Abstract
National HIV prevention goals call for interventions that address Continuum of HIV Care (CoC) for persons living with HIV. Electronic health (eHealth) can leverage technology to rapidly develop and disseminate such interventions. We conducted a qualitative review to synthesize (a) technology types, (b) CoC outcomes, (c) theoretical frameworks, and (d) behavior change mechanisms. This rapid review of eHealth, HIV-related articles (2007–2017) focused on technology-based interventions that reported CoC-related outcomes. Forty-five studies met inclusion criteria. Mobile texting was the most commonly reported technology (44.4%, k = 20). About 75% (k = 34) of studies showed proven or preliminary efficacy for improving CoC-related outcomes. Most studies (60%, k = 27) focused on medication adherence; 20% (k = 9) measured virologic suppression. Many eHealth interventions with preliminary or proven efficacy relied on mobile technology and integrated knowledge/cognition as behavior change mechanisms. This review identified gaps in development and application of eHealth interventions regarding CoC.
Keywords: eHealth, Continuum of Care, HIV care, Interventions, Technology
Introduction
Approximately 36.7 million persons worldwide are living with HIV, including 2.1 million people who were newly infected in 2015 [1]. An estimated 1.2 million persons aged 13 and older were living with HIV infection (PLWH) in the United States at the end of 2012, including 156,300 (12.8%) persons whose infections were undiagnosed [2]. A primary goal for HIV prevention is improving the health of PLWH as outlined in the National HIV prevention goals [3]. This goal is important not only for PLWH but also for the health of their partners. One study demonstrated that the risk of HIV transmission was reduced by ≥ 93% when a PLWH had an undetectable viral load (< 50 RNA copies/ml) [4]. Health outcomes for PLWH must be improved, including: (a) diagnosing all persons who are living with HIV; (b) linking all previously undiagnosed PLWH to care (linkage); (c) retaining all linked PLWH in care (retention); (d) re-engaging those PLWH who have fallen out of care (re-engagement); (e) and achieving viral suppression (< 200 RNA copies/ml) via medication adherence [4]. This sequence of steps is known as the Continuum of HIV Care (CoC).
PLWH face many challenges to staying in care and maintaining a suppressed viral load [5]. Addressing these challenges through more intensive care strategies such as case management and patient navigation services (e.g., coordinating transportation, accompanying to medical appointments, etc.) has been prioritized on a national scale [6]. However, these strategies can often be costly, and resources for scaling up these types of strategies may be limited [7].
One way to keep costs low and deliver timely health information to consumers, including PLWH, may be through electronic health (eHealth) technology [8], such as video interventions being shown in medical waiting rooms [9]. eHealth can be a key tool for addressing HIV-related public health challenges in various capacities including disease surveillance, health care access, health education, and health care provider training [10]. Individuals are increasingly using the internet to access health information, and mobile technology (mHealth), such as delivering risk reduction messages to personal cell phones, is rapidly becoming the primary means of broadband access and health information [11]. Therefore, eHealth approaches, including those that involve mHealth, have been shown to help expand the dissemination of HIV prevention and treatment interventions [12], particularly for more resource-challenged adults. Despite eHealth’s demonstrated effectiveness, its broad application, rapid innovation, and reporting heterogeneity make it difficult to evaluate for HIV prevention purposes [13]. Thus, research on interventions that can be scaled up to reach a large number of PLWH can inform how eHealth technology can be used as an additional HIV prevention tool. We sought to examine the landscape and efficacy of using technology to support outcomes related to steps (b) through (e) in the CoC.
Identification of specific eHealth intervention components responsible for the observed HIV-related outcomes among PLWH participants remains unaddressed in the literature. Analyses would provide insight into which eHealth approaches are effective and what specific components are necessary to increase the likelihood of obtaining favorable outcomes related to the CoC. To address this issue, we conducted a rapid qualitative systematic review to synthesize (a) what types of technologies are being used in eHealth interventions for PLWH, (b) specific health outcomes related to HIV care that are addressed in eHealth interventions, (c) the theoretical basis driving the interventions’ designs, and (d) the mechanisms of change used to achieve favorable behavioral change consistent with the CoC and the national HIV prevention goals. We also will discuss major gaps in the research literature, as well as recommendations for future efforts in the field.
Methods
We conducted a rapid review of eHealth interventions that address CoC outcomes, following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14, 15]. A rapid review uses systematic search strategies but limits particular aspects of the systematic review process to provide a time-sensitive assessment of the quantities of studies in the literature and overall quality/direction of effect [16]. In our review, we omitted formal quality assessment of included studies since our synthesis was primarily narrative and conceptual and did not use any meta-analytic methods to combine studies for effect estimates. Our decision to use a single comprehensive database for our search, as described below, allowed us to forgo de-duplication efforts and still maintain a systematic search strategy. Given the rapid innovation of electronic technology and the changing nature of eHealth interventions, we felt this methodology was the most appropriate for timely dissemination in a swift-moving research area.
Literature Search Strategy
We searched the CDC Prevention Research Synthesis (PRS) project’s cumulative database of HIV/AIDS behavioral prevention research literature for this review. We chose this database because, among other HIV/AIDS behavioral prevention topics, it provides access to a cumulative list of citations on interventions to improve HIV care outcomes from an annual systematic search of the literature. The PRS database is comprised of published literature located through four comprehensive annual automated and quarterly manual searches developed by two staff librarians with expertise in developing and implementing comprehensive literature search strategies [17]. The four comprehensive searches focus on (a) behavioral risk reduction interventions (RR), (b) medication adherence interventions (MA), (c) linkage to, retention in, and re-engagement in HIV medical care interventions (LRC), and (d) HIV prevention related systematic reviews (Overview of Reviews Project-ORP). Automated searching involves developing the search strategy and running it at specified intervals (in this case annually) to find the newest publications that meet the search criteria. All four automated searches are implemented in the databases (platforms): MEDLINE (OVID), EMBASE (OVID), and PsycINFO (OVID). The four searches also include at least one of these databases (platforms) depending on what is appropriate for the subject matter of the search (a–d): CAB Global Health (OVID), CINAHL (EBSCOhost), and Sociological Abstracts (ProQuest).
Each of the automated searches (RR, MA, LRC and ORP) were developed in MEDLINE with indexing and keyword terms cross-referenced using Boolean logic. The finalized MEDLINE search was translated to the other databases to fit the proprietary indexing classification of each database. The four searches as implemented in MEDLINE (OVID), with search restrictions applied, are available in the Online Appendix I (other searches available from the corresponding author). The PRS database coverage is from 1988 to the present for two of the automated searches (RR, ORP), and 1996 to the present for the other two searches (MA, LRC). To cover publication lag, the PRS database is updated annually with the automated searches for the two previous years, and with ongoing manual searches including contacts in the field, reference list check, journal alerts, and a quarterly hand search of journals with a high yield of subject-specific citations (http://www.cdc.gov/hiv/dhap/prb/prs Accessed August 31, 2016). Articles from the four automated searches as well as the hand searches are de-duplicated and uploaded to the database so it is a comprehensive database of HIV prevention research literature, including interventions for medication adherence, linkage to, retention in, and re-engagement in care.
PRS staff code all citations added to the database to organize them based on subject matter according to a detailed coding scheme. After ensuring that the definitions in the PRS coding scheme matched those used in this review, we searched the PRS database for reports coded as interventions for PLWH that reported HIV care outcomes (i.e., medication adherence, linkage, retention, and re-engagement in care). The previous identification of interventions with HIV care outcomes was another time saving benefit to using this database. For this review, included reports were limited to citations with eHealth terms: cell phone, computer, eHealth, internet, mHealth, mobile phone, reminder system, smart-phone, social network, tablet, technology, text message, web, app, application, and text (plurals of words were included where appropriate) in the title, abstract, or keywords, published 2007–present (see Online Appendix I). This specific query of the PRS database was last performed in April 2017.
Pairs of trained coders screened citations to determine if inclusion criteria were met. Screening was performed at two levels: (a) title and abstract level, and if inclusion criteria were met, then (b) full report. Inclusion criteria were (a) published January 2007–April 2017 (we selected 2007 as the start date for our search to be consistent with the year that the modern day smartphones first appeared in the US market); (b) used technology to deliver all or part of the intervention; and (c) an intervention focused on linkage to care, retention in care, re-engagement of those lost to care, adherence to antiretroviral therapy (ART), and/or outcomes related to virologic suppression. If the tested technology was not interactive and accessible to anyone at any place and at any time, the study was excluded. Furthermore, studies were excluded from the review if eHealth technology were primarily used to enhance data collection. Citations reporting interventions that used technology to enhance health care service systems or provider practices were also excluded.
Data Abstraction
Pairs of trained coders independently abstracted information from eligible studies. Linkages among studies were identified to ensure that multiple citations describing a single intervention study were not included in the coding, data abstraction, and analyses.
