Abstract
Background:
This study compares participant’ sretention in three phases of smoking cessation interventions, one provided in a health clinic and the subsequent two in community-based settings.
Methods:
Smoking cessation interventions were conducted in three phases from 2008 to 2015 in two underserved urban communities with low socioeconomic profiles and high rates of smoking (n = 951). Phase I was conducted in a clinic; Phases II and III were conducted in community venues. In Phases II and III, incremental changes were made based on lessons learned from the previous phases. Retention (attending six or more sessions) was the primary predictor of cessation and was analyzed while controlling for associated factors including age, gender, race, employment, education, and nicotine dependence.
Results:
Retention increased substantially over the three phases, with rates for attending six or more sessions of 13.8%, 51.9%, and 67.9% in Phases I, II, and III, respectively. Retention was significantly higher in community settings than in the clinic setting (adjusted odds ratio [OR] = 6.7; 95% confidence intervals [CI] = 4.6, 9.8). In addition to the intervention in community venues, predictors of retention included age and unemployment. Higher retention was significantly associated with higher quit rates (adjusted OR = 2.4; 95% CI = 1.5, 3.8).
Conclusions:
Conducting the intervention in community settings using trained peer motivators rather than health-care providers resulted in significantly higher retention and smoking cessation rates. This was due in part to the ability to tailor cessation classes in the community for specific populations and improving the quality of the intervention based on feedback from participants and community partners.
Keywords: Community-based participatory research, retention, smoking cessation, underserved populations
Introduction
Despite substantial declines in smoking rates over the past few decades, the 2014 US Surgeon General's Report estimated that more than 42 million Americans smoke tobacco regularly. Smoking causes coronary heart disease, cancer, complications in pregnancy, chronic obstructive pulmonary disease, and many other chronic illnesses and is the leading cause of premature deaths.[1,2] Therefore, smoking prevention and cessation are among the highest priorities for public health in the United States.
Low-income and underserved populations in the US continue to use tobacco at disproportionately higher rates than their middle-class counterparts.[3,4] Persons with less education and lower incomes smoke at higher rates, start smoking at younger ages, smoke more cigarettes per day, and are exposed to more secondhand smoke than persons of higher socioeconomic status (SES).[5]
In Baltimore City, 62.9% of the population is African American and the median household income is $42,241 compared to $74,551 for the rest of Maryland and $53,889 for the rest of the US. Of the total population in Baltimore City, 22.7% live in poverty, compared to 9.7% across the state of Maryland and 13.5% in the rest of US.[6] At 21.2%, the smoking prevalence in Baltimore City is higher than the national average (18.8%).[7,8]
Effective smoking cessation interventions involve different sectors and stakeholders and typically require combinations of pharmacotherapy, counseling, and support groups.[9] A major impediment to the success of these programs, however, is high attrition rates.[7] In fact, retention in treatment is one of the main predictors of success in behavior change programs that address smoking and other drugs.[7] The setting for the intervention, the type of provider, and specific incentives offered to participants have all been shown related to retention.[10,11]
From 2008 to 2015, researchers from Morgan State University worked with community partners to plan, implement, and evaluate smoking cessation interventions based on a community-based participatory research (CBPR) approach in two low-income neighborhoods in Baltimore City, Maryland. This paper describes the development and implementation of these interventions across three phases that each built on the lessons of its predecessors. Retention rates are compared, predictors of success are identified, and the benefits of moving the intervention from a health clinic to community-based venues are discussed.
Methods
Background and setting
Our smoking, cessation intervention is called Communities Engaged and Advocating for a Smoke-free Environment (CEASE). The CEASE intervention is based on a long-standing CBPR collaboration between tobacco researchers at Morgan State University, a minority-serving institution, and partners in two neighboring communities in Baltimore with high smoking rates and low SES profiles.[8] In the targeted communities, 75% of the population is African American, and more than 40% of households have incomes under $25,000 a year. When the study began, nearly 70% of the men and 50% of the women over age 18 in these communities reported smoking regularly.[12]
CEASE benefited from a strong and enduring community–campus partnership that began in 2002 and is overseen by a Community Action Board (CAB). The board included community residents, leaders, and representatives of schools and faith-based organizations. The application for funding this study was jointly prepared by the university and its CAB partner. Decisions are made by consensus and challenges are addressed through the collective wisdom of the CAB.
Intervention design, participants, and recruitment
The CEASE intervention was conducted in three phases; each phase informed the planning and development of the next one. A total of 965 participants were enrolled in the three phases of smoking cessation programs from 2008 to 2015. Data from 951 participants with complete information on the number of classes attended (retention) were used for this analysis.
Phase I was a randomized controlled trial with two arms conducted in a community health center in Baltimore. Participants (n = 400) were recruited from the patient population of the health center through flyers and personal referrals. Eligibility criteria included: Being 18 years and older; being a current smoker (defined as smoking at least three cigarettes per day in the past week); having the mental capacity; and the ability to understand the English consent forms. Participants who were recruited but did not attend any of the sessions were excluded from the study.
