Abstract
Background
Non-union humeral shaft fractures are seen frequently in clinical practice at about 2–10% in conservative management and 30% in surgically operated patients. Osteosynthesis using dynamic compression plate (DCP), intramedullary nailing, locking compression plate (LCP), Ilizarov technique along with bone grafting have been reported previously. In cases of prior failed plate-screw osteosynthesis the resultant osteopenia, cortical defect, bone loss, scalloping around screws and metallosis, make the management of non-union more complicated. Fibular graft as an intramedullary strut is useful in these conditions by increasing screw purchase, union and mechanical stability. This study is a retrospective and prospective follow up of revision plating along with autologous non-vascularised intramedullary fibular strut graft (ANVFG) for humeral non-unions following failed plate osteosynthesis.
Materials and methods
Seventy eight cases of nonunion humeral shaft fractures were managed in our institute between 2008 and 2015. Of these, 57 cases were failed plate osteosynthesis, in which 15 cases were infected and 42 cases were noninfected. Out of the 78 cases, bone grafting was done in 55 cases. Fibular strut graft was used in 22 patients, of which 4 cases were of primary nonunion with osteoporotic bone. Applying the exclusion criteria of infection and inclusion criteria of failed plate osteosynthesis managed with revision plating using either LCP or DCP and ANVFG, 17 cases were studied. The mean age of the patients was 40.11 yrs (range: 26–57 yrs). The mean duration of non-union was 4.43 yrs (range: 0.5–14 yrs). The mean follow-up period was 33.41 months (range: 12–94 months). The average length of fibula was 10.7 cm (range: 6–15 cm). Main outcome measurements included bony union by radiographic assessment and pre- and postoperative functional evaluation using the DASH (Disabilities of the Arm, Shoulder and Hand) score. Results: Sixteen out of 17 fractures united following revision plating and fibular strut grafting. Average time taken for union was 3.5 months (range: 3–5 months). Complications included one each of implant failure with bending, transient radial nerve palsy and transient ulnar nerve palsy. No case had infection, graft site morbidity or peroneal nerve palsy. Functional assessment by DASH score improved from 59.14 (range: 43.6–73.21) preoperatively to 23.39 (range: 8.03–34.2) postoperatively (p = 0.0003). Conclusion: The results of our study indicate that revision plating along with ANVFG is a reliable option in humeral diaphyseal non-unions with failed plate-screw osteosynthesis providing adequate screw purchase, mechanical stability and high chances of union with good functional outcome.
Keywords: Nonunion humerus, Failed internal fixation, Fibular graft, Plate osteosynthesis, Humeral shaft fracture
1. Introduction
Humeral shaft fractures are relatively common injuries accounting for 5–8% of all fractures in human body and 14% of all fractures of humerus.1 Historically, fractures of humerus have been associated with high incidence of non-union. The advent of bracing and operative stabilization techniques led to significant decline in non-union rate.2 Both conservative and surgical treatment result in healing. Conservatively managed humeral shaft fractures present with non-union rates of 2–10%, with most of the cases resulting from proximal third fractures or those with a proximal butterfly fragment.3 In a review by Volgas et al., surgically managed fractures fared even worse with non-union rate as high as 30%.4
Most of the non-union humeral shaft fractures can be managed successfully by conventional methods such as Dynamic Compression Plate (DCP) or Locking Compression Plate (LCP) fixation, intramedullary nailing, Ilizarov technique and bone grafting. These therapeutic options alone or in combination can achieve bony union in 82-95% of patients.5 In multi-operated cases extensive bone loss due to previous implant, scalloping around screws, metallosis, osteopenia, nonviable intermediate butterfly fragments and instability pose a challenge for the surgical management along with risk factors such as alcoholism, diabetes mellitus, smoking, obesity and osteoporosis.3, 6 The use of fibular graft as an intramedullary strut in humeral nonunions was originally described by Wright et al. in a clinical and biomechanical study.7
The purpose of this study is to assess the role of autologous nonvascularized intramedullary fibular strut graft (ANVFG) in non-union diaphyseal humeral fractures following failed plate-screw osteosynthesis.
2. Materials and methods
2.1. Study design
A retrospective and prospective study was conducted after obtaining the Institutional Ethical Committee approval from our Institute. Seventy eight cases of nonunion humeral shaft fractures were managed at our institute between 2008 and 2015. Of these, 57 cases were failed plate osteosynthesis, in which 15 cases were infected nonunion managed with Ilizarov method and 42 cases were non-infected managed with revision plating either with or without bone graft. Out of the 78 cases, either iliac crest or fibular bone graft was used in 55 cases. Fibular strut graft was used in 22 patients, of which 4 cases were of primary nonunion with osteoporotic bone. Applying the exclusion criteria of infection, pathological fractures, primary non-union, and revision cases managed with or without iliac crest bone graft alone and inclusion criteria of failed plate osteosynthesis managed with revision plating and ANVFG, we were left with 17 cases for the study (Table 1).
Table 1.
