Abstract
The presence of common physical comorbidities, their demographic and clinical correlates and impact on functioning was assessed in 100 patients with schizophrenia. The patients had a mean age of 35.12±10.7 yr with mean duration of illness of 8.3±0.58 years. Seventy per cent were detected to have a comorbid physical condition. Common conditions included hypertension (21%), diabetes mellitus (15%) and anaemia (12%). Increasing age, being female, being married, longer duration of illness and longer duration of treatment were associated with higher risk of having a comorbid physical illness. Further studies need to be done with a large sample to confirm these findings.
Keywords: Diabetes mellitus, hypertension, physical comorbidity, schizophrenia, tuberculosis
Schizophrenia afflicts approximately one per cent of the population worldwide1 and is among the most disabling diseases in the young age group. Although the disability due to schizophrenia is coming down with advances in treatment2, physical comorbidities such as cardiovascular, respiratory, neurological, infectious and sexually transmitted diseases remain cause for concern3. Comorbid physical illnesses are one of the potential reasons for reduced life expectancy in schizophrenia4,5. Various risk factors associated with lifestyle and treatment such as obesity, smoking, hypertension, dyslipidaemia, hyperglycaemia and neuroleptic medications add to the risk for developing physical illnesses3,5,6,7. The prevalence of physical comorbidities in patients with schizophrenia has been reported to be high compared to the general population with odds ratios varying from 2.62 to 7.548. The patients are often unable to seek adequate physical care due to social isolation, lack of insight, lack of employment, difficulty in communication and reduced pain sensitivity3,5,9. This cross-sectional study was undertaken from March to August 2013 in the department of Psychiatry, All India Institute of Medical Sciences, New Delhi, India, to assess the presence of common physical comorbidities in patients with schizophrenia, their clinical and socio-demographic correlates and impact on functioning. All patients attending the walk- in clinic with a diagnosis of schizophrenia on four days a week were screened for inclusion criteria for the study. To be included, the patients needed to meet the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM IV)10 criteria of schizophrenia, and be above 18 yr with duration of illness of more than two years. Female patients with pregnancy were excluded. Patients and their caregivers were informed in detail about the purpose of the study. Written informed consent was taken from the patient and/ or caregiver. The study was approved by the Institute Ethics Committee.
Socio-demographic and clinical details such as duration of illness, duration of treatment and past and family history of psychiatric illness were recorded. The severity of schizophrenia was assessed using the Positive and Negative Syndrome Scale (PANSS)11. The current status of functioning was assessed using the Global Assessment of Functioning (GAF)10 and Social and Occupational Functioning Assessment Scale (SOFAS)10. All assessments were conducted on the first day of inclusion. Physical illness checklist, prepared for the study, based on earlier studies on physical comorbidity in schizophrenia3,5,6, was used to screen for physical illnesses in the patient and the family. Detailed physical examination was conducted, and laboratory investigations (haemogram, liver and renal function tests, fasting blood sugar and lipid profile), X-ray chest and electrocardiography were conducted on the next day. Patients detected to have physical illness were referred to the concerned speciality in the hospital. Data were analyzed using SPSS (version 20) for Microsoft software (IBM, Armonk, NY, USA). Percentage and frequency was calculated for nominal and ordinal variables, and mean and standard deviation was calculated for continuous variables. Independent sample t test, Mann-Whitney test and Chi-square test were used for comparison.
One hundred patients (55 males and 45 females) were included in the study. The mean age was 35.12±10.7 yr (range 18 to 72 yr), and mean duration of illness was 8.3±7.8 yr (range 2-30 yr) with mean duration of treatment of 7.8 yr (range 1 month-30 yr). Most (86%) patients were on 2nd generation antipsychotic and 12 were on a 1st generation antipsychotic. One patient was on both 1st as well as 2nd generation antipsychotics, and one was maintaining well without any antipsychotic. In 40 per cent patients, comorbid substance abuse in the form of tobacco (40%) and alcohol (13%) was present. The mean total score (±SD) on PANSS was 66.89±11.46. The mean scores on the positive, negative and general psychopathology scales were 14.6±6.12, 22.67±7.98 and 29.56±6.44, respectively. The mean score on GAF was 61.7±15.68 (range 20-90). The mean score on SOFAS was 61.54±15.12 (range 30-90).
