Abstract
As the world’s most populated and rapidly aging country, there is limited information on sex-related differences in factors regarding uncomplicated colonic diverticulosis in China. We aimed to investigate sex differences in individual risk factor in a northern metropolis. Patients with colonic diverticulosis who underwent indicated colonoscopy were queried with respect to medical history and demographic features. Demographic information, life style factors and co-morbidities were retrieved from a prospective dataset. Multiple regression analyses were performed to determine precipitating factors of diverticula. Of 4,386 enrolled patients, colonic diverticulosis were detected in 218 cases (4.97%). Multiple logistic regression analysis implicated increasing age (OR = 1.05, 95%CI 1.03–1.06, P < 0.001), red meat ≥100 g/d (OR = 2.53, 95%CI 1.72–3.70, P < 0.001), smoking (OR = 2.14, 95%CI 1.05–4.33, P = 0.035), rheumatologic diseases (OR = 3.38, 95%CI 1.09–10.5, P = 0.035) and NSAIDs (OR = 2.11, 95%CI 1.12–3.97, P = 0.020) were significantly associated with diverticulosis in men, whilst advancing age (OR = 1.03, 95%CI 1.01–1.05, P = 0.013), BMI (OR = 1.12, 95%CI 1.04–1.19, P = 0.001), smoking (OR = 10.2, 95%CI 2.81–37.4, P < 0.001), rheumatologic diseases (OR = 8.04, 95%CI 3.05–21.2, P < 0.001), hypertension (OR = 1.76, 95%CI 1.01–3.06, P = 0.047), colonic polyps (OR = 3.12, 95%CI 1.82–5.36, P < 0.001) and antihypertensive medications (OR = 2.99, 95%CI 1.66–5.39, P < 0.001) in women. In conclusion, it is pivotal to take account of differentially sex-related factors in regard to the development of uncomplicated colonic diverticulosis.
Introduction
China has underwent rapid growth of aging population during recent decades; those aged ≥ 75 years accounted for 3.5% of the population in 2013, and there were 200 million elderly residents aged ≥ 65 years in 20141. Therefore the burden of diseases, especially entity with a higher prevalence among the elderly, including uncomplicated colonic diverticulosis, is predicted to increase in the future2,3. As a matter of fact, the rates of diverticula have dramatically increased from 2.78% in 2011 to 4.98% in 2015 according to dataset from our endoscopy center (data not shown). Aside from aging, the pathogenesis of diverticulosis is thought to be multifactorial, including diet, colonic motility, obesity, medications and genetic factors4. More recently, it has been recognized that altered gut microbiota composition and abnormal immune signatures may contribute to the development and progression of uncomplicated diverticular disease5,6. Of note, explicit sex-specific diet-microbiota correlations have been documented in humans7. After reviewing current body of literature, gender was evidently associated with the presence of diverticulosis5,8–10. Thus, it is plausible to hypothesize that sex-related differences regarding risk factors for the formation of diverticula. Collectively, we aimed to assess potential factors related to diverticulosis by capturing and analyzing demographic, environmental and pathological information on recruited subjects on a sex disparity basis.
Results
Prevalence and sex differences in baseline characteristics
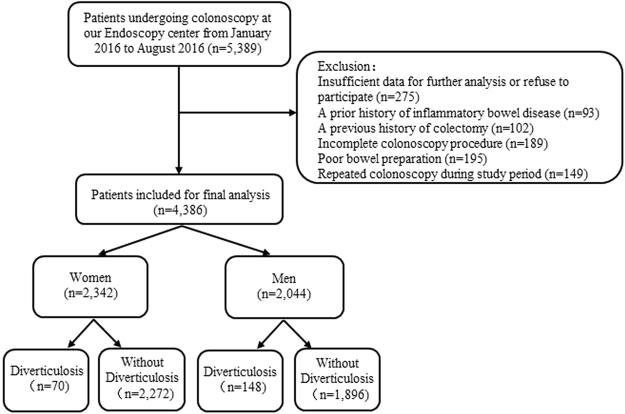
A total of 4,386 consecutive cases undergoing complete colonoscopy were finally recruited during this study period (Fig. 1). Of these, 218 participants with uncomplicated colonic diverticulosis were finally identified, comprising 148 men (7.24% of 2,044 men) and 70 women (2.99% of 2,342 women). The overall prevalence of colonic diverticulosis was 4.97%. Diverticula were right-sided in 67.0%, bilateral in 18.3%, and left-sided in 14.7% of patients with diverticulosis.
Figure 1.
Flow diagram of patients included for current study.
Of the entire population, women were more likely than men to be older (mean age of 54.7 years vs 52.6 years, P < 0.001). There were more women aged 50–59 years (33.5% vs 23.9%) and 60–69 years (32.2% vs 29.2%) in comparison with men. Moreover, women had lower levels of BMI and lower frequencies of weekly exercise, red meat, smoking status as well as alcoholic consumption (P < 0.001 for all). Concerning comorbidities and medication, the prevalence of colonic polyps was significant higher in men, whereas the use of mucosal protective drugs was more common in women (Table 1).
Table 1.