Patient data.
| S/NO | Age (yrs) | Sex | Side | Site | Duration of Nonunion (months) | No. of Prior Surgeries | Type of Nonunion | Risk factors | Approach |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 48 | M | Rt | D/3rd | 6 | 1 | comminuted type | nil | posterior |
| 2 | 33 | M | Lt | M/3rd | 8 | 1 | atrophic type | nil | posterior |
| 3 | 38 | M | Rt | M/3rd | 60 | 2 | atrophic type | nil | posterior |
| 4 | 48 | M | Lt | M/3rd | 48 | 1 | atrophic type | Hepatitis B, Hepatitis C | posterior |
| 5 | 28 | M | Lt | M/3rd | 12 | 1 | atrophic type | epilepsy, on anti-epileptics | posterior |
| 6 | 42 | M | Rt | D/3rd | 6 | 1 | atrophic type | smoking- 10yrs | posterior |
| 7 | 50 | M | Lt | M/3rd | 48 | 2 | atrophic type | Hypertension | anterolateral |
| 8 | 27 | M | Lt | M/3rd | 8 | 1 | comminuted type | nil | anterolateral |
| 9 | 57 | F | Rt | M/3rd | 144 | 1 | atrophic type | Diabetes Mellitus, Hepatitis B | posterior |
| 10 | 53 | M | Lt | M/3rd | 48 | 1 | atrophic type | Diabetes Mellitus | anterolateral |
| 11 | 30 | M | Rt | M/3rd-D/3rd | 48 | 1 | atrophic type | nil | anterolateral |
| 12 | 26 | M | Lt | D/3rd | 24 | 1 | atrophic type | nil | posterior |
| 13 | 45 | F | Lt | M/3rd-D/3rd | 72 | 1 | comminuted type | nil | anterolateral |
| 14 | 50 | F | Rt | M/3rd | 60 | 1 | atrophic type | Hypertension | posterior |
| 15 | 36 | M | Rt | M/3rd | 168 | 1 | atrophic type | nil | anterolateral |
| 16 | 36 | M | Rt | D/3rd | 24 | 2 | atrophic type | Smoking-20yrs | anterolateral |
| 17 | 35 | M | Rt | P/3-M/3rd | 120 | 1 | atrophic type | Smoking | anterolateral |
| S/No | Age (yrs) | Sex | Implant | Fibula | Iliac Crest | Post Operative Complications | Union (months) | Duration of Followup (months) | Pre Op DASH Score | DASH Score at Final Followup |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 48 | M | DCP | 10 cm hemi | − | nil | 3 | 94 | 73.21 | 8.03 |
| 2 | 33 | M | DCP | 8 cm | − | nil | 3 | 69 | 44.4 | 12.5 |
| 3 | 38 | M | DCP | 12 cm | − | nil | 4 | 59 | 43.6 | 21.9 |
| 4 | 48 | M | DCP | 14 cm | − | nil | 4 | 46 | 46.29 | 32.4 |
| 5 | 28 | M | DCP | 8 cm | − | nil | 3 | 36 | 58.3 | 12.96 |
| 6 | 42 | M | DCP | 6 cm | − | nil | 3 | 36 | 47.32 | 15.17 |
| 7 | 50 | M | DCP | 8 cm | − | nil | 3 | 31 | 61.11 | 28.7 |
| 8 | 27 | M | DCP | 10 cm hemi | − | implant failure − bending of plate | nil | 30 | 48.1 | 29.6 |
| 9 | 57 | F | DCP | 13 cm | − | nil | 4 | 25 | 66.4 | 34.2 |
| 10 | 53 | M | DCP | 14 cm | + | nil | 4 | 23 | 59.2 | 31.48 |
| 11 | 30 | M | DCP | 15 cm | + | iatrogenic fracture during implant removal | 4 | 22 | 61.6 | 14.28 |
| 12 | 26 | M | LCP | 15 cm | + | ulnar nerve palsy recovered in due course of time | 5 | 21 | 58.3 | 19.6 |
| 13 | 45 | F | DCP | 8 cm | − | wrist drop recovered by 3 months | 3 | 18 | 69.25 | 33.3 |
| 14 | 50 | F | DCP | 10 cm hemi | − | nil | 3 | 17 | 60.7 | 24.1 |
| 15 | 36 | M | LCP | 15 cm | − | nil | 4 | 15 | 66.6 | 30.5 |
| 16 | 36 | M | DCP | 7 cm | + | Nil | 3 | 14 | 68.75 | 21.4 |
| 17 | 35 | M | PHILOS | 10 cm | − | Nil | 3 | 12 | 72.31 | 27.67 |
2.2. Demographic data
There were 14 male and 3 female patients. The mean age was 40.11 yrs (range: 26–57 yrs). 9 patients had right side and 8 patients had left side involvement. Type of non-union was classified according to Weber and Cech classification.8 Fourteen patients had atrophic type of non-union and 3 patients had comminuted type of avascular non-union. One patient had non-union at proximal third-middle third junction, 10 patients had non-union at middle third junction, and 6 patients had non-union at middle third – distal third junction.
The mean duration of non-union was 4.43 yrs (range: 0.5–14 yrs). While the minimum duration of non-union was 6 months, only 5 cases had less than one year of duration of non-union, 9 cases had non-union in the range of 2–6 yrs and 3 cases had non-union as long as 10–14 yrs. Implant that has been used previously at the time of index procedure was DCP in 16 patients and LCP in one patient. Two patients underwent procedures twice with bone grafting in second procedure. Implant failure was observed in preoperative radiograph in 17 patients. Out of these, 8 patients had breakage of implant, 2 patients had broken screws alone and 11 patients had obvious radiological evidence of excessive bone loss, scalloping around screws, loosened implant with dislodged screws.
