Abstract
The active subunit (S1) of pertussis toxin (PT), a major virulence factor of Bordetella pertussis, ADP-ribosylates Gi proteins in the mammalian cell cytosol to inhibit GPCR signaling. The intracellular pathway of PT includes endocytosis and retrograde transport to the trans-Golgi network (TGN) and endoplasmic reticulum (ER). Subsequent translocation of S1 to the cytosol is presumably preceded by dissociation from the holotoxin. In vitro, such dissociation is stimulated by interaction of PT with ATP. To investigate the role of this interaction in cellular events, we engineered a form of PT (PTDM) with changes to two amino acids involved in the interaction with ATP. PTDM was reduced in (1) binding to ATP, (2) dissociability by interaction with ATP, (3) in vitro enzymatic activity and (4) cellular ADP-ribosylation activity. In cells treated with PTDM carrying target sequences for organelle-specific modifications, normal transport to the TGN and ER occurred, but N-glycosylation patterns of the S1 and S4 subunits were consistent with an inability of PTDM to dissociate in the ER. These results indicate a requirement for interaction with ATP for PT dissociation in the ER and cellular activity. They also indicate that the retrograde transport route is the cellular intoxication pathway for PT.
Keywords: pertussis toxin, intracellular transport, retrograde transport, Bordetella pertussis, bacterial toxin, holotoxin dissociation
Pertussis toxin undergoes retrograde transport to the endoplasmic reticulum, where ATP binding to the toxin B oligomer mediates dissociation of the A subunit from the holotoxin.
INTRODUCTION
Bordetella pertussis, a Gram-negative bacterial pathogen and the causative agent of whooping cough, secretes several virulence factors. One of these factors, pertussis toxin (PT), plays an early role in colonization of the respiratory tract by the pathogen (Carbonetti et al.2003, 2005a; Carbonetti 2007) and a later role in airway inflammation and pathology associated with the disease (Andreasen, Powell and Carbonetti 2009; Connelly, Sun and Carbonetti 2012; Scanlon et al. 2014). PT is an AB5 toxin, composed of the subunits S1 to S5 in the ratio 1:1:1:2:1 (Tamura et al.1982; Stein et al.1994). The A subunit (S1) is an ADP-ribosyltransferase that inhibits signaling through receptors coupled to heterotrimeric Gi proteins on the inner surface of the plasma membrane of mammalian cells (Katada, Tamura and Ui 1983; Moss et al.1983). The B oligomer (subunits S2, S3, S4 and S5) mediates binding of PT to glycoprotein or glycolipid receptors on the cell surface (Brennan et al.1988; Witvliet et al.1989).
Our previous work provided biochemical evidence of the intracellular pathway of PT (Plaut and Carbonetti 2008). Following uptake via endocytosis, PT undergoes retrograde transport to the trans-Golgi network (TGN) and the endoplasmic reticulum (ER). S1 may then be translocated to the cytosol, enabling the toxin to access its G protein targets, perhaps via subversion of the ER-associated protein degradation (ERAD) pathway by which misfolded proteins are transported out of the ER for degradation by the proteasome (Werner, Brodsky and McCracken 1996; Hazes and Read 1997; Worthington and Carbonetti 2007). This retrograde transport pathway is utilized by several other bacterial toxins, as well as the plant toxin ricin and some viruses (Spooner et al.2006; Mukhopadhyay and Linstedt 2013).
In vitro, PT activity is stimulated by interaction with ATP (Lim, Sekura and Kaslow 1985), and the crystal structure of ATP-associated PT shows ATP inserted in the central ‘pore’ of the B oligomer, in the area where the C-terminus of S1 interacts with the B oligomer (Hazes et al.1996). ATP appears to activate PT in vitro by destabilizing the holotoxin and facilitating cleavage of a disulfide bond in S1 (Moss et al.1983, 1986; Hausman, Manclark and Burns 1990), which, in turn, allows interaction of the active site of S1 with its substrates (Stein et al.1994). Interaction with ATP also promotes the dissociation of PT holotoxin in vitro (Burns and Manclark 1986; Krueger and Barbieri 1993). Presumably, in order to enter the cytosol via a pore in the ER membrane, S1 must dissociate from the B oligomer. This dissociation of the holotoxin has been hypothesized to occur following the interaction of PT with ATP in the ER, where ATP is prevalent (Hazes et al.1996; Hazes and Read 1997).
Based on details of the PT-ATP crystal structure (Hazes et al.1996), we modified amino acids thought to be involved in the interaction. In combination with the use of peptide tags that are targets for organelle-specific modifications (Rapak, Falsnes and Olsnes 1997; Plaut and Carbonetti 2008), we were able to study the importance of the PT-ATP interaction to PT dissociation, activity and intracellular transport, and to test the hypothesis that ATP-mediated dissociation of PT occurs in the ER.
MATERIALS AND METHODS
Reagents
Tunicamycin (TM) and carboxy methyl (CM-) Sepharose CL-6B were from Sigma (St. Louis, MO). Na235SO4 and [32P]NAD were from Perkin Elmer (Waltham, MA). α-[32P]ATP was from Amersham (Little Chalfont, UK). HeLa (human cervix epithelial) and CHO-K1 (Chinese hamster ovary epithelial) cells were from American Type Culture Collection (Manassas, VA). Anti-PT rabbit polyclonal antibodies 4696 and 4697 were raised by Lampire Biological Laboratories (Pipersville, PA). For immunofluorescence microscopy, primary antibodies were mouse monoclonal IgG2b against protein disulfide isomerase (PDI) (ThermoScientific, Waltham, MA) and rabbit polyclonal anti-PT #8945 (Lampire Biological Laboratories); secondary antibodies were Alexa Fluor 488 goat anti-mouse IgG (Abcam, Cambridge, MA) and Alexa Fluor 594 goat anti-rabbit IgG (Life Technologies, Frederick, MD).
Bacterial strains and growth conditions
The nalidixic acid- and streptomycin-resistant derivative of Bordetella pertussis W28 (Wellcome, London, UK) and the construction of strain PT-9K/129G (PT*; Pizza et al.1989) were described previously (Carbonetti et al.2003; Plaut and Carbonetti 2008). Growth conditions and strains used for cloning and conjugation were described previously (Plaut and Carbonetti 2008).
Plasmid and strain construction
Amino acid residues of S5 were modified as indicated in Table 1, based on the crystal structure of the interaction between PT and ATP (Hazes et al.1996), using procedures previously described (Plaut and Carbonetti 2008). For construction of all PT mutations (the single mutations (SM) PTSM58 and PTSM62, as well as the PTDM58/62 double mutation (PTDM)), a PCR fragment encoding substitutions of the indicated amino acid residues was ligated into NsiI/SnaBI-digested pS-PT (a 4.7-kb fragment containing the ptx genes inserted into the allelic exchange vector pSS1129; Stibitz and Yang 1991), creating plasmids pS-S5-58, pS-S5-62 and pS-S5-58/62. For PTS1GSDM, a DH10B strain carrying pJ-PTS1GS (a derivative of the allelic exchange vector pJHC1; Kinnear et al.1999; Plaut and Carbonetti 2008) was used as the donor in a conjugation with PTDM as the recipient. For PTS4GSDM, an XbaI-BglII fragment from pS-S5-58/62 was inserted into pJHC1, creating pJ-S5-58/62; a PCR fragment including the target sites at the C-terminus of S4 was then ligated into MluI/NsiI-digested pJ-S5-58/62.