Sex differences in baseline characteristics of the study population.
| Characteristics | Men (n = 2,044) | Women (n = 2,342) | P values | Cohen’s D |
|---|---|---|---|---|
| Demographics and life style factors | ||||
| Age (years), mean (SD) | 52.6 (14.4) | 54.7 (12.9) | <0.001 | 0.15 |
| Age (years), n (%) | <0.001 | 0.29 | ||
| ≤39 | 460 (22.5) | 319 (13.6) | ||
| 40–49 | 303 (14.8) | 289 (12.4) | ||
| 50–59 | 489 (23.9) | 784 (33.5) | ||
| 60–69 | 597 (29.2) | 755 (32.2) | ||
| ≥70 | 195 (9.6) | 195 (8.3) | ||
| Education (years), n (%) | 0.999 | 0.00 | ||
| ≤6 | 172 (8.4) | 197 (8.4) | ||
| 07-Sep | 496 (24.3) | 570 (24.3) | ||
| 10-Dec | 516 (25.2) | 592 (25.3) | ||
| >12 | 860 (42.1) | 983 (42.0) | ||
| Residence, n (%) | 0.870 | 0.01 | ||
| Urban | 1,649 (80.7) | 1,894 (80.9) | ||
| Rural | 395 (19.3) | 448 (19.1) | ||
| BMI (kg/m2), mean (SD) | 24.2 (3.1) | 23.0 (3.4) | <0.001 | 0.37 |
| BMI, n (%) | <0.001 | 0.31 | ||
| <25 | 1,313 (64.2) | 1,834 (78.3) | ||
| 25–30 | 649 (31.8) | 412 (17.6) | ||
| >30 | 82 (4.0) | 96 (4.1) | ||
| Exercise habit, n (%) | <0.001 | 0.26 | ||
| ≤3 times/week | 857 (41.9) | 1,281 (54.7) | ||
| >3 times/week | 1,187 (58.1) | 1,061 (45.3) | ||
| Red Meat, n (%) | <0.001 | 0.32 | ||
| <100 g/d | 1,594 (78.0) | 2,138 (91.3) | ||
| ≥100 g/d | 450 (22.0) | 204 (8.7) | ||
| Smoking index, n (%) | <0.001 | 0.85 | ||
| Nonsmoker | 1,162 (56.8) | 2,314 (98.8) | ||
| <400 | 294 (14.4) | 12 (0.5) | ||
| ≥400 | 588 (28.8) | 16 (0.7) | ||
| Alcohol consumption, n (%) | <0.001 | 0.54 | ||
| Non-drinker | 1,548 (75.7) | 2,315 (98.8) | ||
| Light/Moderate drinker (1–350 g/week) | 96 (4.7) | 27 (1.2) | ||
| Heavy drinker (≥351 g/week) | 400 (19.6) | 0 (0) | ||
| Comorbidities, n (%) | ||||
| Hypertension | 371 (18.2) | 428 (18.3) | 0.915 | 0.00 |
| Diabetes mellitus | 151 (7.4) | 143 (6.1) | 0.09 | 0.05 |
| Coronary heart disease | 94 (4.6) | 111 (4.7) | 0.826 | 0.00 |
| Colonic polyps | 1,030 (50.4) | 919 (39.2) | <0.001 | 0.22 |
| Upper gastrointestinal diseasesa | 151 (7.4) | 164 (7.0) | 0.622 | 0.02 |
| Hepato-biliary diseasesb | 92 (4.5) | 86 (3.7) | 0.165 | 0.04 |
| Dyslipidemia | 46 (2.3) | 64 (2.7) | 0.308 | 0.03 |
| Rheumatologic diseasesc | 46 (2.3) | 43 (1.8) | 0.331 | 0.03 |
| Miscellaneousd | 186 (9.1) | 203 (8.7) | 0.616 | 0.01 |
| Medication, n (%) | ||||
| NSAIDs | 115 (5.6) | 125 (5.3) | 0.675 | 0.01 |
| Corticosteroid | 25 (1.2) | 32 (1.4) | 0.676 | 0.02 |
| PPIs | 123 (6.0) | 169 (7.2) | 0.112 | 0.05 |
| Mucosal protective drugs | 432 (21.1) | 607 (25.9) | <0.001 | 0.12 |
| Antihypertension drugs | 363 (17.8) | 422 (18.0) | 0.823 | 0.01 |
| Hypoglycemic medications | 149 (7.3) | 138 (5.9) | 0.62 | 0.05 |
Data are expressed as mean ± SD or number (percentage).
BMI body mass index, NSAIDs non-steroidal anti-inflammatory drugs, PPIs proton pump inhibitors.
aReflux esophagitis, atrophic gastritis, chronic gastritis, etc.
bCholelithiasis and fatty liver disease.
cRheumatoid arthritis and gout.
dOsteoporosis, arrhythmia, cerebral infarction, thyroid diseases, prostate diseases, etc.
Sex differences in risk factors for diverticulosis
We first implicated that male gender was a precipitating factor for the presence of diverticulosis in whole study population (Table S1). In addition, concerning dramatically disparities regarding the baseline features, we next investigated risk factors associated with the formation of diverticula according to sex differences.
Table 2 implicated that age, smoking index, hypertension, rheumatologic diseases, antihypertension drugs and NSAIDs were associated with the presence of colonic diverticulosis in both men and women on the univariate analyses. Moreover, red meat was a precipitating factor for diverticula in men, whilst BMI and concomitant polyps were associated with the presence of colonic diverticulosis in women.