2.3. Surgical technique
All the patients underwent revision plate osteosynthesis of humerus along with intramedullary fibular strut graft. In the preoperative period, radiological assessment, complete blood counts, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were done in all patients to rule out the possibility of latent infection. Posterior approach was used in 9 patients and anterolateral approach in 8 patients based upon previous approach and non-union site. The previous implant was removed and thorough debridement of non-union site was done, fibrous tissue excised, fracture ends freshened, and medullary canal recanalized on both sides with serial reaming with rigid K-nail reamers. An average length of 10.7 cm (range: 6–15 cm) fibular graft was harvested and kept as intramedullary strut. In one patient fibular graft was kept as onlay in distal fragment as there was extensive bone loss due to previous implant and the non-union site was at distal third shaft. In two patients, hemi-fibula was used as the medullary canal diameter was narrow. For osteosynthesis LCP was used in 4 patients and DCP in 14 patients. As far as possible in all cases at least 3 screws each were placed proximally and distally with quadricortical purchase. Additional iliac crest cortico-cancellous bone graft was used in 4 patients in whom there was extensive bone loss with scalloping due to previous implant.
2.4. Follow-up and assessment
Postoperatively limb was immobilised in J-slab for 4 weeks. Active assisted shoulder and elbow exercises were started after 4 weeks. Patients were followed up at monthly interval till radiological union was seen and then at 6 months interval. The mean follow-up was 33.41 months (range: 12–94 months). Functional assessment was done by using DASH (Disabilities of the Arm, Shoulder and Hand) score both preoperatively and postoperatively at the time of final follow up.9
2.5. Statistical analysis
Statistical analysis was carried out by using the Graphpad Prism software. The nonparametric test, Wilcoxon signed-rank test was used to analyse the data.
3. Results
3.1. Radiological outcome
All fractures, except one, united following revision plating and intramedullary fibular strut graft procedure (Fig. 1, Fig. 2, Fig. 3, Fig. 4). One patient had failure with implant bending but was clinically asymptomatic. The average time for union was 3.5 months (range: 3–5 months).
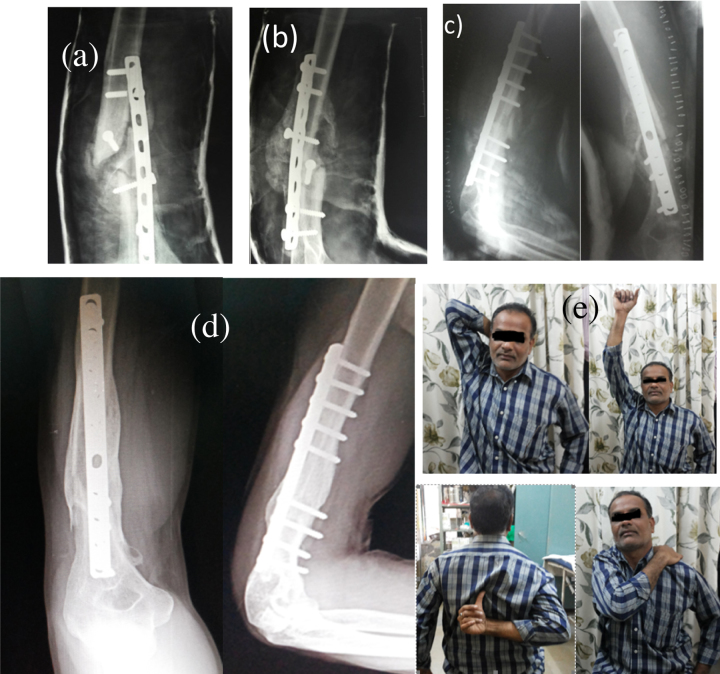
Fig. 1.
(a,b) A 48 yrs old male with 6 months duration of implant failure with non-union humerus distal third and AP, lateral radiograph suggestive of screw breakage implant loosening and comminuted type of non-union. (c) Treated with revision plating and ANVFG. (d) 94 months follow up suggestive of union. (e) With good functional outcome.
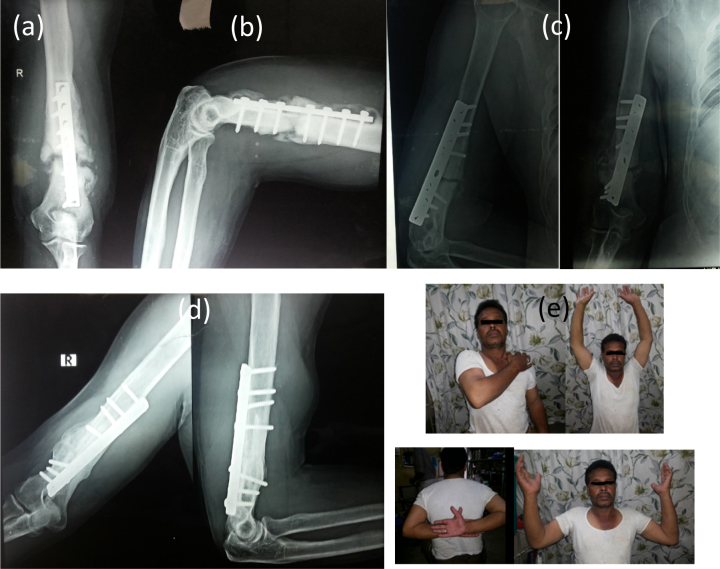
Fig. 2.
(a,b) A 42 yrs male with 7 months duration of implant failure non-union distal third humerus. (c) Treated with revision plating and ANVFG. (d) 36 months follow up suggestive of union at fracture site. (e) With good functional outcome.
