Abstract
Peri-implant fractures of the wrist are uncommon, and usually present as stress fractures distal to the site of the implant. We report an unusual case where the radius has fractured beneath a plate, causing bending and deformity of the implant. This prevented reduction of the fracture under sedation, so urgent intervention became necessary due to neurovascular compromise.
Keywords: Emergency anesthesia, Orthopedic trauma, Peri-implant fracture, Wrist fracture
1. Introduction
Fractures of the distal radius are amongst the most common injury encountered by orthopaedic surgeons.1 While a significant majority of these injuries are treated non-operatively with closed reduction and manipulation, indications for surgical management are well described, frequently with buttress and locked plating devices.1 Volar locking plates have gained popularity because of their wider availability and reliability of the locking technology adapted to the wrist.2 Although there are no studies yet to demonstrate that these plating techniques are associated with better outcomes compared to sufficiently reduced nonsurgical management strategies, it does serve a purpose in specific patient populations.1 However, it must be recognized that this surgical technique can be associated with complications and failures that are widely reported in the medical literature.2 Mechanical failure of the volar locking plate devices are considered to be rare complications with failure being defined as plate breakage/bending, screw breakage/loosening, or collapse of articular fragments resulting in intra-articular screw extrusion.2
This particular case illustrates an exceedingly rare example of a peri-implant re-fracture due to trauma, resulting in bending of the implant and a fracture of the bone beneath the plate. This is therefore quite distinct from a stress fracture. A literature search using PubMed yielded only 1 similar report that described a failed implant with an underlying fracture not associated with stress. This case describes some of the complexities of such an uncommon injury, and how general principles were applied in its management due to a lack of robust guidelines/evidence available.
2. Case report
A 50-year-old male motorcyclist, who had eleven years previously undergone open reduction and internal fixation of a solar Barton fracture on the left wrist, was involved in a single vehicle accident as he was turning his motorbike at a low speed in a paved car-parking area. The motorcycle slid-out from under him and he fell onto his left hand side. He sustained a closed isolated injury to his left (non dominant) wrist and attended the Emergency Department as an ambulatory patient. On arrival he was noted to have gross deformity of the left wrist, with volar displacement of the carpus, and a rather cool left hand with delayed capillary refill of 2–3 s.
As a result of limb compromise, despite a palpable radial pulse and pulse oximetry reading of 99%, the hand was manipulated under procedural sedation with the patient’s consent and appropriate monitoring. Unfortunately, little improvement in the alignment of the hand with respect to the forearm was achieved. A volar slab was applied and an x-ray film obtained. (Fig. 1). Neurological examination after application of the volar slab revealed a sensory nerve deficit in the ulnar nerve distribution at the level of the hand, no motor weakness was found.
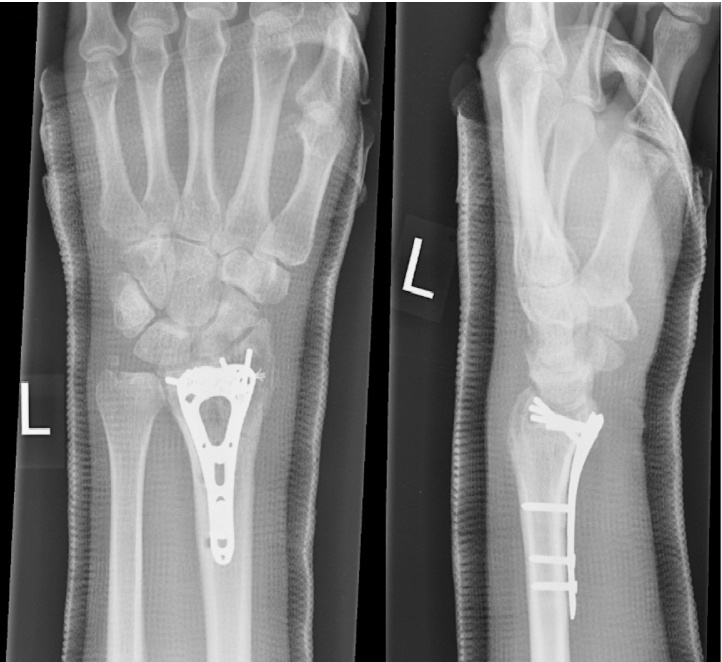
Fig. 1.
Lateral and Anterior-Posterior (AP) Left Wrist Radiograph.
Imaging undertaken in plaster cast. A previous orthopedic internal fixation (Buttress T plate) is seen to the palmar aspect of the distal radius, this is now bent to almost 90°. A comminuted fracture is seen in the distal radius with multiple fragments displaced anteriorly adjacent to the distal end of the plate.
An Orthopaedic consultation was immediately obtained and arrangements made for the patient to undergo open reduction and internal fixation under general anaesthetic.
During the operation, the bent buttress ‘T’ plate had caused gross swelling and tissue damage with tenting of the flexor tendons and concern about the median nerve. The ulnar nerve was neither exposed or explored. This plate was removed, and the fracture was reduced leading to immediate decompression of the soft tissues. The distal radial bony fragments were temporarily held with K wires, and then fixed with a Synthes™ variable angle locking plate. Intra-operative fluoroscopy was used to confirm position and alignment of the fracture and plate (Fig. 2). The comminuted radial styloid was fixed with a Mini QUICKANCHOR ™ Plus (#0 Suture). The wound was washed and closed primarily and a back slab plaster cast applied. Antibiotics were given for 2 postoperative doses, and the arm elevated in a Bradford sling for 24 h. Clinical review of the patient at 6 h post op revealed no remaining neurological deficit.