Phase I participants were randomly assigned to receive either individual counseling from a medical doctor or group counseling facilitated by a nurse or social worker. Because cessation rates were similar in both counseling situations, subsequent interventions relied on the more cost-effective group approach. It was also discovered in Phase I that participants preferred nonclinical venues, so subsequent interventions were based on a variety of community settings.
Phase II (n = 389) was a controlled trial in which laypersons who had overcome their own tobacco habits and who lived in the neighborhoods they served were trained as peer motivators to deliver the intervention. Phase II compared two group counseling methods with different incentives – monetary only versus monetary plus points and certificates for achieving hallmarks. Results from Phase II led to a more enhanced Phase III (n = 162), which was a dissemination and implementation trial using a modified version of the Phase II curriculum. In Phase III, the intervention was implemented in an expanded number and variety of community settings.
In Phases II and III, participants were recruited from the community through word of mouth, personal referrals, flyers, community surveys, and collaborations with community partners. Participants for the final qualitative evaluation were recruited from the list of individuals who had completed the cessation program.
Smoking cessation curriculum
In Phase I, the American Cancer Society's Freshstart® smoking cessation program was used to guide both individual and group counseling programs.[13] Later, the Freshstart® curriculum was expanded in collaboration with the CAB, from its original 4-week intervention to a 12-week program divided into three modules: preparation and motivation (2 weeks); quit smoking (4 weeks); and staying quit (6 weeks).
Selection criteria for peer motivators included having at least a high school education and being smoke free for at least 1 year. A total of 10 peer motivators were paid for their time to deliver the interventions in Phases II and III. All peer motivators attended a 2-day training on the curriculum, class facilitation, documenting, and reporting activities. They were responsible for recruiting smokers as well as facilitating the sessions.
The Phase III curriculum retained the basic components of Phase II (i.e., peer-led, community-based group counseling) but included more diversified tools and activities and implemented the intervention in different settings. In Phase III, a toolbox of activities was made available from evidence-based resources informed by peer motivators’ feedback. The toolbox allowed specific components of the classes to be tailored to individual participants’ needs and levels of readiness. In this phase, relapse prevention sessions were also diversified (e.g., tracked offerings included physical activity, healthy diet, and relationship management) so that participants could choose activities that were most interesting and appropriate.
Medications and incentives
All participants were entitled to nicotine replacement therapy (NRT) during the course of the intervention. In Phase I, participants could get prescription smoking cessation medications free of charge after an evaluation by a health-care professional. In Phases II and III, participants were offered only over-the-counter NRT including gum, patches, and lozenges.
In Phase I, gift cards were given as incentives for participating in the program and achieving specific milestones (e.g., setting a quit day, staying quit for 1 week, 1 month, and 6 months). In Phase II, gift cards were changed to cash and a point system was added to allow participants to earn additional rewards for attendance, completing postsession questionnaires, and achieving milestones. In Phase III, cash was also used to reward attendance at smoking cessation and motivational enhancement classes and participation in follow-up surveys.
Developing the intervention
At each stage of the intervention, quantitative and qualitative findings from the previous phase as well as continuous feedback and communication with all stakeholders (including members of the CAB, site coordinators who partnered the program with local venues, peer motivators, and participants) led to improvements that were incorporated into subsequent phases. At the end of Phase I, health providers at the community health center were interviewed and focus groups were held for participants to evaluate the intervention. Since cessation rates for those who received individual counseling did not differ from those who participated in group counseling, subsequent phases included only the more cost-effective group counseling approach. Other findings from the Phase I qualitative evaluation suggested making services easier to access, increasing the cultural competency of the intervention, and changing the incentives used.
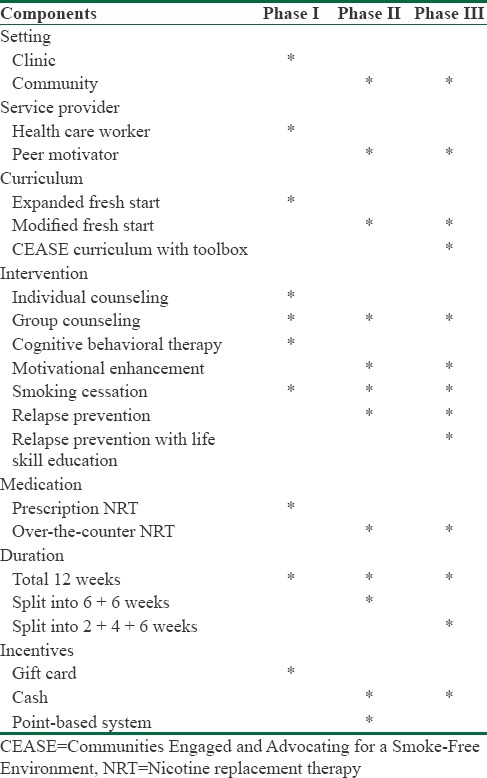
At the end of Phase II, the intervention was evaluated again by engaging all stakeholders and reviewing the results. Feedback included ways to improve motivation to initiate the quitting process and to stay quit after the intervention. These findings then informed changes to Phase III that included motivational enhancement and relapse prevention modules. Feedback from Phase III has further informed a fourth phase which is currently ongoing. Table 1 shows a summary of differences and similarities for the three phases of this intervention.