Table 2.
The sex differences in risk factors of colonic diverticulosis on univariate analyses.
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Div (+) (n = 148) | Div (−) (n = 1,896) | P values | Div (+) (n = 70) | Div (−) (n = 2,272) | P values | |
| Age, (years), mean (SD) | 59.5 (10.6) | 52 (14.5) | <0.001 | 58.0 (11.8) | 54.6 (12.9) | 0.029 |
| Age (years), n (%) | <0.001 | <0.001 | ||||
| ≤39 | 6 (4.0) | 285 (15.0) | 10 (14.3) | 309 (13.6) | ||
| 40–49 | 18 (12.2) | 440 (23.2) | 6 (8.6) | 283 (12.5) | ||
| 50–59 | 49 (33.1) | 548 (28.9) | 12 (17.1) | 772 (33.9) | ||
| 60–69 | 49 (33.1) | 169 (8.9) | 24 (34.3) | 731(32.2) | ||
| ≥70 | 26 (17.6) | 454 (24.0) | 18 (25.7) | 177 (7.8) | ||
| Education (years), n (%) | 0.971 | 0.999 | ||||
| ≤6 | 14 (9.5) | 158 (8.3) | 6 (8.6) | 191 (8.4) | ||
| 7–9 | 35 (23.6) | 461 (24.3) | 17 (24.3) | 553 (24.3) | ||
| 10–Dec | 37 (25.0) | 479 (25.3) | 18 (25.7) | 574 (25.3) | ||
| >12 | 62 (41.9) | 798 (42.1) | 29 (41.4) | 954 (42.0) | ||
| Residence, n (%) | 0.243 | 0.619 | ||||
| Urban | 114 (77.0) | 1,535 (81.0) | 55 (78.6) | 1,839 (80.9) | ||
| Rural | 34 (23.0) | 361 (19.0) | 15 (21.4) | 433 (19.1) | ||
| BMI (kg/m2), mean (SD) | 24.6 (3.4) | 24.2 (3.1) | 0.105 | 24.5 (3.8) | 22.9 (3.3) | <0.001 |
| BMI, n (%) | 0.105 | <0.001 | ||||
| <25 | 86 (58.1) | 1,227 (64.7) | 41 (58.6) | 1,793 (78.9) | ||
| 25–30 | 52 (35.1) | 597 (31.5) | 19 (27.1) | 393 (17.3) | ||
| >30 | 10 (6.8) | 72 (3.8) | 10 (14.3) | 86 (3.8) | ||
| Exercise habit, n (%) | 0.483 | 0.181 | ||||
| ≤3 times/week | 58 (39.2) | 799 (42.1) | 44 (62.9) | 1,237 (54.4) | ||
| >3 times/week | 90 (60.8) | 1,097 (57.9) | 26 (37.1) | 1,035 (45.6) | ||
| Red Meat, n (%) | 0.001 | 0.83 | ||||
| <100 g/d | 99 (66.9) | 1,495 (78.9) | 65 (92.9) | 2,073 (91.2) | ||
| ≥100 g/d | 49 (33.1) | 401 (21.1) | 5 (7.1) | 199 (8.8) | ||
| Smoking index, n (%) | 0.009 | <0.001 | ||||
| Nonsmoker | 67 (45.3) | 1,095 (57.8) | 65 (92.8) | 2,249 (99.0) | ||
| <400 | 30 (20.3) | 264 (13.9) | 1 (1.4) | 11 (0.5) | ||
| ≥400 | 51 (34.4) | 537 (28.3) | 4 (5.8) | 12 (0.5) | ||
| Alcohol consumption, n (%) | 0.153 | 0.199 | ||||
| Non-drinker | 121 (81.8) | 1,427 (75.3) | 70 (100) | 2,245 (98.8) | ||
| Light/moderate drinker | 7 (4.7) | 89 (4.7) | 0 (0) | 27 (1.2) | ||
| (1–350 g/week) | 0 (0) | 0 (0) | ||||
| Heavy drinker (≥351 g/week) | 20 (13.5) | 380 (20.0) | ||||
| Hypertension | 42 (28.4) | 329 (17.4) | 0.002 | 23 (32.9) | 405 (17.8) | 0.003 |
| Diabetes mellitus | 13 (8.8) | 138 (7.3) | 0.512 | 8 (11.4) | 135 (5.9) | 0.071 |
| Coronary heart disease | 10 (6.8) | 84 (4.4) | 0.217 | 5 (7.1) | 106 (4.7) | 0.381 |
| Colonic polyps | 81 (54.7) | 949 (50.1) | 0.306 | 42 (60.0) | 877 (38.6) | 0.01 |
| Upper gastrointestinal diseases | 12 (8.1) | 139 (7.3) | 0.728 | 5 (7.1) | 159 (7.0) | 0.963 |
| Hepato-biliary diseases | 5 (3.4) | 87 (4.6) | 0.494 | 5 (7.1) | 81 (3.6) | 0.117 |
| Dyslipidemia | 4 (2.7) | 42 (2.2) | 0.571 | 4 (5.7) | 60 (2.6) | 0.122 |
| Rheumatologic diseases | 9 (6.1) | 37 (2.0) | 0.001 | 10 (14.3) | 33 (1.5) | <0.001 |
| Miscellaneous | 14 (9.5) | 172 (9.1) | 0.874 | 10 (14.3) | 193 (8.5) | 0.09 |
| NSAIDs | 24 (16.2) | 91 (4.8) | <0.001 | 10 (14.3) | 115 (5.1) | 0.003 |
| Corticosteroid | 4 (2.7) | 21 (1.1) | 0.102 | 3 (4.3) | 29 (1.3) | 0.068 |
| PPIs | 11 (7.4) | 112 (5.9) | 0.47 | 5 (7.1) | 164 (7.2) | 1 |
| Mucosal protective drugs | 35 (23.6) | 397 (20.9) | 0.464 | 24 (34.3) | 583 (25.7) | 0.127 |
| Antihypertension medications | 40 (27.0) | 323 (17.0) | 0.004 | 22 (31.4) | 400 (17.6) | 0.006 |
| Hypoglycemic medications | 15 (10.0) | 134 (7.1) | 0.186 | 7 (10.0) | 131 (5.8) | 0.188 |
Data are expressed as mean ± SD or number (percentage).
