization varied by race. Our findings add to the literature exploring the role of a patient's race/ethnicity on recommendations for contraception and highlights the need for more studies exploring the etiology of health care disparities.
Keywords: contraception, disparities, race/ethnicity, medical students, sterilization
Introduction
Despite national initiatives by organizations like the Department of Health and Human Services and the Centers for Disease Control and Prevention to provide equitable health care, race/ethnicity and socioeconomic status disparities in health outcomes persist.1–3 These disparities reflect not only systematic differences in access to high-quality care, but also the attitudes and behavior demonstrated by healthcare providers toward patients from socially disadvantaged groups.4–7 For example, race and socioeconomic status can influence a woman's contraception use and providers' recommendations of contraceptive methods.8–10 Studies have demonstrated that healthcare providers may be more likely to recommend intrauterine devices (IUDs) to Blacks, Latinas and low socioeconomic status Whites as compared to high socioeconomic status White women.8
Low access to quality healthcare can lead to an increase in unintended pregnancy, particularly among women of color. Although approximately half of all pregnancies in the United States are unintended, Black women have a rate of unintended pregnancy of 79 per 1,000 women age 15 to 44 and Hispanic women have a rate of 58 per 1,000, both are significantly higher than the rate among non-Hispanic White women (33 per 1,000).11 While the endorsement of methods like IUDs, which are long-acting and highly-effective, could reflect an effort to reduce unintended pregnancy among communities that are disparately experiencing unintended pregnancies, it could also be perceived as a method of fertility control.8,10 Women using IUDs and implants must see a health care provider to remove them and regain fertility.
In addition to encouraging the use of highly effective but reversible contraceptive methods, health care providers also perform tubal sterilizations more commonly in minority women (Black and Hispanic), and women with low-income, public insurance, and less education.12,13 This higher tubal sterilization rate may be attributable to cultural preferences among patients, insurance status, and/or racial/ethnic discrimination from providers.12–15 Highlighting the potential role of provider biases in tubal sterilization, low income racial/ethnic minority women are more likely to be advised to limit their childbearing than middle-class White women, and racial minority women have reported that sterilization prevented them from conceiving more wanted children.16–18
The majority of research examining how patient demographics may influence contraceptive recommendations has been conducted in the continental United States (US), where Whites make up 77% of the population.19 Little is known of whether biased recommendations will emerge in contexts where Whites are not the numerical majority, an important consideration given the growing diversity occurring within the US. By 2044, more than half of all individuals living in the US are projected to belong to a racial/ethnic minority group.20 Within the US, Hawai‘i provides a unique setting to examine questions related to racial diversity and majority group status as it reflects the nation's anticipated population diversity. In 2015, 73% of individuals living in Hawai‘i identified as a racial minority, with only 27% identifying as mono-racial White.19 Hawai‘i also has the nation's largest population of Native Hawaiians and Pacific Islanders in the US, comprising 26% of the population, allowing researchers to examine whether known disparities in contraceptive recommendations for Black and Hispanic women extend to women from other disadvantaged racial/ethnic minority groups.21 We sought to explore whether potential race-related biases in providers' contraceptive recommendations are present early in one's medical career, during medical school. We conducted a study of medical students' contraceptive recommendations using standardized case studies that varied only race of the patient to see if this variation affected their recommendations.
Methods
Case Studies
We presented 10 case studies with standardized descriptions of a female patient requesting a method of birth control (see Table 1). Patients in the case studies varied systematically by age (either 23- or 36-years-old), and race/ethnicity, specifically White, Chinese, Filipina, Native Hawaiian, and Micronesian. These are a few of the major racial/ethnic groups in Hawai‘i and research has demonstrated differences in health-related outcomes between these groups.22 The race/ethnicity of the patients was portrayed through the use of prototypical names (Table 2). The names of the White, Chinese, and Hawaiian patients were pre-tested with a sample of 18 undergraduate students from the University of Hawai‘i who demonstrated, on average, 90% agreement that these names represented women from the targeted racial groups. The Filipina and Micronesian names were identified as prototypical based on the researchers' experiences with these population groups in their clinical practice and consultation with leaders in the Filipino and Micronesian medical community.
Table 1.