Table 1.
Components of the interventions in Phases I, II, and III
Qualitative methodology
Throughout Phases I and II, a total of 23 individual in-depth interviews (IDIs) and 11 focus group discussions (FGD) were conducted, involving a total of 84 persons. IDI participants included peer motivators and members of the advisory board. FGD participants were recruited by phone calls from peer motivators and flyers posted throughout the community. They met in three separate groups – those who had quit smoking, those who did not quit, and those who dropped out of the program. FGD participants received financial incentives. The IDIs were audio recorded and transcribed by a trained researcher. The FDGs were facilitated, recorded, and transcribed shortly after each session by two individuals from the research team with prior training in qualitative research. Participants were asked a series of questions about their overall experience with the smoking cessation intervention, their perceptions of the program's strengths and weaknesses, and their recommendations for improvement.
Data collection and analysis
A baseline questionnaire was used to collect information on demographics; smoking history; barriers to quitting (e.g., concerns about weight gain, stress, social support, child care, time to attend sessions, ability to afford treatment, etc.); and stages of change defined by criteria from the transtheoretical model.[14,15] At the end of each cessation or relapse prevention class, participants completed an exit form that recorded information on smoking status, barriers to quitting, aids for success, and other variables. Follow-up questionnaires similar to the exit forms captured information at a later date on smoking cessation and barriers to quitting.
To gather and record qualitative data about participants’ experience with CEASE, semi-structured questionnaires and guides were developed for FGD and key informant interviews. The discussion guides helped researchers probe for detailed information about the curriculum, program logistics, the impact of the intervention, what motivated participants to quit, barriers or challenges to quitting, and recommendations for improvement.
The primary outcome of interest for this study was participant retention, defined as attending six or more of the 12 total smoking cessation and relapse prevention classes offered in each phase. The cutoff point was based on a minimum expectation of attending at least six sessions to cover the quit modules of the curriculum; additional sessions were available to help participants stay quit. Participants were classified as “not retained” if they attended fewer than six classes. Data on sociodemographic characteristics including race, age, gender, employment status, and educational attainment were also analyzed. Employment status and educational attainment were used as measures of SES. The Fagerstrom Test for Nicotine Dependence was used at baseline. Fagerstrom is a validated, six-question measure for self-reporting nicotine dependence, with scores ranging from 0 (no dependence) to 10 (highest dependence).[16]
The treatment effect for each study arm was based on self-reported smoking abstinence verified by expired-air carbon monoxide levels.[17] Smoking status was assessed at completion of the smoking cessation sessions. Based on their smoking status 12 weeks after the intervention, participants were categorized as “quit” or “didn’t quit.”
Statistical analysis
The data were entered into EpiData version 3.1 (EpiData Associations, Odense, Denmark)[18] without personal identifiers and exported into STATA version 11 (College Station, Texas, TX, USA)[19] for cleaning and analysis. A descriptive univariate analysis was conducted to review each variable and summarize demographic information. A bivariate analysis was conducted to compare retention with potential predictor variables. In the bivariate analysis, Chi-square tests of nicotine independence were used for categorical variables including phase, gender, race, education, and employment; the results are presented as numbers with corresponding proportions. The Student's t-test was used for continuous variables, including age and Fagerstrom scores; these results are presented as means with standard deviations. A multivariable analysis was conducted using logistic regression to test the association between intervention setting and retention. Retention was dichotomized into “retained” (i.e., attending six or more sessions) and “not retained” (i.e., attending fewer than six sessions). The association between intervention setting and program retention was adjusted for gender, age, race, education, employment, and Fagerstrom score, to calculate adjusted odds ratios (ORs) and 95% confidence intervals (CI). For this model, age and Fagerstrom scores were also dichotomized as above and below median levels. When a multivariable linear regression model was applied with retention maintained as a continuous variable, the results did not differ from the results of the logistic regression.
A multivariable logistic regression model was used to compare retention in Phase I (clinic setting) with Phases II and III combined (community settings). A second multivariable logistic regression model was used to compare retention in Phase II with Phase III. OR and 95% CI were calculated after adjusting for gender, age, race, education, employment, and Fagerstrom score. Associations between retention and quit rates were calculated using a bivariate logistic regression. The multivariable logistic regression model of the odds of quitting as it relates to other variables is presented in another paper.[20] P < 0.05 was considered statistically significant.