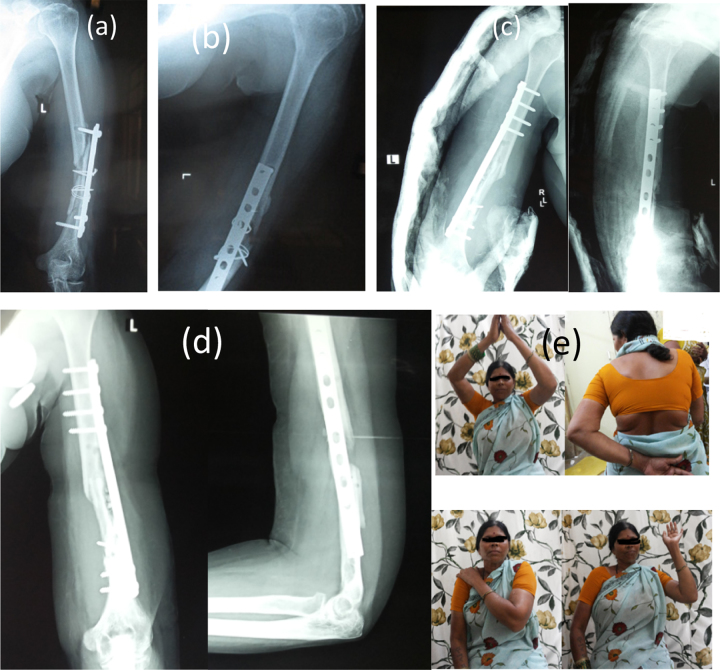
Fig. 3.
(a,b) A 45 yrs old female with 6 months duration of implant failure non-union, and AP, lateral radiograph suggestive of comminuted type of non-union. (c) Treated with revision plating and ANVFG. (d) 7 months follow up suggestive of union. (e) With good functional outcome.
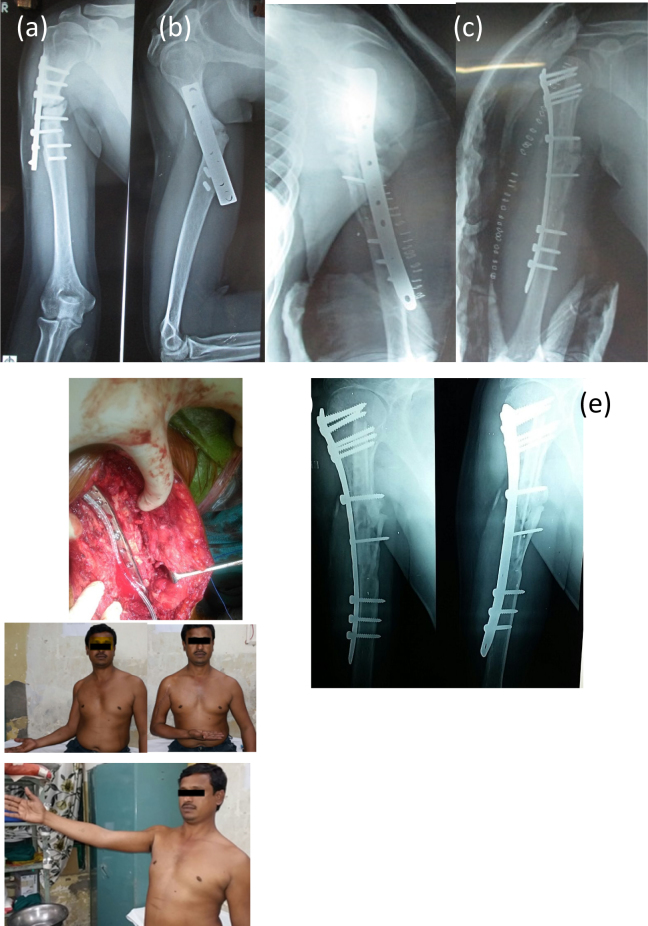
Fig. 4.
(a,b) A 35 yrs old male with 10 yrs duration of implant failure non-union, and AP, lateral radiograph suggestive of screw breakage, atrophic type of non-union with sclerosis of fracture ends. (c) Treated with revision plating and ANVFG. (d) 10 months follow up radiograph suggestive of union. (e) With fair functional outcome.
3.2. Complications
The complications included one patient with implant bending (Fig. 5). Possibility of failure in this patient is probably due to use of hemi-fibula which resulted in relatively less mechanical stability. In one patient iatrogenic fracture occurred during implant retrieval which eventually united (Fig. 6). One patient had transient radial nerve palsy postoperatively which recovered during follow up by 3 months. Another patient had transient ulnar nerve palsy which recovered in due course of time. There was no case of graft site morbidity, peroneal nerve palsy and infection – either at the fracture site or graft donor site.
Fig. 5.
(a,b) A 27 yrs old with 8 months old implant failure non-union Lt humerus and AP, lateral radiograph suggestive of implant breakage. (c) Treated with revision plating and hemi-fibular graft. (d) 4 months follow up radiograph suggestive of implant failure with bending. (e) With fair functional outcome.
Fig. 6.
(a,b) A 30 yrs old male patient with implant failure non-union Rt humerus and AP, lateral radiograph suggestive of implant breakage, sclerosis of fracture ends and atrophic type non-union. (c) Treated with revision plating and ANVFG. Arrow showing intraoperative iatrogenic distal third fracture during implant retrieval. (d) 12 months follow up radiograph suggestive of union at fracture site and iatrogenic fracture site. (e) With good functional outcome.