Table 1.
Modifications to PT subunits. Residues 58 and 62 of S5 were substituted singly and in combination, in order to provide steric hindrance to the interaction between PT and ATP. PTS1GS, PTS4GS, PTS1GSDM and PTS4GSDM were engineered with peptide sequences that are targets for tyrosine sulfation and N-glycosylation (Plaut and Carbonetti 2008) in addition to the indicated changes to residues of S5.
| Name | Residues changed | Source |
|---|---|---|
| PTSM58 | S5: G58N | This study |
| PTSM62 | S5: S62E | This study |
| PTDM | S5: G58N and S62E | This study |
| PTS1GS | S1: tyrosine sulfation and | Plaut and |
| N-glycosylation sites added | Carbonetti (2008) | |
| PTS4GS | S4: tyrosine sulfation and | Plaut and |
| N-glycosylation sites added | Carbonetti (2008) | |
| PTS1GSDM | S1: tyrosine sulfation and | This study |
| N-glycosylation sites added | ||
| S5: G58N and S62E | ||
| PTS4GSDM | S4: tyrosine sulfation and | This study |
| N-glycosylation sites added | ||
| S5: G58N and S62E |
Protein purification and analysis
Native PT and derivatives were purified from B. pertussis culture supernatants and analyzed by SDS-PAGE and western blotting as previously described (Plaut and Carbonetti 2008).
ADP-ribosyltransferase assays
In vitro ADP-ribosylation assays for PT activity using [32P]NAD and GST-αC20 substrate were performed as previously described (Carbonetti et al.2005b). Cellular activity was assessed as previously described (Xu and Barbieri 1995; Carbonetti et al.2005b); briefly, following treatment of cells with PT or derivatives, the post-nuclear supernatant containing target G proteins was used as substrate in an in vitro reaction with [32P]NAD and active PT. If the PT with which the cells were treated was fully active, all G proteins in the cells would be modified and none would be available for ADP-ribosylation in the in vitro reaction, leading to a lack of a band on the fluorograph. If the PT was unable to ADP-ribosylate the targets in the cells, the available G proteins would be modified in the in vitro reaction, leading to appearance of a radiolabeled band on the fluorograph. Increasing activity therefore correlates with decreasing intensity of bands on the fluorograph.
ATP binding assay
The ATP binding capacity of native and modified forms of PT was assessed using [32P]-ATP and a filter binding assay, similar to that previously described (Mattera et al.1986). Reactions contained 10 or 100 nM α-[32P]-ATP, 50 mM Tris pH 7.5, 1 mM EDTA, 15 mM NaCl, 0.4 mM DTT, 2 mM β-mercaptoethanol, 0.5 mg/ml ovalbumin and the indicated amount of PT or PTDM, in a volume of 50 μl. Reactions were incubated 30 min at 32ºC, after which 200 μl ice-cold 50 mM Tris was added, and the reaction was filtered through a nitrocellulose disk using a vacuum manifold. Filters were washed four times with ice-cold 50 mM Tris, and radioactivity retained on the filter was quantified by liquid scintillation counting. Background control values were obtained from reactions with no PT, and these values were subtracted from the experimental counts.
Surface plasmon resonance (SPR)-based PT dissociation assay
SPR-based detection of PT holoxin dissociation was performed using a modification of a previously described assay (Taylor et al. 2011). A gold-plated Reichert (Depew, NY) SPR sensor appended with ganglioside GD1a was set in a Reichert SR7000 dual-channel SPR refractometer and exposed to 0.2 ml of a PBST perfusion buffer containing 1 μg of wild-type or mutant PT for 15 min at a flow rate of 5 μl/min. The second channel was exposed to PBST buffer alone and thus served as a blank to correct for possible bulk flow and baseline drift effects. PBST was then perfused over both channels of the slide at 37°C and a flow rate of 41 μl/min to establish the baseline refractive index unit (RIU) signal corresponding to the mass of the GD1a-captured PT holotoxin. The perfusion buffer was then supplemented with either 10 μM ATP and 0.5% CHAPS for native PT or 100 μM ATP and 0.5% CHAPS for PTDM. When indicated by the arrowheads in the SPR sensorgrams, the perfusion buffer containing ATP and CHAPS was replaced with buffer containing sequential additions of anti-PTS1 and anti-PTS4 antibodies.
Intracellular transport assay
Transport of PT to the TGN and ER was assessed by a sulfation assay as previously described (Plaut and Carbonetti 2008). Cells were incubated with PT or derivatives (20 nM) for 24 h in the presence of Na235SO4. PT was immunoprecipitated from cell lysates and analyzed by SDS-PAGE and fluorography.
Indirect immunofluorescence microscopy
HeLa cells were grown on Lab-Tek chambered borosilicate coverglass and treated with 20 nM purified PT or 20 nM purified PTDM for 3 h at 37°C. Following treatment, cells were washed with PBS and then incubated with 4% w/v paraformaldehyde in PBS for 10 min to fix samples. A second wash in PBS containing 10 mM glycine (PBS/gly) was performed, cells were permeabilized by 3 min incubation in PBS/gly containing 0.5% v/v Triton X-100 and washed again in PBS/gly. A blocking step was performed for 30 min using 1% w/v BSA in PBS/gly and primary antibodies staining for PDI and PT were each added at 1:200 dilution and incubated overnight at 4°C. Cells were washed in PBS/gly, incubated with secondary antibodies diluted in PBS (1:400 anti-mouse Alexa Fluor 488, 2.5 μg/ml anti-rabbit Alexa Fluor 594) for 1 h in the dark and washed again. For controls against non-specific PT labeling, untreated cells were labeled with both anti-PT primary and secondary antibodies, and an isotype control replaced anti-PDI as a negative control with appropriate secondary antibody. Slides were imaged using a LSM510 META confocal microscope and analyzed using the GDSC Colocalization plugin for ImageJ from the University of Sussex.
Mouse infection
Six-week old BALB/c mice (five per group) were inoculated intranasally with 5×105 colony forming units (CFU) of the indicated B. pertussis strains as previously described (Carbonetti et al.2003). Four days later, mice were euthanized, and the lungs and trachea were removed and homogenized. Dilutions were plated and incubated at 37ºC for 4 days, after which the CFU per mouse were determined. Statistical significance of differences in colonization between groups was calculated using a t test.
