Abstract
Background
Hospice, a patient-centered care system for those with limited life expectancy, is important for enhancing quality of life and is understudied in integrated healthcare systems.
Methods
Retrospective, cohort study in the national U.S. VA Health Care System composed of 21,860 decedents with advanced stage lung cancer diagnosed from January 2007–June 2013. Trends over time, geographic regional variability, and patient and tumor characteristics associated with hospice use and the timing of enrollment were examined. Multivariable logistic regression and Cox proportional hazards modeling were utilized.
Results
From 2007–2013, 70.3% of decedents with advanced stage lung cancer were enrolled in hospice. Among patients in hospice, 52.9% were enrolled in the last month of life and 14.7% were enrolled in the last three days of life. Hospice enrollment increased (Adjusted Odds Ratio (AOR)=1.07, p<0.001), while mean time from cancer diagnosis to hospice enrollment decreased by 65 days (32% relative decrease) (Adjusted Hazard Ratio=1.04, p<0.001). A relative decrease in late hospice enrollment was observed in the last month and last three days of life of 7% (AOR=0.98, p=0.04) and 26% (AOR=0.95, p<0.001), respectively. The Southeast region of the U.S. had both the highest rate of hospice enrollment and lowest rate of late enrollment. Patient sociodemographic and lung cancer characteristics were associated with hospice enrollment.
Conclusions
Among patients with advanced stage lung cancer in the VA Health Care System, overall and earlier hospice enrollment increased over time. Considerable regional variability in hospice enrollment and persistence of late enrollment suggests opportunities for improvement in end-of-life care.
Keywords: lung cancer, supportive and palliative car, quality of life, epidemiology, health services research
Introduction
According to National Comprehensive Cancer Network guidelines, early enrollment in hospice maximizes potential benefits and should be emphasized.1 Regarding the timing of referral, patients become eligible when their life expectancy is ≤ six months, and physicians and policy experts indicate that patients should ideally spend about 2–3 months in hospice.2–4 Despite this guidance, hospice referrals often occur too late in the disease trajectory to improve quality of life (QOL) for patients with cancer.5
More recently, use of hospice and earlier enrollment have become important quality metrics in cancer care,6,7 as enrollment can improve physical and psychological symptoms, enhance caregiver well-being, and reduce hospitalizations and in-hospital deaths.8,9 Hospice use among Medicare beneficiaries is increasing, but late enrollment, defined as the last three days of life, more than doubled from 2000 to 2009.10 Other trends observed underscore the continued use of aggressive treatment at the end-of-life including: increased hospitalizations, transitions in care and intensive care unit admissions.10 Similarly, a Dartmouth Atlas report among Medicare beneficiaries with cancer noted an increase in those who saw ten or more physicians or were receiving life-sustaining treatments in the last month of life.11
In addition to these trends, considerable geographic region variability12 in hospice use exists, even among academic and National Cancer Institute-designated medical centers.11 Mechanisms that contribute to these regional trends are not well understood, but are unlikely to be explained by patient preferences.13 Early hospice enrollment and reduced use of high-intensity end-of-life care are both associated with improved patient and family perceptions of the quality of care.14,15 In an effort to improve end-of-life care, the Veterans Health Administration (VA) has created a Hospice and Palliative Care Program Office and mandated that all medical centers have a palliative care consultation team. The VA instituted a Comprehensive End-of-Life Care Initiative (CELC) designed to increase access to palliative care services and local facility collaboration with community hospice programs.16 Aspects unique to VA healthcare, such as the financial structure, may contribute to improved hospice use as financial incentives for high-intensity care are absent.17 Veterans may also receive concurrent disease-modifying treatment while in hospice,18 contrary to non-VA Medicare patients, which may affect enrollment. Although a sizable percentage of Veterans with cancer were reported to receive hospice care in 2012,19 trends in use including the timing of enrollment are unexplored. We analyzed temporal and regional trends in hospice use, timing of enrollment, and patient characteristics that contribute to use in this national, integrated healthcare system. The study cohort was comprised of patients with advanced stage lung cancer, as this is the leading cause of cancer death among both men and women in the U.S.
Methods
In this retrospective cohort study, we identified all decedents with advanced stage lung cancer (stage IIIB & IV) diagnosed from January 2007–June 2013 using the Veterans Affairs Central Cancer Registry (VACCR).20 Patients with non-primary lung cancer or unknown stage or histology were excluded. The VACCR receives and stores information on cancer diagnosis and treatment compiled by local cancer registry staff at each of the 132 VA Medical Centers that diagnose and/or treat Veterans with cancer. VACCR staff carry out case identification and abstraction of variables adhering to the standards of the Commission on Cancer.21 Registry data include extensive demographics, cancer identification, disease staging, and treatment received among other variables. Sociodemographic characteristics at the time of lung cancer diagnosis were also compiled from the VA Corporate Data Warehouse which is a centralized clinical data storage platform.. Cancer specific characteristics, such as stage, were determined by VACCR registrars using the American Joint Committee on Cancer staging system. See the Supplementary Material for additional details regarding patient characteristics, facility regions and disease-modifying treatments received. (VA-IRB approval #00010985)
Hospice Use
Date of hospice enrollment was determined utilizing several sources including VA Fee Basis files through bed section codes, clinic stop codes and ICD-9 CM codes.19 For care purchased external to the VA, we used VA-Purchased Care claims files via visit or Health Care Finance Administration (HCFA) codes.19 We used Medicare claims data through the Medicare hospice file data set using Part A and B claims.10 The VA Medicare hospice file was available through December 2013 and given potential billing delays after date of receipt, the cohort was censored to those diagnosed before June 30, 2013.