Patient Case Studies
| Younger Patient | Name is a 23-year-old woman who comes in to your office requesting a method of birth control. She has no previous pregnancies. Name became sexually active at age 18. She does not have a history of sexually transmitted infections. Testing for gonorrhea and chlamydia three months ago was negative. Name's blood pressure today is normal. Name states that she does not want to become pregnant for at least a couple of years. |
| Older Patient | Name is a 36-year-old woman who comes in to your office requesting a method of birth control. She has two children. Name became sexually active at age 18 and is currently in a monogamous relationship. She does not have a history of sexually transmitted infections. Name's blood pressure today is normal. Name states that she does not want to become pregnant again. |
Table 2.
Names for each Racial/Ethnic Group
| Race/Ethnicity | Name |
| White | Claire Patterson, Heather Anderson |
| Chinese | Ying Cheung, Mei Wong |
| Filipina | Rhea Mae Aquino, Mariel Bautista |
| Hawaiian | Keikilani Kapahu, Kailani Mahelona |
| Micronesian | Jayleen Morelik, Merly Sigrah |
Study Design
We emailed surveys to 195 third and fourth year medical students who had completed all required didactic education in obstetrics and gynecology from the John A. Burns School of Medicine at the University of Hawai‘i between June 2014 and July 2015. Students were emailed a link to an online survey and sent a reminder follow-up email two weeks later. Participants were first presented with case studies and asked to identify which contraceptive method they would recommend from a list of six options (female sterilization [laparoscopic tubal sterilization or hysteroscopic sterilization], intrauterine device [copper or Levonorgestrel IUD], Etonogestrel implant [Nexplanon], depot medroxyprogesterone acetate [DMPA3-month injection], oral contraceptive pills, or condoms). Methods were always presented in this order and students were restricted to selecting only one option. For scoring purposes, contraception methods were reverse coded into ranked data such that responses ranged from least (1 – condoms) to most (6- female sterilization) effective methods. Each participant answered questions about two case studies: one a 23-year-old woman and the other a 36-year-old woman. The race of the patients in the case studies was not explicitly disclosed, but the names were changed systematically to reflect White, Chinese, Filipina, Hawaiian, or Micronesian race. For each participant, the selected names for the 23-year old and 36-year old reflected the same race. The order of the case studies was counterbalanced between participants so that an equal number of students read the scenario about the 23-year old woman versus the 36-year old woman first. The authors created an item to gauge participants' level of experience with contraception in clinical settings (responses included None, Not Very Much, A Little, Some, Very Much, and Substantial). Finally, participants completed a demographic questionnaire which included their racial self-identification.
This study was approved by the Committee on Human Studies at the University of Hawai‘i. All participants provided informed consent before completing the study. To minimize social desirability bias, several questions that did not directly relate to the study objective were included in the survey to blind participants to the primary study objective and the study intent was not revealed to participants until they completed the survey. Students received a $5 gift card for their participation.
Statistical Analyses
Our primary outcome was to describe whether participants' contraceptive recommendations differed by patient race in the case studies. We used a convenience sample of all available third and fourth year medical students at our institution. We used a series of χ2 tests, Spearman correlations, and pre-specified bivariate logistic regressions to analyze whether contraceptive recommendations differed by patient race, participants' clinical experience or participants' race. All analyses were performed with SPSS Version 22 (IBM Corp: Armonk, NY).
Results
One hundred and twenty-four students enrolled in the study and consented to participate, of which 103 unique individuals completed the case studies and provided contraceptive recommendations. Of these 103, four students did not provide their experience with contraception in a clinical setting and eight students did not provide their racial identification. The number of case studies for each race/ethnicity group was balanced (χ2(4) = .54, P = .97); 22 participants read case studies about White patients, 21 about Chinese patients, 22 about Filipina patients, 18 about Hawaiian patients, and 20 about Micronesian patients. Post hoc analysis using G*Power software version 3.1.9.2 (Heinrich-Heine-Universität Düsseldorf: Kiel, Germany) for χ2 goodness-of-fit tests indicated that 103 students provided 68% power to detect a medium effect when comparing recommendations between five racial/ethnic groups using a binary outcome of recommending sterilization.