RESULTS
Changes to residues of the S5 subunit of PT
In an attempt to inhibit the ability of PT to bind ATP and undergo ATP-stimulated dissociation, residues of S5 that are thought to be important for the interaction with ATP (Hazes et al.1996) were modified (Table 1). Glycine 58 and serine 62 were modified singly (PTSM58 and PTSM62) and in combination (PT double mutant or PTDM). These residues were replaced with asparagine and glutamate, respectively, based on the assumption that residues with bulky side groups would provide steric interference to the interaction between PT and ATP (Hazes et al.1996). The genetic modifications were confirmed by PCR and DNA sequencing, and these forms of PT were purified from culture supernatants of the modified Bordetella pertussis strains. SDS-PAGE and silver staining of purified PTDM confirmed that all PT subunits were present (data not shown), indicating that the changes to the residues in S5 did not prevent assembly or secretion of the holotoxin by the bacterium.
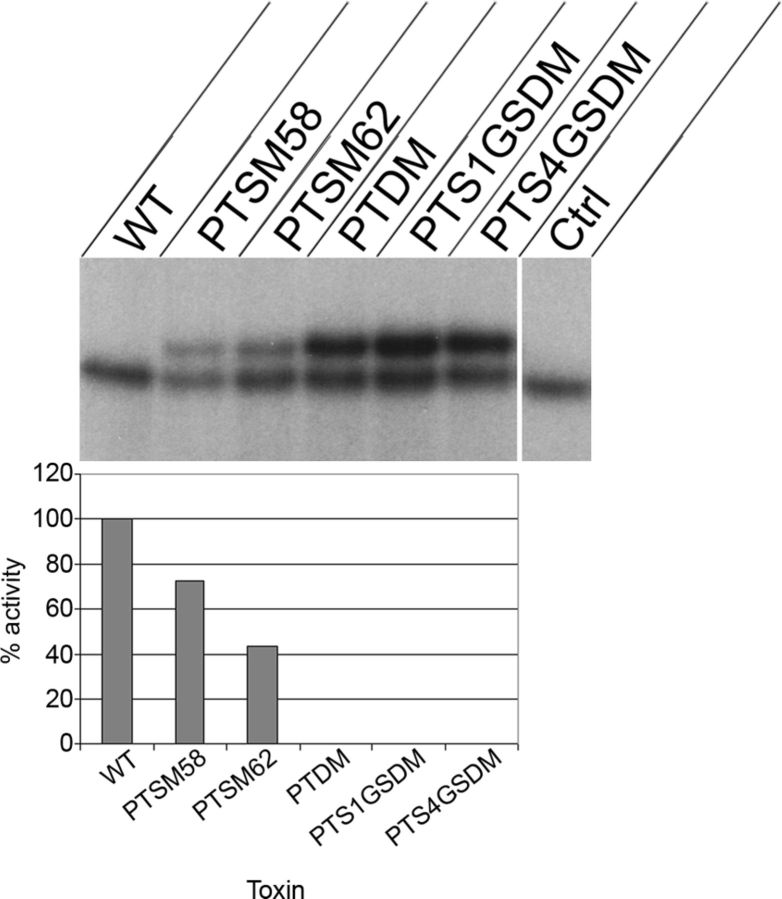
Cellular activity of modified forms of PT
To determine whether the changes to the residues in S5 affected the cellular activity of PT, we performed a cellular ADP-ribosylation assay. CHO-K1 cells were exposed to native or modified PT for 3 h, and the post-nuclear supernatant containing target G proteins was used as the substrate for an in vitro ADP-ribosylation assay. In this assay, absence of a band indicates full activity of the PT added to the cells. At this concentration (2 nM), no activity of PTDM was detected in cells, whereas the single mutants (PTSM58 and PTSM62) had activities that were 72% and 43% of native PT, respectively (Fig. 1). These results indicate that ATP binding by PT is necessary for its cellular activity. Because of the extent of reduction of its cellular activity, further investigations focused on PTDM.
Figure 1.
Cellular ADP-ribosylation assay. Upper panel: CHO-K1 cells were incubated with the indicated toxins (2 nM) for 3 h, and the post-nuclear supernatant was used as substrate in an ADP-ribosylation assay. The upper band (41 kDa) represents radiolabeled Giα; a faint or absent band indicates a high level of toxin activity in cells. The lower band represents endogenously labeled protein and is PT independent, as shown by inclusion of a reaction in which PT was not present in the in vitro portion of the assay (Ctrl). WT: native PT. Lower panel: data were analyzed by densitometry. Cellular activities of modified forms of PT are expressed as percentage of activity of native PT. These data are representative of two similar experiments.
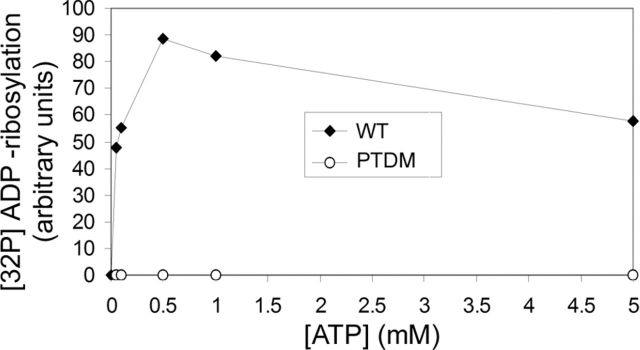
Enzymatic activity of PTDM
To determine whether the changes to the residues in S5 affected in vitro enzymatic activity of the toxin, PTDM was compared to native PT in an in vitro ADP-ribosylation assay at various concentrations of ATP. The assay was performed in the presence of [32P]NAD as the donor of ADP-ribose, with purified GST-αC20 as the target. ADP-ribosylation of GST-αC20 by wild-type PT was detected at concentrations of ATP between 0.05 and 5 mM; the optimal concentration was 0.5 mM (Fig. 2). In contrast, no in vitro activity was observed for PTDM, even at ATP concentrations as high as 50 mM (Fig. 2 and data not shown). These results indicate that the changes to the residues in S5 render PT enzymatically inactive in vitro, in addition to its loss of cellular activity as described above.
Figure 2.
In vitro ADP-ribosylation assay. Native PT (WT) or PTDM was incubated with GSTα-C20 protein as substrate and [32P]NAD as donor of ADP-ribose in the presence of ATP at the indicated concentrations. Data were analyzed by densitometry. These data are representative of two similar experiments.
