Abstract
Background
Glucocorticoids (GCs) are considered first line treatment for PDGFRA-negative hypereosinophilic syndromes (HESs). Despite this, little is known about clinical predictors of GC responsiveness in HES.
Objective
Knowledge of clinical and laboratory predictors of GC response prior to initiation of GC could lead to more rational selection of HES subjects for whom earlier institution of second-line and alternative therapies would be appropriate.
Methods
Response to GC, as defined by reduction of the absolute eosinophil count (AEC) to below 1000/mm3 and control of symptoms, was assessed by retrospective chart review of PDGFRA-negative HES subjects evaluated on an IRB-approved protocol. Demographic, clinical and laboratory parameters obtained prior to institution of GC, as well as final diagnosis, were evaluated to determine predictors of GC response. Proportional odds models were used for univariate and multivariate assessment of predictors with permutation adjusted p-values to correct for multiple comparisons.
Results
164 PDGFRA-negative HES subjects were categorized according to GC response. 39% of the subjects responded to low dose (≤ 10mg) prednisone, 9% did not respond to GC, and the remainder (52%) had variable responses to GC. The HES subtype diagnosis was the best predictor of response to GC with myeloid forms and lymphocytic variants of HES being the least responsive to GC.
Conclusion
In a large cohort of well-characterized HES subjects, the odds of response to GC was predicted by HES subtype. Using this model, clinicians may more readily proceed to second-line agents in subjects with confirmed lymphocytic or myeloid forms of HES.
Keywords: Eosinophil, Hypereosinophilic syndrome, Glucocorticoid, Steroid-resistance, Prednisone
Introduction
Hypereosinophilic syndromes (HES) are a rare group of disorders characterized by marked peripheral and/or tissue eosinophilia resulting in clinical signs and symptoms. The clinical manifestations of HES are heterogeneous, and treatment algorithms vary depending on the clinical scenario(1). Prior to the discovery of imatinib, the treatment of choice for platelet-derived growth factor (PDGFR)-associated HES(2), glucocorticoids (GC) were considered first-line therapy for all patients with HES. Despite this, little is known about steroid-responsiveness in different subgroups of HES patients(3), and few studies have explored the mechanisms underlying GC-resistance in HES(4).
The end organ manifestations of HES are extremely varied, ranging from bothersome symptoms, such as urticaria, myalgia and fatigue, to disabling and/or life-threatening manifestations, such as mononeuritis multiplex, endomyocardial fibrosis and stroke. Although the ultimate aim of HES therapy is to prevent these consequences, surrogate markers of disease activity have not been validated to date. That said, most experts use a combination of clinical symptoms and the peripheral blood absolute eosinophil count (AEC) to help guide therapeutic decisions.
Very few studies have evaluated predictors of response to the various medications used to treat HES(5). Consequently, excluding the 10–20% of HES patients with PDGFR-associated disease for whom imatinib is the treatment of choice, therapeutic interventions typically proceed in a stepwise fashion beginning with GCs(1). Second-line GC-sparing agents are added if response to therapy is suboptimal or significant GC toxicity is observed. Since there is little consensus regarding GC dosing in the treatment of HES, the length of time before a second agent is added varies considerably. To begin to address this issue, we sought to identify predictors of response to GC using a well-characterized, consecutively recruited cohort of HES subjects.
Methods
Subject selection
Between 1993 and February 15, 2014, 330 subjects were evaluated on an IRB approved protocol (NCT00001406) to study unexplained eosinophilia. All subjects signed informed consent prior to undergoing a complete evaluation, including medical history, physical examination, routine laboratory testing, EKG, echocardiogram, pulmonary function testing and assessment of other end organ manifestations of eosinophilia as clinically indicated. HES was defined as AEC ≥1.5 × 109/L with signs and symptoms of organ or tissue involvement attributable to the eosinophilia or prominent tissue eosinophilia accompanied by peripheral eosinophilia (AEC greater than the upper limit of normal)(1). HES subjects with a secondary diagnosis known to cause eosinophilia, such as parasitic infection or drug hypersensitivity, and subjects with myeloid neoplasms (MN), including those associated with mutations in PDGFRA, were excluded (Figure 1). The remaining 259 subjects with confirmed HES had their electronic medical records and outside medical records screened for historical use of GC. Because this was a retrospective study, subjects were not treated with a standardized tapering schedule; however, charts were reviewed to identify those subjects treated with corticosteroids as a single agent followed by a taper (lasting from 2 weeks to several months) and for whom laboratory and clinical data were available prior to and during the taper to assess response to therapy (n=164). Subjects initially treated with a starting dose of ≤40mg of prednisone (or equivalent) were included if responsive; however, to classify a subject as a non-responder they had to have received >40mg of prednisone equivalent for ≥1 week without response. Some subjects had their GC dose increased due to rising counts followed by additional attempts to taper; response to GC was defined as the minimum clinically effective dose at which AEC was below 1.0 × 109/L with concomitant improvement of symptoms or manifestations of organ disease after at least one week of treatment on a given dose. Two abstractors (authors PK and AOA), trained to a standard for the definition of clinical response, reviewed the electronic and paper medical records. Daily equivalent prednisone doses were calculated for subjects taking other GC formulations. An average daily dose was calculated for subjects on alternate day dosing.