Statistical Analysis
Descriptive statistics were used to characterize patient characteristics by hospice enrollment, continuous data are presented as mean ± Standard Deviation (SD) or median (interquartile range-IQR) and categorical variables as proportions. Patient characteristics associated with enrollment or late hospice enrollment were analyzed using multivariable logistic regression with backward stepwise selection, the final models adjusted for age, sex, race/ethnicity, marital status, income, Functional Comorbidity Index (FCI),22 Charlson Comorbidity Index (CCI),23 cancer stage and histology, and year of diagnosis. Logistic regression was used to model hospice enrollment, enrollment in the last month of life, and enrollment in the last three days of life. Cox proportional hazards was used to model time from cancer diagnosis to hospice enrollment. Annual trend was estimated using a “year” variable in each model. All models were adjusted for the same covariates identified in the patient characteristics models excluding year. Regional differences in hospice use were analyzed using multivariable logistic regression adjusted for the same covariates identified in the patient characteristics models, estimated marginal means are presented. The Northeast region was used as a reference group due to sample size and lowest enrollment. All modeling used robust standard errors and statistical testing was 2-sided with a threshold of p<.05. All analyses were done in Stata version 14(StataCorp).
Results
From 2007 to 2013, 21,860 patients died with advanced stage lung cancer in the VA Health Care System. The mean age was 68 years, 98% were men, 70% were white, 57% were not married, and 68% were Medicare beneficiaries at the time of cancer diagnosis. (Table 1) Regarding lung cancer characteristics, 89% had stage IV disease and 69% had non-small cell lung cancer (NSCLC). Median survival from cancer diagnosis was 134 days (IQR 51–307 days), and was similar when stratified by year of diagnosis.
Table 1.
Patient Characteristics at Diagnosis.
| Patient Characteristics | Ever Enrolled in Hospice n= 15,369 |
Not Enrolled in Hospice n=6491 |
|---|---|---|
| Age, years, mean (±SD) | 68 (±9.7) | 67 (±9.4) |
| Sex, male | 15,091 (98) | 6380 (98) |
| Race | ||
| White | 11,034 (72) | 4376 (67) |
| Black | 2165 (14) | 1185 (18) |
| Other | 2125 (14) | 917 (14) |
| Unknown | 45 (<1) | 13 (<1) |
| Marital Status | ||
| Married | 6924 (45) | 2505 (39) |
| Not Married | 8421 (55) | 3967 (61) |
| Unknown | 24 (<1) | 19 (<1) |
| Income, U.S. dollars | ||
| ≤44,000 | 5169 (34) | 2254 (35) |
| >44,000–52,999 | 4881 (32) | 1909 (29) |
| ≥53,000 | 5261 (34) | 2301 (35) |
| Unknown | 58 (<1) | 27 (<1) |
| Home Residence Location | ||
| Urban | 10,742 (70) | 4530 (70) |
| Rural | 4449 (29) | 1833 (28) |
| Unknown | 178 (1) | 128 (2) |
| Medicare Beneficiary, yes | 10,933 (71) | 3896 (60) |
| Functional Comorbidity Index (FCI) | ||
| None (0) | 2627 (17) | 1185 (18) |
| Mild (1–2) | 3581 (23) | 1489 (23) |
| Moderate (3–4) | 4693 (31) | 2024 (31) |
| Severe (≥5) | 4468 (29) | 1793 (28) |
| Charlson Comorbidity Index (CCI) | ||
| None (0) | 1990 (13) | 749 (12) |
| Mild (1–2) | 4030 (26) | 1629 (25) |
| Moderate (3–4) | 3515 (23) | 1480 (23) |
| Severe (≥5) | 5834 (38) | 2633 (41) |
| Tobacco History | ||
| Never | 431 (3) | 182 (3) |
| Current | 8538 (56) | 3720 (57) |
| Former | 5726 (37) | 2328 (36) |
| Unknown | 674 (4) | 261 (4) |
| Cancer Stage | ||
| IIIB | 1544 (10) | 825 (13) |
| IV | 13,825 (90) | 5666 (87) |
| Cancer Histology | ||
| NSCLC | 10,661 (69) | 4355 (67) |
| SCLC | 2724 (18) | 1281 (20) |
| Other | 1984 (13) | 855 (13) |
Reported as n(%) unless otherwise stated;
Abbreviations: SD= standard deviation,, NSCLC= Non-small cell lung cancer, and SCLC= Small cell lung cancer.