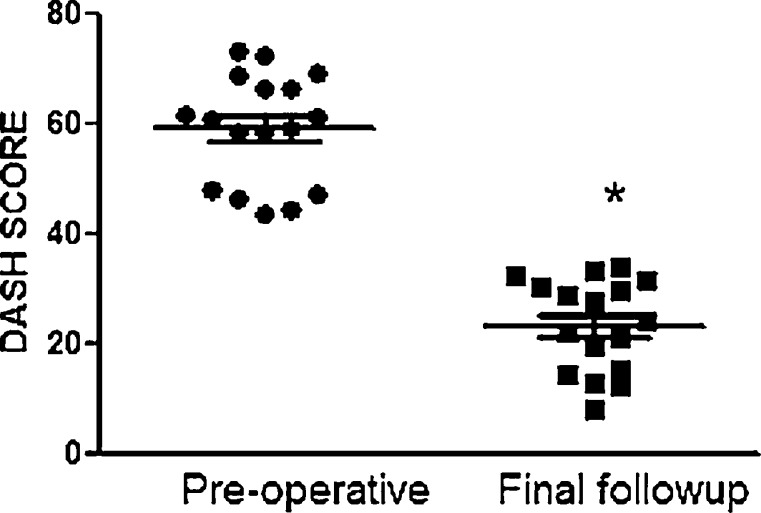
3.3. Functional outcome
The functional outcome which was assessed by DASH score improved significantly from 59.14 (range: 43.6–73.21) preoperatively to 23.39 (range: 8.03–34.2) postoperatively at the final follow up (p = 0.0003) (Fig. 7).
Fig. 7.
The functional assessment by DASH score in pre-operative and at final follow up.
(* P= 0.0003)
4. Discussion
Patients with non-union with implant failure previously treated with internal fixation by plating, exhibit profound metal reaction leading to metallosis with implant breakage, metal debris, bony erosion with extensive bone loss, scalloping around screws and osteopenia. These cases are relatively uncommon, especially difficult to manage with routine procedures and there is dearth of literature regarding management, which is a challenge for orthopaedic surgeons. While a number of methods of management of atrophic non-union have been described each has its own drawbacks.10 Osteosynthesis with plating, intramedullary nailing, and Ilizarov technique have been described in various studies.10, 11, 12, 13, 14, 15, 16, 17, 18, 19 Bone grafting in the form of iliac crest bone graft, fibular strut graft either vascularised or nonvascularised, and autologous or allograft have been described in the management of non-union of humeral shaft fractures.
Dynamic compression plating has been utilized by several authors in the management of the non-union humeral fractures and high rates of union have been claimed.13, 20, 21, 22 It enables compression at fracture site, correction of axial malalignment, stimulation of osteogenesis (by shingling and bone grafting) in a single procedure. It can be applied with great success in non-union humeral fractures that have been managed conservatively with reasonable bone quality and without any implant in situ at the time of osteosynthesis. However, in cases of implant failure with poor bone quality and screw purchase, instead of DCP, LCP may be a reliable option.19, 23 But, as observed in the present study, in cases with extensive bone destruction due to previous implant even LCP alone may not provide adequate stability and may not be a reliable option alone.
Osteopenia as a result of disuse, due to generalised metabolic cause, and previous implant stress shielding along with previous screw hole will interfere with the strength and purchase of the screws inserted subsequently during osteosynthesis.24, 25 Polymethylmethacrylate (PMMA) bone cement has been used to augment the purchase of the screws in osteoporosis, but it carries risks of foreign body reaction, infection, harmful effects on bone vascularity and on fracture healing, in case of inadvertent extrusion into the fracture site.26, 27 It may also cause death of the adjacent cells and inhibit biologic aspects of healing due to heat liberated during exothermic reaction. Many techniques have been suggested for improving the strength and purchase of screws like exchange of loose 4.5 mm cortical screws with 6.5 mm cancellous screws, onlay and inlay fibular strut graft and application of supplementary intramedullary plate to substitute for a deficient opposite cortex.14, 8, 29 Double plating using two DCP at right angles to each other has also been described.6 But onlay graft and double plating require extensive soft tissue stripping and devascularisation of humerus.
Screw purchase is directly related to the cortical thickness and bone mineralization.24, 30 The concept of quadricortical plating through intramedullary fibular strut graft was first described by Wright et al.7 In his cadaveric study on biomechanical properties of strut graft, he demonstrated that the construct strength of quadricortical fixation was similar to that of bicortical fixation augmented with bone cement and significantly stronger than bicortical fixation. This improved mechanical environment may reduce risk of fibrous non-union or failed fixation that can occur as a result of excessive motion and osteoporotic bone.
Locked intramedullary nailing has been used for primary osteosynthesis of humeral shaft fractures. However, exchange nailing or nailing in post implant failure cases is not successful in humeral non-union because of absence of cyclical loading due to weight bearing and higher amount of distractive and torsional loads on the humerus.17 In addition, intramedullary nailing has been reported to carry higher complication rates including persistent shoulder pain, subacromial impingement, rotator cuff injury, iatrogenic fracture comminution or progression, and higher rates of delayed and non-union.31, 32 Unreliability of exchange nailing for management of non-union humeral fractures has further been documented by several authors.16, 17
The Ilizarov external fixation has been used by several authors in the management of humeral non-union.10, 11, 15, 18 However, the disadvantages with this procedure include presence of bulky apparatus on the arm, pin tract infections, painful impingement of the frame on the trunk and risk of neurovascular injury associated with wire insertion. It has a distinct advantage in the management of infected non-union. Time commitment, complexity of procedures, and non-compliance of the patients make it an unreliable and rather unnecessarily complex option in non-infected non-union.
The role of vascularised fibular graft in humeral non-union with bone defect has been described by several authors with successful union rate.5, 28, 29, 33 But the technically demanding nature of the surgery, need for micro-vascular surgical procedure and increased cost of surgery make it an unreliable option in developing countries with less hospital infrastructure. Moreover it has been associated with risk of thrombosis of vascular pedicle. In elderly people with atherosclerotic disease vascularised fibular graft is contraindicated.