Recommendations for Contraception
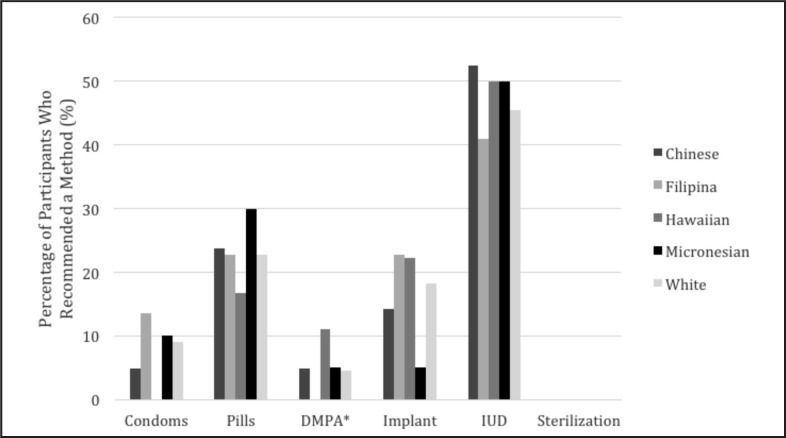
For the 23-year-old patient, a difference in the frequency of contraceptive recommendations was noted (χ2(4) = 59.86, P < .001, Figure 1). Students were most likely to recommend IUDs, followed by the contraceptive pill and Etonogestrel implant. Condoms and depot medroxyprogesterone acetate were less likely to be recommended. No recommendations were made for female sterilization in the younger patient case study. Contraceptive recommendations did not differ by race of the patient presented in the case studies for the younger scenario (χ2(16) = .901, P = .91).
Figure 1.
Contraception recommendations for the 23-year-old by patient race
*DMPA = Depot Medroxprogestereone Acetate
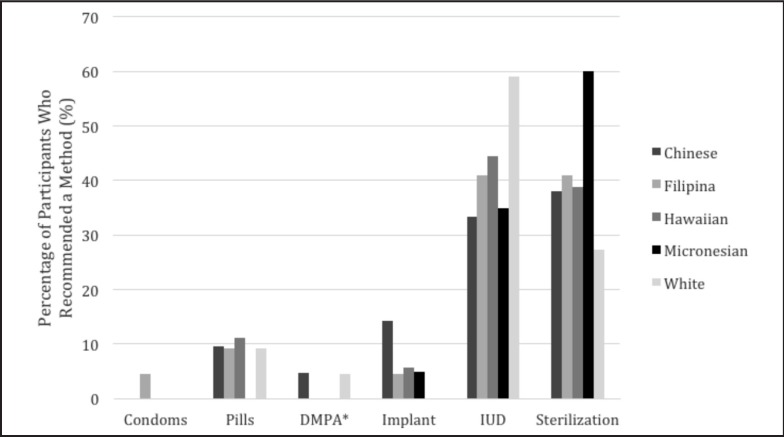
A difference in the frequency of contraceptive recommendations for the 36-year-old patient was noted (χ2(5) = 118.65, P < .001, see Figure 2). Recommendations for the older women most frequently included IUD and female sterilization, followed by the contraceptive pill and Etonogestrel implant. As with the younger patient, recommendations for condoms and depot medroxyprogesterone acetate occurred less frequently. We did not note a difference in contraceptive recommendations when examining all 5 methods separately (ie, condoms, pills, DMPA, implants, IUDs, and sterilization) for the 36-year-old patient (χ2(20) = 17.39, P = .63).
Figure 2.
Contraception recommendations for the 36-year-old by patient race
*DMPA = Depot Medroxprogestereone Acetate
Recommendations for Sterilization
To further examine our a priori assumption that the frequency of sterilization recommendations would differ across patient race, we coded contraceptive recommendations into non-sterilization (IUD, Etonogestrel implant, depot medroxyprogesterone acetate, contraceptive pills, and condoms and sterilization (female sterilization) categories. Because the 23-year-old patient did not receive recommendations for sterilization, we focused on recommendations made for the 36-year-old patient. Previous research has demonstrated that women of color experience disparities in contraception recommendations in relation to White women8–10 so we conducted bivariate logistic regressions to examine sterilization recommendations by race of patient, using White women as the control group. Micronesian women (60%) received more frequent sterilization recommendations compared to White women (27%; B = 1.39, SE = .66, Wald χ2(1) = 4.39, P = .04). In addition, Chinese (38%), Filipina (41%), and Hawaiian (39%) women, were more likely to receive sterilization recommendations as compared to White women, although these comparisons failed to reach conventional levels of statistical significance (P > .34).