In this cohort, 70.3% of patients were enrolled in hospice care. (Table 2) Patients enrolled in hospice spent a median of 27 days (IQR 8–76) in hospice before death. The mean time from lung cancer diagnosis to hospice enrollment was 183 days (SD 256.1) (median=86 days [IQR 27–242]). Among all patients enrolled in hospice, 52.9% were enrolled in the last month of life and 14.7% were enrolled in the last three days of life. Among hospice enrollees, 36.6% received radiation with 4.7% beginning radiation after hospice enrollment. About half (49%), received chemotherapy with 12.5% of these receiving it after hospice enrollment. Among patients not enrolled in hospice, 33.5% received radiation and 44.5% received chemotherapy. Among hospice enrollees, 9.9% and 3.9% received chemotherapy in the last four and two weeks of life, respectively.
Table 2.
Hospice Use and Cancer Treatment Received.
| All Patients n=21,860 |
|
|---|---|
| Ever Enrollment | 15369 (70.3) |
| Hospice daysa, median (IQR) | 27 (8–76) |
| Timing of Hospice Enrollmenta | |
| Cancer diagnosis to enrollment, days, mean (SD) | 183 (±256) |
| Last month of life | 8125 (52.9) |
| Last three days of life | 2253 (14.7) |
| Days per patient, last month of life, mean (SD) | 20 (±12) |
| Cancer Treatments Receiveda | |
| Radiation therapy | 5621 (36.6) |
| Chemotherapy | 7530 (49.0) |
| Last 4 weeks of life | 1514 (9.9) |
| Last 2 weeks of life | 595 (3.9) |
Values are n(%) unless otherwise stated;
. Denominator= patients enrolled in hospice;
Abbreviations: IQR= Intra-quartile range and SD= standard deviation.
Hospice Trends
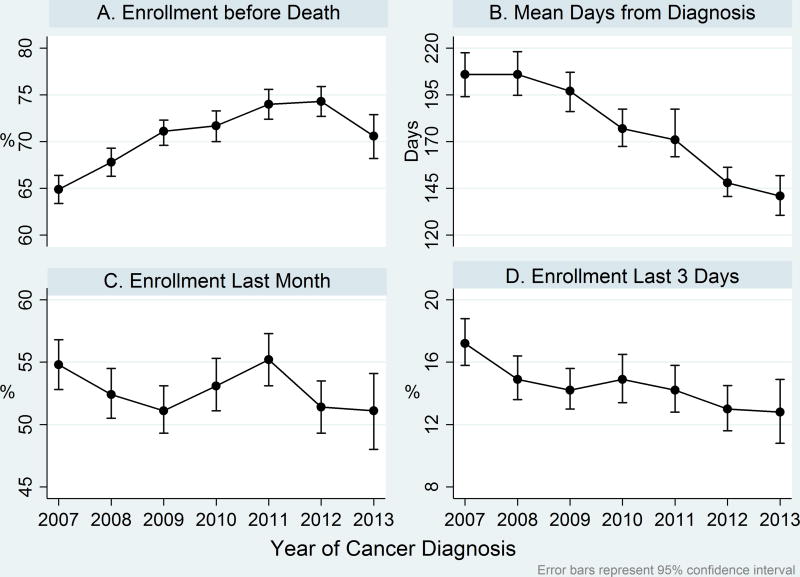
Overall hospice enrollment increased from 64.9% in 2007 to 70.6% in 2013 (per year Adjusted Odds Ratio (AOR)=1.07, p<0.001 for trend), a 9% relative increase. (Figure 1) Mean time from cancer diagnosis to hospice enrollment decreased from 206 days in 2007 to 141 days in 2013 (per year Adjusted Hazard Ratio=1.04, p<0.001 for trend), a 32% relative decrease. Patients enrolled in the last month of life decreased from 54.7% to 51.1% (per year AOR=0.98, p=0.04 for trend) a 7% relative decrease. Patients enrolled in the last three days of life decreased from 17.2% to 12.8% (per year AOR=0.95, p<0.001 for trend) a 26% relative decrease.
Figure 1. Trends in Hospice Use and Timing of Enrollment.
Panel A. Percentage of patients enrolled in hospice before death increased from 64.9% in 2007 to 70.6% in 2013, a 8% relative decrease (p<0.001 for trend). Panel B. Mean days from lung cancer diagnosis to hospice enrollment decreased from 206 days in 2007 to 141 days in 2013, a 32% relative decrease (p<0.001 for trend). Panel C. Percentage of patients enrolled in hospice in the last month of life decreased from 54.7% in 2007 to 51.1% in 2013, a 7% relative decrease (p=0.04 for trend). Panel D. Percentage of patients enrolled in hospice in the last three days of life decreased from 17.2% in 2007 to 12.8% in 2013, a 26% relative decrease (p<0.001 for trend). Trend analyses were adjusted for age, sex, race, marital status, income, FCI, CCI, cancer stage and histology.
