Abstract
Medication adherence is a complex, multi-determined behavior that is often influenced by system- (e.g., cost), drug- (e.g., regimen complexity), and patient-related (e.g., depression) factors. System-level approaches (e.g., making medications more affordable) are critically important but do not address patient-level factors that can undermine adherence. In this paper, we identify patient-level determinants of non-adherence and discuss whether mindfulness-training approaches that target these determinants can help to improve adherence to medical treatment. We highlight two chronic medical conditions (viz., heart failure, HIV) where poor adherence is a significant concern, and examine the evidence regarding the use of mindfulness interventions to improve medication adherence in these two conditions. We also discuss the theoretical underpinnings of mindfulness training with respect to medication adherence, and conclude by suggesting directions for future research.
Introduction
Adherence has been defined as “the extent to which a person’s behavior (e.g., taking a medication, following physical activity prescriptions, attending clinics) coincides with medical advice.” (1) Adherence is a multi-determined behavior, influenced by socioeconomic, health care system-, treatment- and patient-related factors. (2) Patient-level factors (e.g., depression, poor cognitive function, substance use) play an important role in determining adherence and interact with system-levels factors in ways that are often unpredictable and unique to each patient. (2)
Poor adherence to medical regimens is a significant clinical and public health problem. Regardless of the disease or the population considered, poor medication adherence is highly prevalent, even in survivors of serious diseases. Among patients recovering from an acute myocardial infarction, 8% to 20% are no longer taking key medications (such as ACE inhibitors, statin, and aspirin) 6 months after hospital discharge.(3) Among patients with heart failure (HF), medication adherence rates average only 50% (4) and declines over time even among patients who are initially adherent. (5–7) Only about 30% of HIV-positive individuals adhere to antiretroviral medications to the point of achieving viral suppression. (8, 9)
Adherence behaviors have been targeted by a range of interventions. A review by the Agency for Health Care Research and Quality found that the most effective approaches are policy-level interventions, such as programs to lower cost by reducing out-of-pocket expenses, case management, and educational interventions. Some patients, however, remain poorly adherent even when such policy-level interventions are implemented, indicating that system-level approaches are necessary, but likely not sufficient in all patients. More comprehensive adherence approaches that address patient-level determinants of medication adherence are needed.
In this paper, we discuss the possible usefulness of mindfulness training to improve medication adherence, focusing on two chronic conditions: heart failure (HF) and HIV. We chose these conditions as examples because (a) both are chronic diseases in which poor medication adherence is prevalent, and (b) in both conditions, poor medication adherence has major consequences on clinical outcomes. First, we identify patient-level barriers to adherence. Next, we describe mindfulness interventions, review the evidence in support of mindfulness training to improve medication adherence, and present a conceptual model illustrating the possible mechanisms by which mindfulness training might improve adherence. We conclude by making recommendations for future research.
Example 1: Heart Failure and Poor Medication Adherence
Heart failure (HF) is characterized by the inability of the heart to pump the necessary amount of blood to the peripheral tissues. Symptoms include shortness of breath, fatigue, limited exercise tolerance, and fluid retention. (10) Due to the aging of the population, HF is becoming increasingly prevalent in Western countries; (11) in the United States alone, 5.7 million individuals are currently affected. (12–16) The prognosis of HF is largely unfavorable, with hospital re-admission rates reaching 50% within 6 months of discharge (17, 18) and 5-year mortality rates of 50%. (10, 14, 19) Medical therapy improves symptoms and reduces re-hospitalizations and mortality, (20, 21), however such treatments are effective only if patients take their medications regularly; instead, adherence to pharmacological treatment among HF patients is, on average, only 50% (4) and tends to decline over time even among individuals who were initially adherent.(5–7) Poor medication adherence results in high rates of emergency room visits, hospital re-admissions, and mortality. (22–27)
Patient-level Barriers to Medication Adherence in Heart Failure
At the patient level, cognitive impairment, sleep disorders, and depressive symptoms have all been associated with poor adherence.