Coders used standardized coding forms, which had been piloted, to guide data abstraction. Each included study was coded for technology used, recruitment settings/methods, study characteristics (location, recruitment/study dates), and study participant characteristics (targeting criteria, sex, age, race/ethnicity). Types of technology devices coded in our data abstraction included short message service (SMS), mobile phone (non-SMS use), computer/laptop, video, electronic alert system, personal digital assistant (PDA), electronic pager, and automated telephone system. For race/ethnicity, “people of color” was a racial/ethnicity category used for non-US studies, broadly defined as persons of ‘non-white’ race/ethnicity. Each study was also coded for intervention content and characteristics including main focus; theoretical basis; intervention setting; mechanism of change; and whether content incorporated knowledge, motivation, intention, attitudes, norms, self-efficacy, social support, skills-building, risk awareness, structural influences, expectancies, personal goal setting, perceived risk, emotions, barriers/facilitators, sexual or drug triggers, ethnic pride, risk reduction supplies/provisions, and any other intervention components (Table 1).
Table 1.
Study and participant characteristics of eHealth interventions addressing critical points of Continuum of HIV Care, 2007–2017 (ordered alphabetically by author and publication date)
| Author; study location | Sample size; sex; target population | Race and ethnicity | Recruitment setting | Intervention focus; theory; mechanism of change | Intervention content; delivery technology | Research design; findings |
|---|---|---|---|---|---|---|
| Ammassari et al. [62]; Italy | N = 145; male 73%; PLWH who are in care, PLWH who are treatment non-adherent | NR | Health care setting | Medication adherence, virologic suppression; theory: NR; emotional well-being | Reminders; mobile phone with timed reminders | Pre-post design; timed SMS associated with significant increases in self-reported adherence and rates of virological suppression |
| Bigna et al. [47]; Cameroon | N = 242 parent-child pairs; female (adults) 80%, Male (child) 52%; PLWH (parents), youth | NR | Health care setting | Care retention; theory: NR; knowledge | Reminders; cell phone text and call | RCT; all active intervention arms significantly improved care retention compared to control group |
| Brock et al. [63]; country: NR | N = 51; male 51%; adult clinic patients, PLWH who are treatment-experienced | African American ≥ 50% | Health clinic, Hospital | Medication adherence; theory: NR; cognition, knowledge | Self-efficacy, knowledge; video on PDA | Pre-post design; preliminary evidence of improvement in self-reported medication adherence |
| Chang et al. [52]; Uganda | N = 29; Female 67%; PLWH clinic patients, Rural areas | NR | Clinics, Other locations | Medication adherence; theory: NR; emotional well-being | Social support, clinical adherence monitoring, referral, transportation; cell phones | RCT; no significant differences in patients’ risk of virologic failure. Qualitative analyses found improvements in patient care and logistics and broad support for the mHealth intervention among patients, clinic staff, and PHWs. |
| Chung et al. [37]; Kenya | N = 310; female 66%; PLWH newly diagnosed, Clinic patients, HIV treatment naïve | NR | Health clinic | Medication adherence; cognitive and behavioral theories; access, cognition, knowledge | Knowledge, Motivation, barriers and facilitators to performing target behavior; alarm device pill reminder | RCT; no significant impact of using alarm device pill reminder on medication adherence |
| Claborn, et al. [76]; United States | N = 97; male 83%; PLWH who are treatment non-adherent | White 60% | NR | Medication adherence; theory: NR; cognition, knowledge, skills building | Knowledge, self-efficacy, adherence, skills in problem-solving, coping, pill taking, medication, structural influences, transportation, personal goal setting, barriers and facilitators to performing target behavior; computer-based technology | RCT; non-significant statistical differences in adherence between intervention and control group |
| Cook et al. [42]; United States | N = 37; gender: male 78%; PLWH clinic patients who are treatment-experienced | Non-white 51% | Primary HIV care clinic | Medication adherence; theory: model of momentary states; mechanism: cognition, emotional well-being | Knowledge, motivation, attitudes, social support, positive/negative expectancies, emotions, barriers/facilitators to target behaviors, coping; mobile device-SMS text messaging | RCT; no statistically significant difference in improving ART adherence between intervention and control groups |
| Cote et al. [55]; Canada | N = 179; gender: male 85%; PLWH clinic patients who are treatment-experienced | NR | Health care: hospitals | Medication adherence; theory: social learning, attitude change theory; mechanism: cognition, emotional well-being, skills building | Social support, problem solving skills, self-assessment skills, motivational skills building, emotions; computer-delivered | Non-RCT; intervention show preliminary evidence of efficacy for improving ART adherence |
| da Costa et al. [44]; Brazil | N = 21; female 100%; female PLWH who are treatment experienced | People of colora 81% | Maternity clinic | Medication adherence; theory: NR; cognition | Text messages; SMS reminders | RCT; no statistically significant difference in adherence between intervention group (SMS reminders) and control group (no reminders) |
| Davey et al. [20]; Mozambique | N = 830; gender: male 40%, female 60%; PLWH clinic patients who are treatment-experienced | NR | Government run health centers | Medication adherence, care retention; theory: NR; mechanism: access, emotional well-being, knowledge | Knowledge, appointment and medication reminders; SMS text messaging | RCT; intervention shows evidence of improving ART adherence among urban patients. Intervention shows evidence of improving retention in care among patients newly initiated on ART |
| Downshen et al [48]; United States | N = 25; male 92%; PLWH youth and young adults who are treatment non-adherent | African American 60% | Community-based health clinic | Medication adherence, virologic suppression; theory: NR; knowledge | Personalized text messages; SMS (personalized messages) | Pre-post design; there was no significant difference in CD4 cell count or viral load between baseline and (12 and 24 month) follow-up assessments |
| Fisher et al. [32]; United States | N = 922; male 61%; PLWH clinic patients | African American 44%, Hispanic/Latino 25% | HIV clinic | Medication adherence; IMB theory; cognition, emotional well-being, knowledge, skills building | Knowledge, barriers and facilitators to performing target behavior; computer-based tool | RCT; Computer-based intervention group showed higher adherence efficiency compared to control group |
| Garofalo et al. [34]; United States | N = 105; gender: male 82%, female 17%, transgender 1%; PLWH clinic patients who are treatment-experienced and treatment non-adherent, low-income, living in rural setting | African American 65% | Community-based health centers; other unspecified organizations | Medication adherence; theory: social cognitive theory; mechanism: knowledge, cognition, emotional well-being | Knowledge, motivation, self-efficacy: medication self-regulation, positive/negative expectancies, medication reminders; mobile phone | RCT; intervention shows evidence of improving ART adherence at 3 months, but not at 6 months |
| Haberer et al. [43]; United States | N = 52; male 75%; PLWH clinic patients in urban areas/inner cities who are treatment-experienced | African American 40%, white 42% | Community social services agency | Medication adherence; theory: NR; cognition | Medication reminder and messages; electronic pill reminder | Pre-post design; acceptability of Med-eMonitor was determined. HIV RNA significantly correlated with unannounced pill counts (r = −0.34, p = 0.02), and trended toward a significant correlation with unadjusted Med-eMonitor adherence (r = −0.26; p = 0.07). Most, but not all, participants liked using the Med-eMonitor. Med-eMonitor allows for real-time adherence monitoring and potentially intervention |
| Hailey et al. [19]; United States | N = 87; male 80%; PLWH clinic patients. youth and young adults. PLWH who are treatment non-adherent | African American 90% | HIV clinic | Medication adherence and care retention; theory: NR; cognition, knowledge, emotional well-being | Knowledge, skills in adherence, emotions, barriers and facilitators to performing target behavior, medication reminders, directly observed mental health counseling; mobile phone, In-person counseling | Non-RCT; technology use associated with increased medication adherence and retention in care |
| Hardy et al. [53]; United States | N = 19; male 53%; PLWH clinic patients. Females. People of color. PLWH who are treatment-experienced. PLWH who are treatment non-adherent | People of colora 63% | HIV clinic | Medication adherence; theory: NR; access, cognition | Motivation, barriers and facilitators to performing target behavior, SMS reply, text messages, pre-paid mobile phone; SMS (personalized messages) with two-way interaction | RCT; intervention group receiving personalized cell phone reminders showed increased adherence and remained significantly higher than control group |
| Henry et al. [31]; United States | N = 584; gender: NR; PLWH clinic patients, mentally ill, persons with STD diagnosis, military, substance user, homeless | African Americans 33% | Medical appointment data | Care retention; behavioral model of health services utilization; structural change, policy | Additional automated telephone reminder; automated telephone reminder | Non-RCT; patients who were not homeless, who were not diagnosed with depression, and who had five or more appointments scheduled in 6 months had significantly fewer no-shows after intervention. The intervention was not effective in reducing no-shows among homeless patients, racial/ethnic minorities, and patients with mental health disorders |