Regional Variation in Use
Regional variability in hospice enrollment existed nationally, which ranged from 63.9% in the Northeast to 77.0% in the Southeast, these differences were significant (p<0.01). (Table 3) The mean number of days in hospice during the last month of life was significantly different across regions and ranged from 18.9 to 20.6 days. Regional variability in the timing of hospice enrollment was significant; enrollment in the last month of life ranged from 50.0% in the Southeast to 55.6% in the Northeast. Enrollment in the last three days of life ranged from 11.5% in the Southeast to 17.8% in the Northeast. Chemotherapy receipt in the last two weeks of life ranged from 11.3 to 13.3% and was not significantly different across regions. Hospice enrollment trends over time increased similarly across regions.
Table 3.
U.S. Region of Hospice Use by Cancer Reporting Facility Location.
| U.S. Region | ||||||
|---|---|---|---|---|---|---|
| Hospice Use | All Regions n=21,860 |
Northeast n=3481 |
Southeast n=5526 |
Midwest n=7846 |
Southwest n=1682 |
West n=3163 |
| Ever Enrollment | 15,369 (70.3) | 2218 (63.9) reference | 4209 (77.0) p<0.001 | 5477 (70.3) p<0.001 | 1207 (71.5) p<0.001 | 2191 (68.9) p<0.001 |
| Hospice days, last month of life, mean (SE) | 20 (11.6) | 18.9 (0.25) reference | 20.6 (0.18) p<0.001 | 19.1 (0.16) p=0.50 | 20.2 (0.33) p=0.001 | 20.4 (0.26) p<0.001 |
| Enrollment last month of lifea | 8125 (52.9) | 1221 (55.6) reference | 2117 (50.0) p<0.001 | 3009 (55.0) p=0.67 | 616 (51.0) p=0.01 | 1130 (51.8) p=0.01 |
| Enrollment last 3 days of lifea | 2253 (14.7) | 389 (17.8) reference | 518 (11.5) p<0.001 | 899 (16.0) p=0.06 | 163 (13.3) p=0.001 | 280 (12.9) p<0.001 |
| Chemotherapy last 2 weeks of lifea | 1341 (12.9) | 220 (13.3) reference | 286 (11.3) p=0.06 | 500 (12.8) p=0.56 | 105 (12.9) p=0.77 | 212 (12.9) p=0.68 |
Values are n(%) unless otherwise noted; Marginal effects at the means are reported using age, sex, race, marital status, income, FCI, CCI, year of cancer diagnosis, cancer stage and histology as covariates;
. Denominator is patients ever enrolled in hospice.
Abbreviations: SE= standard error; 162 patients from reporting facilities located in the Philippines, US Virgin Islands or Puerto Rico were excluded.
Patient Characteristics
Hospice enrollment was associated with older age (AOR=1.01, p<0.001), moderate income compared to low income (AOR=1.12, p=0.002), higher FCI score (AOR=1.02, p<0.001) and stage (IV) lung cancer (AOR=1.31, p<0.001). (Table 4) Black race (AOR=0.78, p<0.001), unmarried marital status (AOR=0.80, p<0.001), lower CCI score (AOR=0.98,p<0.001) and small cell lung cancer (SCLC) (AOR=0.85, p<0.001) or other histology (AOR=0.91, p=0.03) were all associated with decreased hospice enrollment. Home residence location and tobacco history were not associated with hospice enrollment. Male sex (AOR=1.76, p=0.006), higher CCI score (AOR=1.04, p<0.001), and SCLC (AOR=1.23, p<0.001) and other lung cancer histologies (AOR=1.15, p=0.04) were associated with late hospice enrollment (≤3 days). Older age was associated with decreased likelihood of late hospice enrollment (AOR=0.98, p<0.001).
Table 4.
Patient Characteristics Associated with Hospice or Late Hospice Enrollment.
| Patient Characteristics | Hospice Enrollment Adj-ORa (95% CI) |
Late Hospice Enrollmentb (≤3 last days of life) Adj-ORa (95% CI) |
|---|---|---|
| Age, years | 1.01 (1.01–1.02)d | 0.98 (0.98–0.99)d |
| Sex, male | 0.85 (0.68–1.07) | 1.76 (1.18–2.63)e |
| Race | ||
| White | Reference | Reference |
| Black | 0.78 (0.72–0.84)d | 0.89 (0.78–1.02) |
| Other/Unknown | 0.95 (0.88–1.04) | 0.89 (0.78–1.01) |
| Marital Status | ||
| Married | Reference | Reference |
| Not Married | 0.80 (0.76–0.85)d | 0.95 (0.87–1.04) |
| Unknown | 0.51 (0.28–0.93) | 1.40 (0.54–3.58) |
| Income, U.S. dollars | ||
| ≤44,000 | Reference | Reference |
| >44,000–52,999 | 1.12 (1.04–1.20)e | 1.02 (0.91–1.14) |
| ≥53,000 | 0.99 (0.93–1.07) | 0.99 (0.89–1.11) |
| Unknown | 1.01 (0.63–1.60) | 0.91 (0.43–1.93) |
| Functional Comorbidity Index (FCI) | 1.02 (1.01–1.04)d | 0.99 (0.97–1.01) |
| Charlson Comorbidity Index (CCI) | 0.98 (0.97–0.99)d | 1.04 (1.02–1.05)d |
| Cancer Stage | ||
| IIIB | Reference | Reference |
| IVc | 1.31 (1.19–1.43)d | 1.10 (0.94–1.28) |
| Cancer Histology | ||
| NSCLC | Reference | Reference |
| SCLC | 0.85 (0.79–0.92)d | 1.23 (1.10–1.38)d |
| Other | 0.91 (0.83–0.99)e | 1.15 (1.01–1.32)e |
. Adjusted by age, sex, race, marital status, income, FCI, CCI, year of cancer diagnosis, cancer stage and histology;
. Analyses included those ever enrolled in hospice;
. SCLC histology included as stage IV;
. p<0.001;
. p<0.05.