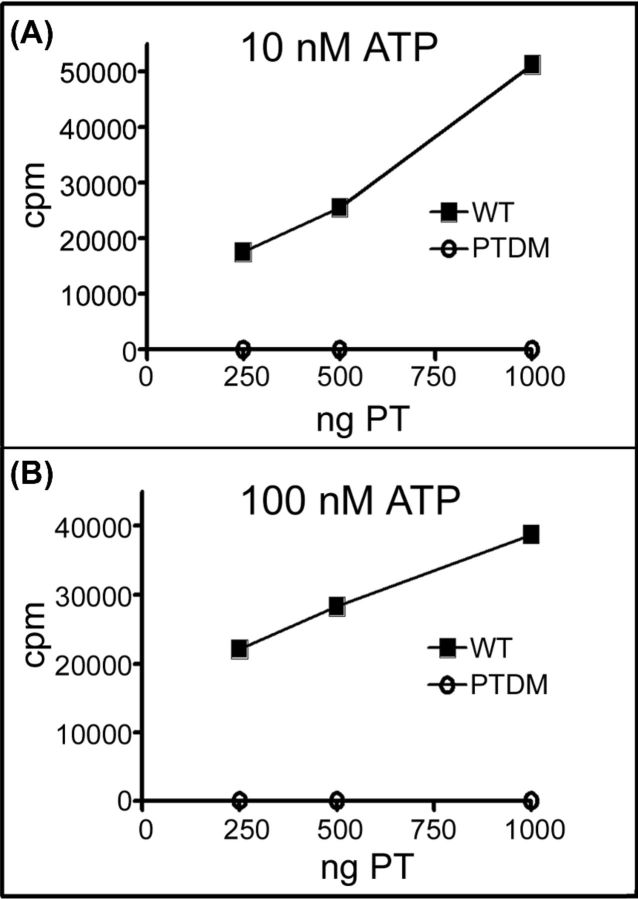
ATP binding property of PTDM
To determine whether replacement of the predicted ATP-interacting S5 residues affected the ability of PT to bind ATP, we performed ATP binding assays with native PT or PTDM. As shown in Fig. 3, as the amount of native PT in the reaction increased, the amount of radiolabeled ATP bound increased; however, PTDM showed no ATP binding, even at a concentration of 100 nM ATP. This result confirms that the changes to the residues in S5 of PTDM cause a complete lack of ATP binding by PT.
Figure 3.
ATP binding by native PT (WT) or PTDM. Filter binding assays were performed with varying amounts of PT and fixed concentrations of α-[32P]ATP (A: 10 nM; B: 100 nM). Results demonstrate a complete lack of ATP binding by PTDM. These data are representative of two similar experiments.
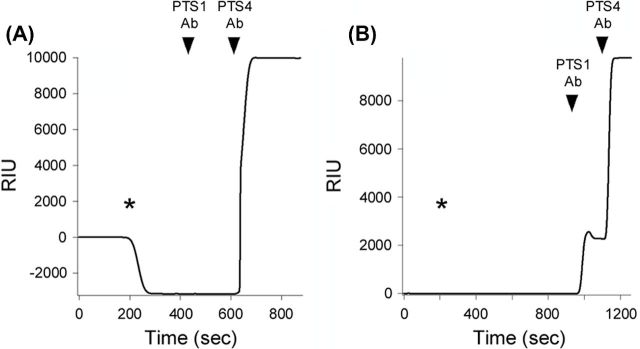
Dissociability of PTDM upon interaction with ATP
To assess whether ATP stimulated dissociation of PT or PTDM holotoxin in vitro, an SPR-based technique was used as previously described (Taylor et al. 2011). As shown in Fig. 4, ATP-induced disassembly of native PT was documented from the drop in RIU below the baseline value corresponding to the mass of PT holotoxin. Subsequent addition of an anti-PTS1 antibody to the perfusion buffer did not alter the RIU, whereas an elevated RIU resulted from the addition of an anti-PTS4 antibody to the perfusion buffer (panel A). This confirmed that PTS1 had been lost from the sensor-bound PTB oligomer. In contrast, a 10-fold higher concentration of ATP (100 μM) did not affect the stability of PTDM. Both anti-PTS1 and PTS4 antibodies generated positive signals when added to the perfusion buffer, thus demonstrating that PTS1 and PTS4 remained associated with the SPR sensor after exposure to 100 μM ATP (panel B). Together, these results confirm that the modifications to residues 58 and 62 on S5 in PTDM inhibit ATP-stimulated PT dissociation.
Figure 4.
SPR-based assay for ATP-stimulated disassembly of PT. PT holotoxin was captured on a SPR slide coated with GD1a. After establishing a baseline measurement (0 RIU) corresponding to the mass of the sensor-bound holotoxin, ATP and 0.5% CHAPS were added to the perfusion buffer at 200 s (asterisk). Anti-PTS1 and anti-PTS4 antibodies (Ab) were then added sequentially, as indicated by the arrowheads. (A) Native PT was exposed to 10 μM ATP. (B) PTDM was exposed to 100 μM ATP. One of two representative experiments is shown for each condition.
Trafficking of PTDM
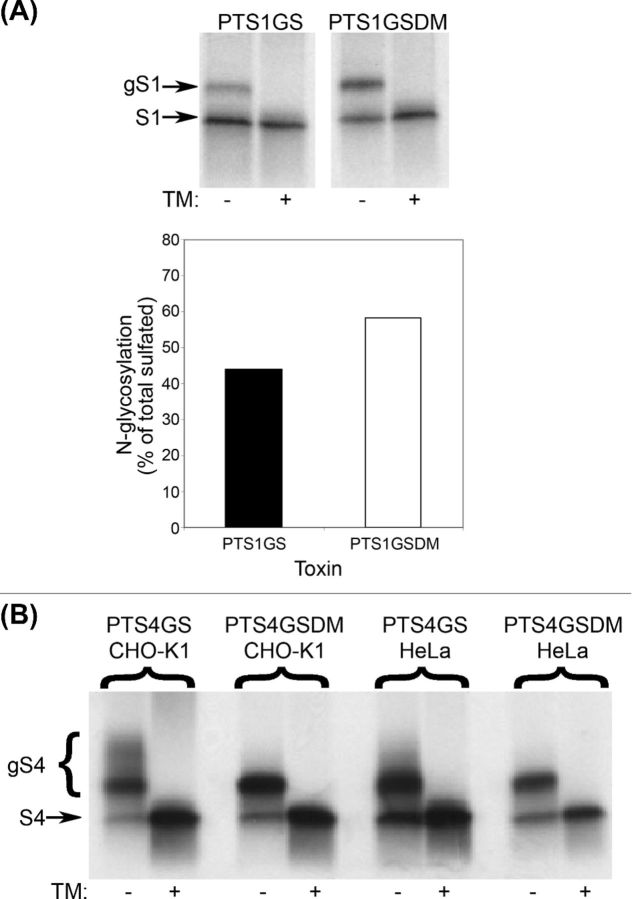
In a previous study on the intracellular transport of PT (Plaut and Carbonetti 2008), target sites for N-glycosylation (an ER-localized activity) and tyrosine sulfation (a TGN-localized activity) (Rapak, Falsnes and Olsnes 1997) were added to the S1 subunit of PT to generate a recombinant holotoxin termed PTS1GS (G for glycosylation, S for sulfation). This toxin exhibited wild-type levels of activity in cultured cells (Plaut and Carbonetti 2008). Here, we added target sites for N-glycosylation and tyrosine sulfation to the S1 or S4 subunits of PTDM to form recombinant holotoxins termed PTS1GSDM and PTS4GSDM, respectively (Table 1). As was the case for PTDM, no activity was detected for either PTS1GSDM or PTS4GSDM in a cellular ADP-ribosylation assay (Fig. 1).