Figure 1.
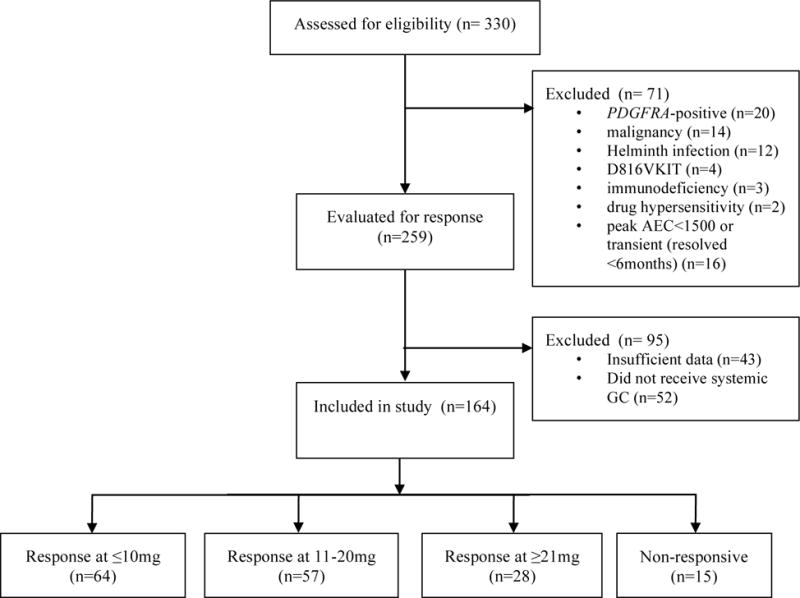
Consort diagram of subjects included in study.
Categorization of response to GC
After abstraction of the data, subjects were grouped according to a priori dose-response categories based on the usual practice of practitioners taking care of these subjects. Subjects were considered to have a response to low-dose prednisone if they could be controlled on ≤10mg of prednisone (Group 1). These subjects were not typically treated with second-line agents, unless required due to GC comorbidities. Subjects whose eosinophil counts, disease manifestations or symptoms required slightly higher doses of prednisone in the range of 11–20mg (Group 2) frequently required second-line eosinophil lowering therapies. Subjects requiring ≥21mg prednisone (Group 3) clinically differed from Group 2 because the urgency of instituting second-line therapies was much greater to prevent progression of HES and/or prevent the significant side effects of longer term, high dose GC. Subjects who had no laboratory or clinical response to high dose prednisone given for at least 2 weeks (Group 4) were considered non-responders.
HES subtype categorization
During their clinical workup, subjects were diagnosed with one of the following HES clinical subtypes (1): lymphocytic variant HES (LHES), myeloid HES (MHES), EGPA/HES overlap, single organ HES (SO-HES) or idiopathic HES (IHES). Subjects with LHES had an aberrant lymphocyte population demonstrated by flow cytometry (6) and/or T cell receptor rearrangement by polymerase chain reaction (PCR). Subjects with clinical features of a myeloid neoplasm(7), but without confirmed cytogenetic or molecular abnormalities in the eosinophil lineage, were diagnosed with MHES. Subjects with HES and organ involvement typical of EGPA (eosinophilic granulomatosis with polyangiitis), but without biopsy proven vasculitis were classified as HES/EGPA overlap. Clinical features in this cohort included asthma, paranasal sinus involvement, nasal polyposis, pulmonary infiltrates, cardiomyopathy, neuropathy with or without perivascular eosinophilia demonstrated by biopsy. Subjects with HES with clinical manifestations restricted to a single organ system (i.e., eosinophilic gastrointestinal disease, eosinophilic hepatitis, eosinophilic fasciitis, chronic eosinophilic pneumonia) were classified single-organ HES (SO-HES) even though the organ involved varied between subjects. Finally, subjects with HES who did not fit any of the categories above were classified as idiopathic HES (IHES).