Abbreviations: NSCLC= Non-small cell lung cancer and SCLC= Small cell lung cancer.
Discussion
This is the largest, most comprehensive study conducted examining hospice use in a national, integrated health system. We observed increased trends in overall and most importantly, earlier hospice enrollment, among patients with advanced lung cancer over time. The considerable geographic variability in hospice use and patient characteristics that were associated with the use and timing of hospice enrollment provide a framework for focused efforts to enhance utilization. Encouraging trends in timely hospice enrollment were identified in the VA, however, opportunities for improvement in end-of-life care exist. Determining healthcare system-related factors that can improve the quality of cancer care, such as timely hospice enrollment, deserve more attention.
Improvements in overall and timing of hospice enrollment that we observed may be related to factors unique to the VA system or are products of an integrated healthcare delivery model.24 VA end-of-life care initiatives, such as the CELC, over the past decade have affected hospice availability which contributes to utilization.25 More importantly, these VA initiatives may have contributed to a “culture change” within the system as physician and hospital practice styles are major drivers of end-of-life care,26,27 as are physicians’ attitudes regarding hospice referrals.28 Additional aspects of the VA system may increase hospice use including the lack of financial incentives for aggressive end-of-life care and the ability for Veterans to receive disease-modifying treatment while in hospice.18 Finally, integrated healthcare within the VA may enhance the timeliness of hospice enrollment among cancer patients, as was observed in another integrated system, Kaiser Permanente of Northern California.29 Patients report issues with care coordination and communication related to healthcare system disorganization and patients favor integrated care models.32 Breakdowns in patient-clinician communication, in non-integrated settings, may contribute to patients’ unrealistic expectations and a desire for aggressive care at the end-of-life,30,31 delaying or decreasing hospice use.
The decreasing trend in late enrollment we observed is particularly meaningful, as early use of hospice is lauded as a cancer care quality metric6,7 and the Center for Medicare and Medicaid Services has begun implementing nationally-endorsed hospice quality measures based on the timing of enrollment.35 Despite the potential benefits of hospice enrollment,8,9 Medicare beneficiaries in non-VA settings continue to experience worsening trends in short hospice stays.10,11 Among cancer decedents, hospice enrollment of about two months is suggested to maximize value and take advantage of the multidisciplinary approach.2–4 Patients and their families report greater benefits from longer stays, and those of about two weeks in length have been perceived as coming “too late”.2,3 While the overall trend in late enrollment is decreasing within the VA, one in seven patients still experienced ≤3 days of hospice care. Short hospice stays may be justified if they are related to sudden medical deterioration or patient preferences.36 Concurrent use of disease-modifying therapy and their related toxicities may contribute to sudden deterioration and increased likelihood of short hospice stays within the VA. Reasons for late hospice enrollment deserve further exploration, which will likely require analysis of patient-level data.
Despite the systematic organization and culture within the VA, this system was not immune to the significant geographic variability in hospice use seen in non-VA settings.37 There is a high concentration of Medicare-certified hospices in the Southeast region of the U.S., which may contribute to increased use.38 A direct relationship exists between supply and utilization/intensity of healthcare.39,40 This can translate to more aggressive care at the end-of-life, as hospice use is higher in areas with fewer inpatient hospital beds per capita.41 Increased end-of-life care intensity is associated with very short hospice stays.42 Hospital and physician capacity are highest in the Northeast, among VA and non-VA settings, potentially contributing to increased end-of-life care intensity.43 Although, hospice variability within a health system is not entirely surprising, as variation in use was not explained by differences in the major components of healthcare infrastructure, instead they were attributed to local factors such as community leadership on end-of-life issues.44 Overall, the trends in hospice use we observed were encouraging, and likely contribute to the reduced aggressive end-of-life care observed in Veterans compared to fee-for-service Medicare beneficiaries.17
Patient characteristics impacted hospice enrollment and were similar to non-VA settings, with a few notable exceptions. Healthcare disparities among black patients in end-of-life care and use of hospice45 persist in the VA. Higher income is associated with greater use of hospice,37,45 likely related to healthcare access. However, extreme economic hardship (i.e., limited resources for caregiving) is associated with a preference for comfort care.46 Our results were mixed regarding income, suggesting income may be a less significant determinant of end-of-life care when healthcare access is not income-dependent. Surprisingly, patients with a greater number or more severe comorbidities, via the CCI, were less likely enrolled and more likely to be enrolled late in hospice potentially demonstrating the contribution of comorbid disease to unexpected, sudden deterioration in lung cancer patients. The timing of comorbidity measurement (e.g., pre-cancer diagnosis) can impact differences in measured hospice use.47 It’s unknown if patients’ characteristics impact their care preferences or if clinicians’ referral patterns are biased; however, these patient subgroups should be targeted for interventions to increase hospice enrollment.