To study the intracellular trafficking of the altered forms of PT, PTS1GSDM was compared to PTS1GS in a sulfation assay (Plaut and Carbonetti 2008). In both HeLa cells (Fig. 5A) and CHO-K1 cells (data not shown), toxin modified with radioactive sulfate was detected by SDS-PAGE and fluorography. Sulfated toxin (S1) that reached the ER could be detected by the mobility shift to a higher molecular weight resulting from its N-glycosylation (gS1). No mobility shift occurred in the presence of TM, an inhibitor of N-linked glycosylation, which confirmed that the larger form of the sulfated toxin was indeed glycosylated. Retrograde trafficking of PTS1GSDM to the TGN and ER was thus demonstrated by its sulfation and glycosylation, respectively. Moreover, in both cell types, a larger proportion of sulfated S1 was N-glycosylated in PTS1GSDM than in PTS1GS (Fig. 5A and data not shown). This result is consistent with the hypothesis that ATP stimulates holotoxin dissociation in the ER, because inhibition of dissociation would lead to retention of S1 in the ER, where it could be subjected to a greater degree of N-glycosylation than S1 from a dissociable (native) form of PT, which would proceed to the cytosol.
Figure 5.
Sulfation assays. CHO-K1 or HeLa cells were incubated for 24 h with the indicated toxins (20 nM) in the presence of radioactive sulfate and in the absence (–) or presence (+) of TM (1 μg/ml). The lower band represents S1 or S4 that was tyrosine sulfated in the TGN, whereas the upper band(s) (gS1 or gS4) represents S1 or S4 that was also N-glycosylated in the ER (and therefore higher molecular weight). Pretreatment of cells with TM, an inhibitor of N-glycosylation, prevented appearance of the upper band(s). (A) HeLa cells were incubated with PTS1GS or PTS1GSDM. Upper panel, fluorograph; lower panel, densitometric analysis, showing the percent N-glycosylated of total sulfated S1. Data plotted are the means of the results of two independent experiments. (B) CHO-K1 or HeLa cells were incubated with PTS4GS or PTS4GSDM.
When PTS4GSDM was compared to PTS4GS in a sulfation assay (Fig. 5B), PTS4GSDM exhibited an altered pattern of N-glycosylation. Whereas multiple high molecular weight TM-sensitive bands were apparent when CHO-K1 or HeLa cells were exposed to PTS4GS, these bands were not observed when cells were treated with PTS4GSDM. The higher molecular weight bands were previously shown to represent S4 that was transported anterograde to the Golgi and further glycosylated after core N-glycosylation in the ER (Plaut and Carbonetti 2008). The lack of ATP-driven holotoxin disassembly thus appeared to trap PTS4GSDM in the ER, thereby preventing its anterograde movement to the Golgi and further glycosylation of its S4 subunit. Alternatively, S4 that remains associated with S1 may be transported to the Golgi, but the proximity of S1 to S4 in the holotoxin (evident in the crystal structure; Stein et al.1994) may prevent any further glycosylation of S4 in the Golgi.
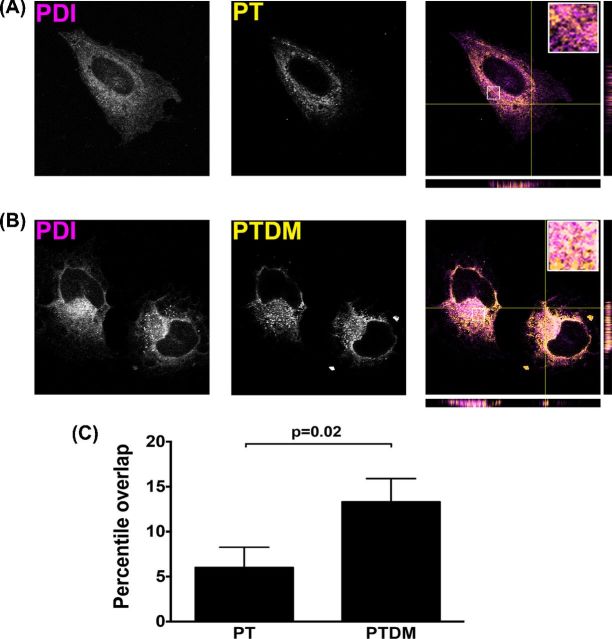
Visualization of intracellular PTDM
Prior efforts to visualize PT in the ER in mammalian cells incubated with PT were unsuccessful (Plaut and Carbonetti 2008), probably because of the transient presence of low levels of PT in the ER in its trafficking pathway. We hypothesized that PTDM might be visualized in the ER if it is trapped and accumulates there due to its inability to undergo ATP-mediated dissociation. To determine whether PTDM could be visualized in the ER, HeLa cells were exposed to 20 nM purified native PT or PTDM for 3 h, and indirect immunofluorescence microscopy was performed. Native toxin exhibited a staining pattern that had very little colocalization with the ER marker PDI (Fig. 6A). In contrast, PTDM was seen in a pattern that had significantly greater colocalization with PDI (Fig. 6B and C). This result is consistent with the hypothesized inability of PTDM to dissociate in the ER, because the holotoxin would accumulate in this organelle to a greater extent than would native PT, allowing its presence there to be visualized by this method. Furthermore, these data indicate that the cellular intoxication pathway for PT is indeed this retrograde pathway through the ER, allowing access of the toxin to the cytosol, rather than any uncharacterized pathway to the cytosol that does not involve the ER.
Figure 6.
Colocalization of PTDM and ER markers. HeLa cells were treated with 20 nM native PT (A) or PTDM (B) for 3 h, fixed and permeabilized. Cells were then stained with a rabbit polyclonal antibody to PT and with a mouse monoclonal antibody to the ER marker PDI. Secondary antibodies were Alexa Fluor 488 goat anti-mouse IgG (pseudocolored magenta) and Alexa Fluor 594 goat anti-rabbit IgG (pseudocolored yellow). The inserts show an enlarged area from each to emphasize the difference in the extent of colocalization. (C) The percentage colocalization (overlap) was determined using the GDSC Stack Colocalization Analyser plugin for ImageJ (n = 3).