Div (−): patients without diverticulosis.
Div (+): patients with diverticulosis.
BMI body mass index, NSAIDs non-steroidal anti-inflammatory drugs, PPIs proton pump inhibitors.
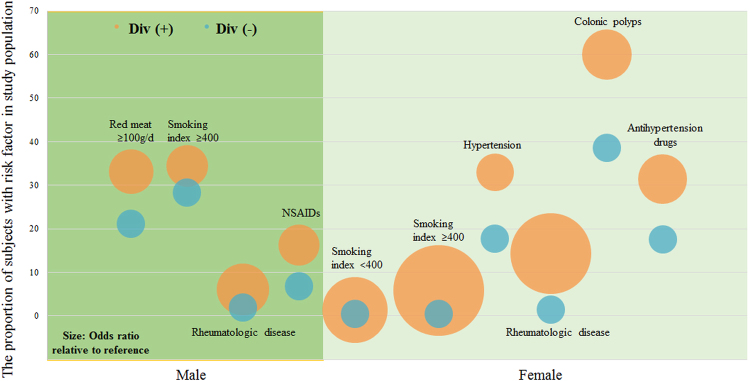
Based on multivariate analyses, advancing age, increasing smoking index and rheumatologic comorbidity were significantly associated with diverticulosis in both men and women. The risk of colonic diverticulosis increased with age; the corresponding adjusted OR (95% CI) were 1.05 (1.03–1.06) and 1.03 (1.01–1.05) in men and women, respectively. Moreover, individuals with smoking index no less than 400 and rheumatologic diseases had a higher risk of diverticulosis, with adjusted OR (95% CI) of 2.14 (1.05–4.33) and 10.2 (2.81–37.4) for smoking status, 3.38 (1.09–10.5) and 8.04 (3.05–21.2) for rheumatologic comorbidity in men and women, respectively. The corresponding adjusted ORs (95% CI) in men were 2.53 (1.72–3.70) for consumed red meat ≥ 100 g per day and 2.11 (1.12–3.97) for NSAIDs; in women, adjusted ORs (95% CI) were 1.12 (1.04–1.19) for elevated BMI, 1.76 (1.01–3.06) for hypertension, 3.12 (1.82–5.36) for polyps and 2.99 (1.66–5.39) for regular usage of antihypertensive medication (Table 3 and Fig. 2).
Table 3.
The sex differences in risk factors of colonic diverticulosis on multivariate analyses.
| Risk factors | Reference | B | Adjusted OR (95% CI) | P values |
|---|---|---|---|---|
| Men | ||||
| Age | — | 0.047 | 1.05 (1.03, 1.06) | <0.001 |
| Red meat ≥ 100 g/d | Red meat < 100 g/d | 0.926 | 2.53 (1.72, 3.70) | <0.001 |
| Smoking index | ||||
| <400 | Nonsmoker | 0.317 | 1.37 (0.96, 1.97) | 0.084 |
| ≥400 | Nonsmoker | 0.759 | 2.14 (1.05, 4.33) | 0.035 |
| Hypertension | Non-hypertension | 1.216 | 3.37 (0.69, 16.4) | 0.133 |
| Rheumatologic diseases | Non-rheumatologic diseases | 1.216 | 3.38 (1.09, 10.5) | 0.035 |
| NSAIDs | Non-NSAIDs | 0.748 | 2.11 (1.12, 3.97) | 0.020 |
| Antihypertension medications | Non-Antihypertension medications | 0.447 | 1.08 (0.52, 11.8) | 0.159 |
| Women | ||||
| Age | — | 0.028 | 1.03 (1.01, 1.05) | 0.013 |
| BMI (kg/m²) | — | 0.109 | 1.12 (1.04, 1.19) | 0.001 |
| Smoking index | ||||
| <400 | Nonsmoker | 1.680 | 5.37 (1.03, 27.9) | 0.046 |
| ≥400 | Nonsmoker | 2.327 | 10.2 (2.81, 37.4) | <0.001 |
| Hypertension | Non-hypertension | 0.564 | 1.76 (1.01, 3.06) | 0.047 |
| Rheumatologic diseases | Non-rheumatologic diseases | 2.084 | 8.04 (3.05, 21.2) | <0.001 |
| Colonic polyps | Non-colonic polyps | 1.138 | 3.12 (1.82, 5.36) | <0.001 |
| Antihypertension drugs | Non-antihypertension drugs | 1.094 | 2.99 (1.66, 5.39) | <0.001 |
| NSAIDs | Non-NSAIDs | 0.095 | 1.10(0.46, 2.66) | 0.833 |
BMI body mass index, NSAIDs non-steroidal anti-inflammatory drugs, OR odds ratio, CI confidence interval.