This study has limitations. The VACCR is limited to Veterans who are diagnosed or receive cancer care within the VA. Patients enrolled in hospice at the time of their lung cancer diagnosis were excluded given our objective to study hospice use related to lung cancer, likely underestimating overall enrollment. Patients who were offered hospice by clinicians, but chose not to enroll would affect results in unpredictable ways. Reasons for not offering hospice, from clinicians’ perspectives, were not explored. Place of residence, such as a nursing home, is associated with short hospice stays and was not studied.48 Regional differences in hospice enrollment may be partially explained by patients’ cultural, religious or personal beliefs, however, these are unlikely to account for significant variation.13 Regional differences in hospice use may be impacted by availability and patients’ regional categorization was based on the reporting facility at diagnosis and does not account for migration.
Conclusions
Within the VA Health Care System, overall and earlier hospice enrollment increased over time among patients with advanced stage lung cancer. Significant regional variability in hospice enrollment exists, suggesting opportunities for improvement. Future studies should focus on identifying regional processes and discrete elements of healthcare systems, such as financial or service models, that contribute to timely hospice use. Extrapolation of these elements to settings with decreased or delayed hospice enrollment is essential to reverse the current dismal trends in end-of-life care.
Supplementary Material
Acknowledgments
The authors would like to thank Sara Golden, Thomas Meath, and Benjamin Chan for their contributions to this work. The Department of Veterans Affairs did not have a role in the conduct of the study, in the collection, management, analysis, interpretation of data, or in the preparation of the manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
Funding and COI: Supported by the National Cancer Institute of the NIH under Award Number K07CA190706 and resources from the VAPHCS.
Footnotes
Contributions: Conceptualization: DRS, LG, LH, EKF, CGS. Methodology: all authors. Formal analysis: DRS, JAL, CGS. Resources: all authors. Writing–original draft: DRS, LG, CGS. Writing–review and editing: all authors.
The authors declare no potential conflicts of interest.
References
- 1.National Comprehensive Cancer Network. [Accessed December, 2016];CCN clinical practice guidelines in oncology: Palliative care. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp#palliative.
- 2.Kapo J, Harrold J, Carroll JT, Rickerson E, Casarett D. Are we referring patients to hospice too late? patients' and families' opinions. J Palliat Med. 2005;8(3):521–527. doi: 10.1089/jpm.2005.8.521. [DOI] [PubMed] [Google Scholar]
- 3.Rickerson E, Harrold J, Kapo J, Carroll JT, Casarett D. Timing of hospice referral and families' perceptions of services: Are earlier hospice referrals better? J Am Geriatr Soc. 2005;53(5):819–823. doi: 10.1111/j.1532-5415.2005.53259.x. [DOI] [PubMed] [Google Scholar]
- 4.Taylor DH, Jr, Ostermann J, Van Houtven CH, Tulsky JA, Steinhauser K. What length of hospice use maximizes reduction in medical expenditures near death in the US medicare program? Soc Sci Med. 2007;65(7):1466–1478. doi: 10.1016/j.socscimed.2007.05.028. [DOI] [PubMed] [Google Scholar]
- 5.Ferrell BR. Late referrals to palliative care. J Clin Oncol. 2005;23(12):2588–2589. doi: 10.1200/JCO.2005.11.908. [DOI] [PubMed] [Google Scholar]
- 6.American Society of Clinical Oncology. ASCO’s choosing wisely® “Top-five” list of recommendations, issued in 2012. 2012 [Google Scholar]
- 7.NQF National Quality Forum. National voluntary consensus standards for quality of cancer care. 2009 [Google Scholar]
- 8.Obermeyer Ziad, Makar Maggie, Abujaber Samer, Dominici Francesca, Block Susan, Cutler David M. Association between the medicare hospice benefit and health care utilization and costs for patients with poor-prognosis cancer. [Accessed 20141112];JAMA. 2014 312(18):1888–1896. doi: 10.1001/jama.2014.14950. doi: http://dx.doi.org/10.1001/jama.2014.14950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dy SM, Shugarman LR, Lorenz KA, Mularski RA, Lynn J RAND--Southern California Evidence-Based Practice Center. A systematic review of satisfaction with care at the end of life. J Am Geriatr Soc. 2008;56(1):124–129. doi: 10.1111/j.1532-5415.2007.01507.x. [DOI] [PubMed] [Google Scholar]
