Abstract
In skilled home health care (SHHC), communication between nurses and physicians is often inadequate for medication reconciliation and needed changes to the medication regimens are rarely made. Fragmentation of electronic health record (EHR) systems, transitions of care, lack of physician-nurse in-person contact and poor understanding of medications by patients and their families put patients at risk for serious adverse outcomes. The aim of this study was to develop and test the HOME tool, an informatics tool to improve communication about medication regimens, share the insights of home care nurses with physicians, and highlight to physicians and nurses the complexity of medication schedules. We used human computer interaction design and evaluation principles, automated extraction from standardized forms, and modification of existing EHR fields to highlight key medication-related insights that had arisen during the SHHC visit. Separate versions of the tool were developed for physicians/nurses and patients/caregivers. A pilot of the tool was conducted using 20 SHHC encounters. Home care nurses and physicians found the tool useful for communication. Home care nurses were able to implement the HOME tool into their clinical workflow and reported improved communication with physicians about medications. This simple and largely automated tool improves understanding and communication around medications in SHHC.
Background
Older adults in the United States who receive skilled home health care (SHHC) are a particularly vulnerable population who are at high risk for adverse events, hospitalizations, and functional decline. Over half of all patients who receive SHHC have recently been in the hospital (Jones, Harris Kojetin & Valverde, 2012; Wolff et al., 2008). After returning home from a hospital admission, patients frequently have problems with new treatment regimens and are confused by medication changes (Brody et al.,2016; Kripalani, Jackson, Schnipper & Coleman, 2007; Kripalani et al., 2012). During the course of inpatient hospitalization, changes to prescribed medications are often made (Muir, Sanders, Wilkinson & Schmader, 2002) and may not be communicated adequately to the patient or their usual care providers. Although patients who receive SHHC tend to be highly vulnerable with significant comorbidity (Brody et al.,2016), more than one-third (34.6%) of Medicare beneficiaries receiving SHHC do not incur any physician evaluation and management visits during their 60-day home health episode (Wolff et al., 2009). One opportunity to improve medication-related outcomes is by improving communication between older adults, their families, home health agencies and primary care physicians.
Medication reconciliation in SHHC focuses on ensuring that the list of medications prescribed during the hospital discharge is reconciled with the medications in the home, with any discrepancies or serious drug interactions clarified (Brody et al.,2016) in close collaboration with the patient’s primary care physician (PCP). However, the post-discharge medication reconciliation process is often conducted in the absence of meaningful and effective communication between the PCP and the home health nurse who visits the patient in their home (Press et al., 2015). Recent work in a large home health agency found that all patients recently discharged from the hospital to SHHC had at least one medication discrepancy (Brody et al.,2016). Polypharmacy was very common in the population studied; the median number of unique medications was 15.
Medication reconciliation ensures that the patient has a correct list of medications but many other issues affect the ability of the patient to successfully take those medications. Home care nurses gain important insights into both medication regimen complexity and patient and family perspectives while they are in the patient’s home. These insights are also often not communicated to the PCP and, therefore, additional changes to the medication regimen are rarely made (Smith et al., 2016). This may hinder the effort of many families who are involved in the complex task of medication management for older adults who receive SHHC services (Giovannetti et al, 2012; Wolff, Boyd, Gitlin, Bruce & Roter, 2012; Wolff et al., 2014). Indeed, overseeing medication regimens is very stressful for families, and they report feeling inadequately prepared for this role ([Smith et al., 2016; Reinhard, Levine & Samis, 2012; Travis et al., 2006).
Currently in the United States, the home care nurse collects information to complete the CMS-485 home health certification and plan of care (hereafter abbreviated to the CMS-485 form). The certification/POC is sent to the physician to sign in order for the home health agency (HHA) to implement the plan of care and be reimbursed by the Centers for Medicare and Medicaid Services (CMS). The CMS-485 form itself does not meaningfully engage physicians in the care of the patient either through its format or the way in which data are presented. The CMS-485 uses very small font, plans of care are presented in bureaucratic language and unsynthesized medication lists, and does not afford a mechanism for the nurse to convey important information relevant to the care of the patient (Siegler et al., 2006). The CMS-485 forms are paperwork the physician must sign, often with no or minimal review (Siegler et al., 2006). Home care nurses report to us that important information they capture and enter in the home health EHR that would help the physician reduce medication regimen complexity and improve the care of patients is not conveyed at all, or conveyed ineffectively at best in the current CMS-485 form.