Cognitive impairment is prevalent among HF patients: in a study conducted among veteran outpatients, previously unrecognized cognitive impairment was found in 58% of subjects; verbal learning, immediate memory, and delayed verbal memory were most impaired. (28) Another study found that a similar proportion of adults with HF had below average measures of cognitive function. (29) Measures of cognitive impairment such as forgetfulness, (4) attention lapses, (30–32) and poor executive function (33) have all been associated with poor medication adherence among adults with HF. The lapses in attention reported among HF patients reduce the patients’ ability to develop consistent adherence patterns; in fact, attentional lapses have been significantly associated with poor medication adherence, (30–32) and forgetfulness is one of the most common barriers to adherence in this population. (4)
Sleep disorders are common among HF patients. (34, 35) Excessive daytime sleepiness (EDS; a consequence of poor sleep quality), (35) was a significant predictor of poor medication adherence in a longitudinal study conducted among 280 HF patients, with 10% increases in non-adherence per each unit increase in EDS (p = .008). (30) Another longitudinal study found that daytime sleepiness was associated with a steep decline in objectively measured adherence. (31) One mechanism by which excessive daytime sleepiness may result in poor adherence behaviors is through cognitive impairment and impairment in vigilant attention. (36) Indeed, EDS has been associated with below average performance on the digit symbol substitution task, a sensitive measure of cognitive performance in HF patients. (29)
Finally, depressive symptoms are reported by about 60% of HF patients (both hospitalized patients and outpatients) (37) and have been associated with poor adherence to medical treatment. (4, 38)
Example 2: HIV/AIDS and Poor Medication Adherence
More than one million adults and adolescents in the United States are currently living with HIV, a virus that attacks the body’s immune system and specifically CD4 cells. (39) If left untreated, HIV progressively reduces the number of CD4 cells and makes the individual susceptible to opportunistic infections and to infection-related cancers. Although there is no cure for HIV, this disease can be controlled successfully with medical treatment. Antiretroviral therapy (ART) has changed the course of this disease by improving viral suppression, reducing infectiousness and HIV-related morbidities, and increasing survival. (40–42) Strict adherence to ART is recommended (43) and yet only 30% of persons living with HIV (PLWH) adhere to ART to the point of achieving viral suppression. (8, 9) Sub-optimal adherence to ART compromises individual health, increases health care costs, and can lead to the development of ART-resistant strains of HIV. (42, 44)
Patient-level Barriers to ART Adherence among PLWH
Among the patient-level barriers to ART adherence among PLWH, life stress and depression are particularly important. (45)
Life stress is common in PLWH. The HIV epidemic disproportionately affects people with considerable economic disadvantage, including those who live in poverty, are homeless, and who experience food insecurity. (46) In addition, many PLWH are members of socially discriminated groups, including racial/ethnic minorities, sexual minorities, and people struggling with mental health or substance use problems. (47–50) HIV remains a stigmatized disease, and some PLWH are reluctant to disclose their serostatus for fear of social rejection. Life stress is important for disease progression because, in addition to undermining ART adherence, stress can directly suppresses immune functioning (and levels of CD4 cells), thereby exacerbating the effects of poor adherence on viral load.
Depression is also a frequent problem given the life-threatening nature of HIV combined with the stressful life circumstances described above. (51, 52) Both depression and stress have been strongly associated with poor ART adherence. (45, 53–62)
Interestingly, predictors of non-adherence to medications among patients living with HF and HIV are similar. Both conditions are associated with depression, which often undermines sleep, which is in turn necessary for optimal cognitive functioning. Indeed, all three factors have been associated with non-adherence across many chronic diseases. Specifically, a meta-analysis of 31 studies involving 18,245 participants found that depressed patients were 1.76 times more likely to be non-adherent than non-depressed patient, and the association was consistent across different chronic conditions. (63)
Mindfulness Training and Medication Adherence
Mindfulness is the most common translation of the word “sati” in Pali, the language in which the most ancient Buddhist texts were originally written. A different translation, perhaps better rendering the fact that mindfulness can be cultivated through practice, (64, 65) is “to be mindful.” Mindfulness has been defined as a “the act of paying attention in a special way – in present moment, with kindness, and non-judgmentally.” (66) Although Western psychology places great emphasis on these “attentional” and more “static” qualities of mindfulness – and certainly such aspects receive great attention in the early phases of mindfulness training – Buddhist scholars have highlighted the cognitive aspect of mindfulness and its connections with working memory. Another meaning of “sati” is in fact “to remember, to keep in mind.” (67)
Mindfulness training (MT) programs – including the well-known Mindfulness-Based Stress Reduction program (MBSR) (66) – are adaptations to a Western, secular context of meditation practices rooted in the Buddhist tradition of the South Eastern regions of Asia. (66) In general, mindfulness training involves learning to notice events arising in the field of consciousness at any given moment and to re-direct attention to the breath (or to any other chosen focus of attention). Research has shown that the cultivation of this particular way of focusing and redirecting attention facilitates self-regulation and strengthens the ability of the individual to avoid absorption in maladaptive and habitual mental patterns, behaviors, and emotional reactions. (68–70)
There is mounting evidence supporting the efficacy of MT on several of the aforementioned patient-level barriers to adherence. Consequently, the potential therapeutic value of mindfulness training for medication adherence has been the subject of research interest in the past decade. We hereby present a summary of the evidence supporting the efficacy on MT on several determinants of adherence behaviors in HIV and HF patients, namely, stress, depressive symptoms, cognitive impairment, and sleep.