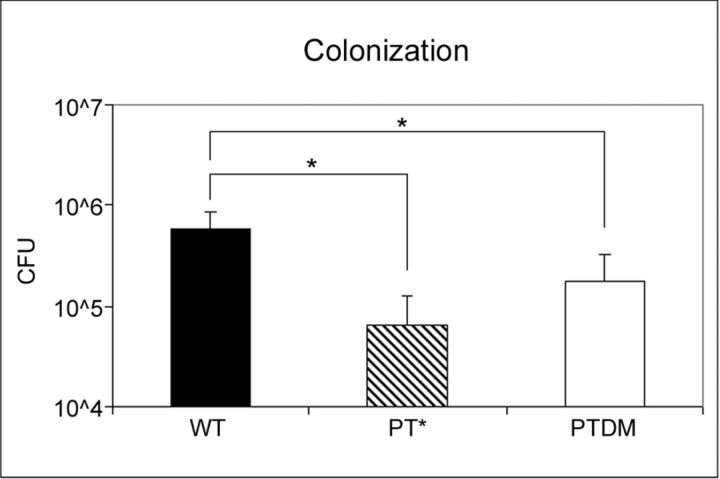
Respiratory tract colonization of mice by W28 PTDM
Strains of B. pertussis either lacking PT or producing an enzymatically inactive form of PT (PT-9K/129G; Pizza et al.1989) exhibit reduced respiratory tract colonization in a mouse model of infection (Carbonetti et al.2003). To test whether the PTDM changes have an effect on the virulence of B. pertussis in vivo, BALB/c mice were inoculated intranasally with either wild-type W28 (WT), W28 PT-9K/129G (PT*) or W28 PTDM strains, and bacterial loads in the respiratory tract were assayed 4 days post-inoculation. As shown in Fig. 7, W28 PTDM exhibited a statistically significant defect in colonization of the mouse respiratory tract compared to WT (p < 0.02). Colonization of W28 PTDM was not significantly different from that of W28 PT-9K/129G (p = 0.14). These results indicate that the modifications to S5 that were engineered in PTDM led to loss of the colonization-enhancing effect of PT, consistent with the results of the in vitro and cellular activity assays.
Figure 7.
Colonization of mouse respiratory tract. BALB/c mice were inoculated intranasally with 5 × 105 CFU of either wild-type W28 (WT), W28 PT-9K/129G (PT*) or W28 PTDM B. pertussis strains, and bacterial loads in the respiratory tract were assayed 4 days post-inoculation. n = 5 mice per treatment group. Asterisks indicate statistically significant differences by t test (p < 0.02).
DISCUSSION
The results presented here support the hypothesis that PT holotoxin dissociation is stimulated by its interaction with ATP in the ER. Furthermore, the results indicate that this event is necessary for the cellular activity of PT, providing further evidence that passage of PT through the ER is part of its cellular intoxication pathway.
Changes were made to two of the amino acid residues of S5 that are thought to be involved in the interaction between PT and ATP (Table 1), based on the crystal structure (Hazes et al.1996). The glycine residue at position 58, which interacts with the alpha phosphate of ATP, was replaced with asparagine. The serine residue at position 62, which forms a hydrogen bond with N-7 of the adenine ring of ATP, was replaced with glutamate. In both cases, the residues chosen to replace the native residues of S5 were intended to provide steric hindrance to the interaction between PT and ATP.
In contrast to native PT, incubation in vitro of a form of PT with changes to two residues in S5 (PTDM) with increasing concentrations of ATP did not lead to an increase in the amount of S1 released from the holotoxin (Fig. 4). The changes to these two residues inhibited the interaction of PT holotoxin with ATP, preventing holotoxin dissociation and/or preventing conformational changes required for cleavage of the disulfide bond in S1. Similarly, in an in vitro activity assay, concentrations of ATP that stimulated the ADP-ribosylation activity of native PT did not stimulate the activity of PTDM (Fig. 1); in fact, this form of PT was not active in vitro at any concentration of ATP tested. The correlation between the failure of PTDM to dissociate and to be activated by exposure to ATP is consistent with previous reports indicating the importance of its interaction with ATP for stimulating PT dissociation and activation (Moss et al.1983, 1986; Burns and Manclark 1986; Hausman, Manclark and Burns 1990; Krueger and Barbieri 1993).
The interaction between PT and ATP has been hypothesized previously to be an important event for the intracellular dissociation of the holotoxin (Moss et al.1986; Hazes et al.1996). While in vitro interaction with ATP has been found to stimulate dissociation of native PT (Burns and Manclark 1986), in that study, extensive dissociation occurred only if the detergent CHAPS was included in the reaction. In the absence of CHAPS, another group found that only 8%–20% of holotoxin was dissociated following the interaction of PT with ATP in vitro (Krueger and Barbieri 1993). Rather than directly causing dissociation, the binding event may destabilize the holotoxin by disrupting contacts between S1 and the B oligomer (Burns and Manclark 1986; Krueger and Barbieri 1993; Hazes et al.1996). Dissociation may require subsequent steps in cells (substituted for CHAPS in vitro), such as binding of PT to membranes or ER chaperones and/or cleavage of the disulfide bond in S1; these events may not be possible without prior destabilization of the holotoxin by ATP (Hazes et al.1996).
In this study, the cellular ADP-ribosylation activities of the different forms of PT listed in Table 1 were assessed. PT with a substitution at either residue 58 or 62 of S5 was partially reduced in activity compared to wild-type PT, whereas changes to both residues led to complete inhibition of cellular activity at the concentration of toxin used (Fig. 1). These results are in line with the model of PT retrograde transport to the ER, followed by translocation of S1 to the cytosol, because S1 translocation across the ER membrane may require prior dissociation from the B oligomer. Thus, inhibition of holotoxin dissociation would lead to reduction of S1 translocation to the cytosol and therefore a decrease in activity, as the amount of S1 that reaches its G protein targets on the inner surface of the host cell plasma membrane would be reduced.
The addition of target sites for tyrosine sulfation and N-glycosylation to either the S1 or S4 subunit of PTDM allowed studies of the transport of this form of PT. The organelle-specific modifications of toxin subunits detected in sulfation assays with PTS1GSDM and PTS4GSDM (Fig. 5) confirmed that the reduction in the cellular activity of this form of PT (compared to native PT) was not due to failure to be transported to the TGN or ER. This suggests that the defect in cellular activity was caused by altered transport of S1 beyond its arrival in the ER; according to the model, translocation out of the ER is the critical step that S1 in PTDM does not undergo, because of a failure to dissociate from the B oligomer.