| Hersch et al. [39]; country: NR | N = 168; male 73%, transgender 6%; PLWH clinic patients who live in urban/inner cities. PLWH who are treatment non-adherent | African American 84% | HIV clinic | Medication adherence; theory: cognitive behavioral therapy; cognition, emotional well-being, skills building | Knowledge, skills in problem solving, goal setting, coping, and communication, emotions, barriers and facilitators to performing target behavior, sexual and drug triggers; computer/internet | RCT; intervention associated with increased medication adherence |
| Herwehe et al. [21]; United States | N = 345; male 62%; PLWH who are lost to care | African American 72% | Health care | Linkage to care, Re-engagement in care; theory: NR; access, knowledge | Out of care alerts; electronic technology (out of care alerts) | Pre–post design; preliminary analyses show that the alert system was associated with increased linkage and retention in care among clients |
| Ingersoll et al. [24]; United States | N = 63; gender: male 60%, female 36%, transgender 3%; PLWH clinic patients who are treatment-experienced and treatment non-adherent, low-income, living in rural setting | African American 65% | Primary HIV care clinics | Medication adherence; theory: IMB, social action; mechanism: cognition, emotional well-being, skills building | Emotions, sexual and drug triggers, queries about taking drug medication; mobile device-SMS text messaging | RCT; intervention shows evidence of improving ART adherence |
| Kalichman et al. [35]; United States | N = 600; gender: male 76%, female 36%, transgender 9%; PLWH clinic patients who are treatment non-adherent | African American 96% | Health care, community/social service agency | Medication adherence; theory: self-regulation theory; mechanism: knowledge, access | Knowledge, personal goal setting, barriers/facilitators to performing target behavior, reminders; mobile device-automated SMS text messaging system | RCT; intervention shows evidence of improving ART adherence |
| Kalichman et al. [33]; United States | N = 40; male 65%, transgender 10%; PLWH who are treatment-experienced and treatment non-adherent | African American 95% | Disease clinic | Medication adherence; I-self regulation model of medication adherence; access, cognition, emotional well-being, knowledge, skills-building | Knowledge, self-regulation of medication, mediation management skills, barriers and facilitators to performing target behavior, pill counts; cell phone (counseling over the phone and in-person) | RCT; self-regulation counseling via cell phone showed significant improvements in adherence compared to control group |
| Kurth et al. [25]; United States | N = 433; male 69%, female 26%, transgender 4%; Hispanic/Latino PLWH clinic patients who are treatment-experienced | Hispanic/Latino 97% | HIV clinic | Medication adherence, virologic suppression; theory: information-motivation behavior, social cognitive role modeling, motivational interviewing; mechanism: cognition, skills building | Knowledge, motivation, skills building, risk assessment and planning, personal goal setting, perceived risk, sexual/drug risk triggers, ethnic pride; computer | RCT; no statistically significant difference in adherence, viral load, or sexual transmission risk behaviors over time between intervention group and control group |
| Kurth et al. [29]; United States | N = 239; male 91%; PLWH clinic patients who are treatment-experienced | African American 25%, American Indian 10%, Hispanic/Latino 7%, White 46% | Community social service agency, E-Health, public HIV clinic | Medication adherence, virologic suppression; information-motivation-behavioral skills model, transtheoretical model, motivational interviewing; cognition, skills building | Motivation, skills–use of risk reduction supplies, communication, and. ART adherence, risk awareness plan, positive/negative expectancies, personal goal setting. Perceived risk, emotions, barriers and facilitators to performing target behavior, sexual and drug risk triggers; computer-based | RCT; intervention group had reduced viral load, significant difference in ART adherence and decreased sexual transmission risk behaviors compared to control group |
| Leider et al. [45]; United States | N = 24,495; male 70%; clinic patients in urban/inner city areas | African American 51% | Hospital emergency department | Linkage to care; theory: NR; access, knowledge | Knowledge; video at pre-and post-HIV test | Pre–post design; a total of 83.6% (97/116) of PLWH were linked into specialized care. Findings suggest that a multimedia testing model that includes a counselor who acts as tester and navigator can successfully link a high percentage of patients into specialized care |
| Lester et al. [51]; Kenya | N = 538; female 65%; PLWH clinic patients who are treatment-naïve, rural, low income | NR | HIV clinic | Medication adherence, virologic suppression; theory: NR; access, emotional well-being | Social support; SMS (interactive) | RCT; patients who received SMS support significantly improved ART adherence and rates of viral suppression compared with control group |
| Lewis et al. [59]; United States | N = 52; male 100%; PLWH who are MSM clinic patients in urban settings | African American 33%, Hispanic/Latino 33% | Clinics | Medication adherence; theory: NR; cognition, emotional well-being, knowledge | Motivation, social support, tailored reminder messages; mobile device (SMS messages) | Pre–post design; self-reported medication adherence significantly improved among participants who began the study as non-adherent and received tailored medication reminders |
| Mbuagbaw et al. [64]; Cameroon | N = 200; female 79%; adult PLWH clinic patients who are treatment experienced | NR | Hospitals | Medication adherence; theory: NR; cognition, reminders | Reminders; SMS (standardized) | RCT; standardized motivational mobile phone text messages did not significantly improve adherence to ART in this study |
| Maduka et al. [60]; Nigeria | N = 104; female 57%; target population: NR | NR | Hospital | Medication adherence, virologic suppression; theory: NR; mechanism: NR | Reminders; SMS (Standardized and monthly face-to-face counseling) | RCT; intervention group achieved statistically significantly higher adherence and CD4 count compared with control group |
| Moore et al. [38]; country: NR | N = 50; male 92%; target population: NR | NR | NR | Medication adherence; theory of planned behavior; mechanism: NR | Knowledge, motivation, intention, coping skills, personalized text reminders: SMS (interactive) | RCT; intervention group had significantly improved dose timing of ART medication compared to control group |
| Naar-King et al. [30]; United States | N = 76; male 80%; PLWH clinic patients who are treatment-naïve youth or young adults | African American 71% | Hospitals | Medication adherence, virologic suppression; motivational interviewing; cognition, emotional well-being, knowledge | Knowledge, motivation, goal setting, barriers and facilitators to performing target behavior, personalized feedback; web-based computer | RCT; effect sizes suggested that the intervention group showed greater drop in viral load from baseline to 6 months compared to control group |
| Nsagha et al. [50]; Cameroon | N = 90; male 39%, female 61%; PLWH clinic patients who are treatment-experienced | NR | Hospital HIV clinic | Medication adherence; theory: NR; mechanism: knowledge | Knowledge, medication reminders; SMS text messaging | RCT; intervention shows evidence of improving ART adherence |
| Orrell et al. [77]; South Africa | N = 230; gender: female 65%; PLWH clinic patients who are treatment-naive | NR | ART outpatient clinic | Medication adherence; theory: NR; mechanism: NR | Positive/negative expectancies, barriers/facilitators to medication adherence reminders; mobile device-SMS text messaging | RCT; no statistically significant difference in improving ART adherence between intervention and control groups |
| Ownby et al. [41]; United States | N = 109; male 71%; PLWH in care | African American 63% | Health care setting | Medication adherence; information-motivation-behavioral skills model; cognition, emotional well-being, knowledge, skills building | Knowledge, medication adherence skills, barriers and facilitators to performing target behavior; computer | Pre–post design; no statistically significant changes in adherence |
| Perera et al. [61]; New Zealand | N = 28; male 93%; PLWH clinic patients who are treatment experience | NR | Community social service agency, hospital | Medication adherence, virologic suppression; theory: NR; knowledge, cognition | Graphical representations of medication levels in body. Pictorial representations of CD4 count and viral load. 24-hour medication clock; smartphone app | RCT; intervention group showed a significantly higher level of self-reported adherence to ART and decreased viral load (p = 0.023) as compared to comparison group |
| Perron et al. [46]; Switzerland | N = 2130; male 57%; PLWH clinic patients in care in urban setting, Refugees and immigrants | NR | HIV clinic in a hospital | Care retention; theory: NR; knowledge | Appointment reminders; mobile device (SMS messages) | RCT; use of electronic appointment reminders significantly reduced the rate of missed appointments compared to control group |
| Pop-Eleches et al. [58]; Kenya | N = 428; female 69%; PLWH clinic patients in rural areas who are treatment-experienced | NR | Rural clinic | Medication adherence; theory: NR; cognition, emotional well-being, knowledge | Social support, barriers and facilitators to performing target behavior, paid mobile phones, SMS messages; cell phone and SMS messages | RCT; SMS messaging group achieved higher rates of adherence and lowers rates of adherence interruptions compared to control group |