Student Characteristics and Contraceptive Recommendations
For the 23-year-old patient, contraceptive recommendations did not differ by the participant's race (χ2(12) = 10.75, P = .55; Table 3). However, recommendations were related to students' previous clinical experience with contraception (Spearman correlation r = .22, P = .029) such that students who reported having more experience with contraception in a clinical setting were more likely to recommend increasingly effective methods (eg, IUDs and implants).
Table 3.
Contraception recommendations for the 23-year-old by participant demographics
| Type of contraception | ||||||
| Condom n (%) | Pill n (%) | Depot Medroxyprogesterone acetate n (%) | Etonogestrel implants n (%) | IUD* n (%) | Female Sterilizationn (%) | |
| Participant Race | ||||||
| East/Southeast Asian (n = 60) | 4 (7) | 14 (23) | 5 (8) | 9 (15) | 28 (47) | 0 |
| Multiracial (n = 17) | 1 (6) | 5 (29) | 0 | 2 (12) | 9 (53) | 0 |
| White (n = 13) | 2 (15) | 2 (15) | 0 | 3 (23) | 6 (46) | 0 |
| Hawaiian (n = 4) | 0 | 3 (75) | 0 | 0 | 1 (25) | 0 |
| Other/Missing (n = 9) | 1 (11) | 0 | 0 | 3 (33) | 5 (56) | 0 |
| Participant Experience with Birth Control in a Clinical Setting | ||||||
| None (n = 20) | 4 (20) | 6 (30) | 3 (15) | 2 (10) | 5 (25) | 0 |
| Not Very Much (n = 17) | 2 (12) | 4 (24) | 0 | 1 (6) | 10 (59) | 0 |
| A Little (n = 21) | 1 (5) | 5 (24) | 1 (5) | 4 (19) | 10 (48) | 0 |
| Some (n = 30) | 1 (3) | 7 (23) | 1 (3) | 6 (20) | 15 (5) | 0 |
| Very Much (n = 9) | 0 | 2 (22) | 0 | 2 (22) | 5 (56) | 0 |
| Substantial (n = 2) | 0 | 0 | 0 | 1 (50) | 1 (50) | 0 |
| Missing (n = 4) | 0 | 0 | 0 | 1 (25) | 3 (75) | 0 |
IUD = intrauterine device. Note. Regardless of Participant Race students more likely to recommend IUDs followed by the contraception pill and Etonogestrel implant (χ2 (4) = 59.86, P < .001). Students who reported having more experience with contraception in a clinical setting were likely to recommend increasingly effective methods (Spearman correlation r = .22, P = .029).
For the 36-year-old patient, contraceptive recommendations did not differ by the student's race (χ2(15) = 15.44, P = .42; Table 4). Recommendations were related to students' previous clinical experience with contraception (spearman correlation r = .28, P = .005) such that students who reported having more experience with contraception in a clinical setting were more likely to recommend increasingly effective methods (eg, IUDs, implants and sterilization). When examining recommendations for sterilization specifically, responses did not differ by participant race (χ2(3) = 2.02, P = .57), but were related to experience (spearman correlation r = .24, P = .018) such that students who reported having more experience in a clinical setting were more likely to recommend sterilization.
Table 4.
Contraception recommendations for the 36-year-old by participant demographics
| Type of contraception | ||||||
| Condom n (%) | Pill n (%) | Depot Medroxyprogesterone Acetate n (%) | Etonogestrel implants n (%) | IUD* n (%) | Female Sterilization n (%) | |
| Participant Race | ||||||
| East/Southeast Asian (n = 60) | 0 | 5 (8) | 1 (2) | 2 (3) | 23 (38) | 29 (48) |
| Multiracial (n = 17) | 0 | 1 (6) | 0 | 0 | 9 (53) | 7 (41) |
| White (n = 13) | 1 (8) | 1 (8) | 0 | 1 (8) | 6 (46) | 4 (31) |
| Hawaiian (n = 4) | 0 | 1 (25) | 0 | 1 (25) | 1 (25) | 1 (25) |
| Other/Missing (n = 9) | 0 | 1 (11) | 1 (11) | 1 (11) | 5 (56) | 1 (11) |
| Participant Experience with Birth Control in a Clinical Setting | ||||||
| None (n = 20) | 1 (5) | 3 (15) | 1 (5) | 1 (5) | 9 (45) | 5 (25) |
| Not Very Much (n = 17) | 0 | 2 (12) | 0 | 0 | 10 (59) | 5 (29) |
| A Little (n = 21) | 0 | 3 (14) | 1 (5) | 2 (9) | 5 (24) | 10 (48) |
| Some (n = 30) | 0 | 0 | 0 | 3 (10) | 11 (37) | 16 (53) |
| Very Much (n = 9) | 0 | 0 | 0 | 0 | 5 (56) | 4 (44) |
| Substantial (n = 2) | 0 | 0 | 0 | 0 | 0 | 2 (100) |
| Missing (n = 4) | 0 | 0 | 0 | 0 | 4 (100) | 0 |
IUD = intrauterine device. Note. Regardless of Participant Race students more likely to recommend IUDs and female sterilization (χ2 (5) = 118.65, P < .001). Students who reported having more experience with contraception in a clinical setting were likely to recommend increasingly effective methods (Spearman correlation r = .28, P = .006), and female sterilization (Spearman correlation r = .24, P = .018).