Strategies to reduce medication regimen complexity have been evaluated within the inpatient setting (Muir et al., 2002; Elliott, O’Callaghan, Paul & George, 2013). Highlighting complexity of medication regimens to physicians has been demonstrated to lead to simplification of timing, dose reduction and discontinuation of harmful or unnecessary medications (Muir et al., 2002). However, such strategies have not been scaled widely, and may miss important information gained by a visit to the home that includes conversations with the patient, his or her family, and the information the home visit itself provides (e.g., where medications are stored, if patient can open medication bottles or organizers, if patient needs verbal or written reminders, if family is able to assist in medication management). Interventions to promote patient participation in medication management have been shown to be acceptable and potentially useful for improving patient outcomes and reducing costs (Greene & Hibbard, 2012). Health Information Technology (HIT) offers solutions to improve care and outcomes for older adults, (Bowles, Dykes & Demiris, 2015) with some effective examples including improved documentation of falls, pressure ulcer and nutritional risk assessments leading to reduced incidence of pressure ulcers and increased guideline adherence through the use of the Electronic Medical Record (EMR) (Dowding, Turley & Garrido, 2012; Dykes et al., 2010; Fossum, Alexander, Ehnfors & Ehrenberg, 2011). Both the Health Information Technology for Economic and Clinical Health (HITECH) Act (Blumenthal, 2010) and Institute of Medicine report (2011) have called for the implementation of emerging HIT solutions to improve the safety, quality and efficiency of care.
Skilled home health care is a critical setting in the care of older adults who are particularly vulnerable to transitions of care, such as post-hospital discharge. We set out to: a.) design and develop a largely automated informatics solution (the HOME tool) to efficiently and clearly communicate information about medication regimens and insights gained in the process of evaluating the patient at home and encourage simplification of medication regimens and b.) test the usability and feasibility of the HOME tool among home care nurses, PCPs, and patients/families in SHHC.
Methodology
Prototype Design
A user experience company was employed to help understand what nurses, PCPs, and patients/families would need to make the HOME tool useful, usable and appealing. Three months of initial consultation took place between the user experience company and the HOME-tool research team made up of geriatricians, SHHC nurses and experts in both HIT and the patient/family caregiver experience. Key concepts were explained and explored including a.) the current system of communication around medications and need for accurate timely communication during transitions of care b.) the importance of simplification of medication regimens c.) the difference between next of kin and the person who helps the patient with medication and d.) the importance of patients and caregivers understanding the medication regimen and knowing who to contact with medication questions and how to contact them.
We employed an iterative user-centered design process (Abras, Maloney-Krichmar, & Preece, 2004) to develop the content and appearance of the tool. A list of key elements of the design was compiled and multiple draft templates revised after feedback. Human computer interaction design and evaluation principles as well automated extraction of information from the CMS-485 form were used to develop the initial prototype of the HOME tool (Muir et al., 2002).