| Rana et al. [22]; United States | N = 32; gender: male 69%; PLWH clinic patients who are in care, newly-diagnosed, treatment non-adherent | White 66% | Primary HIV care clinics | Care retention, virologic suppression; theory: NR; mechanism: access, cognition | Barriers/facilitators to performing target behavior, appointment reminders, medication adherence reminders; mobile device-SMS text messaging | Non-RCT (Pre/post-test); intervention shows preliminary efficacy in improving care retention and virologic suppression |
| Robbins et al. [56]; South Africa | N = 65; gender: female 66%; PLWH clinic patients who are treatment-experienced and treatment non-adherent | NR | Health clinic | Medication adherence; theory: social action; mechanism: knowledge, cognition, emotional well-being, skills building | Knowledge, adherence self-efficacy, social support, skills: problem-solving adherence, positive/negative expectancies, other mental health and substance abuse counseling at counselor’s discretion; computer-based program | RCT; intervention shows preliminary efficacy in improving medication adherence |
| Robbins et al. [65]; United States | N = 1011; male 79%; PLWH clinic patients in care, Service providers | White 54% | HIV clinic | Care retention, virologic suppression; theory: NR; capacity building, social or organizational structure | Electronic alert system; computer alerts | RCT; intervention group using interactive provider alerts showed significantly improved CD4 cell counts and clinic follow-up compared to control group |
| Sabin et al. [78] China | N = 116; gender: males 64%; PLWH who are treatment-naïve, treatment-experienced | NR | Health care: ART clinic | Medication adherence; theory: NR; mechanism: cognition, emotional well-being, reminders | Social support, medication reminders, adherence counselors; mobile phones-SMS text reminders | RCT; intervention shows efficacy for improving ART adherence |
| Schwartz et al. [26]; South Africa | N = 100; gender: female 100%; PLWH clinic patients who are pregnant | NR | Primary care clinic | Care retention; theory: IMB; mechanism: access, cognition, knowledge | Knowledge, motivation, appointment reminders, pregnancy and health information; mobile phones | Non-RCT (1-group); intervention shows preliminary evidence for improving care retention |
| Shet et al. [36]; India | N = 631; male 57%; target population: NR | NR | NR | Medication adherence; theory of planned behavior; mechanism: NR | Motivation, medication reminder; SMS and automated telephone calls | RCT; no statistically significant difference in adherence or viral load between intervention group and control group |
| Simoni et al. [54]; United States | N = 224; male 76%; PLWH clinic patients who are treatment naïve, patients that switch/restart treatment | African American 30%, White 47% | HIV clinic | Medication adherence; theory: NR; access, cognition, emotional well-being, knowledge | Knowledge, social support, problem-solving skills, barriers and facilitators to performing target behavior; pager | RCT; pager intervention not associated with greater adherence but was associated with improved biological outcomes |
| Thurston et al. [40]; country: NR | N = 2; gender: NR; PLWH clinic patients who are treatment-naïve youth or young adults | NR | Health care setting | Medication adherence; theory: motivational interviewing, cognitive behavioral technique; mechanism: NR | Knowledge, attitudes, social support, skills— problem solving, goal setting, coping, communication, personal goal setting, perceived risk, emotions, barriers and facilitators to performing target behaviors, adherence reminders; mobile phones | Non-RCT (case study); intervention shows preliminary evidence of efficacy to improve adherence |
ART antiretroviral therapy, MSM men who have sex with men, NR not reported, PDA personal digital assistant, PHW public health worker, PLWH persons living with HIV infection, RCT randomized controlled trial, SMS short message service, STD sexually transmitted disease
“People of color”: used to broadly describe persons of non-white race/ethnicity (non-US studies only)
The mechanism of change is the means or the way an intervention component would assist participants in making the desired behavioral change. The eHealth interventions included in this review employed one or more of these mechanisms to help persons to link to, retain in, or reengage in care; or adhere to ART, all in effort to ultimately be virally suppressed. For this review, we classified the mechanisms of change used in these eHealth interventions under several categories that help identify the elements that are essential for achieving desired HIV-care related behaviors. Cognition is a mechanism used to directly change individual attitudes or beliefs using the mental process of acquiring understanding. Knowledge is defined as a mechanism designed to change an individuals’ understanding by providing facts and information about HIV. Emotional well-being is a mechanism used to change behavior by modifying an individual’s mental state, mood, emotions, or feelings. Access is designed to achieve desired HIV-related behavioral change by increasing the availability of consumer products or availability/accessibility of health or social services. Lastly, skills building is a change mechanism that attempts to improve a person’s skills by modeling, teaching, demonstrating or practicing skills related to reducing risk for HIV acquisition or transmission.
We also coded intervention delivery characteristics including unit of delivery, deliverer, and delivery methods. Intervention and comparison group characteristics were also coded including duration, number of sessions, total time, and incentives/payment. Lastly, we coded study methodology quality including research design, evaluation outcome data reported, and sample size.
Data Analysis
We conducted qualitative analysis for this review. Therefore, we did not conduct any statistical analyses commonly used in other types of systematic reviews to combine effect sizes (i.e., meta-analysis). We calculated the proportion of studies that had different characteristics to illustrate the frequency with which these occurred among the total number of included studies. In keeping with a qualitative analysis, the proportions were intended to be descriptive, not contribute to a quantitative assessment of the studies. Reflecting the emphasis of rapid review methodology, our analyses do not include assessing the quality of the included studies. In lieu of such an assessment, we identified the studies as having either proven or preliminary evidence of efficacy. Proven efficacy was defined as studies that reported an intervention effect (based on statistical significance) using randomized controlled trial (RCT) research design, which is generally considered the standard for determining efficacy [18]. Preliminary evidence of efficacy was defined as studies that showed intervention impact using a non-RCT research design (e.g., pre–post test).
Results
Characteristics of Included Studies
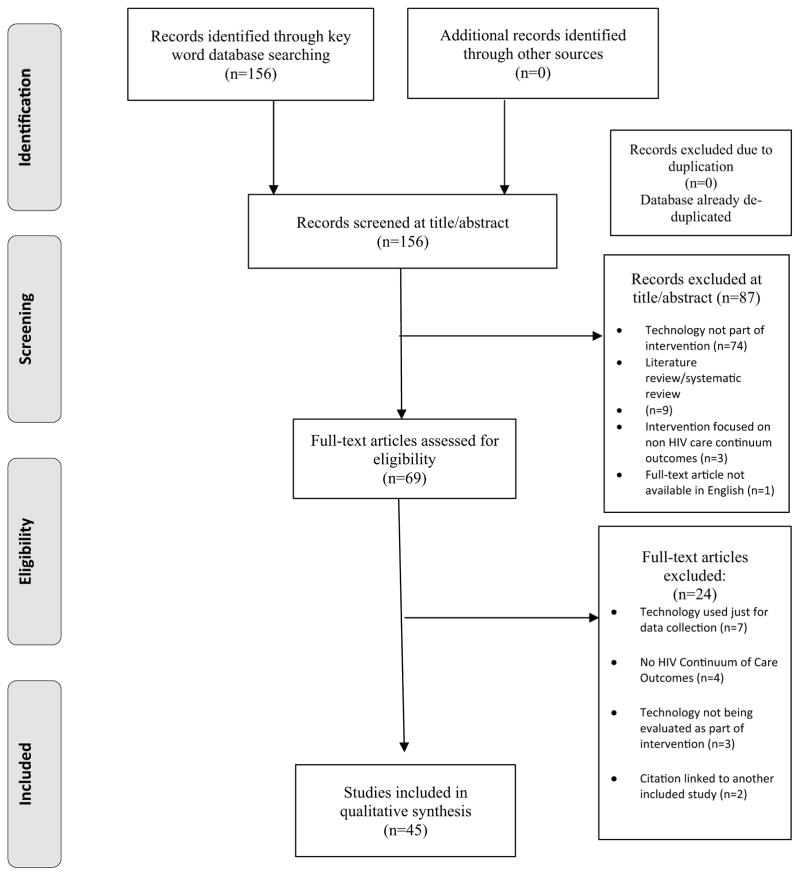
Our initial search query of the PRS Database (Online Appendix 1) yielded 156 citations. Our systematic screening process identified duplicates and excluded citations (k = 111), leaving 45 studies (Fig. 1). The overall coding agreement among the trained coders was 96% with a kappa rate of 80%. Table 2 includes general characteristics of included studies. About two-thirds (k = 30) of studies overall included study samples that were greater than 50% male, and six studies described a sample including transgender persons (data not shown). Eighteen studies reported having samples that were at least 50% racial/ethnic minorities (US-based, k = 17) or “people of color” (non-US based, k = 1). Three studies included samples that were greater than 50% white. Only five studies targeted youth and young adults.
Fig. 1.
PRISMA flow diagram
Table 2.
General characteristics of included studies (k = 45)
| k | % | |
|---|---|---|
| Demographics | ||
| Sample >50% male | 30 | 66.7 |
| Sample >50% people of color | 18 | 40.0 |
| Sample with transgender | 6 | 13.3 |
| Target youth and young adult | 5 | 11.1 |
| Setting | ||
| US based | 22 | 48.9 |
| Non-US based | 19 | 42.2 |
| LRC FOCUS | ||
| Linkage | 1 | 2.2 |
| Retention | 4 | 8.9 |
| ART adherence | 27 | 60.0 |
| Retention and ART adherence | 2 | 4.4 |
| Linkage and re-engagement | 1 | 2.2 |
| ART adherence and virologic suppression | 8 | 17.8 |
| Retention and virologic suppression | 2 | 4.4 |
| Mechanism of change | ||
| Cognition | 27 | 60.0 |
| Knowledge | 23 | 51.1 |
| Emotional well-being | 19 | 42.2 |
| Access | 11 | 24.4 |
| Skills building | 10 | 22.2 |
| Theory-based | 19 | 42.2 |
| Technology | ||
| SMS/mobile phone | 20 | 44.4 |
| Other mobile phone use | 8 | 17.8 |
| Computer | 9 | 20.0 |
| Electronic reminder | 5 | 11.1 |
| Video | 2 | 4.4 |
| Pager | 1 | 2.2 |
| Study design | ||
| RCT | 31 | 68.9 |
| Non-RCT | 14 | 31.1 |
Note Percentages exceed 100% in certain categories due to multiple responses
LRC linkage, retention and care, ART antiretroviral (medication) therapy, SMS short messaging system, RCT randomized controlled trial
Of our 45 included studies, more than half (60%, k = 27) focused on medication adherence. In addition, 17.8% (k = 8) of studies focused on both medication adherence and virologic suppression. Other foci included retention (8.9%, k = 4) and linkage to care (2.2%, k = 1). Two studies (4.4%) focused on both adherence and retention [19, 20], one study (2.2%) focused on both linkage and re-engaging clients back into care outcomes [21], and one study (2.2%) focused on both care retention and virologic suppression [22]. The studies included samples of PLWH experienced with HIV treatment (k = 18), non-adherent to ART (k = 13), or treatment naïve (k = 6). About 75% (k = 34) of studies showed proven or preliminary efficacy at improving the targeted outcome along the CoC.