Stress and depressive symptoms
A meta-analytical review of 39 studies of MT for a range of psychiatric or medical conditions reported that MT led to robust and sustained reductions in self-reported anxiety and depressive symptoms (Hedge s g = 0.95). (71) A systematic review of 31 RCTs found medium-sized post-intervention effects for depression (g = 0.54) and for stress/distress (g = 0.56). (72) Another meta-analysis of studies focusing on participants with a current depressive or anxiety episode found significant benefits on depressive symptom severity for MT relative to controls (73). Three recent meta-analyses reported significant effects (and moderate effect sizes) of MT on depressive symptoms among patients with diverse medical conditions, (74–76) and a meta-analysis of MT delivered online had a significant beneficial impact on depression, mindfulness skills, and stress, with effect sizes ranging from small to moderate. (77)
Cognitive function
The role of attention in cognitive processing consists in selecting which sensory input, among many present at any given moment, will be processed for memory storage and/or further processing. Attention works in two “operating modes” (a) it can be involuntarily captured by salient stimuli from the environment (“alerting attention”) (78) and (b) it can be voluntarily directed according to the needs or purposes of the individual (“oriented attention” (79, 80). Alerting attention is critical for situations that require a rapid response (e.g., an environmental threat). However, in modern life, the threats we face are less immediately existential. Therefore, to complete most tasks, we must ignore irrelevant stimuli and focus instead on stimuli that are relevant for our goals. Neurophysiological studies have shown that the ability to override irrelevant stimuli is associated with working memory capacity, thus indicating that the ability to sustain attention is fundamental for cognitive processing. (81) The initial phases of MT, which emphasize concentration practices (i.e., focusing the attention on the sensations associated with breathing and on bodily sensations), have been shown to improve selective and executive attention. (82–84) Both observational and experimental studies have shown that MT improves memory and cognitive performance. (84) For example, a RCT of a 2-week mindfulness intervention conducted among graduate students demonstrated that mindfulness training improved working memory capacity and reduced the occurrence of distracting thoughts during completion of the graduate record examination. (85) Jha et al. observed an increase in working memory capacity among military personnel who underwent an 8-week mindfulness intervention compared to both military and civilian control groups. (86) A study conducted among experienced meditators showed better performances on all attention measures compared to controls without meditation experience. In the latter study, the duration of individual mindfulness practice correlated positively with measures of attention. (87) Finally, a RCT conducted among 201 older adults demonstrated that participants trained in MBSR showed significant improvements in measures of executive function compared to those in the wait-list control group. (88)
Sleep
Numerous experimental and observational studies across diverse patient populations have found that mindfulness interventions improve sleep quality. (89–93) Significant improvements in sleep quality were found in a RCT of MBSR for women with post-menopausal symptoms versus a wait-list control group. (90) Our group detected improvements in sleep quality ratings after MBSR training compared to baseline among healthy individuals. (89) Gross et al. found that mindfulness training was as effective as pharmacological treatment in improving objective and subjective measures of sleep among adults with chronic insomnia. (92) Another RCT demonstrated that an 8-week mindfulness-based intervention conducted among depressed individuals improved objective (polysomnographic) and subjective measures of sleep, decreased wake time, and increased sleep efficiency. (93)
Evidence supporting the effect of MT on medication adherence. Despite the large body of literature supporting the efficacy of MT on key patient-level determinants of adherence, few studies have investigated the effect of mindfulness training on medication adherence. In the context of cardiovascular disease, there have been no studies of the effect of MT on adherence even though the possible benefit has been suggested. (94) In the context of HIV/AIDS, there has been only very limited research. A RCT explored the efficacy of MBSR compared to a wait-list control group on symptoms and bother/distress related to ART side effects (primary outcome) and self-reported medication adherence (secondary outcome). Results did not show any improvement in ART adherence. (95) It is important to note, however, that in this study, baseline ART adherence was already high, thus undermining the chance to observe improvements (i.e., a ceiling effect). Results from a pilot RCT of MBSR for stress reduction in HIV-infected youth have shown that the intervention group was more likely to have a lower viral load at follow-up (p = .04) compared to the control group, a finding that could be explained by improved ART adherence. (96) A large RCT to determine efficacy of MT on ART adherence among HIV-infected urban youth is now under way (ClinicalTrials.gov NCT02624193).
Proposed Conceptual Model Linking Mindfulness Training and Medication Adherence
The benefits of mindfulness training hinge upon two assumptions. First, we assume that patients receive an adequate dose of the MT intervention both with respect to instruction and individual practice. (97) Second, we assume that mindfulness is a skill that can be cultivated through training and practice. Despite the limitations and challenges encountered in the measurement of mindfulness, (98) studies have shown that mindfulness skills improve in response to training and that the effect of mindfulness interventions on various health outcomes is mediated by improvements in mindfulness levels. (64, 65, 97)
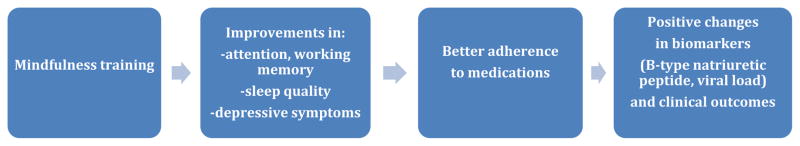
Our model builds upon two extant theories of mindfulness, (68, 69) and on empirical evidence regarding the efficacy of MT on predictors of medication adherence (viz., cognitive impairment, poor sleep quality, depressive symptoms, and stress). Guided by theory and research, we propose the following conceptual model to guide future research. As shown in Figure 1, we posit that mindfulness training could improve adherence via improvements in attention and working memory, sleep, stress and depressive symptoms. Positive changes in adherence will in turn result in improvements in biomarkers and clinical outcomes.
Figure 1.