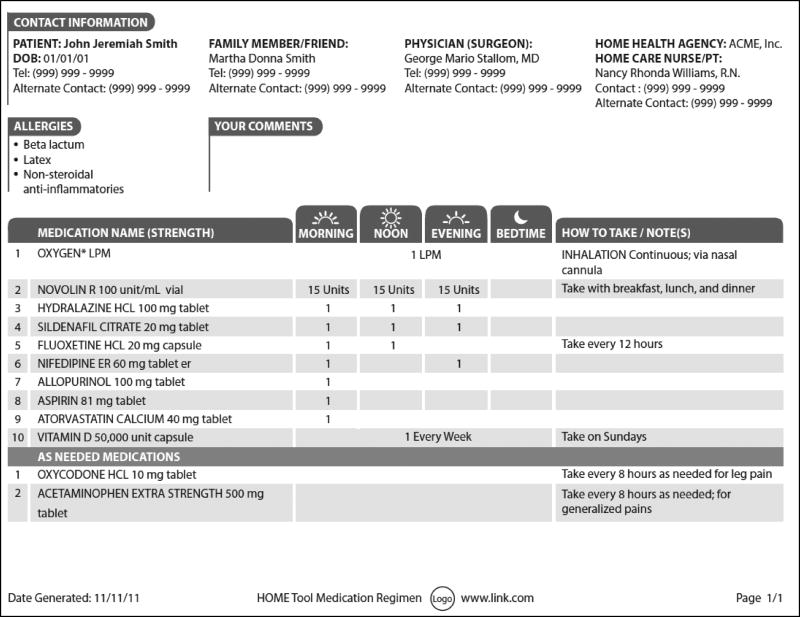
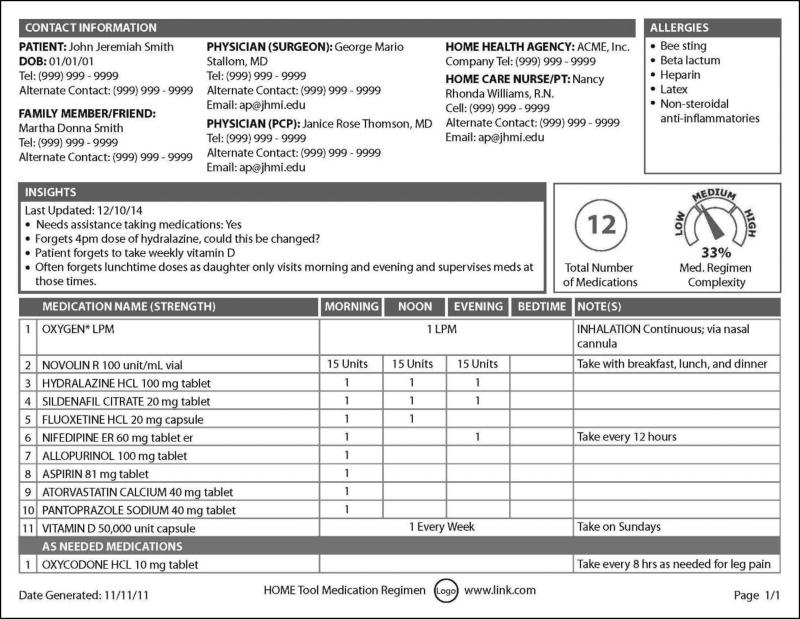
Two versions of the tool were created, one for patients and their caregivers and the other for nurses and physicians. The patient/caregiver version had larger font, graphics to illustrate the times medications should be taken and a section where the patient could make notes or write down questions to ask the nurse or physician. The physician/nurse version aimed to highlight the complexity of the medication regimen by graphically illustrating both the number of medications and the Medication Regimen Complexity Index (MRCI) which quantifies the complexity of prescribed medication regimens (George, Phun, Bailey, Kong & Stewart, 2004; Libby et al., 2013). The physician/nurse version also included an “insights” section where nurses could communicate key insights about the patient and their medication regimen learned during their evaluation of the patient in their home to physicians. Insights could highlight issues with compliance and offer possible solutions. For example, the home health nurse could write “Patient forgets to take lunchtime medications. Could all medications be changed to morning and evening when daughter is there?” Based on the feedback from the interviews and input from the research team, the designs were revised multiple times in order to produce the optimal prototype to go forward for testing (Figure 1).
Figure 1.
Prototype of HOME tool for patients and family members
User interface testing
Key informant interviews were conducted with the expected users of the tool including home care nurses (4 nurses and 1 physical therapist), physicians (n=5) and patients (n=7) and their family members, when available (n=5). Information was obtained on layout, content, design, visualizations and appearance of the tool. Separate interviews guides were prepared for each user group and all interviewees were shown both paper and web based versions of the tool. Questions focused on the layout and usability of the tool as well as the relevance of the information presented. Approval was obtained from the Johns Hopkins Institutional Review Board. Oral consent was obtained by a member of the research team before each interview. A trained facilitator conducted all interviews. Feedback from all user groups was compiled and incorporated into the final prototype.