Setting
Of the included studies in the review, 48.9% (k = 22) were US-based and 42.2% (k = 19) were international-based. Four studies did not explicitly report country setting (Table 2). Approximately 95% (k = 21) of the US-based eHealth interventions included study samples greater than 50% male. In contrast, 63% of the international-based interventions (k = 12) reported study samples that were majority female (with settings all based in African countries). The US-based studies collectively encompassed a broader variation of devices used (e.g., computers, electronic reminders, video) to implement the eHealth technology, while international-based studies reported primarily using conventional mobile phones (k = 15). The US-based eHealth interventions were primarily randomized controlled trails (RCT) (59%, k = 13). In contrast, nearly all (84%, (k = 16) of international-based eHealth studies used RCT designs.
Theory
Among the 45 included studies, 42.2% (k = 19) of the eHealth interventions in our review cited one of several commonly used behavioral theories (Table 2). These cited theories include Information, Motivation and Behavioral (IMB) Skills Model [23–26], Theory of Planned Behavior [27], and Motivational Interviewing [28].
Most of the theory-driven eHealth interventions (k = 19) were efficacious (74%, k = 14) for improving only medication adherence [32, 33, 35, 37, 38]; both medication adherence and virologic suppression [29, 30]; or care retention [26, 31]. Half (k = 7) of these efficacious, theory-based eHealth interventions were US-based [32] [33] [24, 30, 31, 34, 35]. Most (k = 11) of these efficacious, theory-based interventions implemented eHealth using electronic devices that were more technologically advanced (e.g., multimedia messaging) instead of or in conjunction with SMS texting. The theoretically-driven international-based interventions (k = 5) primarily used non-interactive (i.e., one-way communication) eHealth technology using either SMS texting [36] or electronic pill reminder alarm device [26, 37]. A few theory-driven interventions (k = 3) did not report the country setting in the report [38] [39, 40]. We located five theory-driven eHealth interventions [25, 36, 37, 41, 42] that showed no evidence for improving any health outcomes related to the CoC.
Mechanisms of Change
Cognition
Approximately 60% (k = 27) of studies included in this review used cognition to change behavior. Most of the interventions (k = 20) using cognition as a mechanism of change were focused on ART adherence for their clients. Other interventions using cognition as a change mechanism focused on both ART adherence and virologic suppression (k = 4); one study [19] focused on both ART adherence and care retention, and one study focused on both care retention and virologic suppression [22]. All of the eHealth interventions using cognition were augmented with another change mechanism except for two studies [i.e., [43, 44] ]. About two-thirds (k = 13) of the studies using cognition showed either preliminary or proven evidence of efficacy for improving HIV medication adherence.
Knowledge
Over half (k = 23) of included studies identified knowledge as a mechanism of change. We discovered that most (56.5%, k = 13) of these studies focused only on improving medication adherence. Only one study [45] focused on linkage to care, three studies [26, 46, 47] focused on care retention, and another six studies [19–21, 30, 47, 48] focused on multiple outcomes related to CoC. All of the eHealth interventions using knowledge also employed other mechanisms of change except for four studies [46, 47, 49, 50].
Over 78% (k = 18) of the studies using knowledge had either preliminary or proven evidence of efficacy for improving HIV medication adherence (k = 9), linkage to care (k = 1), retention in care (k = 3) or multiple outcomes related to CoC (k = 5).
Emotional Well-Being
About 42% of the reviewed studies (k = 19) incorporated emotional well-being as a behavioral change mechanism. The primary outcome for most of these studies (k = 14) was HIV medication adherence. In addition, the majority of these studies (k = 17) incorporated emotional well-being in conjunction with other mechanisms of change behaviors, except for two studies [51] [52] (see Table 2). Most of the studies (k = 10) that included emotional well-being had preliminary or proven evidence of efficacy for improving only HIV medication adherence.
Access
About 24% (k = 11) of included studies used access as a mechanism of change. Most of the studies (k = 5) focused on improving ART adherence; one intervention focused only on linkage to care [45], and one intervention focused on retention in care [26]. Other interventions using access as a change mechanism focused on multiple LRC-related outcomes (k = 4). We discovered that most of the studies that included access as a change mechanism had preliminary or proven evidence of efficacy (k = 9) for improving HIV medication adherence [33, 35, 53]; linking to care after initial HIV diagnosis [21, 45]; care retention [21, 26], and multiple foci [20–22, 51]. Most of the studies using access that reported preliminary or proven evidence of efficacy used devices that involved bi-directional communication between client and provider (meaning that either provider or client can initiate interaction) [33, 51, 53]. The two non-efficacious studies [37, 54] did not use access as a change mechanism nor used devices that facilitated real-time two-way communication exchanges between clients and providers.
Skills Building
About 22% of studies in this review included skills building as a change mechanism (k = 10). Eighty percent of studies with skills building (k = 8) focused on improving HIV medication adherence. Two studies focused both on medication adherence and virologic suppression [25, 29]. These studies also included cognition in conjunction with skills building to improve adherence. The majority of studies using skills building as a mechanism of change (k = 7) showed efficacy in improving LRC-related outcomes (k = 7) [24, 29, 32, 39, 55–57].
Technology Type and Intended Outcomes
Short message service (SMS) texting, primarily via mobile phone accounted for the technology type most commonly reported (44.4%, k = 20). One study [58] described an SMS-based intervention comprised of four specific text messages that increased ART adherence among PLWH living in Kenya. Another study [38] also identified that an individualized SMS texting intervention improved dose timing among PLWH with co-occurring bipolar disorders. An additional study [19] found preliminary evidence of efficacy for a SMS-based intervention improving medication adherence (as well as retention in care) among youth and young adults.
Other studies examined SMS texting as a two-way interactive communication tool between providers and clients to increase HIV medication adherence. For example, one study [53] reported that an eHealth intervention that involved sending SMS text messages (and requiring clients to reply) showed increased HIV ART adherence efficacy compared to using a beeper (with no messaging component) among PLWH recruited from an outpatient clinic in Boston, MA. Another study [59] also described similar results in a pilot study of a two-way text messaging intervention tailored for men who have sex with men (MSM). The study reported that the eHealth intervention showed preliminary evidence of efficacy (based on pre-post design) for improving HIV medication adherence, CD4 count, and overall viral load. Similarly, a Kenya-based study found that a SMS-based intervention that facilitated real-time conversations between health care workers and their clients improved overall adherence to HIV antiretroviral medication [51]. We identified other SMS-based interventions combined with other modalities showing either preliminary or proven evidence of efficacy for improving HIV ART adherence. An additional study reported that SMS text message reminders combined with monthly face-to-face counseling led to improved adherence to HIV medication and CD4 count among the intervention group compared with the control group [60].
The studies included in our review show a reliance on SMS-based technology as opposed to other technologies to improve HIV medication adherence. Most of the efficacious SMS-based interventions (e.g., [38, 51, 53, 59, 60]) have a bidirectional component whether via the electronic device or augmented by other modalities (e.g., face-to-face counseling) that facilitate a more interactive experience between client and provider. We also found few studies (k = 3) that used SMS texting to increase retention of PLWH in HIV care. Other studies [26, 46] reported an SMS-based intervention that used SMS texting to increase retention of PLWH into HIV care by sending appointment reminders. These findings show that the use of electronic appointment reminders significantly reduced the rate of missed appointments compared to control group [26, 46]. Another study [47] found that an SMS-based intervention was efficacious in reminding parents living with HIV to bring their child to the child’s HIV care visit. In addition, Hailey et al. [19] described an SMS-based intervention showing preliminary evidence of efficacy for increasing attendance to care appointments and medication adherence among youth and young adult clients. No SMS-based interventions among our studies addressed linkage to or re-engagement in HIV care.
Other Mobile Phone Use
Aside from SMS text messaging, two studies report on other mobile phone technologies that promote medication adherence. Perera et al. [61] described a smartphone application using personalized health-related imagery to be efficacious in improving ART adherence. For this intervention, the health-related images included (1) a graphic of a 24-hour medication clock; (2) graphical representation of plasma concentration of each medication; and (3) a personalized graphical simulation of immune activity. Clients who received the intervention showed significantly higher levels of self-reported HIV medication adherence and decreased viral load compared to comparison group. In addition to Perera et al. [61], Kalichman et al. [33] described an intervention that combined in-person counseling along with counseling done via cell phone provided by program staff. The findings revealed that self-regulation counseling via cell phone showed significant improvements in adherence compared to the control group. Kalichman et al. [33] included the use of electronic devices to augment the face-to-face interactions between client and provider. Both Perera et al. [61] and Kalichman et al. [33] demonstrated evidence of efficacy for using eHealth applications to improve HIV medication adherence. This analysis included several studies [48, 52, 58, 61–65] not specifically referenced in this section.