Statistics and model building
Fifteen baseline predictor variables were measured (Table 2) and fit using a univariate proportional odds model. All but 3 of the 15 variables had less than 8% missing, and we assumed missing to be completely at random. Inferences were made using the Rao’s score test with a sandwich estimator of variance, so that the inferences would be asymptotically valid whether or not the model was misspecified(8). Because there was collinearity among the 15 predictors, and to adjust for multiple comparisons, a multiple comparison permutation adjustment method was used(9). For models that did not converge, a more conservative estimate was utilized by moving a patient to the next response category to allow convergence. The best fit univariate model used HES diagnosis to predict GC response, and we tested whether any additional predictors could be added to significantly improve fit using a permutation multiple comparison adjustment method(9). Tests for association with demographic variables used Fisher’s exact test (gender, race) and analysis of variance (age). R (Version 3.3.2) (10) and SAS (Version 9.4) were used for statistical analysis.
Table 2.
Predictors from univariate proportional odds model.
| Predictor Variable | N | Unadjusted p-value* | Adjusted p-value** |
|---|---|---|---|
| HES subtype | 164 | 0.012 | p<.001 |
| LDH | 146 | 0.038 | 0.156 |
| Cardiac involvement | 164 | 0.058 | 0.156 |
| Serum vitamin B12 | 151 | 0.083 | 0.467 |
| Dermatologic involvement | 163 | 0.089 | 0.627 |
| Peak absolute Eosinophil count | 153 | 0.104 | 0.627 |
| Neurologic involvement | 164 | 0.189 | 0.871 |
| T-cell receptor rearrangement | 161 | 0.297 | 0.918 |
| IgE | 159 | 0.461 | 0.982 |
| Pulmonary involvement | 164 | 0.462 | 0.982 |
| Sinus involvement | 160 | 0.472 | 0.982 |
| Erythrocyte sedimentation rate | 88 | 0.59 | 0.982 |
| Pulmonary function testing | 94 | 0.666 | 0.982 |
| Gastrointestinal involvement | 163 | 0.685 | 0.982 |
| Serum tryptase | 152 | 0.974 | 0.982 |
Generalized estimating equations Score method, two-sided;
Permutation method adjusted for multiple comparisons; two-sided. HES-hypereosinophilic syndrome; LDH-lactose dehydrogenase,
Results
Most subjects with HES are steroid-responsive
Overall, 90% (149/164) of subjects responded to GC (Figure 1). Among the 149 responders, 64 (43.0%) were controlled on ≤10mg of prednisone equivalent (median 5mg, range 1.5–10mg) and 57 (38.3%) on 11–20mg of prednisone equivalent (median 16mg, range 11–20mg). Only 28 (18.8%) of the responders required ≥21mg of prednisone (median 37.5, range 21–80) to control AEC and symptoms. There were no significant differences between any of the groups with respect to demographics (Table 1).
Table 1.
Patient characteristics by dose category of prednisone.
