Abstract
Aim
Laparoscopic adjustable gastric banding (LAGB) migration is an uncommon late complication after bariatric surgery. It usually presents with an unexplained weight increase or without any symptom. Current guidelines do not establish the timing of a clear endoscopic follow-up to prevent and/or to treat this kind of complication.
Patients and methods
Long-term follow-up was performed in 217 patients with LAGB (37 underwent surgery in other bariatric centers). At the endoscopic check, 3 patients presented banding erosion respectively 7, 9 and 11 years after surgery. In all three cases the patients, lost at the follow-up in their bariatric centers, had weight gain. During the endoscopy was treated just one patient because of the advanced migration. For the other patients, with a minimal migration, the choice was to perform an endoscopic surveillance every 4 months.
Discussion
Removal of eroded gastric banding with common endoscopic devices is feasible, safe, and effective.
Conclusion
With our experience we suggest to perform planned endoscopy at least within 2 years in order to guarantee the early diagnosis and managing of gastric banding erosion.
Keywords: Bariatric surgery, Gastric banding migration, Obesity, Endoscopy
Introduction
Laparoscopic adjustable gastric banding (LAGB) is one of the first-line treatment options in bariatric surgery (1).
Although it is a safe and easy performing procedure, there are serious associated complications such as banding erosion through the stomach wall, band slippage and associated pouch dilatation, gastric wall perforation, abscess formation (2).
The banding migration into the stomach lumen could be easily individuated and, in selected cases, treated by an upper endoscopy (1, 3).
Current guidelines do not establish the timing of a clear endoscopic follow-up to prevent and/or to treat complications (4).
We present an experience of evaluation and managing LAGB erosion.
Patients and methods
Long-term follow-up was performed in 217 patients with LAGB. Out of 217, 37 patients underwent surgery in other bariatric centers.
Three of these patients, lost at the follow-up in their bariatric centers and evaluated for the first time in the last year, presented banding erosion respectively 7, 9 and 11 years after surgery. All three cases had weight gain, without any other symptom or sign.
Just one of these, a 36-year old woman was treated by an endoscopic procedure in January 2017.
Upon admission, her vital signs were normal.
Her weight increased of 15 Kg in the last 2 years and was completely asymptomatic for gastroesophageal reflux or stomach ache. Furthermore she did not take part to endoscopic follow-up checks in the last 4 years. Blood tests proved only a slight increase in white blood cells.
In September 2016 the patient had a port-site infection on the upper left quadrant of the abdomen and as first approach the device was removed leaving the port-tube on site.
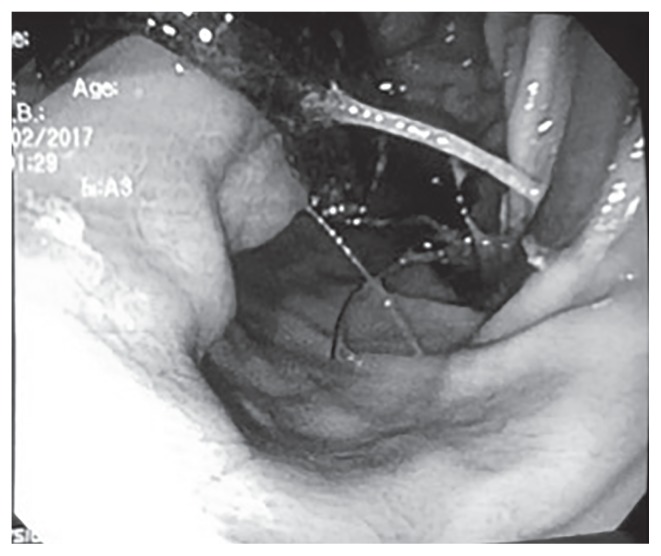
After 4 months she came at our attention and then, with a mild sedation, we performed a gastroscopy that showed the erosion of gastric wall and that 4/5 of the banding migrated inside the antrum (Figure 1).
Figure 1.
Migration of 4/5 of the banding and port tube connection in the gastric antrum.
Even the closure buckle and the port-tube connection were totally migrated inside the stomach.