The different glycosylation patterns of our recombinant toxins are indicative of different ER-localized processing events for the DM and native toxins. Sulfated PTS1GSDM was N-glycosylated to a greater extent than sulfated PTS1GS (Fig. 5A), suggesting that the lack of PTS1GSDM disassembly led to its retention in the ER and increased availability of its S1 subunit for core N-glycosylation. This result is comparable to the results of a study using a form of cholera toxin (CT) with ablation of the cleavage site on the A subunit and with an N-glycosylation target sequence on the B subunit (Fujinaga et al.2003). The A subunit from this form of CT co-immunoprecipitated with CT B subunits that were N-glycosylated in the ER, whereas this did not occur with CT containing the native cleavage site on the A subunit. The similar approach used in this study confirmed that dissociation of PT, like that of CT, occurs in the ER. Moreover, the extensive Golgi-localized glycosylation of S4 observed when cells were incubated with PTS4GS was not seen with PTS4GSDM (Fig. 5B). Two possibilities could explain this last result: either S4 that has not dissociated from the other subunits is not transported anterograde to the Golgi after arrival in the ER or S4 in intact holotoxin that is transported in this way cannot be glycosylated in the Golgi, because of the proximity in the holotoxin of S1 to the C-terminus of S4 (where the N-glycosylation target site is located in this form of PT; Stein et al.1994). Further investigation would be required to distinguish between these two possibilities, but in either case, the results are consistent with a failure of this form of PT to dissociate.
Indirect immunofluorescence microscopy also provided evidence of PT transport to the ER. Colocalization of native PT with the ER marker PDI was not observed; in contrast, PTDM colocalized extensively with PDI (Fig. 6). These results are consistent with inhibition of PT dissociation leading to its accumulation in the ER. Additionally, these results suggest that the difficulty in detection of wild-type PT in the ER by indirect immunofluorescence microscopy is due to its low level and transient presence in this organelle, rather than to any defect in binding of the polyclonal antibody to PT in the environment of the ER.
Exposed hydrophobic regions of misfolded proteins in the ER are thought to target the proteins for degradation by ERAD (Ellgaard and Helenius 2003). For PT, residues 184–203 of S1 form a hydrophobic sequence (Stein et al.1994), the exposure of which may target S1 for export from the ER (Hazes and Read 1997). Reduction of the disulfide bond linking the cysteines at residues 41 and 201 of S1 and/or dissociation of S1 from the B oligomer may expose this sequence, and these events may require prior destabilization of PT by interaction of the holotoxin with ATP (Hazes et al.1996). Thus, for the form of PT in this study with two changes to the ATP binding site, an inability to dissociate likely prevented exposure of the sequence that could target S1 for export from the ER, leading to the detected loss in cytotoxicity. This hypothesis is contradicted by the cytotoxic activity detected in cells expressing residues 1–180 of S1 with an ER signal peptide (Castro, McNamara and Carbonetti 2001), which suggests that the hydrophobic sequence in residues 184–203 is not required for translocation of S1 to the cytosol; however, the question remains open, because of the artificially high overexpression of S1 in the transfectants in that study.
The intrinsic instability of the S1 subunit provides an alternative potential mechanism for its translocation to the cytosol. Whereas the PT holotoxin is a stable complex (Krell et al. 2003), the isolated S1 subunit is a thermally unstable protein with a highly disordered conformation at 37°C (Pande et al.2006). PT disassembly in the ER would thus lead to the unfolding of dissociated S1 and its ERAD-directed export to the cytosol. In further support of this model, conditions that prevent the thermal unfolding of free S1 also block its entry into the cytosol and protect cultured cells from PT intoxication (Banerjee, Cilenti, Taylor, Showman, Tautlian and Teter, manuscript in preparation). An interaction with NAD or other host factors may promote the refolding of cytosolic S1 to an active state (Pande et al.2006). S1 lacks the lysine residues required for ubiquitin conjugation and thus evades the ubiquitin-dependent proteasomal degradation that clears most ERAD substrates from the cytosol (Hazes and Read 1997; Worthington and Carbonetti 2007).
In this study, analysis of the activity of forms of PT with substitutions in residues that are important in the interaction of PT with ATP provided evidence that cellular intoxication of cells by PT requires interaction of the holotoxin with ATP. Additionally, sulfation assays demonstrated that subunits of forms of PTDM with added peptide tags were transported to the TGN and ER, and the observed altered patterns of N-glycosylation of the subunits were consistent with a failure of the holotoxin to dissociate in the ER. These results provide evidence that the intracellular transport pathway involving retrograde transport to the ER and subsequent translocation of S1 to the cytosol is the cellular intoxication pathway of PT.
Acknowledgments
We thank Ria Achong-Bowe and Charlotte Andreasen for technical assistance and Randy Read for helpful advice.
FUNDING
This work was supported by the National Institute of Allergy and Infectious Diseases [grant numbers AI50022 and AI063080 to NHC and grant number AI099493 to KT].
Conflict of interest. None declared.
REFERENCES
- Andreasen C, Powell DA, Carbonetti NH. Pertussis toxin stimulates IL-17 production in response to Bordetella pertussis infection in mice. PLoS One. 2009;4:e7079. doi: 10.1371/journal.pone.0007079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan MJ, David JL, Kenimer JG, et al. Lectin-like binding of pertussis toxin to a 165-kilodalton chinese hamster ovary cell glycoprotein. J Biol Chem. 1988;263:4895–9. [PubMed] [Google Scholar]
- Burns DL, Manclark CR. Adenine nucleotides promote dissociation of pertussis toxin subunits. J Biol Chem. 1986;261:4324–7. [PubMed] [Google Scholar]
- Carbonetti NH. Immunomodulation in the pathogenesis of Bordetella pertussis infection and disease. Curr Opin Pharmacol. 2007;7:272–8. doi: 10.1016/j.coph.2006.12.004. [DOI] [PubMed] [Google Scholar]
- Carbonetti NH, Artamonova GV, Andreasen C, et al. Pertussis toxin and adenylate cyclase toxin provide a one-two punch for establishment of Bordetella pertussis infection of the respiratory tract. Infect Immun. 2005a;73:2698–703. doi: 10.1128/IAI.73.5.2698-2703.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonetti NH, Artamonova GV, Mays RM, et al. Pertussis toxin plays an early role in respiratory tract colonization by Bordetella pertussis. Infect Immun. 2003;71:6358–66. doi: 10.1128/IAI.71.11.6358-6366.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonetti NH, Mays RM, Artamonova GV, et al. Proteolytic cleavage of pertussis toxin S1 subunit is not essential for its activity in mammalian cells. BMC Microbiol. 2005b;5:7. doi: 10.1186/1471-2180-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro MG, McNamara U, Carbonetti NH. Expression, activity and cytotoxicity of pertussis toxin S1 subunit in transfected mammalian cells. Cell Microbiol. 2001;3:45–54. doi: 10.1046/j.1462-5822.2001.00092.x. [DOI] [PubMed] [Google Scholar]