| Group 1 (≤10mg) n=64 |
Group 2 11–20mg n=57 |
Group 3 (≥21mg) n=28 |
Group 4 Non-responders n=15 |
|
|---|---|---|---|---|
| Median Minimally Effective Dose of Prednisone in mg (range) |
5 (1.5–10) |
16 (11–20) |
37.5 (21–80) |
NA |
| Gender M/F |
38M/26F | 26M/31F | 10M/18F | 5M/10F |
| Race W/B/A/O/U* |
55/4/4/0/1 | 53/2/2/0/0 | 22/5/1/0/0 | 11/3/1/0/0 |
| Median peak AEC (range) |
4164 (500–48080) |
7900 (910–76500) |
4824 (897–26688) |
11237 (1100–82000) |
| Median Age in years (range) |
52.5 (2–85) |
42 (4–84) |
42 (14–63) |
49 (16–70) |
| Median Serum IgE level in unit (range) |
164.5 (3.3–6530) | 277 (5–16300) | 214 (3.7–42874) | 93.2 (1.6–2786) |
| Median Serum B12 level in (range) |
603.5 (227–3914) |
664 (293–5055) |
677 (201–1312) |
993 (205–2583) |
| Median Serum Tryptase level in (range) |
5.32 (0.99–18.4) |
4.86 (0.99-28.1) |
5.20 (1.22–16.5) |
4.5 (1.7–25.3) |
| Median Serum LDH in (range) |
193 (115–409) |
203 (90–435) |
205 (115–695) |
313 (100–587) |
| HES Subtype | ||||
| I-HES | 38 | 26 | 15 | 6 |
| HES/EGPA | 15 | 18 | 5 | 0 |
| LHES | 5 | 8 | 8 | 3 |
| MHES | 0 | 0 | 0 | 5 |
| SO-HES | 6 | 5 | 0 | 1 |
| Organ involvement | ||||
| Cardiac | 9/64 (14%) | 5/57 (9%) | 4/28 (14%) | 9/15 (50%) |
| Neurologic | 12/64 (19%) | 14/57 (25%) | 9/28 (32%) | 4/15 (27%) |
| Pulmonary | 37/64 (58%) | 39/57 (68%) | 17/28 (61%) | 10/15 (67%) |
| Gastrointestinal | 22/64 (34%) | 19/57 (33%) | 12/28 (43%) | 5/15 (33%) |
| Dermatologic | 32/64 (50%) | 36/57 (63%) | 20/28 (71%) | 9/15 (60%) |
| Sinus | 24/64 (37.5%) | 31/57 (54%) | 16/28 (57%) | 4/15 (27%) |
W-White, B-Black or African-American, A-Asian, O-Other, U-Unknown.
Abbreviations: LDH-Lactose dehydrogenase, IHES-idiopathic hypereosinophilic syndrome; HES/EGPA-Hypereosinophilic syndrome/Eosinophilic granulomatosis with polyangiitis; LHES-lymphocytic variant hypereosinophilic syndrome, MHES-myeloid hypereosinophilic syndrome, SO-HES-single organ hypereosinophilic syndrome.
Fifteen baseline clinical and laboratory variables were selected for the predictive analysis based on their importance in defining clinical subtype and/or reports of association with GC response (Table 2). We cannot exclude that the lack of association with GC response for the two variables with fewest observed values (“N”s denoted in Table 2), erythrocyte sedimentation rate and pulmonary function testing, was not due to a smaller sample size. In the univariate analysis, HES subtype and elevated serum LDH were significantly predictive of GC response. However, after correction for multiple comparisons, only HES subtype remained significantly predictive (Table 2). To confirm that the model fit was appropriate, the observed and the predicted proportion of each of the four response values (dose) within each diagnosis group (HES subtype) were plotted (Figure 2) and show that the model fit mirrors the sample proportions very closely. No additional predictors improved the model fit when combined with HES subtype in the proportional odds model (all adjusted p>0.4).
Figure 2.
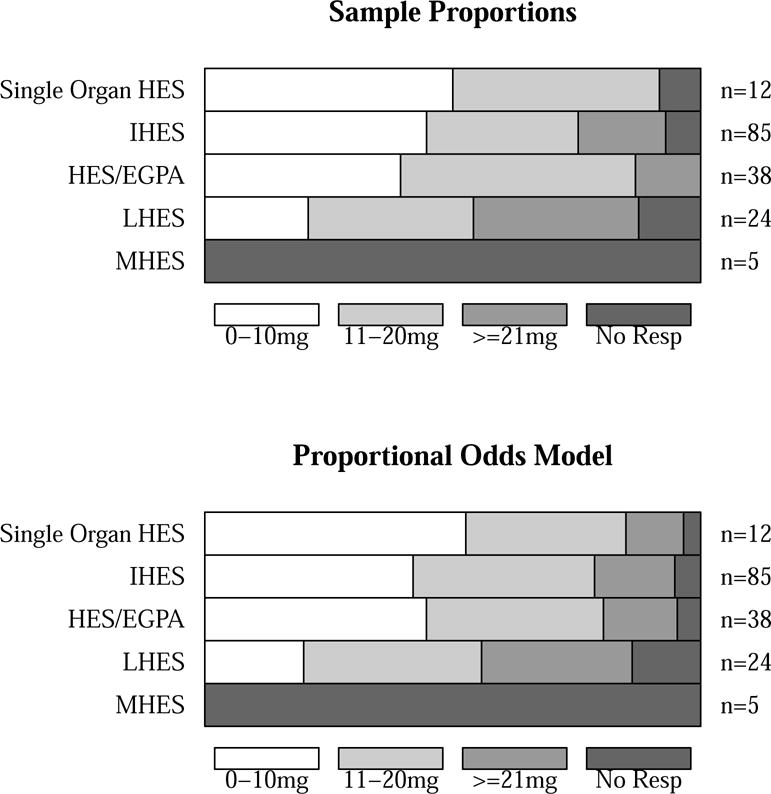
Graphical representation of sample and predicted proportions. Top, sample proportions for each response category (dose in mg) by HES subtype. Bottom, predicted proportions for each response category (dose in mg) by HES subtype from the proportional odds model.