The qualitative data analysis was conducted using Atlas. ti 6.1.[21] A codebook was developed by two trained research assistants and structured according to objectives of the assessment. The FGD recordings were transcribed by CEASE researchers and each transcript was coded separately by two researchers, then cross-checked to verify analysis and form a consensus of the coding. The IDIs and FGDs from former CEASE participants, peer motivators, and site coordinators were analyzed separately for emergent themes.
Ethical considerations
The proposals for each phase of this intervention were approved by Morgan State University's Institutional Review Board and the CEASE CAB. Every participant signed an informed consent form before being enrolled in the study.
Results
Quantitative
Data from a total of 951 individuals (400, 389, and 162 individuals from Phases I, II, and III, respectively) were used for this analysis. The total population consisted of 60.6% males, with a mean age of 46.5 years (standard deviation = 10.7 years). African Americans comprised 73.5% of the total study population; 37.4% of participants had not graduated from high school; and 71.6% of participants were unemployed at the time of the intervention. The mean Fagerstrom score for all participants was 4.1 (standard deviation = 2.6). Table 2a shows the distribution of these factors across the three phases.
Table 2a.
Comparing variables across phases
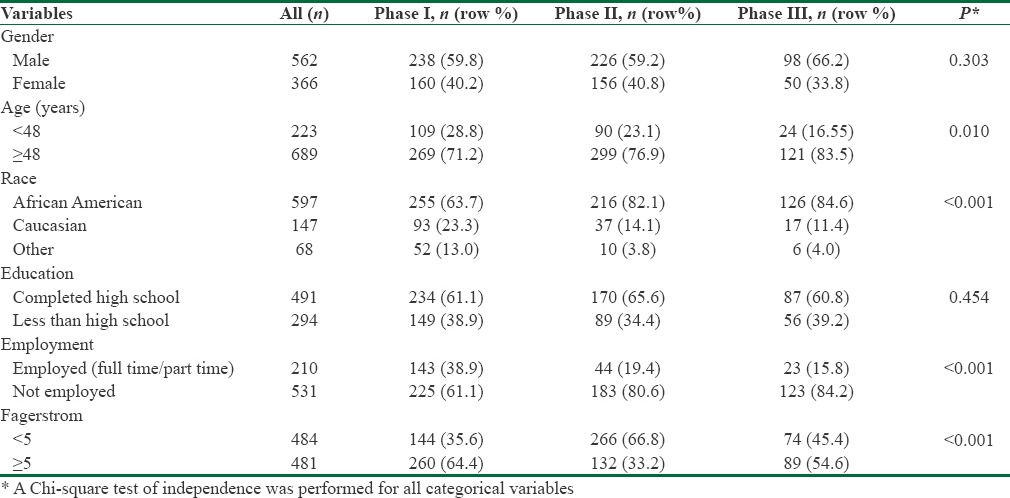
Table 2b shows a bivariate analysis of retention (i.e., attending six or more classes in each phase) and potential predictors. Retention increased significantly from 13.8% in Phase I to 51.9% in Phase II, and 67.9% in Phase III.
Table 2b.
Predictors of retention in bivariate analyses
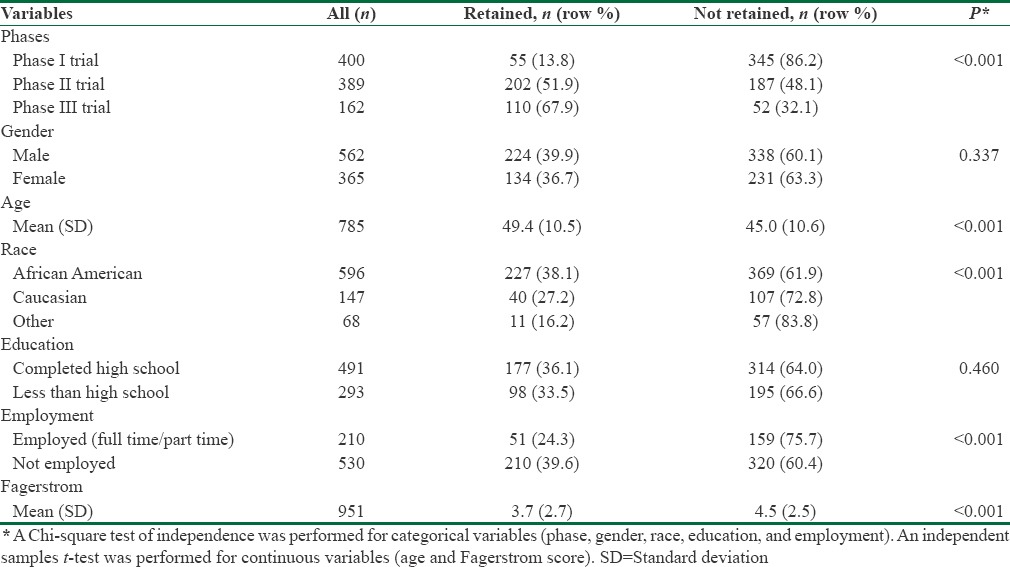
In this analysis, being older, African American, unemployed, and having a lower level of nicotine dependence were all associated with higher retention rates. Gender and education were not significantly associated with retention.