- 10.Teno JM, Gozalo PL, Bynum JPW, et al. Change in end-of-life care for medicare beneficiaries: Site of death, place of care, and health care transitions in 2000–2005, and 2009. [Accessed 20130206];JAMA. 2013 309(5):470–477. doi: 10.1001/jama.2012.207624. doi: https://dx.doi.org/10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodman D, Morden N, Chang C, Fisher E, Wennberg J. Trends in cancer care near the end of life. The Dartmouth Institute for Health Policy and Clinical Practice. 2013 Sep 4th; [PubMed] [Google Scholar]
- 12.Meier DE. Increased access to palliative care and hospice services: Opportunities to improve value in health care. [Accessed 20110921];Milbank Q. 2011 89(3):343–380. doi: 10.1111/j.1468-0009.2011.00632.x. doi: https://dx.doi.org/10.1111/j.1468-0009.2011.00632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences?: A study of the US medicare population. Med Care. 2007;45(5):386–393. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright AA, Keating NL, Ayanian JZ, et al. Family perspectives on aggressive cancer care near the end of life. [Accessed 20160120];JAMA. 2016 315(3):284–292. doi: 10.1001/jama.2015.18604. doi: https://dx.doi.org/10.1001/jama.2015.18604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wachterman MW, Pilver C, Smith D, Ersek M, Lipsitz SR, Keating NL. Quality of end-of-life care provided to patients with different serious illnesses. JAMA Internal Medicine. 2016;176(8):1095–1102. doi: 10.1001/jamainternmed.2016.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Health Services Research & Development. Improving end-of-life care for veterans: PROMISE. [Accessed 3/9, 2017]; https://www.hsrd.research.va.gov/for_managers/stories/promise.cfm.
- 17.Keating NL, Landrum MB, Lamont EB, Earle CC, Bozeman SR, McNeil BJ. End-of-life care for older cancer patients in the veterans health administration versus the private sector. Cancer. 2010;116(15):3732–3739. doi: 10.1002/cncr.25077. [DOI] [PubMed] [Google Scholar]
- 18.Casarett DJ, Fishman JM, Lu HL, et al. The terrible choice: Re-evaluating hospice eligibility criteria for cancer. Journal of Clinical Oncology. 2009;27(6):953–959. doi: 10.1200/JCO.2008.17.8079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gidwani R, Joyce N, Kinosian B, et al. Gap between recommendations and practice of palliative care and hospice in cancer patients. [Accessed 20160827];J Palliat Med. 2016 19(9):957–963. doi: 10.1089/jpm.2015.0514. doi: https://dx.doi.org/10.1089/jpm.2015.0514. [DOI] [PubMed] [Google Scholar]
- 20.Zullig LL, Jackson GL, Dorn RA, et al. Cancer incidence among patients of the U.S. veterans affairs health care system. Mil Med. 2012;177(6):693–701. doi: 10.7205/milmed-d-11-00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Commission-on-cancer. cancer program standards. Chicago, IL: American College of Surgeons; 2015. American College of Surgeons. [Google Scholar]
- 22.Groll DL, To T, Bombardier C, Wright JG. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58(6):595–602. doi: 10.1016/j.jclinepi.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 23.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 24.Kizer KW, Demakis JG, Feussner JR. Reinventing VA health care: Systematizing quality improvement and quality innovation. Med Care. 2000;38(6 Suppl 1):I7–16. [PubMed] [Google Scholar]
- 25.Virnig BA, Ma H, Hartman LK, Moscovice I, Carlin B. Access to home-based hospice care for rural populations: Identification of areas lacking service. J Palliat Med. 2006;9(6):1292–1299. doi: 10.1089/jpm.2006.9.1292. [DOI] [PubMed] [Google Scholar]
- 26.Obermeyer Z, Powers BW, Makar M, Keating NL, Cutler DM. Physician characteristics strongly predict patient enrollment in hospice. [Accessed 20150609];Health Aff (Millwood) 2015 34(6):993–1000. doi: 10.1377/hlthaff.2014.1055. doi: https://dx.doi.org/10.1377/hlthaff.2014.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morden NE, Chang C, Jacobson JO, et al. End-of-life care for medicare beneficiaries with cancer is highly intensive overall and varies widely. [Accessed 20120411];Health Aff (Millwood) 2012 31(4):786–796. doi: 10.1377/hlthaff.2011.0650. doi: https://dx.doi.org/10.1377/hlthaff.2011.0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bradley EH, Cramer LD, Bogardus STJ, Kasl SV, Johnson-Hurzeler R, Horwitz SM. Physicians' ratings of their knowledge, attitudes, and end-of-life-care practices. Acad Med. 2002;77(4):305–311. doi: 10.1097/00001888-200204000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Keating NL, Herrinton LJ, Zaslavsky AM, Liu L, Ayanian JZ. Variations in hospice use among cancer patients. JNCI: Journal of the National Cancer Institute. 2006;98(15):1053–1059. doi: 10.1093/jnci/djj298. [DOI] [PubMed] [Google Scholar]