Discussion
This qualitative rapid review provides a detailed analysis of how eHealth interventions are used to improve health-related outcomes along the CoC. Overall, we identified a nearly even split between eHealth studies based in US (k = 16) and non-US (k = 12) locations. Our reviewed eHealth studies consist of majority male and racially/ethnically heterogeneous study samples. Therefore, the intended targets have been racially/ethnically diverse, while still primarily focused on males, which is reflective of the overall HIV epidemiologic profile. Medication adherence is the intended outcome for most of the eHealth interventions. Lastly, most of the reviewed eHealth interventions (68.9%) included more than one mechanism of behavior change. This finding shows that technology is being used to improve outcomes along the CoC in multiple ways, even within a single intervention. As such, this may make it difficult to determine which mechanism is the most effective for use in future interventions.
Characteristics of eHealth with Evidence of Efficacy
Our review reveals several characteristics associated with preliminary or proven evidence of efficacy regarding eHealth interventions that address outcomes related to HIV CoC (k = 34). eHealth interventions that facilitate two-way communication between clients and providers appear to improve HIV care outcomes. The ability for clients to be able to interact with a provider using an electronic device, in particular via mobile phones, seems to be an important element to facilitate intended HIV-related health behaviors. We found that these interactions are often facilitated with SMS texting. Some of these interactions are facilitated either solely with SMS texting [38, 47, 51, 53, 59] or augmented with in-person counseling [19, 60]. Based on this finding, eHealth interventions may contribute to enhancing individual-level interactions by reducing the burden of clients using resources related to travel and information access that can impede these interactions.
In addition to bidirectional interactions, our analysis shows that being based in theory may be another key characteristic that contributes to efficacy among these interventions. We found that 74% of the studies designed based on theory improved LRC-related outcomes. Half of these theory-driven eHealth interventions with preliminary or proven evidence of efficacy include skills-building components [29, 32, 33, 38, 39]. Throughout the history of HIV intervention development, many theory-based risk reduction interventions have often been applied to develop skills specific to risk reduction, including recent non-eHealth examples [57, 66]. Our review provides support for the notion that eHealth interventions incorporating theoretical frameworks may be critical to improve health outcomes related to HIV care.
We also discovered that eHealth interventions that used knowledge and cognition as mechanisms of change showed preliminary or proven efficacy. The concepts of knowledge and cognition are fundamental components related to an individual’s attainment and comprehension of new information. In context of the CoC, studies have shown that PLWH with low health literacy are likely to miss HIV-related medical appointments, report a lower CD4 count, and have detectable viral loads [67]. In our review, about 75% of eHealth interventions with preliminary or proven efficacy included knowledge or cognition as a mechanism of change. This finding sheds light on the potential efficiency of using eHealth interventions to disseminate HIV related information to a large, geospatially-dispersed population. Integrating personal HIV-related health information (e.g., biologic data) to encourage HIV ART adherence is an effective strategy for using knowledge and cognition as behavioral change mechanisms to ensure clients stay engaged in care and ultimately achieve viral suppression.
Gaps in Research Literature
We identified several gaps related to research and implementation of eHealth interventions designed to address HIV care. First, we found that only a third of the reviewed eHealth interventions were designed based on major behavioral theories. It is possible that the absence of an explicitly stated theory could be due to reporting omission by eHealth research investigators. However, we purport that the rapid innovation of technology, particularly those that are mobile-based, may partially explain the lack of theory-based eHealth interventions [68]. Rapid changes in technology present new opportunities for designing and delivering interventions to improve HIV care. This rapid innovation of mobile technology may encourage focusing on new delivery mechanisms for eHealth interventions and may move too quickly for behavioral theory to be incorporated when developing the intervention content. While reasons may be unclear, the few number of interventions that explicitly reported theoretical premises makes it challenging to evaluate efficacious components that may be theory-driven. Furthermore, it can further hinder efforts to enhance the eHealth intervention mapping process to increase likelihood of successful intervention adaptation and replication.
Beyond the lack of theory-based eHealth interventions, we also found only one eHealth intervention that employs smartphone apps. There is a heavy reliance on SMS texting in these interventions. While SMS texting is widely available, smartphone use has grown exponentially over recent years [68]. Mobile-based apps designed for smart-phones (such as iPhone and Android-based phones) allow for greater flexibility in designing the end-user interactive experience beyond the rote text messaging involved with SMS texting. Several factors may explain the relatively low number of eHealth interventions based on mobile smartphone apps designed for PLWH. Millions of mobile apps are available in the open marketplace [69]. The rapid development and dissemination of new mobile apps in the general marketplace make it challenging for the slower process of scientific research and evaluation to keep pace. In addition, mobile apps need to be able to run on multiple platforms to be accessible and functional on a wide range of manufacturers’ devices. Although mobile phones are widely available [68], smartphone access is considerably less available in “resource-limited” international settings [70]. Whether in US or non-US settings, eHealth interventions can better leverage SMS-based interventions rather than mobile app-based versions because of the greater accessibility to conventional mobile phones.
Our review also revealed that less than 25% of studies included biological outcomes (i.e. virologic suppression). This finding is somewhat counter-intuitive to the emphasis on biomedical interventions (e.g., ART, pre-exposure prophylaxis) in the HIV prevention and care field [71]. However, a closer look at the chronological trend show that 80% of the eHealth interventions in this review that included biological outcomes were published in the last 5 years (since 2012). Therefore, we suspect that a greater proportion of eHealth interventions will include outcomes measuring virologic suppression to reflect the overall increased emphasis on biomedical interventions in the HIV public health field.
Our findings also reveal the greater need for more eHealth interventions targeting youth. In the US, the HIV incidence rate is high among adolescents and young adults, particularly young African American MSM [72]. Compared to older adults, youth are less likely to know their HIV status, stay in care, and achieve viral suppression [73, 74]. Studies report that technology use among youth in the US is approximately 90% [68]. We identified only five of our reviewed eHealth studies that specifically targeted youth and young adults living with HIV. More eHealth interventions need to be developed in order to take advantage of the high technology use among youth living with HIV to increase their access to HIV care. eHealth interventions might be more attractive to youths and young adults who are engaged in increased risk or PLWH if the interventions were linked to websites associated with high risk behaviors, such as popular dating websites where many youths and young adults seek sexual partnerships. Although not examined as a part of this study, partnering with these websites may help eHealth intervention developers design smartphone apps with appropriate content that effectively helps reduce transmission risk and improve health care outcomes for PLWH that might utilize these websites.
Limitations
There are several limitations for this review. First, the intervention elements identified in this review were limited by what was reported in published articles. We did not seek further documentation from authors regarding interventions (e.g., manuals). Second, we did not conduct an extensive search in the grey literature (e.g., dissertations, conference abstracts, and unpublished reports). Third, while comprehensive in its coverage of the behavioral HIV prevention literature, the literature search designed for the PRS Project (or the PRS database) does not specifically search for studies of technology use, so it is possible that some studies were missed. Lastly, many eHealth interventions contain rapidly evolving technology; there are likely some technology-driven interventions that have not yet been formally evaluated for inclusion in this review.
Conclusion
The evolution of eHealth technology has fundamentally shifted our approach to improving HIV care in the US. With 90% of adults in US owning a cell phone and 64% owning a smartphone [11, 75], the growth and subsequent sophistication of mobile technology have stimulated many innovative strategies for improving HIV care. In our review, we found that the majority of studies showed proven or preliminary efficacy at improving targeted outcomes along the CoC. We have identified several key characteristics that are associated with eHealth interventions that show preliminary or proven evidence of efficacy for improving HIV care-related outcomes, particularly adherence to HIV medication. These key characteristics include (a) having a two-way interactive component between providers and client, (b) designing eHealth interventions based on behavioral theory, and (c) integrating content that facilitates behavior change using knowledge and cognition.
We also identified several gaps in the development and application of eHealth interventions regarding HIV care. Future efforts should include leveraging the perpetually evolving technology to increase the number of persons who are linked to care and achieve viral suppression. In addition, future studies should include cost effectiveness analyses of implementing eHealth technology in the context of deaths averted and medical costs savings. This review can be used as a guide to develop more innovative interventions and scale up of regional efforts to expand use of eHealth technologies for improved HIV care. This work can be facilitated by applying the evidence-based components and strategies identified in this review to design future eHealth interventions that will increase the likelihood of being efficacious in improving CoC related outcomes.
Supplementary Material
Acknowledgments
Funding No external funding was obtained for this study.
We would like to acknowledge the PRS Project of the Prevention Research Branch, Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention for their support.
Footnotes
Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Compliance with Ethical Standards
Conflicts of interest None of the authors declare any conflicts of interest.
Ethical approval This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent Informed consent is not applicable since this study does not involve human participants.
Electronic supplementary material The online version of this article (doi:10.1007/s10461-017-1923-2) contains supplementary material, which is available to authorized users.