We note that the proposed model is a only a “roadmap” to guide future research on mindfulness and medication adherence and it is by no means exhaustive of all the possible ways in which mindfulness training can affect the various factors that influence medication adherence. This model will likely evolve as new experimental evidence confirms or refutes our hypotheses, and as research shows that mindfulness training can affect other important patient-level determinants of medication adherence.
Directions For Future Research
As noted above, currently available interventions to promote medication adherence do not sufficiently target important patient-level determinants of adherence. Mindfulness interventions have been proven effective on several predictors of poor adherence (i.e., sleep, cognitive impairment, depression, and stress) and thus hold great potential to improve medication adherence. At present, however, there is only limited, preliminary evidence for an effect of mindfulness training on medication adherence. Future studies should be well-designed randomized controlled trials including both self-reported and objective measures of adherence (e.g., MEMS caps or pill counts), rigorous intervention protocols, and monitoring of intervention fidelity. In addition to traditional class-based training, non-traditional mobile-health approaches (i.e., web-based training, phone delivery, and smartphone mindfulness applications) hold great promise for removing barriers to access (e.g., transportation, parking, group scheduling), reducing costs, and for promoting the dissemination of mindfulness interventions. (77)
In sum, based on the previously expounded arguments, we believe that the exploration of the role of mindfulness meditation in the promotion of medication adherence is a worthwhile research endeavor that has great potential to contribute to the improvement of this relevant public health problem.
Acknowledgments
The writing of this paper was supported by a grant from the National Centers for Complementary and Integrative Health (R34-AT008930) to Drs. Carey and Salmoirago-Blotcher.
The funding agency had no involvement in the writing of this paper or in the decision to submit it for publication.
Footnotes
Conflicts of Interest: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Haynes RB, Taylor DW, Sackett DL. Compliance in health care. Baltimore: Johns Hopkins University Press; 1979. p. xvi.p. 516. [Google Scholar]
- 2.Overview: Medication Adherence—Where Are We Today? Geneva, Switzerland: 2003. [Google Scholar]
- 3.Eagle KA, Kline-Rogers E, Goodman SG, Gurfinkel EP, Avezum A, Flather MD, et al. Adherence to evidence-based therapies after discharge for acute coronary syndromes: an ongoing prospective, observational study. The American journal of medicine. 2004 Jul 15;117(2):73–81. doi: 10.1016/j.amjmed.2003.12.041. [DOI] [PubMed] [Google Scholar]
- 4.Wu JR, Moser DK, Lennie TA, Burkhart PV. Medication adherence in patients who have heart failure: a review of the literature. Nurs Clin N Am. 2008 Mar;43(1):133-+. doi: 10.1016/j.cnur.2007.10.006. WOS:000253819200009. English. [DOI] [PubMed] [Google Scholar]
- 5.Wu JR, Corley DJ, Lennie TA, Moser DK. Effect of a medication-taking behavior feedback theory-based intervention on outcomes in patients with heart failure. Journal of cardiac failure. 2012 Jan;18(1):1–9. doi: 10.1016/j.cardfail.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler J, Arbogast PG, Daugherty J, Jain MK, Ray WA, Griffin MR. Outpatient utilization of angiotensin-converting enzyme inhibitors among heart failure patients after hospital discharge. J Am Coll Cardiol. 2004 Jun 2;43(11):2036–43. doi: 10.1016/j.jacc.2004.01.041. [DOI] [PubMed] [Google Scholar]
- 7.DiMatteo MR, Sherbourne CD, Hays RD, Ordway L, Kravitz RL, McGlynn EA, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: results from the Medical Outcomes Study. Health psychology: official journal of the Division of Health Psychology, American Psychological Association. 1993 Mar;12(2):93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 8.Bradley H, Hall HI, Wolitski RJ, van Handel MM, Stone AE, LaFlam M, et al. Vital Signs: HIV Diagnosis, care, and treatment among persons living with HIV -- United States, 2011. Morbidity and Mortality Weekly Report. 2014;63:1–6. [PMC free article] [PubMed] [Google Scholar]
- 9.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013 Oct;57(8):1164–71. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 10.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jun 5; doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed]
- 11.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013 May;6(3):606–19. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Executive summary: heart disease and stroke statistics-2015 update: a report from the american heart association. Circulation. 2015 Jan 27;131(4):434–41. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 13.Curtis LH, Whellan DJ, Hammill BG, Hernandez AF, Anstrom KJ, Shea AM, et al. Incidence and prevalence of heart failure in elderly persons, 1994–2003. Arch Intern Med. 2008 Feb 25;168(4):418–24. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 14.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, et al. Trends in heart failure incidence and survival in a community-based population. JAMA: the journal of the American Medical Association. 2004 Jul 21;292(3):344–50. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 15.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013 Jan 1;127(1):143–52. doi: 10.1161/CIR.0b013e318282ab8f. [DOI] [PubMed] [Google Scholar]