- 30.Matsuyama R, Reddy S, Smith TJ. Why do patients choose chemotherapy near the end of life? A review of the perspective of those facing death from cancer. [Accessed 20060719];J Clin Oncol. 2006 24(21):3490–3496. doi: 10.1200/JCO.2005.03.6236. doi: https://dx.doi.org/10.1200/JCO.2005.03.6236. [DOI] [PubMed] [Google Scholar]
- 31.Weeks JC, Catalano PJ, Cronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. [Accessed 20121025];N Engl J Med. 2012 367(17):1616–1625. doi: 10.1056/NEJMoa1204410. doi: https://dx.doi.org/10.1056/NEJMoa1204410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stremikis K, Schoen C, Fryer AK. A call for change: The 2011 commonwealth fund survey of public views of the U.S. health system. Issue Brief (Commonw Fund) 2011;6:1–23. [PubMed] [Google Scholar]
- 33.Jacobson M, O'Malley AJ, Earle CC, Pakes J, Gaccione P, Newhouse JP. Does reimbursement influence chemotherapy treatment for cancer patients? [Accessed 20060308];Health Aff (Millwood) 2006 25(2):437–443. doi: 10.1377/hlthaff.25.2.437. doi: https://dx.doi.org/10.1377/hlthaff.25.2.437. [DOI] [PubMed] [Google Scholar]
- 34.Colla CH, Morden NE, Skinner JS, Hoverman JR, Meara E. Impact of payment reform on chemotherapy at the end of life. [Accessed 20120903];J Oncol Pract. 2012 8(3 Suppl):e6s–e13s. doi: 10.1200/JOP.2012.000539. doi: https://dx.doi.org/10.1200/JOP.2012.000539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Centers for Medicare & Medicade Services. Hospice quality reporting. [Accessed 3/8, 2017]; https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Hospice-Quality-Reporting/index.html.
- 36.Teno JM, Casarett D, Spence C, Connor S. It is “Too late” or is it? bereaved family member perceptions of hospice referral when their family member was on hospice for seven days or less. J Pain Symptom Manage. 2012;43(4):732–738. doi: 10.1016/j.jpainsymman.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 37.Lackan NA, Ostir GV, Freeman JL, Mahnken JD, Goodwin JS. Decreasing variation in the use of hospice among older adults with breast, colorectal, lung, and prostate cancer. Med Care. 2004;42(2):116–122. doi: 10.1097/01.mlr.0000108765.86294.1b. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Medicare and Medicaid Services. Centers for medicare and medicaid services (CMS) provider of service file (POS) 2012 [Google Scholar]
- 39.Welch WP, Miller ME, Welch HG, Fisher ES, Wennberg JE. Geographic variation in expenditures for physicians' services in the united states. N Engl J Med. 1993;328(9):621–627. doi: 10.1056/NEJM199303043280906. [DOI] [PubMed] [Google Scholar]
- 40.Wennberg JECM. The quality of medical care in the united states: A report on the medicare program. Chicago, IL: American Hospital Association Press; 1999. [PubMed] [Google Scholar]
- 41.Virnig BA, Kind S, McBean M, Fisher E. Geographic variation in hospice use prior to death. J Am Geriatr Soc. 2000;48(9):1117–1125. doi: 10.1111/j.1532-5415.2000.tb04789.x. [DOI] [PubMed] [Google Scholar]
- 42.Wang SY, Aldridge MD, Gross CP, et al. End-of-life care intensity and hospice use: A regional-level analysis. Med Care. 2016;54(7):672–678. doi: 10.1097/MLR.0000000000000547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goodman DC, Fisher ES, Bronner KK. Hospital and physician capacity update. The Dartmouth Institute for Health Policy and Clinical Practice. 2009 [PubMed] [Google Scholar]
- 44.Iwashyna TJ, Chang VW, Zhang JX, Christakis NA. The lack of effect of market structure on hospice use. Health Serv Res. 2002;37(6):1531–1551. doi: 10.1111/1475-6773.10562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saito AM, Landrum MB, Neville BA, Ayanian JZ, Weeks JC, Earle CC. Hospice care and survival among elderly patients with lung cancer. [Accessed 20110803];J Palliat Med. 2011 14(8):929–939. doi: 10.1089/jpm.2010.0522. doi: https://dx.doi.org/10.1089/jpm.2010.0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Borum ML, Lynn J, Zhong Z. The effects of patient race on outcomes in seriously ill patients in SUPPORT: An overview of economic impact, medical intervention, and end-of-life decisions. study to understand prognoses and preferences for outcomes and risks of treatments. J Am Geriatr Soc. 2000;48(5 Suppl):S194–8. doi: 10.1111/j.1532-5415.2000.tb03132.x. [DOI] [PubMed] [Google Scholar]
- 47.Obermeyer Z, Clarke AC, Makar M, Schuur JD, Cutler DM. Emergency care use and the medicare hospice benefit for individuals with cancer with a poor prognosis. J Am Geriatr Soc. 2016;64(2):323–329. doi: 10.1111/jgs.13948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miller SC, Weitzen S, Kinzbrunner B. Factors associated with the high prevalence of short hospice stays. J Palliat Med. 2003;6(5):725–736. doi: 10.1089/109662103322515239. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.