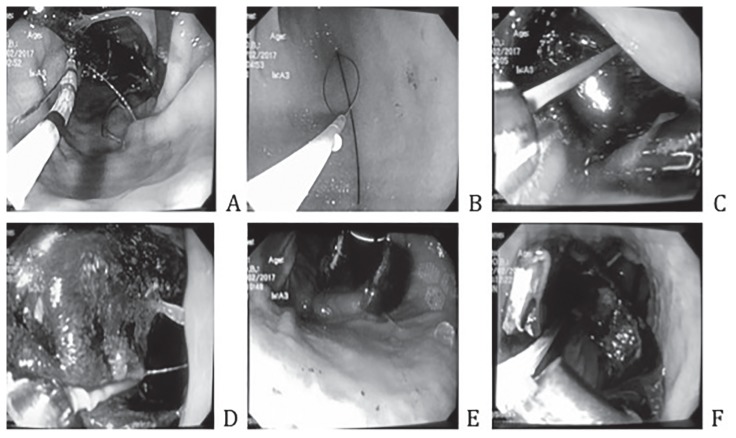
We passed a guidewire (0,035 Hydra Jagwire-Boston Scientific) through a standard endoscope (Olympus GIF-Q-165) between the gastric wall and the banding using a sphincterotome (TRI-20 sphincterotome – COOK medical) in order to obtain a loop (Figure 2 A, B, C). We put the Sohendra’s lithotripter on the guidewire tightening and cutting the banding (Figure 2 D, E, F).
Figure 2.
Banding removal phases.
Then the device was pulled off using endoscopic polipectomy snare (Captivator 13 mm - Boston Scientific) (Figure 3).
Figure 3.
Pulled off banding.
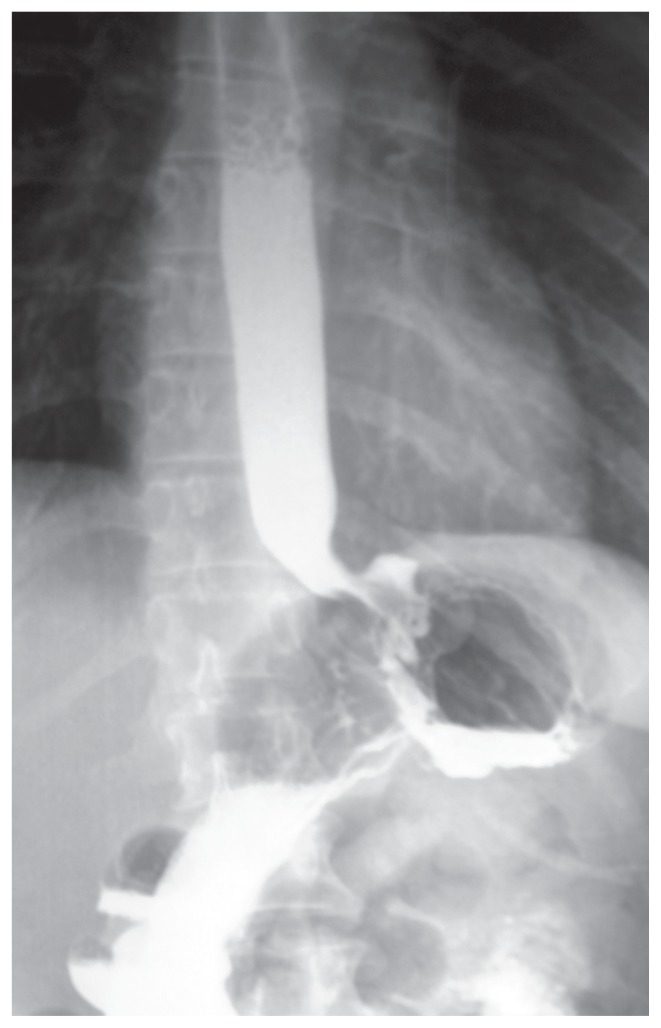
To evaluate the integrity of the stomach and the oesophagus, the day after the endoscopic procedure, a Gastrografin Swallow was performed. It showed a mild thinning of the gastric wall but no evidence of fistulas or spreading of the contrast agent (Figure 4).
Figure 4.
Gastrografin swallow.
Results
The procedure time was 10 minutes. There was no blood loss. After two days the patient was discharged taking anti-reflux, PPI (proton pump inhibitors) and antiemetics drugs. For the other two patients with a partial and minimal migration, the choice was to perform an endoscopic surveillance every 4 months.
Discussion
LAGB is considered a safe and effective method of weight loss and reduction of comorbidities associated with obesity.
It is one of the most common methods of bariatric surgery (1, 6). It allows to adjust the size of the band, and to restore previous anatomy if band removal is required (7).
However, postoperative complications, such as pouch enlargement, band slip, band erosion, port-site infections and port breakage are possible, and their management, including the use of endoscopic procedures, has become important (2, 8, 9).
Band erosion is an uncommon complication of LAGB. The incidence is less than 1% (10) with a reported prevalence varying from 0% to 11% (11).
It usually presents as a late complication with an unexplained weight increase or without any symptom. Furthermore, patients should be informed of all risks associated to LAGB in order to implement their attendance at follow-up.
According to current guidelines a clinical follow-up should be performed every 3 months during the first year and then once a year. Instead the endoscopy is advised only if clinical examination is suggestive (4).
This kind of scheduling doesn’t allow the prompt individuation of every complication as the banding migration in asymptomatic patients.
Even if different approaches are shown in literature, endoscopic procedure in the post-bariatric follow-up is a valid possibility to diagnose and treat complications (1, 3, 9, 12, 13).