In 70 per cent patients, comorbid physical illnesses were detected on history and physical assessment. Common comorbidities included hypertension (21%), diabetes mellitus (15%), anaemia (12%), tuberculosis (7%), obesity (6%) and menstrual disturbances (5%). Less frequent physical illnesses included thyroid disorder (4%), epilepsy (3%), cerebrovascular accident (2%), coronary artery disease (CAD) (2%), deafness (2%), liver disease (2%), other gastrointestinal illnesses (2%) and dementia (1%). The mean body mass index score of participants was 24.4±3.8 kg/m2 ranging from 16.5 to 39.5. Thirty two per cent suffered from only one comorbid physical illness, whereas 21 and 11 per cent had two and three comorbid illnesses, respectively. Those with current physical illness were significantly older than those without physical illness (P =0.001). Current physical illnesses were significantly more commonly seen in females (P =0.016) and in the married (P =0.004) individuals. Participants with a comorbid physical illness tended to have a longer duration of illness [median duration 8.0 (2-21) vs 5.0 (2-30) years, P =0.016] as well as longer duration of treatment [median duration 7.5 (0.1-20) vs 4.5 (2-30) years, P =0.024]. There was no difference in the level of functioning between the participants with or without physical comorbidity as assessed on SOFAS and GAF (Table).
Table.
Association of socio-demographic and clinical variables with current physical illnesses (n=100)
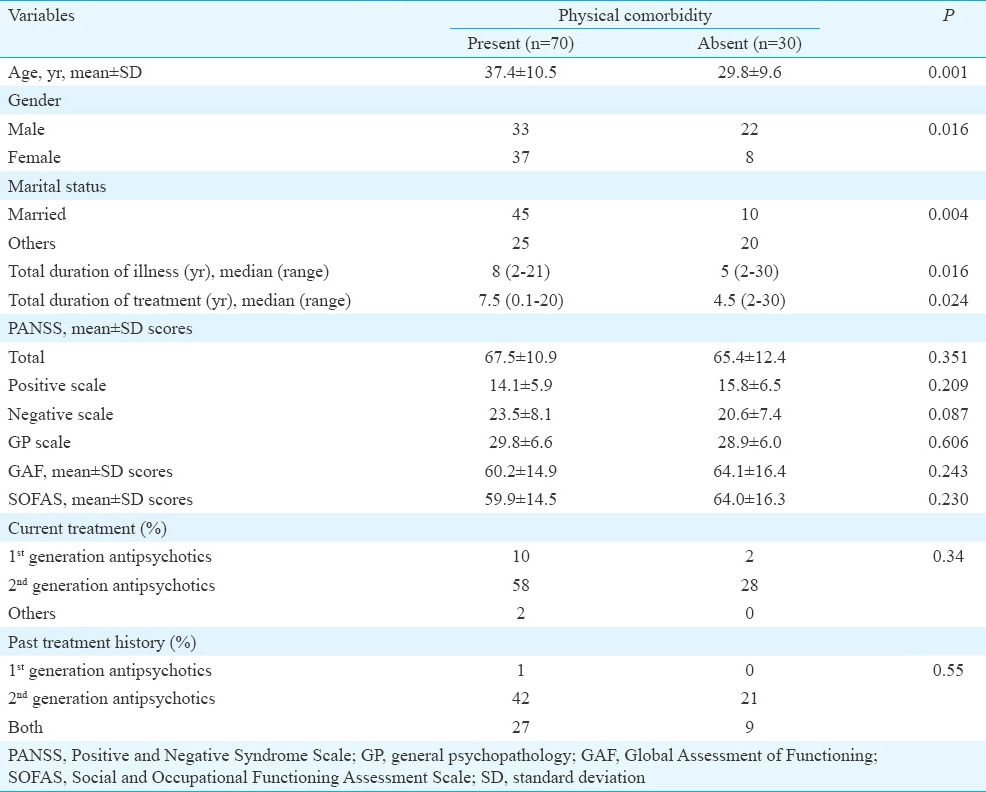
Although 70 per cent of patients suffered from a comorbid physical condition, an average number of physical comorbidities was low at 1.34 (range=0-5), which was lower than that reported in an earlier study12. Patients with physical illnesses tended to be older, married and female and had a longer duration of illness. Age has been identified as a risk factor in an earlier study also12. Similarly, a longer duration of illness and duration on treatment were significantly associated with higher risk to develop physical illnesses. Long duration of exposure to antipsychotic treatment, especially the 2nd generation antipsychotics, is a known risk factor for the common physical comorbidities5. Lifestyle illnesses such as diabetes mellitus, hypertension and CAD have common risk factors which are accentuated by 2nd generation antipsychotics and sedentary lifestyle5. Fifty five patients suffered from lifestyle illnesses, and among them, 43 were on 2nd generation antipsychotics. No significant difference was observed between the patients on 1st and 2nd generation antipsychotics probably due to limited sample size in our study.