Table 3 shows the associations between retention and attending classes in a community setting (Phases II and III) versus a clinical setting (Phase I). Community settings were associated with significantly higher retention, with an OR (95% CI) of 8.2 (5.9–11.4). After adjusting for gender and age, this association remained strong and statistically significant with an OR (95% CI) of 6.9 (4.8–9.8). After further adjustments for race, education, employment, and Fagerstrom score, the positive association between community setting and retention remained strong and statistically significant with an OR (95% CI) of 6.7 (4.6–9.8). After these adjustments, being older and being unemployed remained significantly associated with higher retention while race and Fagerstrom score lost their statistical significance.
Table 3.
Predictors of retention in multivariate logistic regression analyses
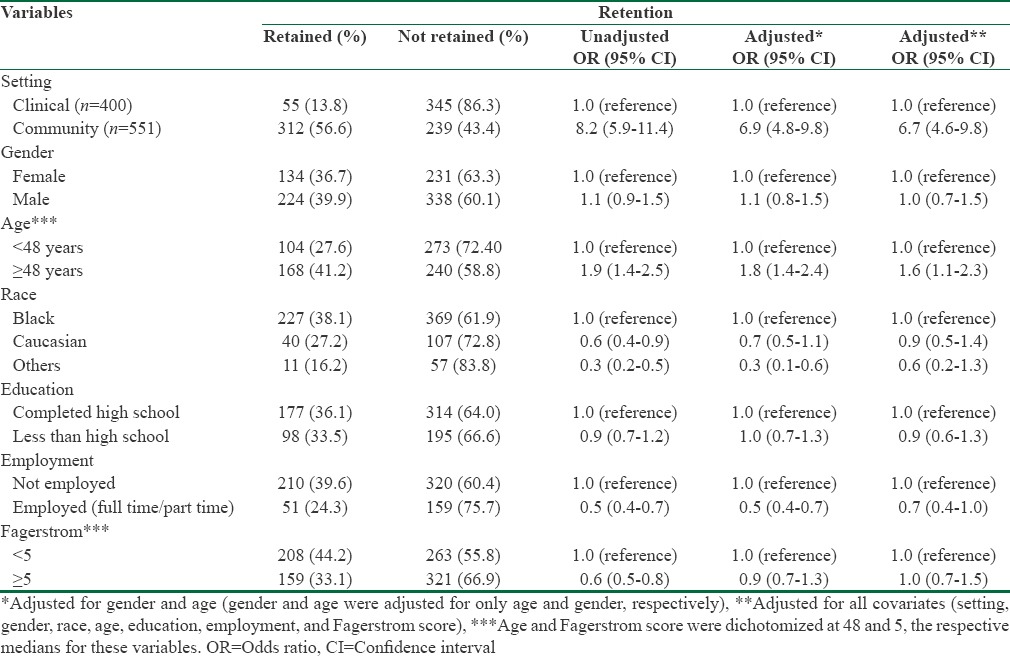
Table 4 shows differences in retention across the three phases of intervention. Phases II and III were associated with substantial improvements in retention rates compared to Phase I, with statistically significant adjusted ORs of 4.9 (3.2–7.3) and 12.0 (7.3–19.5), respectively. Retention in Phase III was also significantly higher when compared with Phase II (both were in community settings), with an adjusted OR (95% CI) of 2.5 (1.6–3.9).
Table 4.
Comparing retention in Phases I, II, and III and between Phases II and III (both in community settings) using logistic regression analyses
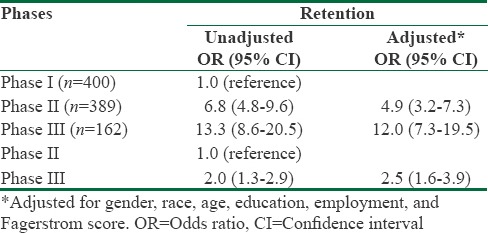
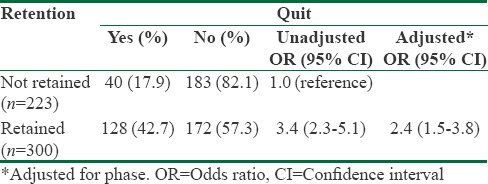
Table 5 shows a bivariate logistic regression of quit rates and retention. A total of 523 participants (55%) had complete follow-up data including information about their class attendance and smoking status. The overall quit rate among all participants (n = 951) was 18%. In Phases I, II, and III, the quit rates were 9.4%, 21.1%, and 30.1%, respectively (data not shown in Table 5). In unadjusted analyses, retention (defined as attending six or more sessions) was significantly associated with a higher quit rate, with an OR (95% CI) of 3.4 (2.3–5.1). In analyses adjusted for phase, the results remained statistically significant, with an OR (95% CI) of 2.4 (1.5–3.8).