Subjects with MHES and LHES are less responsive to GC than other HES subtypes
To quantify the odds of response to GC in various subtypes of HES, odds ratios were defined using idiopathic HES (IHES) as the reference (Table 3). Because the odds of response for the MHES subtype did not converge (OR=∞), one MHES non-responder was moved to the responsive category “>=21mg” for analysis purposes to allow statistical convergence (Table 3). Despite this change, the decreased response to GC in this clinical subtype remained significant. Subjects with HES/EGPA overlap and subjects with SO-HES did not have significantly different odds of response to GC when compared to subjects with IHES (1.12 [0.57–2.18], p=0.75 and 1.54[0.50–4/67], p=0.45, respectively). In contrast, subjects with LHES and MHES had significantly worse odds of response (0.34 [0.15–0.81], p=0.015 and 0.013 [0.0013–0.118, p=0.0001, respectively) when compared to IHES.
Table 3.
Odds ratios of response to GC compared to IHES reference
| Diagnosis Group | Odds Ratio = Odds (Diagnosis Group)/Odds (HES) | Lower 95% Confidence Limit | Upper 95% confidence limit | Two-sided p-value (testing for significant difference from HES) |
|---|---|---|---|---|
| I-HES | reference | – | – | – |
| HES/EGPA | 1.12 | 0.57 | 2.18 | 0.75 |
| LHES | 0.34 | 0.15 | 0.81 | 0.015 |
| MHES | 0.013* | 0.0013 | 0.118 | 0.0001 |
| SO-HES | 1.54 | 0.50 | 4.67 | 0.45 |
One subject was moved from “non-responsive” to “≥21mg” to allow convergence. I-HES-idiopathic hypereosinophilic syndrome; HES/EGPA-hypereosinophilic syndrome/eosinophilic granulomatosis with polyangiitis overlap, LHES-lymphocytic variant hypereosinophilic syndrome; MHES-myeloid hypereosinophilic syndrome; SO-HES, single-organ hypereosinophilic syndrome.
Discussion
Heterogeneity of response to GC has been appreciated since the first descriptions of HES in the 1970s(11)(12). However, the inclusion of patients with PDGFRA-associated disease in these case series complicates the interpretation of GC response data, since this mutation is known to be GC-resistant. In fact, in a large multicenter study of 188 subjects with HES(3), 179 of whom were treated with GC, subjects with known FIP1L1-PDGFRA mutations accounted for 13 (65%) of the 20 non-responders (Ogbogu et al., unpublished data). In the present study, subjects with known mutations involving PDGFRA were excluded. Overall, 9% of PDGFRA-negative subjects with HES were found to be unresponsive to GC. This is similar to the findings in a recent series of 33 patients with idiopathic HES, in which 18% of subjects were GC-resistant (p=0.13, Fisher’s exact test)(13).