First of all, endoscopy allows to assess the stage of migration.
In the stage I a small part of band is visible in the gastric lumen, in the stage II more than half of the band is migrated in the gastric lumen, stage III corresponds to a complete migration of the band and connecting tube into the stomach (14). In the case of an asymptomatic patient, with a partial migration, could be appropriate to wait a full band migration into the stomach, making easier the endoscopic removal of the device (14, 15).
In our experience, we reported that a migrated banding can be individuated and removed using common devices present in each endoscopy centre. This kind of approach is the key to obtain a quick resumption of oral feeding and rapid discharge of the patients (9, 16).
Conclusion
Since band erosion is an asymptomatic complication, patients with LAGB should undergo gastroscopy checks at least once every two years. Removal of eroded gastric banding with common endoscopic devices is feasible, safe, and effective. In case of minimal migration, could be suitable an endoscopic surveillance every 4 months.
References
- 1.Chisholm J, et al. Gastric band erosion in 63 cases: endoscopic removal and rebanding evaluated. Obes Surg. 2011;21(11):1676–81. doi: 10.1007/s11695-011-0468-0. [DOI] [PubMed] [Google Scholar]
- 2.Sonavane SK, et al. Laparoscopic adjustable gastric banding: what radiologists need to know. Radiographics. 2012;32(4):1161–78. doi: 10.1148/rg.324115177. [DOI] [PubMed] [Google Scholar]
- 3.Dogan UB, et al. Endoscopic management of gastric band erosions: a 7-year series of 14 patients. Can J Surg. 2014;57(2):106–11. doi: 10.1503/cjs.001313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fried M, et al. Interdisciplinary European Guidelines on metabolic and bariatric surgery. Obes Facts. 2013;6(5):449–68. doi: 10.1159/000355480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Coq B, et al. Impact of Surgical Technique on Long-term Complication Rate After Laparoscopic Adjustable Gastric Banding (LAGB): Results of a Single-blinded Randomized Controlled trial (ANOSEAN Study) Ann Surg. 2016;264(5):738–744. doi: 10.1097/SLA.0000000000001835. [DOI] [PubMed] [Google Scholar]
- 6.Buchwald H, Oien DM. Metabolic/bariatric surgery Worldwide 2008. Obes Surg. 2009;19(12):1605–11. doi: 10.1007/s11695-009-0014-5. [DOI] [PubMed] [Google Scholar]
- 7.Dixon JB, Dixon ME, O’Brien PE. Pre-operative predictors of weight loss at 1-year after Lap-Band surgery. Obes Surg. 2001;11(2):200–7. doi: 10.1381/096089201321577884. [DOI] [PubMed] [Google Scholar]
- 8.Joo MK. Endoscopic Approach for Major Complications of Bariatric Surgery. Clin Endosc. 2017;50(1):31–41. doi: 10.5946/ce.2016.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mozzi E, et al. Treatment of band erosion: feasibility and safety of endoscopic band removal. Surg Endosc. 2011;25(12):3918–22. doi: 10.1007/s00464-011-1820-0. [DOI] [PubMed] [Google Scholar]
- 10.O’Brien PE, Dixon JB. Weight loss and early and late complications--the international experience. Am J Surg. 2002;184(6B):42S–45S. doi: 10.1016/s0002-9610(02)01179-0. [DOI] [PubMed] [Google Scholar]
- 11.Abu-Abeid S, Szold A. Laparoscopic management of Lap-Band erosion. Obes Surg. 2001;11(1):87–9. doi: 10.1381/096089201321454169. [DOI] [PubMed] [Google Scholar]
- 12.Boules M, et al. Endoscopic management of post-bariatric surgery complications. World J Gastrointest Endosc. 2016;8(17):591–9. doi: 10.4253/wjge.v8.i17.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blero D, et al. Endoscopic removal of dysfunctioning bands or rings after restrictive bariatric procedures. Gastrointest Endosc. 2010;71(3):468–74. doi: 10.1016/j.gie.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 14.Nocca D, et al. Migration of adjustable gastric banding from a cohort study of 4236 patients. Surg Endosc. 2005;19(7):947–50. doi: 10.1007/s00464-004-2183-6. [DOI] [PubMed] [Google Scholar]
- 15.Lantsberg L, et al. Jejunal obstruction caused by migrated gastric band. Obes Surg. 2008;18(2):225–7. doi: 10.1007/s11695-007-9380-z. [DOI] [PubMed] [Google Scholar]
- 16.Kim SY, et al. Endoscopic Treatment of Diverse Complications Caused by Laparoscopic Adjustable Gastric Banding: A Study in Eastern Asia. Gut Liver. 2017 doi: 10.5009/gnl16089. [DOI] [PMC free article] [PubMed] [Google Scholar]