References
- 1.World Health Organization. HIV/AIDS: data and statistics. Global summary of AIDS epidemic-2015. 2016 [Google Scholar]
- 2.Hall HI, An Q, Tang T, Song R, Chen M, Green T, et al. Prevalence of diagnosed and undiagnosed HIV infection—United States, 2008–2012. MMWR. 2015;64(24):657–62. [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. National HIV/AIDS strategy: updated to 2020. AIDSgov. 2015 [Google Scholar]
- 4.Department of Health and Human Services. Lab test and results. HIVgov. 2017 [Google Scholar]
- 5.Steele C, Meléndez-Morales L, Campoluci R, DeLuca N, Dean H. Health disparities in HIV/AIDS, viral hepatitis, sexually transmitted diseases, and tuberculosis: issues, burden, and response, a retrospective review, 2000–2004. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 6.Coleman S, Boehmer U, Kanaya F, Grasso C, Tan J, Bradford J. Retention challenges for a community-based HIV primary care clinic and implications for intervention. AIDS Patient Care STDs. 2007;21:691–701. doi: 10.1089/apc.2006.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumaranayake L. The economics of scaling up: cost estimation for HIVAIDS interventions. AIDS. 2008;22:S23–33. doi: 10.1097/01.aids.0000327620.47103.1d. [DOI] [PubMed] [Google Scholar]
- 8.Pew Research Center. Health Online 2013. 2013. [Google Scholar]
- 9.Myint-U A, Bull S, Greenwood G, Patterson J, Rietmeijer C, Vrungos S, et al. Safe in the city: developing an effective video-based intervention for STD clinic waiting rooms. Health Promot Pract. 2010;11(3):408–17. doi: 10.1177/1524839908318830. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Observatory. Geneva: WHO; 2011. WHO global observatory for e-health series—new horizons for health through mobile technologies; p. 3. [Google Scholar]
- 11.Pew Research Center. The Smartphone Difference. 2015 [Google Scholar]
- 12.Young S, Cumberland W, Nianogo R, Menacho L, Galea J, Coates T. The HOPE social media intervention for global prevention in Peru: a cluster randomized controlled trial. Lancet HIV. 2014;2(1):e27–32. doi: 10.1016/S2352-3018(14)00006-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Catalani C, Philbrick W, Fraser H, Mechael P, Israelski D. mHealth for IV treatment & prevention: a systematic review of the literature. Open AIDS J. 2013;7:17–41. doi: 10.2174/1874613620130812003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liberat A, Altman D, Tetzlaff J, Mulrow C, Gotzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman D, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6(7):1–6. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grant M. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inform Libr J. 2009;26:91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 17.Deluca J, Mullins M, Lyles C, Crepaz N, Kay L, Thadiparthi S. Developing a comprehensive search strategy for evidence based systematic reviews. Evid Based Libr Inform Pract. 2008;3:3–32. [Google Scholar]
- 18.Akobeng A. Understanding randomised controlled trials. Arch Dis Child. 2005;90:840–4. doi: 10.1136/adc.2004.058222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hailey J, Arscott J. Using technology to effectively engage adolescents and young adults into care: STAR TRACK adherence program. J Assoc Nurses AIDS Care. 2013;24(6):582–6. doi: 10.1016/j.jana.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 20.Davey D, Nhavoto J, Augusto O, Ponce W, Traca D, Nguimfack A, et al. SMSaude: evaluating mobile phone text reminders to improve retention in HIV care for patients on antiretroviral therapy in Mozambique. J Acquir Immunodefic Syndr. 2016;73:e23–30. doi: 10.1097/QAI.0000000000001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herwehe J, Wilbright W, Abrams A, Bergson S, Foxhood J, Kaiser M, et al. Implementation of an innovative, integrated electronic medical record (EMR) and public health information exchange for HIV/AIDS. J Am Med Inform Assoc. 2012;19:448–52. doi: 10.1136/amiajnl-2011-000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rana A, van den Berg J, Lamy E, Beckwith C. Using a mobile health intervention to support HIV treatment adherence and retention among patients at risk for disengaging with care. AIDS Patient Care STDs. 2016;30:178–84. doi: 10.1089/apc.2016.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher W, Fisher J, Harman J. Social psychological foundations of health and illness. Malden, MA: Blackwell; 2003. The information-motivation-behavioral skills model: a general social psychological approach to understanding and promoting health behavior; pp. 82–106. [Google Scholar]
- 24.Ingersoll K, Dillingham R, Freeman J, Reynolds G, Hosseinbor S. Pilot RCT of bidirectional text messaging for ART adherence among nonurban substance users with HIV. Health Psychol. 2015;34:1305–15. doi: 10.1037/hea0000295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kurth A, Chhun N, Cleland C, Crespo-Fierro M, Pares-Avila J, Lizcano J, et al. Linguistic and cultural adaptation of a computer-based counseling program (CARE+Spanish) to support HIV treatment adherence and risk reduction for people living with HIV/AIDS: a randomized controlled trial. J Med Internet Res. 2016;18:1–15. doi: 10.2196/jmir.5830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schwartz S, Clouse K, Yende N, Van Rie A, Bassett J, Ratshefola M, et al. Acceptability and feasibility of a mobile phone-based case management intervention to retain mothers and infants from an Option B+ program in postpartum HIV care. Matern Child Health J. 2015;19:2029–37. doi: 10.1007/s10995-015-1715-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ajzen I. Action control: from cognition to behavior. New York: Springer; 1985. From intentions to actions: a theory of planned behavior; pp. 11–39. [Google Scholar]
- 28.Miller W, Rollnick S. Motivational interviewing: preparing people for change. New York: Guilford Press; 1991. [Google Scholar]
- 29.Kurth A, Spielberg F, Cleland C, Lambdin B, Bangsberg D, Frick P, et al. Computerized counseling reduces HIV-1 viral load and sexual transmission risk: findings from a randomized controlled trial. JAIDS. 2014;65(5):611–20. doi: 10.1097/QAI.0000000000000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naar-King S, Outlaw A, Sarr M, Parsons J, Belzer M, MacDonell K, et al. Motivational enhancement system for adherence (MESA): pilot randomized trial of a brief computer-delivered prevention intervention for youth initiating antiretroviral treatment. J Pediatr Psychol. 2013;38(6):638–48. doi: 10.1093/jpepsy/jss132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henry S, Goetz M, Asch S. The effect of automated telephone appointment reminders in HIV primary care no-shows by veterans. J Assoc Nurses AIDS Care. 2012;23(5):409–18. doi: 10.1016/j.jana.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 32.Fisher J, Amico K, Fisher W, Cornman D, Shuper P, Traling C, et al. Computer-based intervention in HIV clinical care setting improves antiretroviral adherence: the LifeWindows Project. AIDS Behav. 2011;15:1635–46. doi: 10.1007/s10461-011-9926-x. [DOI] [PubMed] [Google Scholar]
- 33.Kalichman S, Kalichman M, Cherry C, Swetzes C, Amaral C, White D, et al. Brief behavioral self-regulation counseling for HIV treatment adherence delivered by cell phone: an initial test of concept trial. AIDS Patient Care STDs. 2011;25(5):303–10. doi: 10.1089/apc.2010.0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garofalo R, Kuhns L, Hotton A, Johnson A, Muldoon A, Rice D. A randomized controlled trial of personalized text message reminders to promote medication adherence among HIV-positive adolescents and young adults. AIDS Behav. 2016;20:1049–59. doi: 10.1007/s10461-015-1192-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kalichman S, Kalichman M, Cherry C, Eaton L, Cruess D, Schinazi R. Randomized factorial trial of phone-delivered support counseling and daily text message reminders for HIV treatment adherence. J Acquir Immunodefic Syndr. 2016;73:47–54. doi: 10.1097/QAI.0000000000001020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shet A, De Costa A, Kumarasamy N, Rodrigues R, Rewari B, Ashorn P, et al. Effect of mobile telephone reminders on treatment outcome in HIV: evidence from a randomised controlled trial in India. BMJ. 2014;349:g5978. doi: 10.1136/bmj.g5978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chung M, Richardson B, Tapia K, Benki-Nugent S, Kiarie J, Simoni J, et al. A randomized controlled trial comparing the effects of counseling and alarm device on HAART adherence and virolgic outcomes. PLoS Med. 2011;8(3):e1000422. doi: 10.1371/journal.pmed.1000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moore D, Poquette A, Casaletto K, Gouaux B, Montoya J, Posada C, et al. Individualized texting for adherence building (iTAB): improving antiretroviral dose timing among HIV-infected persons with co-occurring bipolar disorder. AIDS Behav. 2015;19:459–71. doi: 10.1007/s10461-014-0971-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hersch R, Cook R, Billings D, Kaplan S, Murray D, Safren S, et al. Test of a web-based program to improve adherence to HIV medications. AIDS Behav. 2013;17:2963–76. doi: 10.1007/s10461-013-0535-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thurston I, Bogart L, Wachman M, Closson E, Skeer M, Mimiaga M. Adaptation of an HIV medication adherence intervention for adolescents and young adults. Cogn Behav Pract. 2014;21:191–205. doi: 10.1016/j.cbpra.