Figure 2.
Proportion of subjects with indicated risk factor (P < 0.05 for all) and odds ratio (OR) relative to reference in study population by the presence of diverticula. Circles show the proportion (y-axis) and OR (diameter) relative to each reference. Div (+), patients with diverticulosis; Div (−), patients without diverticulosis.
Discussion
To our knowledge, this is the first cross-sectional study to evaluate relevant risk factors of uncomplicated colonic diverticulosis in mainland China. Furthermore, we reported sex differences in risk factors for the formation of diverticula, whereas older age, increasing tabacco consumption and rheumatologic diseases were independent risk factors in both men and women.
It has been renewed interest and urgent reappraisal towards colonic diverticula, as this entity and its related complications may impose a serious burden on public healthcare systems. With the growing body of elder population and advent of widely colonoscopy-based examinations, the estimated prevalence of the disease has been still increasing in Western countries on a yearly basis. While still low in comparison to Western countries, an increasing trend regarding prevalence was also observed in several Asian countries and areas, including Singapore (45%), Thailand (28.5%), Japan (20.3%) and Taiwan (13.5%)10–13. More recently, a study form Southern China has implied an overall diverticulosis prevalence as 1.97% without significant change over more than one decade14. However, the representative of study mentioned above is limited, partly due to relatively small proportion of elderly, various lifestyle and dietary pattern differences across North and South China15. Aside from aging, environmental factors have also been identified as risk factors for the formation of diverticula. Recent epidemiological data indicated that genetic variants and underlying molecular pathobiology may contribute to the development to some extent. Intriguingly, Barbara and colleagues provided evidence integrating mucosal immunological information with gut microbiota and metabolic profiles with respect to the pathogenesis of diverticulosis6. Diet and sex have been broadly investigated and suggested as possible predisposed factors for the presence of diverticula in extensive research. Diet, as a source of colonizing bacteria, can alter the gut nutritional environment and subsequently influence the composition of microbiota7. As being a genetic trait, sex, may also affect the microbiota through hormone-microbe interaction and sex-specific immune responses. It has been addressed that studies omitting sex difference will overlook these interactions and consequently fail to determine environmental impacts. Moreover, several observations suggested a sharp sex distinction in regard to diverticular disease and its manifestations, that is, men were predisposed to diverticular bleeding while women were more likely present with strictures/obstructions16. Collectively, we intend to detect sex-related risk factors of colonic diverticulosis in this cross-sectional study after reviewing dramatically distinct baseline characteristics within the sexes.
Although a growing body of literature has been published to demonstrate the association between diverticulosis and conventional risk factors, the results remain controversial and predominantly arise in theoretical models. Of note, it is evident that several long-held beliefs, time-honored concepts and classic teachings on diverticula are challenged by recent research. For instance, dietary fiber is no longer regarded as protective against the development of diverticulosis3.
We found advancing age, heavy tobacco consumption and rheumatologic diseases were strong risk factors associated with the formation of diverticular in both men and women. Age has been posited as the most pronounced risk factor for diverticulosis in previous many reports. It has been proposed that elderly may develop abnormal thickness of colonic wall and frail muscular structure which is susceptible to incremental intraluminal pressure17,18. A positive association of diverticulosis and smoking status was unveiled in our study, whose role and exact mechanism were still in controversy; however, pertaining to a proinflammatory stimulus, disturbance on colonic motility and impacts against microflora homeostasis have all been postulated to play a role19–21. Furthermore, we also noted a higher prevalence of rheumatologic disorders in patients with diverticulosis. This is in accordance with previous findings implying association between inflammatory connective tissue diseases and diverticula5,22. While, smoking by itself is so far the most well-established environmental risk factor in the development of rheumatoid arthritis23.
In women, we also demonstrated that concomitant hypertension and antihypertensive medications were more prevalent in subjects with diverticulosis, which is consistent with previous findings by Yazici and colleagues5. This may partly be a reflection of older age amongst patients with diverticula, and elder women were more likely to have hypertension and higher systolic blood pressure than men24. Additionally, an outperformed study in China implied that a traditional northern dietary pattern was closely associated with both higher prevalence of hypertension and blood pressure, and the associations were largely explained by BMI. It is noteworthy that women with diverticulosis were likely to be obese (BMI > 30) compared to men as shown in Table 2. Moreover, numerous studies have been conducted in investigating the effects of obesity on shifts in microbiota in human beings, and further efforts are warranted to see if it can explain increasing risk of diverticulosis in such population25–27. At last, the coexisting colonic polyps and diverticulosis should be attributed to many similarities form the epidemiologic stand points and risk factors instead of causative relationship28,29.