The nonvascularized fibular graft is easy to harvest with least possible tissue trauma and least graft site morbidity. The cortical bone gives immediate structural stability at fracture site. Intramedullary fibular strut act as an internal splint giving stability at fracture site and also increases screw purchase as described by Wright et al.7 Several authors have shown successful results with the non-vascularized fibular graft (Table 2).7, 15, 34, 35, 36, 37, 38, 39 However, the grafts longer than 6 cm have been shown to have decreased capacity for incorporation and healing. 28, 40 The drawbacks to this technique are possibility of disruption of both endosteal and periosteal blood supply, iatrogenic fracture during insertion of graft and possible nerve palsy.
Table 2.
Comparison with other studies in the literature where fibular graft was used in treating humeral non-unions.
| Study | No of Subjects (FG Used) | Properties of Study; Procedure Done | Average Age (yrs) | Mean Interval of Nonunion | Mean Follow Up (months) | Duration of Union (months) | Results | Complications |
|---|---|---|---|---|---|---|---|---|
| Wright et al.7 | 9 (9) | 8 cases of failed fixation; DCP + Allograft in 4 pts & Autograft in 5 pts, also biomechanical analysis of fibular graft assessed | 49.8 (28–67) | 16.25 (3.5–72) months | 38.6 (12-74) | 3.37 (3-4) | 8 achieved union | 1-nonunion, 1- radial nerve palsy, 1-supracondylar fracture, 1- peroneal nerve palsy |
| Farouk O et al.38 | 10 (10) | 3 cases of failed plating; DCP + FG | – | 16 (6–36)months | 10 (8–16) | 4 (3–6) | 10 achieved union | stress supracondylar fracture |
| Vidhyadara S et al.39 | 6 (6) | in osteoporotic humerus, 1 case of failed fixation; DCP + FG | 65.33 (54–84) | 13.33 (7–26) months | 15.83 (11–24) | 3 | all achieved union DASH score 84 ± 5 to 28 ± 13 | 1- transient peroneal nerve palsy, 1-iatrogenic splinter, 2-superficial infection |
| Kilic A et al.34 | 4 (4) | 3 cases of failed fixation; DCP + FG | 67 (65–69) | – | 48 (36–72) | 3.2 (3–4) | union in all DASH score ≥58–17 | nil |
| Erder ER et al.35 | 5 (5) | 2 cases of failed plating; LCP + FG | 49.2 | 70 (24–128) months | 22.8 (12–36) | 5 (4–5.5) | union in all with Constant Murley score of 88 | nil |
| Gopisankar et al.36 | 7 (7) | infected nonunions with mean previous surgery of 2.7; DCP + FG | 40 (29–59) | – | 15 (13–24) | 5.4 (4–8) | 6 achieved normal function, 1 has brachial plexus injury with poor outcome | 2 case of wound infection |
| Padhye KP et al.15 | 35 (4) | infected, noninfected, osteoporotic nonunion included. Ilizarov, plating ± BG | 42 (24–71) | – | 16 (6–60) | infected-6.5, noninfected − 5, osteoporotic- 10 | union achieved in all | pin site complications in Ilizarov cases |
| Willis MP et al.37 | 20 (20) | 10 cases of failed fixation, LCP+ fibular allograft | 61 (44–81) | – | 36 (12–94) | 4 | 19 achieved union with normal daily activities | 1- nonunion, 3-adhesive capsulitis of shoulder |
| Kumar MN et al.23 | 24 (3) | all cases of failed fixation, LCP ± BG | 41.04 (24–57) | 26.3 (7–276) months | 39 (27–65) | – | 23 attained union, | 2- delayed union,1- persistent nonunion, 2- transient radial nerve palsies |
| Our Study (2015) | 17 (17) | 17 cases are previously operated, 2 cases operated twice | 40.11 (26–57) | 53.17 (6–168) months | 33.41(12–94) | 3.5 (3–5) | 16 attained union with DASH score ≥59.14–23.39 | 1- implant bending, 1- transient radial nerve palsy, 1- transient ulnar nerve palsy, 1-iatrogenic splinter during implant removal. |
(FG – Fibular Graft, BG – Bone Graft, DCP – Dynamic Compression Plate, LCP – Locking Compression Plate.
To the best of our knowledge, present study is the largest comprising 17 cases where autologous fibular graft was used in humeral shaft nonunions after failed plate fixation (Table 2). Wright et al.,7 was first to describe the use of intramedullary fibular strut graft along with DCP in non-union humeral fractures. They used both autograft and allograft in 8 patients. Vidhyadhara et al.,39 described the use of intramedullary fibular strut, as a novel adjunct to plating in atrophic non-union of humerus in 6 patients. Kumar et al.23 studied 24 cases of humeral shaft nonunions following failed internal fixation treated with LCP and autologous bone graft. Only three cases were treated with fibular graft. In our study we have used DCP in all cases except three where we have used LCP and we are of the opinion that LCP is not mandatory in treating these type of cases so long as fibular graft is used as an adjunct. The drawback of present study was that it is not a comparative study and cannot differentiate between the use of LCP and DCP in implant failure non-union humerus with significant cortical defect; we also did not have a matched control group treated without use of fibular graft.
We have observed that patients with non-union humerus previously treated with plate fixation present late despite non-union, which is the reason for metallosis, bone loss around screws necessitating the use of fibular graft. We had patients who presented as late as 10–14 yrs (vide Section 2.2 and Table 1). In our study, the average length of fibular graft used was 10.88 cm (range: 6–15 cm). According to current literature, a nonvascularized fibular graft >6 cm has relatively decreased capacity for incorporation and healing.5, 28, 40 Augmentation with iliac crest graft, as we have done in 4 cases, in the presence of large cortical defect created by previous implant will increase the incorporation and healing; and probably combination of longer fibular graft and iliac crest graft may form an alternative to complicated vascularised fibular graft procedures in developing countries. But to confirm, we need to do similar study in larger population group along with a control group.