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ownby R, Waldrop-Valverde D, Caballero J, Jacobs R. Baseline medication adherence and response to an electronically delivered health literacy intervention targeting adherence. Neurobehav HIV Med. 2012;12(4):113–21. doi: 10.2147/NBHIV.S36549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cook P, Carrington J, Schmiege S, Starr W, Reeder B. A counselor in your pocket: feasibility of mobile health tailored messages to support HIV medication adherence. Patient Prefer Adher. 2015;9:1353–66. doi: 10.2147/PPA.S88222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haberer J, Robbins G, Ybarra M, Monk A, Ragland K, Weiser S, et al. Real-time electronic adherence monitoring is feasible, comparable to unannounced pill counts, and acceptable. AIDS Behav. 2012;16(2):375–82. doi: 10.1007/s10461-011-9933-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DaCosta T, Barbosa B, Costa D, Sigulem D, Marin H, Filho A, et al. Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. Int J Med Inform. 2012;81:257–69. doi: 10.1016/j.ijmedinf.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leider J, Fettig J, Calderon Y. Engaging HIV-positive individuals in specialized care from an urban emergency department. AIDS Patient Care STDs. 2011;25(2):89–93. doi: 10.1089/apc.2010.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Perron N, Dao N, Kossovsky M, Miserez V, Chuard C, Calmy A, et al. Reduction of missed appointments at an urban primary care clinic: a randomised controlled study. BMC Fam Pract. 2010;79:1–8. doi: 10.1186/1471-2296-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bigna J, Noubiap J, Kouanfack C, Plottel C, Koulla-Shiro S. Effect of mobile phone reminders on follow-up medical care of children exposed to or infected with HIV in Cameroon (MORE CARE): a multicentre, single-blind, factorial, randomised controlled trial. Lancet Infect Dis. 2014;14:600–8. doi: 10.1016/S1473-3099(14)70741-8. [DOI] [PubMed] [Google Scholar]
- 48.Downshen N, Kuhns L, Johnson A, Holoyda B, Garofalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: a pilot study using personalized, interactive, daily text message reminders. J Med Int Res. 2012;14:e51. doi: 10.2196/jmir.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dowshen N, Kuhns L, Johnson A, Holoyda B, Garafalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: a pilot study using personalized, interactive, daily text message reminders. J Med Int Res. 2012;14(2):e51. doi: 10.2196/jmir.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nsagha D, Lange I, Fon P, Assob J, Tanue E. A randomized controlled trial on the usefulness of mobile text phone messages to improve the quality of care of HIV and AIDS patients in Cameroon. Open AIDS J. 2016;10:93–103. doi: 10.2174/1874613601610010093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lester R, Ritvo P, Mills E, Kariri A, Karanja S, Chung M, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (Welel Kenya1): a randomised trial. Lancet. 2010;376:1838–45. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- 52.Chang L, Kagaayi J, Arem H, Nakigozi G, Ssempijja V, Quinn T, et al. Impact of a mHealth intervention for peer health workers on AIDS care in rural Uganda: a mixed methods evaluation of a cluster-randomized trial. AIDS Behav. 2011;15:1776–84. doi: 10.1007/s10461-011-9995-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hardy H, Kumar V, Doros G, Farmer E, Drainoni M, Rybin D, et al. Randomized controlled trial of a personalized cellular phone reminder system to enhance adherence to antiretroviral therapy. AIDS Patient Care STDs. 2011;25(3):153–61. doi: 10.1089/apc.2010.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simoni J, Huh D, Frick P, Pearson C, Andrasik M, Dunbar P, et al. Peer support and pager messaging to promote antiretroviral modifying therapy in Seattle: a randomized controlled trial. JAIDS. 2009;52:465–73. doi: 10.1097/qai.0b013e3181b9300c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cote J, Godin G, Ramirez-Garcia P, Rouleau G, Bourbonnais A, Gueheneuc Y, et al. Virtual intervention to support self-management of antiretroviral therapy among people living with HIV. J Med Int Res. 2015;17:1–12. doi: 10.2196/jmir.3264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Robbins R, Mellins C, Leu C, Rowe J, Warne P, Abrams E, et al. Enhancing lay counselor capacity to improve patient outcomes with multimedia technology. AIDS Behav. 2015;19:S163–76. doi: 10.1007/s10461-014-0988-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Essien E, Mgbere O, Monjok E, Ekong E, Holstad M, Kalichman S. Effectiveness of a video-based motivational skills-building HIV risk-reduction intervention for female military personnel. Soc Sci Med. 2011;72(1):63–71. doi: 10.1016/j.socscimed.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pop-Eleches C, Thirumurthy H, Habyarimana J, Zivin J, Goldstein M, de Walque D, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25:825–34. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lewis M, Uhrig J, Bann C, Harris J, Furberg R, Coomes C, et al. Tailored text messaging intervention for HIV adherence: a proof-of-concept study. Health Psychol. 2013;32(3):248–53. doi: 10.1037/a0028109. [DOI] [PubMed] [Google Scholar]
- 60.Maduka O, Tobin-West C. Adherence counseling and reminder text messages improve uptake of antiretroviral therapy in a tertiary hospital in Nigeria. Niger J Clin Pract. 2013;16(3):302–8. doi: 10.4103/1119-3077.113451. [DOI] [PubMed] [Google Scholar]
- 61.Perera A, Thomas M, Moore J, Faasse K, Petrie K. Effect of a smartphone application incorporating personalized health-related imagery on adherence to antiretroviral therapy: a randomized clinical trial. AIDS Patient Care STDs. 2014;28:579–86. doi: 10.1089/apc.2014.0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ammassari A, Trotta M, Shalev N, Tettoni M, Maschi S, Sora F, et al. Timed short messaging service improves adherence and virological outcomes in HIV-1 inflected patients with suboptimal adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2011;58:e113–5. doi: 10.1097/QAI.0b013e3182359d2a. [DOI] [PubMed] [Google Scholar]
- 63.Brock T, Smith S. Using digital videos displayed on personal digital assistants (PDAs) to enhance patient education in clinical settings. Int J Med Inform. 2007;76:829–35. doi: 10.1016/j.ijmedinf.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 64.Mbuagbaw L, Thabane L, Ongolo-Zogo P, Lester R, Mills E, Smieja M, et al. The Cameroon mobile phone SMS (CAMPS) trial: a randomized trial of text messaging versus usual care for adherence to antiretroviral therapy. PLoS ONE. 2012;7:e46909. doi: 10.1371/journal.pone.0046909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Robbins G, Lester W, Johnson K, Chang Y, Estey G, Surrao D, et al. Efficacy of a clinical decision-support system in an HIV practice. Ann Intern Med. 2012;157:757–66. doi: 10.7326/0003-4819-157-11-201212040-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McCabe B, Schaefer S, Gattamorta K, Villegas N, Cianelli R, Mitrani V, et al. Development and psychometric evaluation of a condom use self-efficacy measure in Spanish and English. HIV Clin Trials. 2016;17(5):212–7. doi: 10.1080/15284336.2016.1213487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jones D, Cook R, Rodriguez A, Waldrop-Valverde D. Personal HIV knowledge, appointment adherence and HIV outcomes. AIDS Behav. 2013;17:242–9. doi: 10.1007/s10461-012-0367-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pew Research Center. Cell phone and smartphone ownership demographics. 2014 [Google Scholar]
- 69.Statista Inc. Number of apps available in leading app stores as of June 2016. Statista: The Statistics Portal. 2016 [Google Scholar]
- 70.Pew Research Center. Cell phones in Africa: a communication lifeline. 2015 [Google Scholar]
- 71.Centers for Disease Control and Prevention. Recommendations for HIV prevention with adults and adolescents with HIV in the United States, 2014. Washington, DC: CDC Stacks: Public Health Publication; 2014. [Google Scholar]
- 72.Centers for Disease Control and Prevention. HIV Surveillance Report. 2015 [Google Scholar]
- 73.Idele P, Gillespie A, Porth T, Suzuki C, Mahy M, Kasedde S, et al. Epidemiology of HIV and AIDS among adolescents: current status, inequities, and data gaps. J Acquir Immunodefic Syndr. 2014;66(Suppl 2):S144–53. doi: 10.1097/QAI.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 74.Zanoni B, Mayer K. The adolescent young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care STDs. 2014;28(3):128–35. doi: 10.1089/apc.2013.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.ITU. ICT facts & figures. 2015. [Google Scholar]
- 76.Claborn K, Leffingwell T, Miller M, Meiser E, Stephens J. Pilot study examining the efficacy of an electronic intervention to promote HIV medication adherence. AIDS Care. 2014;26(3):404–9. doi: 10.1080/09540121.2013.824534. [DOI] [PubMed] [Google Scholar]
- 77.Orrell C, Cohen K, Mauff K, Bangsberg D, Maartens G, Wood R. A randomized controlled trial of real-time electronic adherence monitoring with text message dosing reminders in people starting first-line antiretroviral therapy. J Acquir Immunodefic Syndr. 2015;70:495–502. doi: 10.1097/QAI.0000000000000770. [DOI] [PubMed] [Google Scholar]
- 78.Sabin L, DeSilva M, Gill C, Zhong L, Vian T, Xie W, et al. Improving adherence to antiretroviral therapy with triggered real-time text message reminders: the China Adherence through Technology Study. J Acquir Immunodefic Syndr. 2015;69:551–9. doi: 10.1097/QAI.0000000000000651. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.