- 16.Dar O, Cowie MR. The epidemiology and diagnosis of heart failure. In: Fuster V, Walsh R, Harrington R, editors. Hurst’s The Heart. 13. McGraw Hill; 2010. [Google Scholar]
- 17.Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, et al. Patterns of Hospital Performance in Acute Myocardial Infarction and Heart Failure 30-Day Mortality and Readmission. Circulation: Cardiovascular Quality and Outcomes. 2009 Sep 1;2(5):407–13. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 18.Chun S, Tu JV, Wijeysundera HC, Austin PC, Wang X, Levy D, et al. Lifetime analysis of hospitalizations and survival of patients newly admitted with heart failure. Circulation Heart failure. 2012 Jul 1;5(4):414–21. doi: 10.1161/CIRCHEARTFAILURE.111.964791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, et al. Long-term trends in the incidence of and survival with heart failure. The New England journal of medicine. 2002 Oct 31;347(18):1397–402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 20.Cubbon RM, Gale CP, Kearney LC, Schechter CB, Brooksby WP, Nolan J, et al. Changing characteristics and mode of death associated with chronic heart failure caused by left ventricular systolic dysfunction: a study across therapeutic eras. Circulation Heart failure. 2011 Jul;4(4):396–403. doi: 10.1161/CIRCHEARTFAILURE.110.959882. [DOI] [PubMed] [Google Scholar]
- 21.Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80% Bmj. 2003 Jun 28;326(7404):1419. doi: 10.1136/bmj.326.7404.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li H, Morrow-Howell N, Proctor EK. Post-acute home care and hospital readmission of elderly patients with congestive heart failure. Health & social work. 2004 Nov;29(4):275–85. doi: 10.1093/hsw/29.4.275. [DOI] [PubMed] [Google Scholar]
- 23.Hope CJ, Wu J, Tu W, Young J, Murray MD. Association of medication adherence, knowledge, and skills with emergency department visits by adults 50 years or older with congestive heart failure. American journal of health-system pharmacy: AJHP: official journal of the American Society of Health-System Pharmacists. 2004 Oct 1;61(19):2043–9. doi: 10.1093/ajhp/61.19.2043. [DOI] [PubMed] [Google Scholar]
- 24.Esposito D, Bagchi AD, Verdier JM, Bencio DS, Kim MS. Medicaid beneficiaries with congestive heart failure: association of medication adherence with healthcare use and costs. The American journal of managed care. 2009 Jul;15(7):437–45. [PubMed] [Google Scholar]
- 25.Fitzgerald AA, Powers JD, Ho PM, Maddox TM, Peterson PN, Allen LA, et al. Impact of medication nonadherence on hospitalizations and mortality in heart failure. Journal of cardiac failure. 2011 Aug;17(8):664–9. doi: 10.1016/j.cardfail.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 26.Wu JR, Moser DK, Chung ML, Lennie TA. Objectively measured, but not self-reported, medication adherence independently predicts event-free survival in patients with heart failure. Journal of cardiac failure. 2008 Apr;14(3):203–10. doi: 10.1016/j.cardfail.2007.11.005. WOS:000254962000004. English. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miura T, Kojima R, Mizutani M, Shiga Y, Takatsu F, Suzuki Y. Effect of digoxin noncompliance on hospitalization and mortality in patients with heart failure in long-term therapy: a prospective cohort study. European journal of clinical pharmacology. 2001 Apr;57(1):77–83. doi: 10.1007/s002280100272. [DOI] [PubMed] [Google Scholar]
- 28.Hawkins LA, Kilian S, Firek A, Kashner TM, Firek CJ, Silvet H. Cognitive impairment and medication adherence in outpatients with heart failure. Heart & lung: the journal of critical care. 2012 Nov-Dec;41(6):572–82. doi: 10.1016/j.hrtlng.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 29.Riegel B, Lee CS, Glaser D, Moelter ST. Patterns of Change in Cognitive Function over Six Months in Adults with Chronic Heart Failure. Cardiology research and practice. 2012;2012:631075. doi: 10.1155/2012/631075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Riegel B, Moelter ST, Ratcliffe SJ, Pressler SJ, De Geest S, Potashnik S, et al. Excessive daytime sleepiness is associated with poor medication adherence in adults with heart failure. Journal of cardiac failure. 2011 Apr;17(4):340–8. doi: 10.1016/j.cardfail.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riegel B, Lee CS, Ratcliffe SJ, De Geest S, Potashnik S, Patey M, et al. Predictors of objectively measured medication nonadherence in adults with heart failure. Circulation Heart failure. 2012 Jul 1;5(4):430–6. doi: 10.1161/CIRCHEARTFAILURE.111.965152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dinges DF, Pack F, Williams K, Gillen KA, Powell JW, Ott GE, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep. 1997 Apr;20(4):267–77. [PubMed] [Google Scholar]