Surprisingly, relatively few studies(14)(15) have explored the potential mechanisms of GC resistance in HES subjects. The selective absence of GC receptor expression on eosinophils was reported in a subset of GC-resistant patients with HES in 1989(4). However, the clinical characteristics of many of the receptor-deficient patients in this cohort are suggestive of PDGFRA-positive disease (male gender, elevated serum B12, cardiac involvement). Thus, the broader applicability of the findings to PDGFRA-negative HES is uncertain. In vitro studies have focused on the reciprocal relationship between IL-5 and GC in regulating eosinophil apoptosis as a potential cause of GC-resistance in HES(14)(15), although this has not been convincingly demonstrated in vivo. From a clinical standpoint, GC-responsiveness has been associated with elevated IgE levels in several small studies(12), but this relationship was not confirmed in two larger studies where PDGFRA-positive subjects were excluded(3,13). Finally, although elevated serum thymus and activation regulated chemokine (TARC) levels were more frequent in GC-responsive patients with HES in two studies(3,16), measurement of this mediator is not standardized and its utility as a predictor of response remains unproven.
A major limitation of prior studies of GC responsiveness in HES has been the fact that the definition of “response” has not been universally applied. In the present study, statistical models were used to determine predictors of response to GC using a standard definition of response in a large cohort of subjects with PDGFRA-negative HES treated with GC. Predictors were chosen from data collected as part of a typical evaluation for HES and were based on available information on GC response from the literature. One limitation of this study was the retrospective design, which resulted in missing variables for some subjects. The lack of association with GC response for the variables with most missing values in the univariate testing may be related to the smaller sample size. The best-fit model with the available data showed that HES subtype was the most predictive of response to GC. Fortunately, the plausibility of the findings after correction for testing 15 predictors mirrors clinical experience in this disorder. A second limitation of the study was the potential for over-fitting of the model because of the number of variables included in the model. We used a permutation multiple comparison procedure(9) to account for over-fitting while considering issues of collinearity of abnormal laboratory values. Finally, we had to move one MHES subject from the non-response category to a prednisone-response category to allow the model to converge. If anything, this suggests that the odds of response to GC in PDGFRA-negative MHES is even less than predicted in this model. In clinical practice, an HES subtype diagnosis is made using a combination of signs and symptoms in addition to individual laboratory parameters. It became apparent after the model was designed that these laboratory parameters became irrelevant once an HES subtype diagnosis was made.
In summary, our findings suggest that assignment of an HES subtype diagnosis is an important determinant of GC response in HES. Historically, patients with PDGFRA mutations have been described to be unresponsive to corticosteroids; however, a diagnosis of PDGFRA-negative MHES also predicts non-response to GC. For patients with LHES, initiation of second-line therapies may be useful early in the course of disease, since more than two thirds of the subjects with LHES in this retrospective cohort required moderate to high dose corticosteroids for disease control. Elucidation of the biologic reasons for the heterogeneity of response to GC could provide further insight into the etiology of different HES subtypes.
Highlights box.
What is already known about this topic?
Although small case series and one retrospective multicenter review suggest that steroid response is variable in HES, this has not been examined systematically in a diverse group of subjects with HES evaluated in a uniform manner.
What does this article add to our knowledge?
This article characterized the predictors of response to corticosteroids among groups of subjects with HES and may inform treatment decisions based on clinical HES subtype.
How does this study impact current management guidelines?
There are no standardized guidelines for management of HES. Results of this study may inform decisions to initiate second-line therapy in certain HES subtypes or consideration of referral to tertiary centers with experience in HES.
Acknowledgments
We would like to thank the Laboratory of Parasitic Diseases staff and the research subjects without whom the studies described would not have occurred.
Funding:
This study was funded by the Division of Intramural Research, NIAID, NIH. This project has been funded in whole or in part with federal funds from the National Cancer Institute, National Institutes of Health, under Contract No. HHSN261200800001E. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Abbreviations used
- AEC
absolute eosinophil count
- EGPA
eosinophilic granulomatosis with polyangiitis
- GC
glucocorticoid
- HES
hypereosinophilic syndrome
- IHES
idiopathic hypereosinophilic syndrome
- LHES
lymphocytic variant HES
- MHES
myeloid HES
- MN
myeloid neoplasm
- PCR
polymerase chain reaction
- PDGFRA
platelet-derived growth factor α
- SO-HES
single-organ HES
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No authors disclose any conflicts of interest.