Our results indicated that higher intake of red meat consumption and the usage of NSAIDs were both associated with the presence of diverticula in men. Whether the association between red meat consumption and uncomplicated diverticular disease remains unclear, red meat intake might influence the gut microflora or contribute to high energy intakes, which provide partial explanation for these correlations23. NSAIDs users hold more risk to develop symptomatic diverticular diseases than non-users. And it was hypothesized that this increased risk was attributable to mucosal damage resulting in impaired barrier of the colonic mucosa allowing bacteria translocation, which aggravate inflammation30.
We should not overlook potential limitations of our study. First, it is difficult to formally draw conclusions about causality due to its cross-sectional design in nature. However, this problem is mitigated by the inclusion of subjects with various colonoscopic indications, although residual bias may still exist. Second, data on lifestyle factors were retrieved by questionnaires referring to a period of almost one year, which may give rise to recall error. However, a face-to-face reviewed system with two well trained investigators (FY and YZ) can eliminate this adverse impact to some degree. Third, we lack of detailed information on dietary patterns (e.g. fruit, bean or nut fiber). Although we tried to adjust for major demographic and environmental factors simultaneously, residual confounding by unmeasured or unknown factors might be present. Conversely, taken account of the magnitude of many of the risk estimates and consistency of our results with past reports in regard to risk factors of colonic diverticula, it is improbable that all of the identified risk differences are attributable to the results of residual confounding. Fourth, we failed to determine a definite association between alcohol use and the presence of diverticulosis, inconsistent with prior cohort studies, while influence of this upon diverticulosis is still controversial3,13,20,31. Our sample population had therefore a higher proportion of non-drinkers in both genders (more than 75% of enrolled participants) compared with research from western countries which have made it difficult to detect an association between alcohol and diverticulosis. Actually, the East-West paradox are paramount in disease prevalence and phenotype28.
Conclusions
In conclusion, the prevalence of diverticulosis was 7.24% in men and 2.99% in women among the study population in a metropolitan area from Northern China. This study was the first to explore sex differences on associated risk factors among patients with uncomplicated colonic diverticulosis. Advancing age, increasing smoking index and rheumatologic comorbidity were significantly associated with diverticulosis in both men and women. Specifically, men with higher red meat consumption and use of NSAIDs were predisposed to colonic diverticula, whilst this entity was more prevalent in women with incremental BMI, concurrent hypertension, polyps and use of antihypertension drugs. Therefore, our results pave the way for further large-scale survey aiming at identifying sex-specific conventional risk factors; individualized uncomplicated diverticulosis prevention/intervention and promotion of healthy lifestyle are critical.
Materials and Methods
Participants and study design
We conducted a cross-sectional single-center study in adults undergoing colonoscopy at the Endoscopy Center, Department of Gastroenterology and Hepatology, Tianjin Medical University General Hospital (TJMUGH) from January 2016 to August 2016. The TGMUGH is a tertiary referral hospital with 2,468 beds located in Tianjin - a metropolis with more than 15 million population - in Northern China. Out- and inpatients were referred to the colonoscopy for any reason, including diagnosis, screening, surveillance as well as endoscopic treatment. All investigative protocols were approved by the ethic committee of TJMUGH; the clinical procedures were carried out in accordance with the Declaration of Helsinki.
The exclusion criteria were as follows: (1) subjects with insufficient data for analysis or refused to participate; (2) patients with a prior history of inflammatory bowel disease; (3) or a previous history of colectomy; (4) incomplete colonoscopy procedure; (5) poor bowel preparation. All participants were evaluated before enrollment. If an individual underwent more than one colonoscopies during the study period, all procedures were regarded as one examination.
Colonoscopy procedure
All colonoscopies were performed by expert endoscopists at our endoscopy center. An electronic colonoscopy (CF-Q260, Olympus Optical Co., Tokyo, Japan) was used during the study period. Bowel preparation was achieved by using 2 L of polyethylene glycol the day before examination. The bowel preparation was rated as excellent, good, fair, or poor according to the degree of visibility of intestinal mucosa devoid of stool.
We regarded complete colonoscopy as cecal intubation followed by identification of ileo-cecal valve. The location of diverticulosis was defined as right-sided (involving the cecum, ascending colon, or transverse colon); left-sided (involving the splenic flexure, descending colon, or sigmoid colon); or bilateral (involving the entire colon). An instruction was sent to each endoscopist, which covering the purpose of our current study (learn more about the risk factors of uncomplicated colonic diverticulosis). In addition, our research staff were present during the examination when the gastroenterologists detected any diverticulum. The distribution, number and type of diverticula were documented in our digital database by the endoscopists.