The presence of physical comorbidity for individual illnesses such as hypertension, diabetes mellitus, anaemia, obesity and CAD was similar to an earlier nationwide study on hospitalized patients from Spain on physical comorbidity in patients with schizophrenia13 though lower than general estimates reported in another study5.
There was no significant difference in the level of functioning as measured on GAF and SOFAS between the patients with or without physical comorbidity. In one of the previous studies assessing psychosocial functioning in patients of schizophrenia with comorbid physical illnesses12, physical comorbidity was found to have only a limited effect on psychosocial functioning.
Though our study had a limitation of cross-sectional design, limited sample size, use of a basic set of physical investigations and lack of a control population, it showed presence of physical comorbidities in a substantial number of patients with schizophrenia even with a limited number of investigations. There is a need for multicentre nationwide studies with a larger sample and an expanded battery of investigations to reach to a valid conclusion.
Footnotes
Conflicts of Interest: None.
References
- 1.Freedman R. Schizophrenia. N Engl J Med. 2003;349:1738–49. doi: 10.1056/NEJMra035458. [DOI] [PubMed] [Google Scholar]
- 2.Thirthalli J, Venkatesh BK, Kishorekumar KV, Arunachala U, Venkatasubramanian G, Subbakrishna DK, et al. Prospective comparison of course of disability in antipsychotic-treated and untreated schizophrenia patients. Acta Psychiatr Scand. 2009;119:209–17. doi: 10.1111/j.1600-0447.2008.01299.x. [DOI] [PubMed] [Google Scholar]
- 3.Leucht S, Burkard T, Henderson J, Maj M, Sartorius N. Physical illness and schizophrenia: A review of the literature. Acta Psychiatr Scand. 2007;116:317–33. doi: 10.1111/j.1600-0447.2007.01095.x. [DOI] [PubMed] [Google Scholar]
- 4.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: Is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–31. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 5.DE Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeste DV, Gladsjo JA, Lindamer LA, Lacro JP. Medical comorbidity in schizophrenia. Schizophr Bull. 1996;22:413–30. doi: 10.1093/schbul/22.3.413. [DOI] [PubMed] [Google Scholar]
- 7.De Hert M, Cohen D, Bobes J, Cetkovich-Bakmas M, Leucht S, Ndetei DM, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011;10:138–51. doi: 10.1002/j.2051-5545.2011.tb00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carney CP, Jones L, Woolson RF. Medical comorbidity in women and men with schizophrenia: A population-based controlled study. J Gen Intern Med. 2006;21:1133–7. doi: 10.1111/j.1525-1497.2006.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lambert TJ, Velakoulis D, Pantelis C. Medical comorbidity in schizophrenia. Med J Aust. 2003;178(Suppl):S67–70. doi: 10.5694/j.1326-5377.2003.tb05311.x. [DOI] [PubMed] [Google Scholar]
- 10.4th ed. Washington DC, USA: American Psychiatric Association; 2000. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. [Google Scholar]
- 11.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 12.Chwastiak LA, Rosenheck RA, McEvoy JP, Keefe RS, Swartz MS, Lieberman JA. Interrelationships of psychiatric symptom severity, medical comorbidity, and functioning in schizophrenia. Psychiatr Serv. 2006;57:1102–9. doi: 10.1176/ps.2006.57.8.1102. [DOI] [PubMed] [Google Scholar]
- 13.Bouza C, López-Cuadrado T, Amate JM. Physical disease in schizophrenia: A population-based analysis in Spain. BMC Public Health. 2010;10:745. doi: 10.1186/1471-2458-10-745. [DOI] [PMC free article] [PubMed] [Google Scholar]