Bibliography
- 1.Klion AD. How I treat hypereosinophilic syndromes. Blood. 2015 Aug 27;126(9):1069–77. doi: 10.1182/blood-2014-11-551614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cools J, DeAngelo DJ, Gotlib J, Stover EH, Legare RD, Cortes J, et al. A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med. 2003 Mar 27;348(13):1201–14. doi: 10.1056/NEJMoa025217. [DOI] [PubMed] [Google Scholar]
- 3.Ogbogu PU, Bochner BS, Butterfield JH, Gleich GJ, Huss-Marp J, Kahn JE, et al. Hypereosinophilic syndrome: a multicenter, retrospective analysis of clinical characteristics and response to therapy. J Allergy Clin Immunol. 2009 Dec;124(6):1319–25.e3. doi: 10.1016/j.jaci.2009.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prin L, Lefebvre P, Gruart V, Capron M, Storme L, Formstecher P, et al. Heterogeneity of human eosinophil glucocorticoid receptor expression in hypereosinophilic patients: absence of detectable receptor correlates with resistance to corticotherapy. Clin Exp Immunol. 1989 Dec;78(3):383–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Khoury P, Desmond R, Pabon A, Holland-Thomas N, Ware JM, Arthur DC, et al. Clinical features predict responsiveness to imatinib in platelet-derived growth factor receptor-alpha-negative hypereosinophilic syndrome. Allergy. 2016 Jun;71(6):803–10. doi: 10.1111/all.12843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roufosse F, Cogan E, Goldman M. Lymphocytic variant hypereosinophilic syndromes. Immunol Allergy Clin North Am. 2007 Aug;27(3):389–413. doi: 10.1016/j.iac.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Klion AD, Noel P, Akin C, Law MA, Gilliland DG, Cools J, et al. Elevated serum tryptase levels identify a subset of patients with a myeloproliferative variant of idiopathic hypereosinophilic syndrome associated with tissue fibrosis, poor prognosis, and imatinib responsiveness. Blood. 2003 Jun 15;101(12):4660–6. doi: 10.1182/blood-2003-01-0006. [DOI] [PubMed] [Google Scholar]
- 8.Boos DD, Stefanski LA. Essential statistical inference : theory and methods. New York: Springer; 2013. [Google Scholar]
- 9.Westfall PH, Young SS. Resampling-Based Multiple Testing: Examples and Methods for P-Value Adjustment. John Wiley & Sons; 1993. [Google Scholar]
- 10.R Development Core Team. R: A language and environment for statistical computing [Internet] Vienna, Austria: R Foundation for Statistical Computing; 2016. Available from: http://www.R-project.org. [Google Scholar]
- 11.Chusid MJ, Dale DC, West BC, Wolff SM. The hypereosinophilic syndrome: analysis of fourteen cases with review of the literature. Medicine. 1975 Jan;54(1):1–27. [PubMed] [Google Scholar]
- 12.Parrillo JE, Fauci AS, Wolff SM. Therapy of the hypereosinophilic syndrome. Ann Intern Med. 1978 Aug;89(2):167–72. doi: 10.7326/0003-4819-89-2-167. [DOI] [PubMed] [Google Scholar]
- 13.Helbig G, Wiśniewska-Piąty K, Francuz T, Dziaczkowska-Suszek J, Kyrcz-Krzemień S. Diversity of clinical manifestations and response to corticosteroids for idiopathic hypereosinophilic syndrome: retrospective study in 33 patients. Leuk Lymphoma. 2013 Apr;54(4):807–11. doi: 10.3109/10428194.2012.731602. [DOI] [PubMed] [Google Scholar]
- 14.Debierre-Grockiego F, Leduc I, Prin L, Gouilleux-Gruart V. Dexamethasone inhibits apoptosis of eosinophils isolated from hypereosinophilic patients. Immunobiology. 2001 Dec;204(4):517–23. doi: 10.1078/0171-2985-00060. [DOI] [PubMed] [Google Scholar]
- 15.Wallen N, Kita H, Weiler D, Gleich GJ. Glucocorticoids inhibit cytokine-mediated eosinophil survival. J Immunol. 1991 Nov 15;147(10):3490–5. [PubMed] [Google Scholar]
- 16.de Lavareille A, Roufosse F, Schmid-Grendelmeier P, Roumier A-S, Schandené L, Cogan E, et al. High serum thymus and activation-regulated chemokine levels in the lymphocytic variant of the hypereosinophilic syndrome. J Allergy Clin Immunol. 2002 Sep;110(3):476–9. doi: 10.1067/mai.2002.127003. [DOI] [PubMed] [Google Scholar]