- 33.Alosco ML, Spitznagel MB, van Dulmen M, Raz N, Cohen R, Sweet LH, et al. Cognitive function and treatment adherence in older adults with heart failure. Psychosomatic medicine. 2012 Nov-Dec;74(9):965–73. doi: 10.1097/PSY.0b013e318272ef2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.MacDonald M, Fang J, Pittman SD, White DP, Malhotra A. The current prevalence of sleep disordered breathing in congestive heart failure patients treated with beta-blockers. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine. 2008 Feb 15;4(1):38–42. [PMC free article] [PubMed] [Google Scholar]
- 35.Riegel B, Ratcliffe SJ, Sayers SL, Potashnik S, Buck HG, Jurkovitz C, et al. Determinants of excessive daytime sleepiness and fatigue in adults with heart failure. Clinical nursing research. 2012 Aug;21(3):271–93. doi: 10.1177/1054773811419842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lim J, Dinges DF. Sleep deprivation and vigilant attention. Annals of the New York Academy of Sciences. 2008;1129:305–22. doi: 10.1196/annals.1417.002. [DOI] [PubMed] [Google Scholar]
- 37.Moser DK, Dracup K, Evangelista LS, Zambroski CH, Lennie TA, Chung ML, et al. Comparison of prevalence of symptoms of depression, anxiety, and hostility in elderly patients with heart failure, myocardial infarction, and a coronary artery bypass graft. Heart & lung: the journal of critical care. 2010 Sep-Oct;39(5):378–85. doi: 10.1016/j.hrtlng.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tang HY, Sayers SL, Weissinger G, Riegel B. The Role of Depression in Medication Adherence Among Heart Failure Patients. Clinical nursing research. 2013 Apr 2; doi: 10.1177/1054773813481801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. [Accessed [27 June 2016]];HIV Surveillance Report. 2014 26 http://www.cdc.gov/hiv/library/reports/surveillance/. Published November 2015. 2015. [Google Scholar]
- 40.Buchacz K, Baker RK, Moorman AC, Richardson JT, Wood KC, Holmberg SD, et al. Rates of hospitalizations and associated diagnoses in a large multisite cohort of HIV patients in the United States, 1994–2005. AIDS. 2008;22:1345–56. doi: 10.1097/QAD.0b013e328304b38b. [DOI] [PubMed] [Google Scholar]
- 41.Palella FJ, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med. 1998;338:853–60. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 42.Giordano TP, Gifford AL, White AC, Suarez-Almazor ME, Rabeneck L, Hartman C, et al. Retention in care: A challenge to survival with HIV infection. Clinical Infectious Diseases. 2007;44:1493–9. doi: 10.1086/516778. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Living with HIV [10/28/2014] Available from: http://www.cdc.gov/hiv/living/index.html.
- 44.Park WB, Choe PG, Kim SH, Jo JH, Bang JH, Kim HB, et al. One-year adherence to clinic visits after highly active antiretroviral therapy: a predictor of clinical progress in HIV patients. Journal of internal medicine. 2007 Mar;261(3):268–75. doi: 10.1111/j.1365-2796.2006.01762.x. [DOI] [PubMed] [Google Scholar]
- 45.Langebeek N, Gisolf EH, Reiss P, Vervoort SC, Hafsteinsdottir TB, Richter C, et al. Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC medicine. 2014;12:142. doi: 10.1186/s12916-014-0142-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kalichman SC, Grebler T. Stress and poverty predictors of treatment adherence among people with low-literacy living with HIV/AIDS. Psychosomatic medicine. 2010 Oct;72(8):810–6. doi: 10.1097/PSY.0b013e3181f01be3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Crawford N, Galea S, Ford C, Latkin C, Link B, Fuller C. The Relationship Between Discrimination and High-Risk Social Ties by Race/Ethnicity: Examining Social Pathways of HIV Risk. J Urban Health. 2014 Feb 01;91(1):151–61. doi: 10.1007/s11524-013-9806-y. English. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hurd NM, Varner FA, Caldwell CH, Zimmerman MA. Does perceived racial discrimination predict changes in psychological distress and substance use over time? An examination among Black emerging adults. Developmental Psychology. 2014;50(7):1910–8. doi: 10.1037/a0036438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological bulletin. 2009 Sep;135(5):707–30. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological bulletin. 2003 Sep;129(5):674–97. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285(11):1466–74. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- 52.Do AN, Rosenberg ES, Sullivan PS, Beer L, Strine TW, Schulden JD, et al. Excess Burden of Depression among HIV-Infected Persons Receiving Medical Care in the United States: Data from the Medical Monitoring Project and the Behavioral Risk Factor Surveillance System. PloS one. 2014;9(3):e92842. doi: 10.1371/journal.pone.0092842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Starace F, Ammassari A, Trotta MP, Murri R, De Longis P, Izzo C, et al. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. Journal of acquired immune deficiency syndromes. 2002 Dec 15;31( Suppl 3):S136–9. doi: 10.1097/00126334-200212153-00010. [DOI] [PubMed] [Google Scholar]