Discussion
We found statistically significant differences in the frequency of recommendations for sterilization when identical case descriptions of a 36-year old woman requesting birth control were presented with variations in only the patient's name. This study adds to the literature exploring the role of a patient's race/ethnicity in recommendations for contraception. Although this topic has been examined in other published studies describing differences in contraceptive use in women of different races, the mechanisms underlying these differences are unclear.8,10 Social psychological research suggests that subconscious biases held toward certain groups of people is widespread, even among those who self-identify as non-discriminatory.23,24 Providers' personally held beliefs, in addition to their previous experience, could influence their interactions with patients and clinical recommendations, thereby contributing to continuing health disparities.4, 5 Though we are unable to draw conclusions on the biases of health care providers early in their training, our findings suggest that women of different races may receive different contraceptive recommendations.
That IUDs were most frequently recommended, regardless of the race/ethnicity of the patient, may reflect the increased emphasis for recommending long-acting reversible contraception (LARC) as a “top-tier” contraceptive.25, 26 Medical students may recognize both the high efficacy and reversibility of LARC, particularly in younger women when future fertility is likely to be desired. Although participants may have identified the IUD as a “top-tier” method, their recommendations were not solely based on contraceptive efficacy. Though DMPA has a lower failure rate than oral contraceptive pills, pills were more commonly recommended than DMPA. We did not collect data on why participants recommended pills more frequently than DMPA in this survey. However, their recommendations parallel current contraceptive use in the United States where 4.5% of reproductive age women who use contraception select DMPA compared to 25.9% who select the oral contraceptive pill.27 Additionally, participants may have perceived fewer barriers to the continuation of oral contraceptive pills which are often prescribed and refilled at 12 month intervals in contrast to DMPA which requires a return visit to a health center every 3 months for continuation.
While IUDs were commonly recommended for the older patients, particularly for White women, in line with other studies examining differences in contraceptive recommendations in racial minorities in the continental US, a trend toward Micronesian women receiving more frequent recommendations for sterilization was noted.12,14,18,28 Though we did not elicit reasons for different contraceptive recommendations and therefore cannot draw conclusions on the etiology of different recommendations, biases of health care providers towards Micronesians has been described.22,29 Micronesian migrants frequently cite limited economic resources in their western Pacific island of origin as a reason for moving to the US and are often categorized as “low income” once they arrive to the US.30 These results are consistent with several previous studies demonstrating that, in comparison to White women, Black women and Hispanic women more frequently report that they were encouraged by providers to limit their family size.8, 10, 17, 31, 32 Whereas society may encourage white, middle-class women to become mothers, low-income, minority women may be discouraged from childbearing both through media messages and public policy.8,17 For example, “welfare family caps”, policies which deny or reduce cash aid for babies born to women already receiving financial assistance exist in many states.17 When comparing hospital admission rates across a range of diseases (eg, cardiac, infections, cancer, endocrine, or substance abuse), in comparison to other racial/ethnic groups in Hawai‘i, Micronesians tend to be younger and manifest more severe symptoms.22 When socioeconomic standing is compounded with limited English proficiency, cultural differences in communication styles and limited skills in navigating a complex health care system, health care providers may classify Micronesian patients as “difficult” with a higher risk of non-compliance and loss to follow up.30 This may have been why a method like sterilization, which requires no ongoing compliance or return visits on the part of the user to remain highly effective, was recommended more frequently for Micronesian patients.