All user groups expressed positive feedback about the use of the HOME tool. They found the information presented useful and felt that the HOME tool would be used by all parties. When asked about content, nurses particularly like the ability to use the tool to communicate with physicians and highlighted their inability to add comments to the current CMS-485 form. They also expressed concerns about the need to avoid duplication of effort and not enter data already present in the EHR. This concern was also shared by physicians who would have preferred that all data be sent to them electronically and not by mail or fax as happens most commonly with the CMS-485 form. Patients and caregivers liked that the tool was easy to read and understand. They felt they could bring it with them to different physicians and they liked that multiple copies could be given to caregivers.
Feedback on design and appearance was also provided with most users preferring section headings with white text on a dark background, font sizes 12 points or higher, and horizontal text. The insights section was not understood by some users at first and it was suggested that greater emphasis be placed on that section in the design by either changing the location or adding greater visual emphasis to the section. Patients and family members suggested other elements that could be added to the tool such as e-mail addresses, pharmacy information and medication side effects.
Many changes were made to the design based on the feedback from the user interviews. The layout was modified and the graphics were simplified. Where possible additional content suggestions were added to the design, (e.g. email addresses) however, taking into account that the overriding theme from the qualitative interviews was that all users liked the simplicity of the design we decided against adding pharmacy information and medication side effects. As most physicians reported receiving the CMS-485 form by paper or fax we modified the color scheme and design to ensure maximum readability. A higher specification web format was also created for users who wished to view the tool electronically. Figures 1 and 2 show the final prototypes of the paper versions of the patient/family and physician/nurse versions of the HOME tool.
Figure 2.
Prototype of HOME tool for home health care staff and physicians
Application development
The HOME tool was programmed using a web scripting language and was hosted on a secure server. Extraction of data from the CMS-485 pdf form and from the Electronic Health Record (EHR) was automated where possible to avoid a significant increase in workload on home care nurses and avoid duplicate entry. The program could populate the HOME tool fields in two ways – through the parsing and extraction of information from specified fields within the CMS-485 form or by the generation of a custom report that extracted pre-specified variables from the EHR used by Johns Hopkins Home Care Group, McKesson’s Horizon Clinical® (Horizons). Information unavailable from either source was manually entered by the home health nurse or Physical Therapist (PT), for example the name of the person who assisted with medication was available in Horizons but not in the CMS-485 form.
Over a three-month period, the HOME-tool application was developed and hosted on a secure webserver with access restricted to persons involved in the clinical care of the patient. Out-of-network access to the application required the entry of two unique usernames and passwords, one to access the Johns Hopkins system and a second to access the HOME tool. One tool was created for each patient with the ability to print or save versions tailored to the patient/caregiver or physician/nurse.
Results
Feasibility and usability pilot
The tool was pilot tested with patients receiving SHHC from Johns Hopkins Home Care group. Two hours of in-person training on the use of the tool was provided to the home care nurses prior to the commencement of the pilot with special attention given to both the insights section and to the family member/friend contact details to ensure that the person who assists with medications was recorded and not the next of kin. Additional phone and electronic support resources as well as written protocols were made available to nurses for the duration of the pilot. Although the tool can be used by any physician, PCPs commonly supervise home health care so twenty PCPs from Johns Hopkins University’s network of community physicians who regularly referred patients to home health care were identified and agreed to participate. Patients referred for SHHC whose PCP was on the list of participating physicians were identified by the intake and scheduling staff in Johns Hopkins Home Care Group and referred to the study team. Patients were assigned to either the CMS-485 or the EHR automated extraction arms of the pilot using a computer generated program. At the end of the SHHC episode feedback forms were sent to the patient, the family member who the home care nurse identified as helping the patient with their medications, the PCP and the home care nurse.