Baseline characteristics, risk factors and measurements
The current study was conducted by two well trained research staff (FY and YZ) in our department. After informed consent, all participants were asked to complete a detailed questionnaire through face-to-face interviews on the same day prior to colonoscopic examination or endoscopic treatment. The following information was collected in detail: demographics (including sex, age, educational level, body mass index [BMI]), and lifestyle factors (including exercise habit [<3 or ≥3 per week], red meat consuming [<100/d or ≥100/d], smoking index [defined as the duration of smoking years multiplied by the number of cigarettes per day, then was categorized into nonsmoker, <400 and ≥400], and current alcohol intake [defined as non-drinker, light/moderate drinker consuming 1–350 g of alcohol and heavy drinker at least 351 g per week]). Patients were also evaluated about comorbidities on account of sex differences regarding distinct spectrum of diseases. Notably, we evaluated the presence or absence of hypertension, diabetes mellitus, coronary heart disease, colonic polyps, upper gastrointestinal diseases (chronic/atrophic gastritis, reflux esophagitis and peptic ulcer), hepato-biliary diseases (cholelithiasis and fatty liver disease), dyslipidemia, thyroid diseases and rheumatologic diseases (rheumatoid arthritis and gout), etc. Prevalent hypertension, diabetes mellitus and dyslipidemia were confirmed in terms of self-reported diagnosis or taking specific medications.
Estimated regular use of prescription were NSAIDs, corticosteroid (prednisolone, methylprednisolone and dexamethasone), PPIs (esomeprazole, rabeprazole, omeprazole and lansoprazole), mucosal protective drugs (rebamipide, hydrotalcite and gefarnate), antihypertension drugs and hypoglycemic medications. We regarded regular use as continuously oral administration for at least 3 months (comprising NSAIDs, corticosteroid, PPIs and mucosal protective drugs) or 6 months (comprising antihypertension drugs and hypoglycemic medications) prior to our interview. We only took account of official prescription at our clinic or other certificated medical institution/pharmacy. Since it is difficult to definitely delineate, the usage of OTC, herbals and dietary supplementary were not recorded.
Statistical analysis
Continuous data were demonstrated as mean (standard deviation) and categorical variables as counts or frequencies. In univariate analysis between binary groups according to the presence of diverticulosis, an independent student’s t test or the method of Mann-Whitney test was employed. Likewise, we compared categorical variables using Pearson’s χ2 or Fisher’s exact statistic to identify differences in the baseline characteristics. Age and BMI were evaluated by continuous variables. The risk factors for predicting the presence of diverticulosis were determined individually for men and women using a stepwise binary logistic regression model. We demonstrated odds ratio (OR) and 95% confidence interval (CI) for each independent variable. A P value < 0.05 was regarded as statistically significant and all tests were two-sided. The statistical analyses were performed with SPSS 22.0 (IBM, New York NY, USA) or STATA 12.0 (Stata Corporation, College Station Texas, USA).
Availability of data and materials
Available under request.
Consent for publication
The participant gave informed consent before taking part in this study. The samples were de-identified.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and was approved by Ethics Committee of Tianjin Medical University General Hospital.
Electronic supplementary material
Table S1 Comparison of characteristics in whole study population
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81500397 to CS and No. 81503019 to JZ).
Author Contributions
F.Y., Y.Z., K.J. and C.S. carried out the studies, conducted data analysis and drafted the manuscript. F.Y., Y.Z., X.J., Z.S., Y.W., L.L., J.Z., H.L., J.Z. and B.W. participated in data collection. All of the authors read and approved the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Fang Yang and Yanmin Zheng contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-017-18517-1.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kui Jiang, Email: kjiang@tmu.edu.cn.
Chao Sun, Email: chaosun@tmu.edu.cn.
References
- 1.Li B, et al. Sex Differences in Outcomes and Associated Risk Factors After Acute Ischemic Stroke in Elderly Patients: A Prospective Follow-up Study. J Stroke Cerebrovasc Dis. 2015;24:2277–2284. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Faucheron JL, Roblin X, Bichard P, Heluwaert F. The prevalence of right-sided colonic diverticulosis and diverticular haemorrhage. Colorectal Dis. 2013;15:e266–270. doi: 10.1111/codi.12137. [DOI] [PubMed] [Google Scholar]
- 3.Peery AF, et al. A high-fiber diet does not protect against asymptomatic diverticulosis. Gastroenterology. 2012;142:266–272 e261. doi: 10.1053/j.gastro.2011.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rezapour, M., Ali, S. & Stollman, N. Diverticular Disease: An Update on Pathogenesis and Management. Gut Liver. (2017). [DOI] [PMC free article] [PubMed]
- 5.Yazici C, et al. Breath Methane Levels Are Increased Among Patients with Diverticulosis. Dig Dis Sci. 2016;61:2648–2654. doi: 10.1007/s10620-016-4174-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barbara G, et al. Gut microbiota, metabolome and immune signatures in patients with uncomplicated diverticular disease. Gut. 2017;66:1252–1261. doi: 10.1136/gutjnl-2016-312377. [DOI] [PubMed] [Google Scholar]