Table 5.
Logistic regression analysis of quit rate associated with retention rate
Qualitative
In Phase I, IDIs and FGDs were held with 30 CEASE participants, 3 clinical staff and 9 CAB members. In Phase II, the IDIs and FGDs included 31 former CEASE participants, 7 peer motivators, and 4 site coordinators (i.e., community partners related to the sites used). The main themes that emerged from Phase I and II assessments included: reasons for dropping out; ease of accessing services; participant–provider relationships; motivation to quit; barriers to quitting; and flexibility of the curriculum.
Phase I participants reported concerns about accessing the clinic, the high turnover of health providers who led the classes, and a general sense of discomfort in the clinical environment. For example, one participant who had dropped out of the classes said that “smoking is not a disease. It's a nasty behavior, I agree. But I don’t agree to treating it like a disease in a clinic.” An African American woman explained, “I am not very far from here. But I don’t have a car and I have two small kids. Without a ride and child care it was hard for me to go to those classes every week. In addition, every time that I went there was a new nurse running the class.”
Since CAB members and many of the participants viewed smoking as a behavioral problem rather than a clinical disease, they thought that the intervention would be better managed in the community. However, clinicians expressed concerns about providing care outside the clinic setting due to logistical issues, Health Insurance Portability and Accountability Act requirements, and budgetary challenges. Therefore, the Phase II intervention was designed to be conducted in community venues and facilitated by trained peers rather than clinical staff.
The goals of the qualitative evaluation in Phase II included increasing interaction with participating community sites, strengthening the curriculum, and improving the quality of services. Qualitative findings reflected increased satisfaction with the new version of the program. The curriculum was rated as better structured than the original version, and most participants reported better bonding with their peer motivators. However, many participants also expressed a desire for more diversified teaching tools, including audiovisual materials. All peer motivators believed that having these additional tools located at a central site would increase coordination and the overall quality of the program. As one participant put it: “The film that (a Peer Motivator) showed us helped. Seeing the inside of the organs all messed up, stuff like that. That helped me pretty good.”
Peer motivators liked the flexibility of the improved curriculum, but they also wanted greater clarity and more subjects for classes. As one peer motivator stated: “I actually think it's a really decent foundation of what the participants are looking for, but for me it's more of a bare bones. It's not complete.” Site coordinators reported some relationship and communication challenges with program participants and peer motivators. One site coordinator said: “I had some interaction. Which was very like choppy and chaotic. It just seemed like a lot of miscommunication. A lot of ‘he said she said.’ It was just very chaotic.”
The feedback from Phase II was used to further improve the curriculum and guide the development of Phase III.
Discussion
Findings from this research reveal significant increases in retention from Phases I to Phases II and III. The increases were associated with providing the services in community settings rather than in a health clinic, using peer motivators rather than health-care providers to deliver the services, and enhancing the quality of the curriculum based on lessons learned in previous phases.[22] These are important factors because retention is a key predictor of success in almost every smoking cessation program.[23] Historically, it has been difficult to recruit and retain African Americans and members of other minority groups in research studies.[24] Guidance from the CEASE CAB is also very valuable in adjusting the intervention to increase outreach and recruitment of those most in need of smoking cessation assistance, as well as improving the cultural and linguistic appropriateness of the intervention.
The decision to move from the clinic to various community-based settings was an important factor in eliminating barriers to participation and retention.[25] Qualitative findings from Phase I showed that participants were not comfortable coming to the clinic for cessation classes. At the same time, medical personnel reported major impediments to their providing services outside the clinic. Moving to community-based venues increased access for participants by decreasing the distance they had to travel and the transportation barriers they faced, including cost.[10,24] Participants reported being more comfortable in familiar surroundings than in a clinical setting where the intervention felt more like “treatment.” As one Phase II participant explained it, “Seems like when you get around people that are struggling with the same thing it's kind of a big help, well to me.” Another Phase II participant said, “I was surprised at how many people were sitting at the table willing to learn stuff about themselves, to find out what's going on with their health. That was a good experience. The group, in the whole, was a blessing and supportive for me.” Other studies have also shown the value of community settings in familiar environments[22,26] where participants report feeling a greater sense of normalcy and control.
Phases II and III also replaced the medical personnel who had led the clinic-based Phase I classes with trained peer motivators who live in the neighborhoods they serve. African Americans and members of other minority groups have reported a mistrust of and perceived distance from government and academic institutions, and this has been a barrier to recruitment and retention.[26] Consistent with other research, participants in CEASE community-based classes were more open and forthcoming with their peer motivators than participants had been with health-care providers. One participant reported: “And I thank God, for Ms. (Peer Motivator) because whether they know it or not, I do not talk too much to people, but when I got in the group I started to talk about this. I cried a little bit, because I lost my children. Cried a little bit. But they do not know how good they helped me and I thank god each and every day for ‘me’.”