Pilot testing of the HOME tool began in September 2015 and continued until 19 patients had completed 20 Home Health encounters. The 19 patients were managed by 7 physicians and 6 home care nurses. The mean age of the patients was 76.8 years (SD 13.2), 78.9% were Caucasian (15/19) and 78.9% were female (15/19). Polypharmacy was common with an average of 10.9 medications (SD 4.3). All home care nurses were female and had more than 10 years of experience in home health care. The supervising physicians were mainly female (71.4%). Four were geriatricians and the other three were internal medicine physicians.
We piloted two data extraction methods for the tool. The first was EHR neutral and extracted information directly from the CMS-485 form for 10 patient encounters. The second method extracted the data from the Horizons EHR used by Johns Hopkins Home Health Group for the other 10 encounters. The HOME tool was successfully created and populated for all encounters. When asked to rate the usability of the tool on a 1–4 scale (1 = strongly disagree, 4 = strongly agree) physicians and nurses both found the tool easy to use (Mean (SD) physicians 3.7 (0.5), nurses 4.0 (0.0)). All nurses reported that the HOME tool improved communication with physicians about medications (Mean (SD) 4.0 (0.0)) but were less clear if the tool improved communication with families (Mean (SD), 2.4 (0.4)). Only 3 patients and no family caregivers returned feedback forms so the impact of the tool on patients and their families could not be assessed.
Discussion
Simple methods can improve nurse and physician communication by facilitating discussion regarding issues or problems around medications identified in the home (Coleman, 2003, Leonard, Graham & Bonacum, 2004; Hall, Longhurst & Higginson, 2009). Many issues contribute to poor communication around medications in SHHC including transitions of care, lack of access or fragmentation of EHR systems, lack of physician-nurse in-person contact and poor understanding of medications by patients and their families.
We have designed and built a tool with the goal of improving communication around medications in SHHC. This tool has the potential to benefit patients, families, and physicians by increasing family and patient understanding of medications, reducing medication regimen complexity and polypharmacy, reducing hospitalizations and the anxiety and stress around medications often experienced after a discharge. The twofold strategy to accomplish this was by drawing attention to the medication schedule and its complexity with physicians as well as working to improve communication with home health nurses. The overall goal is to manage polypharmacy and encourage simplification of regimens by tapering or discontinuing drugs and consolidating the number of times during the day medications are taken.
Home health care agencies must record all data elements mandated in the CMS-485 form in order to receive reimbursement from the federal government. Although efforts have been made to improve upon the CMS-485 and allow improved information exchange (Siegler et al., 2006) the CMS-485 form remains the method still in use by most HHAs. The decision on whether or not to integrate the HOME tool into an EHR or keep it EHR neutral is not straightforward. An EHR neutral tool could be used by all home health care agencies across the country and could extract information from standard CMS-485 fields. However, some of the unique features of the tool including the “insights” field and contact information for the person assisting with medications are not found in the CMS-485 form and would need to be entered by hand by the home health care nurse. In many cases this would be duplicate entry as they may already have entered the information into their EHR. Integrating the tool with a single EHR limits its use to those SHHC patients whose records exist in that EHR system, and in many cases home health care uses different EHRs to the health system referring the patients. EHRs were not primarily designed for home health care. Earlier issues integrating EHRs into existing home health workflows have largely been solved by EHR providers offering packages tailored to or designed for home health care. EHR integration of the HOME tool has multiple advantages including reducing the workload for the nurse, avoiding duplicate entry and creating a fast and efficient method of delivering the tool to physicians through their inboxes as well as to patients via patient portals.
The pilot identified many workflow challenges in identification of and communication with the correct people involved in each patient’s medication management. The referring physician is often not the physician who supervises the home health care episode. The PCP is the person most likely to sign the 485 and to take overall responsibility for medication reconciliation in the presence of multiple prescriptions from different physicians. On the physician/nurse version of the HOME tool we added an option of adding the contact details of a second physician (e.g. referring surgeon) if the PCP was not the referring physician. Home care nurses were encouraged to list the PCP in the first physician contact details field. In most care encounters in both hospital and community settings a next of kin is or has been identified for each patient and entered into the medical record. This may not be the person who assists with medication management, although often the same person fulfills both roles. E-mail addresses were added for home care nurses and physicians as this is now the preferred method of communication for some physicians with secure institutional e-mail addresses. Cellphone numbers were added for home health care nurses on the physician version to encourage physicians to call them directly and avoid the need to go through triage offices and await a call back. Out of hours contact numbers for the home health care agency were also added to the patient/caregiver version to help direct enquiries appropriately.