Fig. 2.
Intra-operative Fluoroscopy.
A Fluoroscopic intra-operative image of a left distal radius and ulnar, showing a distal radius locking plate and suture anchor.
Clinical review of the surgical wound occurred at two weeks, with removal of the plaster cast, fitting of a futura™ Spint and early physiotherapy.
6 weeks later a check x-ray (Fig. 3) was performed and resistance physiotherapy commenced. Two months after the injury, the patient was able to perform most of his farming duties with the support of a Futura splint on the affected wrist for heavy lifting. At his 6 month follow up he had regained full function, including both motor and sensory, as compared to prior to the injury
Fig. 3.
AP and Lateral Left Wrist Radiograph.
The wrist is held in a Plaster of Paris in neutral carpal alignment. Distal radius has a volar plate fixation with distal locking pegs and proximal non-locking screws. There is a single anchor within the distal radial styloid. There is some evidence of bony union within the distal radius, the ulnar styloid does not show signs of union.
3. Discussion
The implementation of different plating constructs to surgically repair distal radius fractures is becoming a widely popular technique. The goals of surgical treatment of fractures of the distal radius are to re-establish articular congruity and normal bony alignment, with failure resulting in radiographic arthritis and poor outcomes.3 Peri-implant fractures secondary to mechanical failure are a rare occurrence.4 This case illustrates a middle-aged male who sustained a re-fracture of the distal radius after initial fixation with buttress ‘T’ plate. Usually, these fractures manifest as stress fractures which occur at or near the distal end of the implant. Our case is quite unusual in that the fracture is caused by trauma resulting in mechanical bending of the buttress ‘T’ plate, with an associated fracture of the bone beneath the deformed plate. Such a case, has only been described once in the literature according to our search.
Indications for operative intervention with distal radius fractures are well described, and include displaced intra-articular fractures, comminuted unstable fracture patterns, or failure of closed reduction and manipulation.5 Rarely, in closed fracture patterns does fixation require emergency surgery, except those cases where neurovascular compromise is present. Significantly displaced dorsal fractures can result in median nerve tension and urgent reduction is required, this alone is usually sufficient to improve neurological symptoms and allow ‘next day’ operative planning.
The presence of bent metalwork in this volar displaced fracture resulted in ulnar nerve symptoms and reduction of this fracture around a bent T plate may have worsened these. As such it required urgent surgical exploration and definitive fixation.
Elective removal of metal work at this site is not commonly performed due to the additional morbidity associated with repeat surgery, despite the fact that the very presence of an implant may predispose to fracture at a later time, by changing the structure of the bone, delayed fracture healing due to endosteal ischaemia, and prosthetic loosening due to abnormal joint biomechanics.6 Thus peri-implant fracture repair may be disadvantaged due to more limited options and a higher rate of complications than first-time surgery.
In conclusion, peri-implant fractures of the wrist must be dealt with on a case-by-case basis, applying some general principles: The aim should be to restore the biomechanical integrity of the bone. Great care needs to be taken with soft tissue handling, and periosteal stripping kept to an absolute minimum. Both periosteal and endosteal blood supplies need to be conserved, dead space avoided, and bone grafting utilised if needed. The patient’s medical condition and nutrition should be optimised, and this may include encouragement to stop smoking, where applicable.7
Conflict of interest
None.
Acknowledgements
Mr. Dineen − The responsible Orthopaedic Consultant overseeing the patient’s care.
The patient − For their kindness and enthusiasm to share their case.
References
- 1.Min W., Kaplan K., Miyamoto R., Tejwani N.C. A unique failure mechanism of a distal radius fracture fixed with volar plating − a case report. Bull NYU Hosp Jt Dis. 2010;68(4):304–306. [PubMed] [Google Scholar]
- 2.Foo T.L., Gan A.W., Soh T., Chew W.Y. Mechanical failure of the distal radius volar locking plate. J Orthop Surg. 2013;21(3):332–336. doi: 10.1177/230949901302100314. [DOI] [PubMed] [Google Scholar]
- 3.Beck J.D., Harness N.G., Spencer H.T. Volar plate fixation failure for volar shearing distal radius fractures with small lunate facet fragments. J Hand Sug Am. 2014;39:670–678. doi: 10.1016/j.jhsa.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Geurts G.F., Van Riet R.P., Verstreken F. Successful closed reduction of refractured wrist with a bent volar distal radius plate. Acta Orthop Belg. 2012;78(1):126–128. [PubMed] [Google Scholar]
- 5.Leung F., Kwan K., Fang C. 2013. Distal radius fracture: current concepts and management. [(Accessed February 06 2017) Available at: http://www.boneandjoint.org.uk/content/focus/distal-radius-fracture-current-concepts-and-management] [Google Scholar]
- 6.Fleischman A.N., Chen A.F. Periprosthetic fractures around the femoral stem: overcoming challenges and avoiding pitfalls. Ann Transl Med. 2015;3:234. doi: 10.3978/j.issn.2305-5839.2015.09.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baek S.-H. Identification and preoperative optimization of risk factors to prevent periprosthetic joint infection. World J Orthop. 2014;5:362–367. doi: 10.5312/wjo.v5.i3.362. [DOI] [PMC free article] [PubMed] [Google Scholar]