- 54.Uthman OA, Magidson JF, Safren SA, Nachega JB. Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Current HIV/AIDS reports. 2014 Sep;11(3):291–307. doi: 10.1007/s11904-014-0220-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Blashill AJ, Gordon JR, Safren SA. Depression longitudinally mediates the association of appearance concerns to ART non-adherence in HIV-infected individuals with a history of injection drug use. Journal of behavioral medicine. 2014 Feb;37(1):166–72. doi: 10.1007/s10865-012-9476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wagner GJ, Goggin K, Remien RH, Rosen MI, Simoni J, Bangsberg DR, et al. A closer look at depression and its relationship to HIV antiretroviral adherence. Annals of Behavioral Medicine. 2011 Dec;42(3):352–60. doi: 10.1007/s12160-011-9295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kong MC, Nahata MC, Lacombe VA, Seiber EE, Balkrishnan R. Association between race, depression, and antiretroviral therapy adherence in a low-income population with HIV infection. Journal of general internal medicine. 2012 Sep;27(9):1159–64. doi: 10.1007/s11606-012-2043-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gibbie T, Hay M, Hutchison CW, Mijch A. Depression, social support and adherence to highly active antiretroviral therapy in people living with HIV/AIDS. Sexual health. 2007 Dec;4(4):227–32. doi: 10.1071/sh06062. [DOI] [PubMed] [Google Scholar]
- 59.Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. Journal of acquired immune deficiency syndromes. 2011 Oct 1;58(2):181–7. doi: 10.1097/QAI.0b013e31822d490a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ortego C, Huedo-Medina TB, Llorca J, Sevilla L, Santos P, Rodriguez E, et al. Adherence to highly active antiretroviral therapy (HAART): a meta-analysis. AIDS and behavior. 2011 Oct;15(7):1381–96. doi: 10.1007/s10461-011-9942-x. [DOI] [PubMed] [Google Scholar]
- 61.White JM, Gordon AJ, Mimiaga MJ. The role of substance use and mental health problems in medication adherence among HIV-infected MSM. LGBT Health. 2014:2. doi: 10.1089/lgbt.2014.0020. [DOI] [PubMed] [Google Scholar]
- 62.Springer SA, Dushaj A, Azar MM. The impact of DSM-IV mental disorders on adherence to combination antiretroviral therapy among adult persons living with HIV/AIDS: a systematic review. AIDS and behavior. 2012 Nov;16(8):2119–43. doi: 10.1007/s10461-012-0212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Grenard JL, Munjas BA, Adams JL, Suttorp M, Maglione M, McGlynn EA, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. Journal of general internal medicine. 2011 Oct;26(10):1175–82. doi: 10.1007/s11606-011-1704-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baer RA. Self-Focused Attention and Mechanisms of Change in Mindfulness-Based Treatment. Cognitive Behaviour Therapy. 2009;38(1 supp 1):15–20. doi: 10.1080/16506070902980703. [DOI] [PubMed] [Google Scholar]
- 65.Nyklicek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2008 Jun;35(3):331–40. doi: 10.1007/s12160-008-9030-2. Epub 2008/06/07. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing; 1990. [Google Scholar]
- 67.Dreyfus GB. Is mindfulness present-centred and non-judgmental? A discussion of the cognitive dimensions of mindfulness. Contemporary Buddhism. 2011;12(1):41–54. [Google Scholar]
- 68.Malinowski P. Neural mechanisms of attentional control in mindfulness meditation. Frontiers in neuroscience. 2013;7:8. doi: 10.3389/fnins.2013.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. Journal of clinical psychology. 2006;62:373–86. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- 70.Carmody J. Evolving conceptions of mindfulness in clinical settings. Journal of Cognitive Psychotherapy. 2009;23(3) [Google Scholar]
- 71.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Journal of consulting and clinical psychology. 2010;78:169. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.de Vibe M, Bjorndal A, Tipton E, Hammerstrom KT, Kowalski K. Mindfulness based stress reduction (MBSR) for improving health, quality of life and social functioning in adults. Campbell Systematic Reviews. 2012:3. [Google Scholar]
- 73.Strauss C, Cavanagh K, Oliver A, Pettman D. Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: a meta-analysis of randomised controlled trials. PLoS One. 2014;9(4):e96110. doi: 10.1371/journal.pone.0096110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. Journal of psychosomatic research. 2010 Jun;68(6):539–44. doi: 10.1016/j.jpsychores.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 75.Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation Programs for Psychological Stress and Well-being: A Systematic Review and Meta-analysis. JAMA internal medicine. 2014 Jan 6; doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Younge JO, Gotink RA, Baena CP, Roos-Hesselink JW, Hunink MM. Mind-body practices for patients with cardiac disease: a systematic review and meta-analysis. European journal of preventive cardiology. 2014 Sep 16; doi: 10.1177/2047487314549927. [DOI] [PubMed] [Google Scholar]
- 77.Spijkerman MP, Pots WT, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical psychology review. 2016 Apr;45:102–14. doi: 10.1016/j.cpr.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 78.Yantis S, Jonides J. Abrupt visual onsets and selective attention: voluntary versus automatic allocation. Journal of experimental psychology Human perception and performance. 1990 Feb;16(1):121–34. doi: 10.1037//0096-1523.16.1.121. [DOI] [PubMed] [Google Scholar]