5. Conclusion
The findings from our study show that revision plating along with autologous nonvascularized fibular graft is a reliable option in humeral diaphyseal non-unions with failed plate-screw osteosynthesis with significant cortical defect to achieve adequate screw purchase, stability at fracture site and high chance of union with good functional outcome.
Conflict of interest
The authors have none to declare.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgement
The authors would like to thank Dr. Vijay Kumar Kutala for his valuable help in statistical analysis and proof reading of the article.
References
- 1.Garnavos C. Humeral shaft fractures. In: Court-Brown C.M., Heckman J.D., McQueen M.M., Ricci W.M., Tornetta P., editors. Rockwood and green fractures in adults. 1st, 8th ed. Wolter Kluwer; 2015. pp. 1287–1340. [Google Scholar]
- 2.Sarmiento A., Horowitch A., Aboulafia A. Functional bracing for comminuted extra-articular fractures of the distal third of the humerus. J Bone Joint Surg Br. 1990;72(2):283–287. doi: 10.1302/0301-620X.72B2.2312570. [DOI] [PubMed] [Google Scholar]
- 3.Castella F.B., Garcia F.B., Berry E.M. Nonunion of the humeral shaft: long lateral butterfly fracture?a nonunion predictive pattern? Clin Orthop Relat Res. 2004;424:227–230. [PubMed] [Google Scholar]
- 4.Volgas D.A., Stannard J.P., Alonso J.E. Nonunions of the humerus. Clin Orthop Relat Res. 2004;419:46–50. doi: 10.1097/00003086-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Muramatsu K., Doi K., Ihara K. Recalcitrant posttraumatic nonunion of the humerus. Acta Orthop Scand. 2003;74:95–97. doi: 10.1080/00016470310013734. [DOI] [PubMed] [Google Scholar]
- 6.Rubel I.F., Kloen P., Campbell D. Open reduction and internal fixation of humeral nonunions: a biomechanical and clinical study. J Bone Joint Surg Am. 2002;84-A(8):1315–1322. doi: 10.2106/00004623-200208000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Wright T.W., Miller G.J., Vander Griend R.A. Reconstruction of humerus with an intramedullary fibular graft: A clinical and biomechanical study. J Bone Joint Surg Br. 1993;75(5):804–807. doi: 10.1302/0301-620X.75B5.8376445. [DOI] [PubMed] [Google Scholar]
- 8.Weber B.G., Cech O. Grune and Stratton; New York, NY: 1976. Pseudarthrosis: pathophysiology, biomechanics, therapy, results. [Google Scholar]
- 9.Hudak P.L., Amadio P.C., Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 10.Kontakis G.M., Tosounidis T., Pagkalos J. Humeral diaphyseal aseptic non-unions: An algorithm of management. Injury. 2007;38S:S39–S49. doi: 10.1016/s0020-1383(07)80008-8. [DOI] [PubMed] [Google Scholar]
- 11.Brinker M.R., O'Connor D.P., Crouch C.C. Ilizarov treatment of infected nonunions of the distal humerus after failure of internal fixation: an outcomes study. J Orthop Trauma. 2007;21(3):178–184. doi: 10.1097/BOT.0b013e318032c4d8. [DOI] [PubMed] [Google Scholar]
- 12.Allende C., Paz A., Altube G. Revision with plates of humeral nonunions secondary to failed intramedullary nailing. Int Orthop. 2014;38(4):899–903. doi: 10.1007/s00264-013-2180-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hierholzer C., Sama D., Toro J.B. Plate fixation of ununited humeral shaft fractures: effect of type of bone graft on healing. J Bone Joint Surg Am. 2006;88(7):1442–1447. doi: 10.2106/JBJS.E.00332. [DOI] [PubMed] [Google Scholar]
- 14.Hornicek F.J., Zych G.A., Hutson J.J. Salvage of humeral nonunions with onlay bone plate allograft augmentation. Clin Orthop Relat Res. 2001;386:203–209. doi: 10.1097/00003086-200105000-00026. [DOI] [PubMed] [Google Scholar]
- 15.Padhye K.P., Kulkarni V.S., Kulkarni G.S. Plating, nailing, external fixation, and fibular strut grafting for non-union of humeral shaft fractures. J Orthop Surg (Hong Kong) 2013;21(3):327–331. doi: 10.1177/230949901302100313. [DOI] [PubMed] [Google Scholar]
- 16.Martinez A.A., Cuenca J., Herrera A. Treatment of humeral shaft nonunions: nailing versus plating. Arch Orthop Trauma Surg. 2004;124(2):92–95. doi: 10.1007/s00402-003-0608-7. [DOI] [PubMed] [Google Scholar]
- 17.McKee M.D., Miranda M.A., Riemer B.L. Management of humeral nonunion after the failure of locking intramedullary nails. J Orthop Trauma. 1996;10(7):492–499. doi: 10.1097/00005131-199610000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Patel V.R., Menon D.K., Pool R.D. Nonunion of the humerus after failure of surgical treatment: Management using the Ilizarov circular fixator. J Bone Joint Surg Br. 2000;82(7):977–983. doi: 10.1302/0301-620x.82b7.10180. [DOI] [PubMed] [Google Scholar]
- 19.Ring D., Kloen P., Kadzielski J. Locking compression plates for osteoporotic nonunions of the diaphyseal humerus. Clin Orthop Relat Res. 2004;425:50–54. doi: 10.1097/01.blo.0000131484.27501.4b. [DOI] [PubMed] [Google Scholar]
