Sir,
Cystic artery pseudoaneurysms have been described secondary to trauma, inflammation, and vascular disease, with only 23 nontraumatic cases reported in the literature.[1,2,3,4,5,6] We report the diagnosis and transcatheter embolization of a cystic artery pseudoaneurysm caused by acute, ruptured cholecystitis, a previously undescribed etiology.
A 54-year-old female with hepatitis C cirrhosis and portal hypertension was admitted for intermittent burning epigastric abdominal pain, low-grade fever, and melena. Laboratory results revealed obstructive jaundice, anemia, thrombocytopenia, and elevated international normalized ratio (INR).
Esophagogastroduodenoscopy and colonoscopy were noncontributory. Abdominal ultrasonography revealed a hyperemic, edematous gallbladder wall, gallbladder sludge, and pericholecystic fluid. In addition, there was a cystic, echogenic lesion with internal flow in a “yin-yang” pattern, characteristic of a pseudoaneurysm [Figure 1]. Subsequent contrast-enhanced computed tomography (CT) demonstrated an enhancing gallbladder wall lesion corresponding to the cystic artery pseudoaneurysm. Additionally, calcified gallstones were noted adjacent to the gallbladder and within the pelvis [Figure 2]. The cystic artery pseudoaneurysm, cholecystitis, and extracystic gallstones were not present on a contrast-enhanced CT obtained 3 months prior, suggesting acute cholecystitis with gallbladder perforation resulting in a bleeding cystic artery pseudoaneurysm.
Figure 1(A and B).
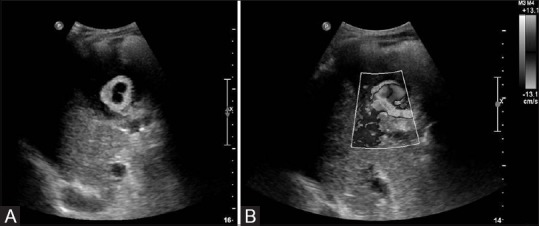
Grayscale (A) and color Doppler (B) images of the gallbladder demonstrate a 3.2 cm cystic artery pseudoaneurysm within the gallbladder. On color Doppler imaging, blood flow is seen within the pseudoaneurysm in the classic “yin-yang” pattern
Figure 2(A-C).
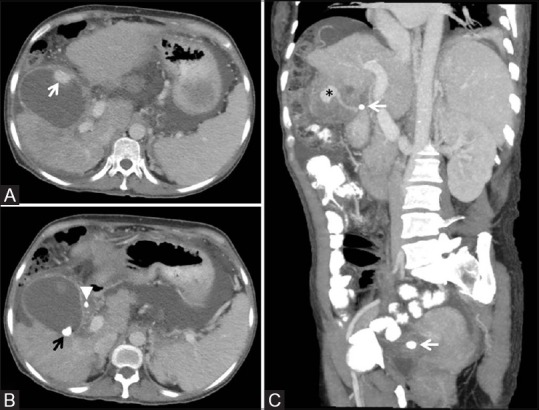
Axial images from a contrast-enhanced CT (A and B) demonstrates the enhancing cystic artery pseudoaneurysm in the anterior wall of the gallbladder (A, white arrow). There are intraluminal (B, black arrow) and extraluminal (B, white arrowhead) gallstones. A coronal oblique 4 mm maximum intensity projection image (C) demonstrates the pseudoaneurysm (asterisk) being supplied by the cystic artery. Note the gallstones adjacent to the gallbladder and in the pelvis (white arrows), which were previously seen within the gallbladder on a CT from 3 months prior
Considering the perforated gallbladder and bleeding pseudoaneurysm, general surgery was consulted; however, the patient was deemed a poor surgical candidate. Interventional radiology was then consulted for further evaluation.
The bleeding pseudoaneurysm was addressed first, given the patient's anemia. Fluoroscopically-guided embolization was undertaken in the angiography suite under general anesthesia. Through a 5-French angiographic sheath (Boston Scientific; Boston, MA, USA) in the right common femoral artery, a 4-French Slip-Cath Beacon Tip Cobra catheter (Cook Medical; Bloomington, IN, USA) was advanced into the common hepatic artery. The cystic artery was selected with a 2.7-French microcatheter (Terumo; Somerset, NJ, USA), and an angiogram showed a large pseudoaneurysm. Further microcatheter advancement was not possible, hence, four 3-mm pushable feathered microcoils (Cook Medical; Bloomington, IN, USA) were deployed. Due to elevated INR and thrombocytopenia, the pseudoaneurysm persisted; hence, 500 units (1000 units/mL) of thrombin (King Pharmaceutical; Bristol, TN, USA) were injected through the catheter. Detachable coils and glue were unavailable. Completion angiography demonstrated occlusion of the pseudoaneurysm [Figure 3].
Figure 3(A-D).