- 79.Desimone R, Duncan J. Neural mechanisms of selective visual attention. Annual review of neuroscience. 1995;18:193–222. doi: 10.1146/annurev.ne.18.030195.001205. [DOI] [PubMed] [Google Scholar]
- 80.Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Annual review of neuroscience. 2001;24:167–202. doi: 10.1146/annurev.neuro.24.1.167. [DOI] [PubMed] [Google Scholar]
- 81.Fukuda K, Vogel EK. Human variation in overriding attentional capture. The Journal of neuroscience: the official journal of the Society for Neuroscience. 2009 Jul 8;29(27):8726–33. doi: 10.1523/JNEUROSCI.2145-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Canter PH, Ernst E. The cumulative effects of Transcendental Meditation on cognitive function - a systematic review of randomised controlled trials. Wien Klin Wochenschr. 2003 Nov 28;115(21–22):758–66. doi: 10.1007/BF03040500. WOS:000188061000005. English. [DOI] [PubMed] [Google Scholar]
- 83.Newberg AB, Wintering N, Khalsa DS, Roggenkamp H, Waldman MR. Meditation Effects on Cognitive Function and Cerebral Blood Flow In Subjects with Memory Loss: A Preliminary Study. J Alzheimers Dis. 2010;20(2):517–26. doi: 10.3233/JAD-2010-1391. WOS:000279537700017. English. [DOI] [PubMed] [Google Scholar]
- 84.Chiesa A, Calati R, Serretti A. Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clinical psychology review. 2011 Apr;31(3):449–64. doi: 10.1016/j.cpr.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 85.Mrazek MD, Franklin MS, Phillips DT, Baird B, Schooler JW. Mindfulness training improves working memory capacity and GRE performance while reducing mind wandering. Psychological science. 2013 May;24(5):776–81. doi: 10.1177/0956797612459659. [DOI] [PubMed] [Google Scholar]
- 86.Jha AP, Stanley EA, Kiyonaga A, Wong L, Gelfand L. Examining the protective effects of mindfulness training on working memory capacity and affective experience. Emotion. 2010 Feb;10(1):54–64. doi: 10.1037/a0018438. [DOI] [PubMed] [Google Scholar]
- 87.Moore A, Malinowski P. Meditation, mindfulness and cognitive flexibility. Consciousness and cognition. 2009 Mar;18(1):176–86. doi: 10.1016/j.concog.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 88.Moynihan JA, Chapman BP, Klorman R, Krasner MS, Duberstein PR, Brown KW, et al. Mindfulness-based stress reduction for older adults: effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology. 2013;68(1):34–43. doi: 10.1159/000350949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Salmoirago-Blotcher E, Hunsinger M, Morgan L, Fischer D, Carmody J. Mindfulness-Based Stress Reduction and Change in Health-Related Behaviors. Journal of Evidence-Based Complementary & Alternative Medicine. 2013 May;8:2013. [Google Scholar]
- 90.Carmody JF, Crawford S, Salmoirago-Blotcher E, Leung K, Churchill L, Olendzki N. Mindfulness training for coping with hot flashes: results of a randomized trial. Menopause. 2011 Jun;18(6):611–20. doi: 10.1097/gme.0b013e318204a05c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Britton WB, Haynes PL, Fridel KW, Bootzin RR. Mindfulness-based cognitive therapy improves polysomnographic and subjective sleep profiles in antidepressant users with sleep complaints. Psychotherapy and psychosomatics. 2012;81(5):296–304. doi: 10.1159/000332755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gross CR, Kreitzer MJ, Reilly-Spong M, Wall M, Winbush NY, Patterson R, et al. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: a randomized controlled clinical trial. Explore. 2011 Mar-Apr;7(2):76–87. doi: 10.1016/j.explore.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Andersen SR, Wurtzen H, Steding-Jessen M, Christensen J, Andersen KK, Flyger H, et al. Effect of mindfulness-based stress reduction on sleep quality: results of a randomized trial among Danish breast cancer patients. Acta oncologica. 2013 Feb;52(2):336–44. doi: 10.3109/0284186X.2012.745948. [DOI] [PubMed] [Google Scholar]
- 94.Loucks EB, Schuman-Olivier Z, Britton WB, Fresco DM, Desbordes G, Brewer JA, et al. Mindfulness and Cardiovascular Disease Risk: State of the Evidence, Plausible Mechanisms, and Theoretical Framework. Curr Cardiol Rep. 2015 Dec;17(12):112. doi: 10.1007/s11886-015-0668-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Duncan LG, Moskowitz JT, Neilands TB, Dilworth SE, Hecht FM, Johnson MO. Mindfulness-based stress reduction for HIV treatment side effects: a randomized, wait-list controlled trial. Journal of pain and symptom management. 2012 Feb;43(2):161–71. doi: 10.1016/j.jpainsymman.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sibinga EM, Perry-Parrish C, Thorpe K, Mika M, Ellen JM. A small mixed-method RCT of mindfulness instruction for urban youth. Explore. 2014 May-Jun;10(3):180–6. doi: 10.1016/j.explore.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 97.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008 Feb;31(1):23–33. doi: 10.1007/s10865-007-9130-7. Epub 2007/09/28. eng. [DOI] [PubMed] [Google Scholar]
- 98.Grossman P. On measuring mindfulness in psychosomatic and psychological research. Journal of psychosomatic research. 2008 Apr;64(4):405–8. doi: 10.1016/j.jpsychores.2008.02.001. [DOI] [PubMed] [Google Scholar]