The CBPR approach taken by CEASE identified and supported meaningful incremental improvements in the program based on input from participants and the CAB.[26] Including community members as key decision-makers and incorporating bi-directional feedback increased participation and retention.[10] In addition to moving from the clinic to community settings and using peer motivators instead of health-care providers, progressive changes suggested by the CAB and participants included amending the curriculum topics, going from open to closed groups, and changing the incentives from gift cards to cash. The improvements in retention and cessation that followed illustrate the value of community involvement in CBPR research and interventions.[27]
Bivariate analyses showed that, in addition to intervention setting, being older than 48 years, being Black, not being employed, and having less nicotine dependence (i.e., lower Fagerstrom scores) were significantly associated with higher retention. However, after adjusting for all other variables, the multivariable analysis showed that only age over 48 and being unemployed remained significantly associated with increased retention. Previous research has produced similar results.[28] A study of retention in a smoking cessation program for Latinos in the US identified unemployment as one of the predictors of program completion. Another study found that younger age predicted more no-shows in a smoking cessation program for African Americans.[29] It is possible that older persons perceive greater risks associated with smoking than do younger persons. The limited relationship between unemployment and retention could be the result of having more time to attend classes and greater need for the monetary incentives. Other studies have identified additional predictors of retention that were not statistically significant in this research. Women have higher dropout rates than men from smoking cessation interventions. Higher dropout is also related to having greater nicotine dependence, poorer motivation, time conflicts, health concerns, being single, using other substances, and having less than a high school education.[11,30] Conversely, a study of minorities showed that reduced dropout from the program intervention was related to having cardiovascular problems and generally poor health, lower income, and increased confidence in the ability to stop smoking.[31]
The current study was limited by the unavailability of some information. Data on some known and potential predictors of retention, including anxiety, alcohol, and substance abuse, were only collected in Phases II and III of this research and therefore could not be compared across all three phases. Some data were also missing for some variables that were tracked, but these omissions did not seem to limit the findings that emerged.
The strengths of this research include the fairly large sample size and the fact that the study was conducted in an underserved community that had a long-standing relationship with the researchers. Another strength is that all three phases of the intervention were designed and implemented by the same collaborative of researchers and community partners.
Conclusions
This study showed that moving a smoking cessation intervention out of a clinic and into community settings, using trained peers to facilitate the cessation process, and making incremental changes in the intervention based on lessons learned and feedback from participants and the community significantly increased participants’ retention in the program and improved quit rates. Being older and unemployed were also significantly associated with increased retention. Other factors, including gender, race, education, and Fagerstrom scores, were not found to be significantly related to retention.
The authors of this study also recommend that to increase retention and ensure completion of smoking cessation programs, the interventions be tailored to the specific populations they serve. Input from the target market for the intervention should be sought at the outset and incorporated throughout the process.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This research received financial support from the National Institute on Minority Health and Health Disparities (grants MD000217 and MD002803), the National Institute on Drug Abuse (Grants DA012390 and DA019805), National Institute of General Medical Sciences (grant UL1GM118973), and Pfizer Inc.
In addition, we acknowledge members of the CEASE partnership including the members of the CAB, peer motivators, the staff and administrators of People's Community Health Center, and other community partners and organizations that supported our planning and hosted CEASE programs.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion d. Smoking and Tobacco Use; Tobacco Control State Highlights. Maryland: 2010. [Last accessed on 2016 Feb 02]. Available from: http://www.cdc.gov/tobacco/data_statistics/state_data/state_highlights/2010/states/maryland . [Google Scholar]
- 2.Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Centers for Disease Control and Prevention. Tobacco Control Highlights 2012. 2013. [Last accessed on 2016 Feb 02]. Available from: http://www.cdc.gov/tobacco/data_statistics/state_data/state_highlights/2010/states/maryland .
- 3.Barbeau EM, Krieger N, Soobader MJ. Working class matters: Socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health. 2004;94:269–78. doi: 10.2105/ajph.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: A review. Ann N Y Acad Sci. 2012;1248:107–23. doi: 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- 5.Margerison-Zilko C, Cubbin C. Socioeconomic disparities in tobacco-related health outcomes across racial/ethnic groups in the United States: National Health Interview Survey 2010. Nicotine Tob Res. 2013;15:1161–5. doi: 10.1093/ntr/nts256. [DOI] [PubMed] [Google Scholar]
- 6.Bureau UC. American Community Survey (ACS) [Last accessed on 2017 Jun 12]. Available from: https://www.census.gov/programs-surveys/acs .