Potential limitations should be noted. Prototypical names are frequently used to depict individuals from different racial groups within social psychological research.33 The names used in this study were carefully selected to be representative of the targeted racial groups. It is still possible, however, that individual participants may not have associated names with the targeted race. Additionally, we did not state if the patient's insurance covered all forms of contraception in the case studies, which may have limited the recommendations made by some of the students. Students may have recommended methods like the IUD not because of its characteristics but because patients could continue to use the method regardless of insurance status, access to health care providers or their ability to pay for ongoing use which could be a problem with methods like condoms, DMPA or the oral contraceptive pill. Our measure of clinical experience was subjective; whether participants used similar criteria to gauge previous experience is unclear.
Our findings suggest that the push by national organizations to increase the use of LARC has been successful. Participants were overall more likely to recommend IUDs, as compared to all other methods, to the 23-year-old patient and equally likely to recommend IUDs and sterilization to the 36-year-old patient; making IUDs the most recommended method across the entire study. The literature on health care disparities frequently attempts to address whether better or poorer health is due to individuals of different races being clinically different or being treated differently by clinicians. Our results draw attention to potential of racial/ethnic differences in patient counseling and the need for awareness of potential differences when promoting sterilization. Future research must investigate ways to promote patient-centered, unbiased care in order to help reduce current health disparities.
Conflict of Interest
None of the authors identify any conflict of interest.
Disclosure Statement
This research was supported by a Society for the Psychological Study of Social Issues (SPSSI) Grant-In-Aid awarded to Dr. Williams; and a NICHD award R00HD065741 awarded to Dr. Pauker. Drs. Kaneshiro, Soon, Salcedo, and Tschann receive research funding from Merck, Mithra Pharmaceuticals, Contramed and Gynuity Health Projects. Drs. Williams, Kajiwara, Elia, and Pauker have no competing financial interests to disclose.
References
- 1.Koh HK, Graham G, Glied SA. Reducing racial and ethnic disparities: the action plan from the department of health and human services. Health Aff (Millwood) 201110:1822–1829. doi: 10.1377/hlthaff.2011.0673. [DOI] [PubMed] [Google Scholar]
- 2.Frieden TR Centers for Disease C, Prevention, author. Strategies for reducing health disparities - selected CDC-sponsored interventions, United States, 2016. MMWR Suppl. 2016;1:1–69. [PubMed] [Google Scholar]
- 3.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;7:678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 4.Major B, Mendes WB, Dovidio JF. Intergroup relations and health disparities: a social psychological perspective. Health Psychol. 2013;5:514–524. doi: 10.1037/a0030358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Penner LA, Hagiwara N. Racism and Health. Wiley Blackwewll; 2014. [Google Scholar]
- 6.White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv Res. 2012;3(Pt 2):1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood) 2005;2:325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 8.Dehlendorf C, Ruskin R, Grumbach K, Vittinghoff E, Bibbins-Domingo K, Schillinger D, Steinauer J. Recommendations for intrauterine contraception: a randomized trial of the effects of patients' race/ethnicity and socioeconomic status. American Journal of Obstetrics and Gynecology. 2010;4:319 e311–318. doi: 10.1016/j.ajog.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dehlendorf C, Park SY, Emeremni CA, Comer D, Vincett K, Borrero S. Racial/ethnic disparities in contraceptive use: variation by age and women's reproductive experiences. American Journal of Obstetrics and Gynecology. 2014;6:526 e521–529. doi: 10.1016/j.ajog.2014.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dehlendorf C, Foster DG, de Bocanegra HT, Brindis C, Bradsberry M, Darney P. Race, ethnicity and differences in contraception among low-income women: methods received by Family PACT Clients, California, 2001–2007. Perspect Sex Reprod Health. 2011;3:181–187. doi: 10.1363/4318111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008–2011. The N Eng J Med. 2016;9:843–852. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borrero S, Schwarz EB, Reeves MF, Bost JE, Creinin MD, Ibrahim SA. Race, insurance status, and tubal sterilization. Obstetrics and Gynecology. 2007;1:94–100. doi: 10.1097/01.AOG.0000249604.78234.d3. [DOI] [PubMed] [Google Scholar]