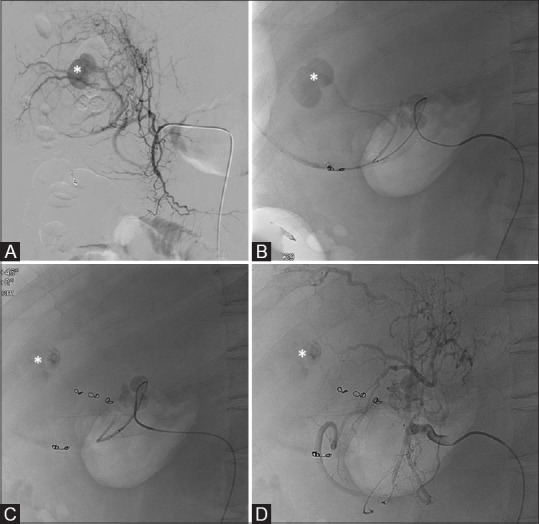
Catheter-based arteriography demonstrates a pseudoaneurysm within the gallbladder (A, asterisk). Subselective catheterization reveals this pseudoaneurysm to arise from the cystic artery (B, asterisk). After deployment of coils and thrombin, the pseudoaneurysm no longer fills with contrast (C, asterisk). On completion angiography from the common hepatic artery (D), note the stagnant contrast within the pseudoaneurysm
A percutaneous cholecystostomy tube was then inserted for the patient's acute, perforated cholecystitis. It initially drained frank blood, however, over the next few hours, began to drain nonbloody, bilious fluid. The patient's melena ceased. Unfortunately, she subsequently had recurrent bouts of peritonitis and ultimately succumbed to sepsis.
In 1871, Quincke described a triad of symptoms for cystic artery pseudoaneurysms – right upper quadrant pain, obstructive jaundice, and hemobilia.[7] Imaging now predominates diagnosis, with color Doppler ultrasonography, contrast-enhanced CT, and catheter-based angiography successfully detecting the pseudoaneurysm in our case. Use of magnetic resonance imaging (MRI) has also been described.[1]
It has been postulated that cholecystitis may ulcerate the serosa and injure the arterial wall, thus resulting in cystic artery pseudoaneurysms.[8] In our case, the most likely cause of the cystic artery pseudoaneurysm was gallbladder perforation, evidenced by the development of patient's symptoms, the cystic artery pseudoaneurysm, and the extracystic gallstones when compared to imaging from only 3 months prior.
Cystic artery pseudoaneurysms can be treated by cholecystectomy with ligation of the cystic artery; selective transcatheter embolization; percutaneous direct injection of an embolization agent; or a staged approach, with initial embolization followed by elective cholecystectomy.[9] Embolization may be more attractive in unstable patients; however, it cannot address any associated cholecystitis and may require a percutaneous cholecystostomy.
In conclusion, we report acute cholecystitis with gallbladder perforation resulting in a bleeding cystic artery pseudoaneurysm. While a variety of diagnostic and therapeutic options exist, our critically ill patient was successfully managed nonsurgically with transcatheter arterial embolization and percutaneous gallbladder drainage.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Komatsu Y, Orita H, Sakurada M, Maekawa H, Hoppo T, Sato K. Report of a case: Pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization. J Med Cases. 2011;2:178–83. [Google Scholar]
- 2.Leung JL, Kan WK, Cheng SC. Mycotic cystic Artery pseudoaneurysm. Hong Kong Med J. 2010;16:156–7. [PubMed] [Google Scholar]
- 3.Ahmed I, Tanveer UH, Sajjad Z, Munazza B, Azeem UD, Basit S. Cystic artery pseudo-aneurysm: A complication of xanthogranulomatous cholecystitis. Br J Radiol. 2010;83:e165–7. doi: 10.1259/bjr/34623636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Molla Neto OL, Ribeiro MAF, Saad WA. Pseudoaneurysm of cystic artery after laparoscopic cholecystectomy. HPB (Oxford) 2006;8:318–9. doi: 10.1080/13651820600869628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desai AU, Sauders MP, Anderson HJ, Howlett DC. Successful transcatheter arterial embolisation of a cystic artery pseudoaneurysm secondary to calculus cholecystitis: A case report. J Radiol Case Rep. 2010;4:18–22. doi: 10.3941/jrcr.v4i2.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saluja SS, Ray S, Gulati MS, Pal S, Sahni P, Chattopadhyay TK. Acute cholecystitis with massive upper gastrointestinal bleed: A case report and review of literature. BMC Gastroenterol. 2007;7:12. doi: 10.1186/1471-230X-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quincke H. Ein fall von aneurysma der leberarterie. Klin Wochenschr. 1871;30:349–52. [Google Scholar]
- 8.Maeda A, Kunou T, Saeki S, Aono K, Murata T, Niinomi N, et al. Pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization and elective cholecystectomy. J Hepatobiliary Pancreat Surg. 2002;9:755–8. doi: 10.1007/s005340200105. [DOI] [PubMed] [Google Scholar]
- 9.Akatsu T, Tanabe M, Shimizu T, Handa K, Kawachi S, Aiura K, Ueda M, et al. Pseudoaneurysm of the cystic artery secondary to cholecystitis as a cause of hemobilia: Report of a case. Surg Today. 2007;37:412–7. doi: 10.1007/s00595-006-3423-2. [DOI] [PubMed] [Google Scholar]