Although training sessions were conducted with nurses prior to the pilot, our feedback identified areas in which training could be improved including extending training to include physicians and providing more information to home health nurses including specific examples of insights. The training of multiple user groups and a larger insights section have both been incorporated into training which is now provided via an e-learning module designed to teach users how the HOME tool should be used, encourage simplification of regimens and improve patient and family understanding of medications. Requiring separate usernames and passwords to access the hospital system and the tool was time consuming and confusing for users. The tool now uses a single sign on to make it more accessible.
Finally, limited feedback was available from patients and their family caregivers. Feedback forms were mailed to each patient and family caregiver after the completion of each home health care episode, however, only 15% of participants returned these forms. These patients are often housebound, frail and can have multiple co-existing conditions (Hall et al., 2009) and challenges to participation in such efforts are significant. In the future we may explore asking the home care nurses to personally deliver feedback forms during a visit however this raises ethical considerations as participants may want to please the home care nurse on who they depend for care, or they may believe the quality of their care would be affected if they choose not to participate (Locher, Bronstein, Robinson, Williams & Ritchie, 2006).
Poor medication-related communication in SHHC is a problem. One potential avenue to address this is through the use of technology. We have designed a simple, largely automated tool to improve understanding and communication around medications. Future iterations of the tool could potentially contain all elements of the current CMS-485 form and provide effective communication around many aspects of care, not just medications. We have used the knowledge from our work to date to refine the tool, adding a single sign on, integrating it into the EHR, and developing an online training module for users of the tool. Further study is necessary to test this tool in a trial involving larger patient groups across multiple home health agencies and determine the effect of the tool on healthcare utilization and outcomes including emergency department visits, hospitalizations, physician visits and adverse drug events.
Suggested callouts.
However, the post-discharge medication reconciliation process is often conducted in the absence of meaningful and effective communication between the primary care physician and the home health nurse who visits the patient in their home.
Highlighting complexity of medication regimens to physicians has been demonstrated to lead to simplification of timing, dose reduction and discontinuation of harmful or unnecessary medications.
When asked about content, nurses particularly like the ability to use the tool to communicate with physicians and highlighted their inability to add comments to the current CMS-485 form.
Many issues contribute to poor communication around medications in skilled home healthcare including transitions of care, lack of access or fragmentation of EHR systems, lack of physician-nurse in-person contact and poor understanding of medications by patients and their families.
Acknowledgments
Funding
Funds to support this project were provided to Orla Sheehan, Cynthia Boyd, Kimberly Carl, Hadi Kharrazi, Bruce Leff and Jennifer Wolff by a Johns Hopkins School of Medicine Discovery Fund Synergy Award and to Kimberly Carl, Cynthia Boyd and Orla Sheehan from the Johns Hopkins University Edward R. Roybal Center for Translation Research of the National Institute on Aging (NIA) under award number P30AG048773.
We sincerely thank the physicians, nurses, patients and their families who participated in this research. We also thank the user experience consultancy firm, GravityDrive who worked with us to design the prototype of the HOME tool.
Footnotes
The author(s) declare(s) no conflicts of interest:
Contributor Information
Orla C. Sheehan, Division of Geriatric Medicine and Gerontology, Center on Aging and Health, Johns Hopkins University, Baltimore, Maryland.
Hadi Kharrazi, Health Policy and Management, Bloomberg School of Public Health, Baltimore, Johns Hopkins University Maryland.
Kimberly J. Carl, Home Health Services, Johns Hopkins Home Care Group, Baltimore, Maryland.
Bruce Leff, Division of Geriatric Medicine and Gerontology, Center for Transformative Geriatric Research, Johns Hopkins University, Baltimore, Maryland.