- 13.Borrero S, Moore CG, Qin L, Schwarz EB, Akers A, Creinin MD, Ibrahim SA. Unintended pregnancy influences racial disparity in tubal sterilization rates. J Gen Intern Med. 2010;2:122–128. doi: 10.1007/s11606-009-1197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramaswamy M, Kelly PJ. Factors associated with sterilization use among women leaving a U.S. jail: a mixed methods study. BMC Public Health. 2014:773. doi: 10.1186/1471-2458-14-773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stern AM. Sterilized in the name of public health: race, immigration, and reproductive control in modern California. American Journal of Public Hhealth. 2005;7:1128–1138. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garcia G, Richardson DM, Gonzales KL, Cuevas AG. Trends and Disparities in Postpartum Sterilization after Cesarean Section, 2000 through 2008. Women's Health Issues. 2015;6:634–640. doi: 10.1016/j.whi.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 17.Downing RA, LaVeist TA, Bullock HE. Intersections of ethnicity and social class in provider advice regarding reproductive health. American Journal of Public Health. 2007;10:1803–1807. doi: 10.2105/AJPH.2006.092585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shreffler KM, McQuillan J, Greil AL, Johnson DR. Surgical sterilization, regret, and race: contemporary patterns. Soc Sci Res. 2015:31–45. doi: 10.1016/j.ssresearch.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.US Census Bureau Quick Facts. 2016. [November 11, 2016]. https://www.census.gov/quickfacts/table/PST045215/00.
- 20.Colby SL, Ortman JM. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. 2015. [November 11, 2016, 2016]. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf.
- 21.2014 State and County Population Characteristics. 2016. [November 5, 2016]. http://census.hawaii.gov/whats-new-releases/2014-state-and-county-population-estimates/
- 22.Hagiwara MK, Miyamura J, Yamada S, Sentell T. Younger and Sicker: Comparing Micronesians to Other Ethnicities in Hawaii. American Journal of Public Health. 2016;3:485–491. doi: 10.2105/AJPH.2015.302921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCubbin LD, Antonio M. Discrimination and obesity among Native Hawaiians. Hawaii J Med Public Health. 2012;12:346–352. [PMC free article] [PubMed] [Google Scholar]
- 24.Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;6:882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Contraception for adolescents. Pediatrics. 2014;4:e1244–e1256. doi: 10.1542/peds.2014-2299. [DOI] [PubMed] [Google Scholar]
- 26.ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstetrics and Gynecology. 2011;1:184–196. doi: 10.1097/AOG.0b013e318227f05e. [DOI] [PubMed] [Google Scholar]
- 27.Daniels K, Daugherty J, Jones J, Mosher W. Current Contraceptive Use and Variation by Selected Characteristics Among Women Aged 15–44: United States, 2011–2013. Natl Health Stat Report. 2015;86:1–14. [PubMed] [Google Scholar]
- 28.Borrero S, Abebe K, Dehlendorf C, Schwarz EB, Creinin MD, Nikolajski C, Ibrahim S. Racial variation in tubal sterilization rates: role of patient-level factors. Fertil Steril. 2011;1:17–22. doi: 10.1016/j.fertnstert.2010.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blair C. 2017. [August 14, 2017]. http://www.civilbeat.org/2011/06/11650-no-aloha-for-micronesians-in-hawaii/. No Aloha for Micronesians in Hawaii [2011; http://www.civilbeat.org/2011/06/11650-no-aloha-for-micronesians-in-hawaii/
- 30.Pobutsky A, Buenconsejo-Lum L, Chow C, Palafox N, Maskarinec G. Micronesian Migrants in Hawaii: Health Issues and Culturally Appropriate, Community-Based Solutions Californian. Journal of Health Promotion. 2005;4:59–72. [Google Scholar]
- 31.Borrero S, Schwarz EB, Creinin M, Ibrahim S. The impact of race and ethnicity on receipt of family planning services in the United States. J Womens Health (Larchmt) 2009;1:91–96. doi: 10.1089/jwh.2008.0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Becker D, Tsui AO. Reproductive health service preferences and perceptions of quality among low-income women: racial, ethnic and language group differences. Perspect Sex Reprod Health. 2008;4:202–211. doi: 10.1363/4020208. [DOI] [PubMed] [Google Scholar]
- 33.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;6:1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]