- 7.Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: A systematic review of risk factors. Clin Psychol Rev. 2013;33:1010–24. doi: 10.1016/j.cpr.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Wagner FA, Sheikhattari P, Buccheri J, Gunning M, Bleich L, Schutzman C, et al. A community-based participatory research on smoking cessation intervention for urban communities. J Health Care Poor Underserved. 2016;27:35–50. doi: 10.1353/hpu.2016.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs. US Department Health Human Services Center Disease Control Prevention National Center Chronic Disease Prevention Health Promotion Office Smoking Health. 2014 [Google Scholar]
- 10.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 11.El-Khorazaty MN, Johnson AA, Kiely M, El-Mohandes AA, Subramanian S, Laryea HA, et al. Recruitment and retention of low-income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC Public Health. 2007;7:233. doi: 10.1186/1471-2458-7-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheikhattari P, Zhu S, Clubb P, Wagner FA. New insights on tobacco smoking among underserved and poor. World Academy of Science, Engineering, and Technology. 2010:400–5. [Google Scholar]
- 13.Freshstart Program by American Cancer Society Workplace olutions. [Last accessed on 2016 Feb 05]. Available from: http://www.acsworkplacesolutions.com/freshstart.asp .
- 14.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 15.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102–14. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 16.Fagerstrom KO, Heatherton TF, Kozlowski LT. Nicotine addiction and its assessment. Ear Nose Throat J. 1990;69:763–5. [PubMed] [Google Scholar]
- 17.Ryter SW, Choi AM. Carbon monoxide in exhaled breath testing and therapeutics. J Breath Res. 2013;7:017111. doi: 10.1088/1752-7155/7/1/017111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.EpiData Software. EpiData Software. Odense, Denmark: EpiData Association. [Last accessed on 2016 Feb 02]. Available from: http://www.epidata.dk .
- 19.Stata Statistical Software. College Station, TX: StataCorp LP: StataCorp. 2011. [Last accessed on 2016 Feb 02]. http://www.stata.com1 .
- 20.Sheikhattari P, Apata J, Kamangar F, Schutzman C, O’Keefe A, Buccheri J, et al. Examining smoking cessation in a community-based versus clinic-based intervention using community-based participatory research. J Community Health. 2016;41:1146–52. doi: 10.1007/s10900-016-0264-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ATLAS.ti: The Qualitative Data Analysis & Research Software. Atlas.ti. [Last accessed on 2016 Oct 26]. Available from: http://www.atlasti.com .
- 22.Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: A randomized controlled trial. Am J Public Health. 2011;101:2253–60. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hooper MW, Larry R, Okuyemi K, Resnicow K, Dietz NA, Robinson RG, et al. Culturally specific versus standard group cognitive behavioral therapy for smoking cessation among African Americans: An RCT protocol. BMC Psychol. 2013;1:15. doi: 10.1186/2050-7283-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wallen J, Randolph S, Carter-Pokras O, Feldman R, Kanamori-Nishimura M. Engaging African Americans in smoking cessation programs. Am J Health Educ. 2014;45:151–7. [Google Scholar]
- 25.Amendola MG, Nazario N, Sanchez V. Using CBPR to assess client needs at a social service agency. Public Health Nurs. 2016;33:167–75. doi: 10.1111/phn.12204. [DOI] [PubMed] [Google Scholar]
- 26.Andrews JO, Tingen MS, Jarriel SC, Caleb M, Simmons A, Brunson J, et al. Application of a CBPR framework to inform a multi-level tobacco cessation intervention in public housing neighborhoods. Am J Community Psychol. 2012;50:129–40. doi: 10.1007/s10464-011-9482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rhodes SD, Kelley C, Simán F, Cashman R, Alonzo J, McGuire J, et al. Using Community-Based Participatory Research (CBPR) to develop a community-level HIV prevention intervention for Latinas: A local response to a global challenge. Womens Health Issues. 2012;22:e293–301. doi: 10.1016/j.whi.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee CS, Hayes RB, McQuaid EL, Borrelli B. Predictors of retention in smoking cessation treatment among Latino smokers in the Northeast United States. Health Educ Res. 2010;25:687–97. doi: 10.1093/her/cyq010. [DOI] [PubMed] [Google Scholar]
- 29.Ahluwalia JS, Harris KJ, Catley D, Okuyemi KS, Mayo MS. Sustained-release bupropion for smoking cessation in African Americans: A randomized controlled trial. JAMA. 2002;288:468–74. doi: 10.1001/jama.288.4.468. [DOI] [PubMed] [Google Scholar]
- 30.Curtin L, Brown RA, Sales SD. Determinants of attrition from cessation treatment in smokers with a history of major depressive disorder. Psychol Addict Behav. 2000;14:134–42. doi: 10.1037//0893-164x.14.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nevid JS, Javier RA, Moulton JL., 3rd Factors predicting participant attrition in a community-based, culturally specific smoking-cessation program for Hispanic smokers. Health Psychol. 1996;15:226–9. doi: 10.1037//0278-6133.15.3.226. [DOI] [PubMed] [Google Scholar]