- Connelly C, Sun Y, Carbonetti NH. Pertussis toxin exacerbates and prolongs airway inflammatory responses during Bordetella pertussis infection. Infect Immun. 2012;80:4317–32. doi: 10.1128/IAI.00808-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellgaard L, Helenius A. Quality control in the endoplasmic reticulum. Nat Rev Mol Cell Bio. 2003;4:181–91. doi: 10.1038/nrm1052. [DOI] [PubMed] [Google Scholar]
- Fujinaga Y, Wolf AA, Rodighiero C, et al. Gangliosides that associate with lipid rafts mediate transport of cholera and related toxins from the plasma membrane to endoplasmic reticulum. Mol Biol Cell. 2003;14:4783–93. doi: 10.1091/mbc.E03-06-0354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausman SZ, Manclark CR, Burns DL. Binding of ATP by pertussis toxin and isolated toxin subunits. Biochemistry. 1990;29:6128–31. doi: 10.1021/bi00478a003. [DOI] [PubMed] [Google Scholar]
- Hazes B, Boodhoo A, Cockle SA, et al. Crystal structure of the pertussis toxin-ATP complex: A molecular sensor. J Mol Biol. 1996;258:661–71. doi: 10.1006/jmbi.1996.0277. [DOI] [PubMed] [Google Scholar]
- Hazes B, Read RJ. Accumulating evidence suggests that several AB-toxins subvert the endoplasmic reticulum-associated protein degradation pathway to enter target cells. Biochemistry. 1997;36:11051–4. doi: 10.1021/bi971383p. [DOI] [PubMed] [Google Scholar]
- Katada T, Tamura M, Ui M. The A protomer of islet-activating protein, pertussis toxin, as an active peptide catalyzing ADP-ribosylation of a membrane protein. Arch Biochem Biophys. 1983;224:290–8. doi: 10.1016/0003-9861(83)90212-6. [DOI] [PubMed] [Google Scholar]
- Kinnear SM, Boucher PE, Stibitz S, et al. Analysis of BvgA activation of the pertactin gene promoter in Bordetella pertussis. J Bacteriol. 1999;181:5234–41. doi: 10.1128/jb.181.17.5234-5241.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krell T, Greco F, Nicolai MC, et al. The use of microcalorimetry to characterize tetanus neurotoxin, pertussis toxin and filamentous haemagglutinin. Biotechnol Appl Bioc. 2003;38:241–51. doi: 10.1042/BA20030089. [DOI] [PubMed] [Google Scholar]
- Krueger KM, Barbieri JT. Molecular characterization of the in vitro activation of pertussis toxin by ATP. J Biol Chem. 1993;268:12570–8. [PubMed] [Google Scholar]
- Lim LK, Sekura RD, Kaslow HR. Adenine nucleotides directly stimulate pertussis toxin. J Biol Chem. 1985;260:2585–8. [PubMed] [Google Scholar]
- Mattera R, Codina J, Sekura RD, et al. The interaction of nucleotides with pertussis toxin. Direct evidence for a nucleotide binding site on the toxin regulating the rate of ADP-ribosylation of Ni, the inhibitory regulatory component of adenylyl cyclase. J Biol Chem. 1986;261:11173–9. [PubMed] [Google Scholar]
- Moss J, Stanley SJ, Burns DL, et al. Activation by thiol of the latent NAD glycohydrolase and ADP-ribosyltransferase activities of Bordetella pertussis toxin (islet-activating protein) J Biol Chem. 1983;258:11879–82. [PubMed] [Google Scholar]
- Moss J, Stanley SJ, Watkins PA, et al. Stimulation of the thiol-dependent ADP-ribosyltransferase and NAD glycohydrolase activities of Bordetella pertussis toxin by adenine nucleotides, phospholipids, and detergents. Biochemistry. 1986;25:2720–5. doi: 10.1021/bi00357a066. [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay S, Linstedt AD. Retrograde trafficking of AB5 toxins: mechanisms to therapeutics. J Mol Med. 2013;91:1131–41. doi: 10.1007/s00109-013-1048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pande AH, Moe D, Jamnadas M, et al. The pertussis toxin S1 subunit is a thermally unstable protein susceptible to degradation by the 20S proteasome. Biochemistry. 2006;45:13734–40. doi: 10.1021/bi061175+. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizza M, Covacci A, Bartoloni A, et al. Mutants of pertussis toxin suitable for vaccine development. Science. 1989;246:497–500. doi: 10.1126/science.2683073. [DOI] [PubMed] [Google Scholar]
- Plaut RD, Carbonetti NH. Retrograde transport of pertussis toxin in the mammalian cell. Cell Microbiol. 2008;10:1130–9. doi: 10.1111/j.1462-5822.2007.01115.x. [DOI] [PubMed] [Google Scholar]
- Rapak A, Falsnes PO, Olsnes S. Retrograde transport of mutant ricin to the endoplasmic reticulum with subsequent translocation to the cytosol. P Natl Acad Sci USA. 1997;94:3783–8. doi: 10.1073/pnas.94.8.3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scanlon KM, Gau Y, Skerry C, et al. The epithelial anion transporter pendrin contributes to inflammatory lung pathology in Bordetella pertussis infection. Infect Immun. 2014;82:4212–21. doi: 10.1128/IAI.02222-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spooner RA, Smith DC, Easton AJ, et al. Retrograde transport pathways utilised by viruses and protein toxins. Virol J. 2006;3:26. doi: 10.1186/1743-422X-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein PE, Boodhoo A, Armstrong GD, et al. The crystal structure of pertussis toxin. Structure. 1994;2:45–57. doi: 10.1016/s0969-2126(00)00007-1. [DOI] [PubMed] [Google Scholar]
- Stibitz S, Yang MS. Subcellular localization and immunological detection of proteins encoded by the vir locus of Bordetella pertussis. J Bacteriol. 1991;173:4288–96. doi: 10.1128/jb.173.14.4288-4296.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamura M, Nogimori K, Murai S, et al. Subunit structure of islet-activating protein, pertussis toxin, in confosrmity with the A-B model. Biochemistry. 1982;21:5516–22. doi: 10.1021/bi00265a021. [DOI] [PubMed] [Google Scholar]
- Taylor M, Banerjee T, Ray S, et al. Protein disulfide isomerase displaces the cholera toxin A1 subunit from the holotoxin without unfolding the A1 subunit. J Biol Chem. 2011;286:22090–100. doi: 10.1074/jbc.M111.237966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner ED, Brodsky JL, McCracken AA. Proteasome-dependent endoplasmic reticulum-associated protein degradation: An unconventional route to a familiar fate. P Natl Acad Sci USA. 1996;93:13797–801. doi: 10.1073/pnas.93.24.13797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witvliet MH, Burns DL, Brennan MJ, et al. Binding of pertussis toxin to eucaryotic cells and glycoproteins. Infect Immun. 1989;57:3324–30. doi: 10.1128/iai.57.11.3324-3330.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worthington ZEV, Carbonetti NH. Evading the proteasome: absence of lysine residues contributes to pertussis toxin activity by evasion of proteasome degradation. Infect Immun. 2007;75:2946–53. doi: 10.1128/IAI.02011-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y, Barbieri JT. Pertussis toxin-mediated ADP-ribosylation of target proteins in Chinese hamster ovary cells involves a vesicle trafficking mechanism. Infect Immun. 1995;63:825–32. doi: 10.1128/iai.63.3.825-832.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]