- 7.Bolnick DI, et al. Individual diet has sex-dependent effects on vertebrate gut microbiota. Nat Commun. 2014;5:4500. doi: 10.1038/ncomms5500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamamichi N, et al. Trend and risk factors of diverticulosis in Japan: age, gender, and lifestyle/metabolic-related factors may cooperatively affect on the colorectal diverticula formation. PLoS One. 2015;10:e0123688. doi: 10.1371/journal.pone.0123688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dore MP, et al. Risk factors associated with colonic diverticulosis among patients from a defined geographic area. Tech Coloproctol. 2016;20:177–183. doi: 10.1007/s10151-015-1401-7. [DOI] [PubMed] [Google Scholar]
- 10.Nagata N, et al. Increase in colonic diverticulosis and diverticular hemorrhage in an aging society: lessons from a 9-year colonoscopic study of 28,192 patients in Japan. Int J Colorectal Dis. 2014;29:379–385. doi: 10.1007/s00384-013-1808-4. [DOI] [PubMed] [Google Scholar]
- 11.Fong SS, Tan EY, Foo A, Sim R, Cheong DM. The changing trend of diverticular disease in a developing nation. Colorectal Dis. 2011;13:312–316. doi: 10.1111/j.1463-1318.2009.02121.x. [DOI] [PubMed] [Google Scholar]
- 12.Lohsiriwat V, Suthikeeree W. Pattern and distribution of colonic diverticulosis: analysis of 2877 barium enemas in Thailand. World J Gastroenterol. 2013;19:8709–8713. doi: 10.3748/wjg.v19.i46.8709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang FW, et al. Prevalence and risk factors of asymptomatic colorectal diverticulosis in Taiwan. BMC Gastroenterol. 2015;15:40. doi: 10.1186/s12876-015-0267-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong W, et al. Prevalence of colonic diverticulosis in mainland China from 2004 to 2014. Sci Rep. 2016;6:26237. doi: 10.1038/srep26237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He Y, et al. Dietary patterns as compared with physical activity in relation to metabolic syndrome among Chinese adults. Nutr Metab Cardiovasc Dis. 2013;23:920–928. doi: 10.1016/j.numecd.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 16.McConnell EJ, Tessier DJ, Wolff BG. Population-based incidence of complicated diverticular disease of the sigmoid colon based on gender and age. Dis Colon Rectum. 2003;46:1110–1114. doi: 10.1007/s10350-004-7288-4. [DOI] [PubMed] [Google Scholar]
- 17.Commane DM, Arasaradnam RP, Mills S, Mathers JC, Bradburn M. Diet, ageing and genetic factors in the pathogenesis of diverticular disease. World J Gastroenterol. 2009;15:2479–2488. doi: 10.3748/wjg.15.2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakaji S, et al. Comparison of etiology of right-sided diverticula in Japan with that of left-sided diverticula in the West. Int J Colorectal Dis. 2002;17:365–373. doi: 10.1007/s00384-002-0403-x. [DOI] [PubMed] [Google Scholar]
- 19.Reichert MC, Lammert F. The genetic epidemiology of diverticulosis and diverticular disease: Emerging evidence. United European Gastroenterol J. 2015;3:409–418. doi: 10.1177/2050640615576676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nagata N, et al. Alcohol and smoking affect risk of uncomplicated colonic diverticulosis in Japan. PLoS One. 2013;8:e81137. doi: 10.1371/journal.pone.0081137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Razik R, Nguyen GC. Diverticular disease: changing epidemiology and management. Drugs Aging. 2015;32:349–360. doi: 10.1007/s40266-015-0260-2. [DOI] [PubMed] [Google Scholar]
- 22.Myasoedova E, Matteson EL, Talley NJ, Crowson CS. Increased incidence and impact of upper and lower gastrointestinal events in patients with rheumatoid arthritis in Olmsted County, Minnesota: a longitudinal population-based study. J Rheumatol. 2012;39:1355–1362. doi: 10.3899/jrheum.111311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.He J, et al. Dietary intake and risk of rheumatoid arthritis-a cross section multicenter study. Clin Rheumatol. 2016;35:2901–2908. doi: 10.1007/s10067-016-3383-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pu Y, et al. Geographic and sex difference in the distribution of intracranial atherosclerosis in China. Stroke. 2013;44:2109–2114. doi: 10.1161/STROKEAHA.113.001522. [DOI] [PubMed] [Google Scholar]
- 25.Ly, N. P., Litonjua, A., Gold, D. R. & Celedon, J. C. Gut microbiota, probiotics, and vitamin D: interrelated exposures influencing allergy, asthma, and obesity? J Allergy Clin Immunol. 127, 1087–1094; quiz 1095–1086 (2011). [DOI] [PMC free article] [PubMed]
- 26.Ley RE, et al. Obesity alters gut microbial ecology. Proc Natl Acad Sci USA. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turnbaugh PJ, Backhed F, Fulton L, Gordon JI. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe. 2008;3:213–223. doi: 10.1016/j.chom.2008.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong ER, et al. Diverticular Disease and Colorectal Neoplasms: Association between Left Sided Diverticular Disease with Colorectal Cancers and Right Sided with Colonic Polyps. Asian Pac J Cancer Prev. 2016;17:2401–2405. [PubMed] [Google Scholar]
- 29.Peery AF, Martin CF, Levinson SE, Sandler RS. Colonic Diverticula Are Not Associated With an Increased Risk of Colorectal Adenomas. Am J Gastroenterol. 2015;110:1694–1697. doi: 10.1038/ajg.2015.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gravante G, Yahia S. Medical influences, surgical outcomes: role of common medications on the risk of perforation from untreated diverticular disease. World J Gastroenterol. 2013;19:5947–5952. doi: 10.3748/wjg.v19.i36.5947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sharara AI, et al. Alcohol consumption is a risk factor for colonic diverticulosis. J Clin Gastroenterol. 2013;47:420–425. doi: 10.1097/MCG.0b013e31826be847. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Comparison of characteristics in whole study population
Data Availability Statement
Available under request.