Jennifer L. Wolff, Health Policy and Management, School of Public Health, Johns Hopkins University, Baltimore, Maryland.
David L. Roth, Center on Aging and Health, Division of Geriatrics and Gerontology, Johns Hopkins University, Baltimore, Maryland.
Jennifer Gabbard, Wake Forest University, Section of Gerontology and Geriatrics. Winston-Salem, North Carolina.
Cynthia M. Boyd, Division of Geriatric Medicine and Gerontology, Center for Transformative Geriatric Research. Johns Hopkins University, Baltimore, Maryland.
References
- Abras C, Maloney-Krichmar D, Preece J. User-Centered Design. In: Bainbridge W, editor. Encyclopedia of Human-Computer Interaction. Thousand Oaks: Sage publications; 2004. [Google Scholar]
- Blumenthal D. Launching HITECH. New England Journal of Medicine. 2010;362(5):382–385. doi: 10.1056/NEJMp0912825. [DOI] [PubMed] [Google Scholar]
- Bowles KH, Dykes P, Demiris G. The Use of Health Information Technology to Improve Care and Outcomes for Older Adults. Research Gerontologic Nursing. 2015;8(1):5–10. doi: 10.3928/19404921-20121222-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody AA, Gibson B, Tresner-Kirsch D, Kramer H, Thraen I, Coarr ME, Rupper R. High Prevalence of Medication Discrepancies Between Home Health Referrals and Centers for Medicare and Medicaid Services Home Health Certification and Plan of Care and Their Potential to Affect Safety of Vulnerable Elderly Adults. Journal of the American Geriatrics Society. 2016;64(11):166–170. doi: 10.1111/jgs.14457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. Journal of the American Geriatrics Society. 2003;51(4):549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- Dowding DW, Turley M, Garrido T. The impact of an electronic health record on nurse sensitive patient outcomes: An interrupted time series analysis. Journal of the American Medical Informatics Association. 2012;19:615–620. doi: 10.1136/amiajnl-2011-000504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykes PC, Carroll DL, Hurley A, Lipsitz S, Benoit A, Chang F, Middleton B. Fall prevention in acute care hospitals: A randomized trial. JAMA. 2010;304(17):1912–1918. doi: 10.1001/jama.2010.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott RA, O’Callaghan C, Paul E, George J. Impact of an intervention to reduce medication complexity for older hospital inpatients. International Journal of Clinical Pharmacy. 2013;35:217–24. doi: 10.1007/s11096-012-9730-3. [DOI] [PubMed] [Google Scholar]
- Fossum M, Alexander GL, Ehnfors M, Ehrenberg A. Effects of a computerized decision support system on pressure ulcers and malnutrition in nursing homes for the elderly. American Medical Informatics Association. 2011;80(9):607–617. doi: 10.1016/j.ijmedinf.2011.06.009. [DOI] [PubMed] [Google Scholar]
- George J, Phun YT, Bailey MJ, Kong DC, Stewart K. Development and validation of the medication regimen complexity index. Annals of Pharmacotherapthy. 2004;38(9):1369–1376. doi: 10.1345/aph.1D479. [DOI] [PubMed] [Google Scholar]
- Giovannetti ER, Wolff JL, Xue QL, Weiss CO, Leff B, Boult C, Hughes T, Boyd CM. Difficulty assisting with health care tasks among caregivers of multimorbid older adults. Journal of General Internal Medicine. 27(1):37–44. doi: 10.1007/s11606-011-1831-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. Journal of General Internal Medicine. 2012;27(5):520–526. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall S, Longhurst S, Higginson IJ. Challenges to conducting research with older people living in nursing homes. BMC Geriatrics. 2009;9(1):1–8. doi: 10.1186/1471-2318-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press; 2011. https://doi.org/10.17226/12956. [PubMed] [Google Scholar]
- Jones AL, Harris-Kojetin L, Valverde R. National health statistics reports; no 52. Hyattsville MD: National Center for Health Statistics; 2012. Characteristics and Use of Home Health Care by Men and Women Aged 65 and Over. [PubMed] [Google Scholar]
- Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. Journal of Hospital Medicine. 2007;2(5):314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Roumie CL, Dalal AK, Cawthon C, Businger A, Eden SK, Schnipper JL for PILL-CVD (Pharmacist Intervention for Low Literacy in Cardiovascular Disease) Study Group. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. Annals Internal Medicine. 2012;157(1):1–10. doi: 10.7326/0003-4819-157-1-201207030-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Quality and Safety in Health Care. 2004;13(Suppl 1):85–90. doi: 10.1136/qhc.13.suppl_1.i85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libby AM, Fish DN, Hosokawa PW, Linnebur SA, Metz KR, Nair KV, Hirsh JD. Patient-level medication regimen complexity across populations with chronic disease. Clinical Therapeutics. 2013;35(4):385–398. doi: 10.1016/j.clinthera.2013.02.019. [DOI] [PubMed] [Google Scholar]
- Locher JL, Bronstein J, Robinson CO, Williams C, Ritchie CS. Ethical Issues Involving Research Conducted With Homebound Older Adults. Gerontologist. 2006;46(2):160–164. doi: 10.1093/geront/46.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muir AJ, Sanders LL, Wilkinson WE, Schmader K. Reducing medication regimen complexity: a controlled trial. Journal of General Internal Medicine. 2002;16(2):77–82. doi: 10.1046/j.1525-1497.2001.016002077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press MJ, Gerber LM, Peng TR, Pesko MF, Feldman PH, Ouchida K, Casalino LP. Post discharge Communication Between Home Health Nurses and Physicians: Measurement, Quality, and Outcomes. Journal of the American Geriatrics Society. 2015;63(7):1299–1305. doi: 10.1111/jgs.13491. [DOI] [PubMed] [Google Scholar]
- Reinhard S, Levine C, Samis S. Home Alone: Family Caregivers Providing Complex Chronic Care. Washington, DC: AARP Public Policy Institute; 2012. Retrieved from http://www.aarp.org/homealone. [Google Scholar]
- Siegler EL, Murtaugh CM, Rosati RJ, Clark A, Ruchlin HS, Sobolewski S, Feldman P, Callahan M. Improving the transition to home healthcare by rethinking the purpose and structure of the CMS 485: first steps. Home Health Care Services Quarterly. 2006;25(3–4):27–38. doi: 10.1300/J027v25n03_02. [DOI] [PubMed] [Google Scholar]
- Smith PD, Boyd C, Bellantoni J, Roth J, Becker KL, Savage J, Nkimbeng M, Szanton SL. Communication between office-based primary care providers and nurses working within patients' homes: an analysis of process data from CAPABLE. Journal of Clinical Nursing. 2016;25(3–4):454–462. doi: 10.1111/jocn.13073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis SS, McAuley WJ, Dmochowski J, Bernard MA, Kao HF, Greene R. Factors associated with medication hassles experienced by family caregivers of older adults. Patient Education and Counseling. 2006;66(1):51–57. doi: 10.1016/j.pec.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JL, Boyd CM, Gitlin LN, Bruce ML, Roter DL. Going it together: persistence of older adults' accompaniment to physician visits by a family companion. Journal of the American Geriatrics Society. 2012;60(1):106–112. doi: 10.1111/j.1532-5415.2011.03770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JL, Meadow A, Boyd CM, Weiss CO, Leff B. Physician evaluation and management of Medicare home health patients. Medical Care. 2009;47(11):1147–1155. doi: 10.1097/MLR.0b013e3181b58e30. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Meadow A, Weiss CO, Boyd CM, Leff B. Medicare home health patients' transitions through acute and post-acute care settings. Medical Care. 2008;46(11):1188–1193. doi: 10.1097/MLR.0b013e31817d69d3. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Roter DL, Barron J, Boyd CM, Leff B, Finucane TE, Gallo JJ, Rabins PV, Roth DL, Gitlin LN. A tool to strengthen the older patient-companion partnership in primary care: results from a pilot study. Journal of the American Geriatrics Society. 2014;62(2):312–319. doi: 10.1111/jgs.12639. [DOI] [PMC free article] [PubMed] [Google Scholar]