- 20.Barquet A., Fernandez A., Luvizio J. A combined therapeutic protocol for aseptic nonunion of the humeral shaft: a report of 25 cases. J Trauma. 1989;29(1):95–98. doi: 10.1097/00005373-198901000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Healy W.L., White G.M., Mick C.A. Nonunion of the humeral shaft. Clin Orthop Relat Res. 1987;219:206–213. [PubMed] [Google Scholar]
- 22.te Velde E.A., van der Werken C. Plate osteosynthesis for pseudarthrosis of the humeral shaft. Injury. 2001;32(8):621–624. doi: 10.1016/s0020-1383(00)00231-x. [DOI] [PubMed] [Google Scholar]
- 23.Kumar M.N., Ravindranath V.P., Ravishankar M. Outcome of locking compression plates in humeral shaft nonunions. Indian J Orthop. 2013;47(2):150–155. doi: 10.4103/0019-5413.108899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ansell R.H., Scales J.T. A study of some factors which affect the strength of screws and their insertion and holding power in bone. J Biomech. 1968;1(4):279–302. doi: 10.1016/0021-9290(68)90023-7. [DOI] [PubMed] [Google Scholar]
- 25.Trader J.E., Johnson R.P., Kalbfleisch J.H. Bone-mineral content, surface hardness, and mechanical fixation in the human radius: A correlative study. J Bone Joint Surg Am. 1979;61(8):1217–1220. [PubMed] [Google Scholar]
- 26.Cameron H.U., Jacob R., MacNab I. Use of polymethylmethacrylate to enhance screw fixation in bone. J Bone Joint Surg Am. 1975;57:655–656. [PubMed] [Google Scholar]
- 27.Trotter D.H., Dobozi W. Nonunion of the humerus: rigid fixation, bone grafting, and adjunctive bone cement. Clin Orthop Relat Res. 1986;204:162–168. [PubMed] [Google Scholar]
- 28.Kerfant N., Valenti P., Kilinc A.S. Free vascularised fibular graft in multi-operated patients for an aseptic non-union of the humerus with segmental defect: surgical technique and results. Orthop Traumatol Surg Res. 2012;98(5):603–607. doi: 10.1016/j.otsr.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 29.Taylor G.I., Miller G.D., Ham F.J. The free vascularized bone graft: a clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55(5):533–544. doi: 10.1097/00006534-197505000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Schatzker J., Sanderson R., Murnaghan J.P. The holding power of orthopedic screws in vivo. Clin Orthop Relat Res. 1975;108:115–126. doi: 10.1097/00003086-197505000-00019. [DOI] [PubMed] [Google Scholar]
- 31.Putti A.B., Uppin R.B., Putti B.B. Locked intramedullary nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong) 2009;17(2):139–141. doi: 10.1177/230949900901700202. [DOI] [PubMed] [Google Scholar]
- 32.Robinson C.M., Bell K.M., Court-Brown C.M. Locked nailing of humeral shaft fractures: Experience in Edinburgh over a two-year period. J Bone Joint Surg Br. 1992;74(4):558–562. doi: 10.1302/0301-620X.74B4.1624516. [DOI] [PubMed] [Google Scholar]
- 33.Jupiter J.B. Complex non-union of the humeral diaphysis Treatment with a medial approach, an anterior plate, and a vascularized fibular graft. J Bone Joint Surg Am. 1990;72(5):701–707. [PubMed] [Google Scholar]
- 34.Kilic A., Arslan A., Mutlu H., Cetinkaya E., May C., Parmaksizoglu A.S. Fibula non-vascularized graft might be a practical solution for treatment of osteopenic humeral shaft non-union in elderly obese patients. J Acad Res Med. 2011;1:15–17. [Google Scholar]
- 35.Erden E.R., Arda C., Mesut S.M. Implementation of locking compression plate together with intramedullary fibular graft in atrophic type humeral nonunions. Eur J Orthop Surg Traumatol. 2012;22(8):661–665. doi: 10.1007/s00590-011-0900-0. [DOI] [PubMed] [Google Scholar]
- 36.Gopisankar G., Justin A.S., Nithyananth M. Non-vascularised fibular graft as an intramedullary strut for infected non-union of the humerus. J Orthop Surg (Hong Kong) 2011;19(3):341–345. doi: 10.1177/230949901101900316. [DOI] [PubMed] [Google Scholar]
- 37.Willis M.P., Brooks J.P., Badman B.L. Treatment of atrophic diaphyseal humeral nonunions with compressive locked plating and augmented with an intramedullary strut allograft. J Orthop Trauma. 2013;27(2):77–81. doi: 10.1097/BOT.0b013e31825360fa. [DOI] [PubMed] [Google Scholar]
- 38.Farouk O., El-Sherif E., Mostafa K. Intramedullary fibular graft and quadricortical plate fixation in atrophic non-union of the osteoporotic humerus. Injury extra [electronic resource] 2008;39(4):152–154. [Google Scholar]
- 39.Vidyadhara S., Vamsi K., Rao S.K. Use of intramedullary fibular strut graft: a novel adjunct to plating in the treatment of osteoporotic humeral shaft nonunion. Int Orthop. 2009;33(4):1009–1014. doi: 10.1007/s00264-008-0596-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Springfield D.S. Massive autogenous bone grafts. Orthop Clin North Am. 1987;18(2):249–256. [PubMed] [Google Scholar]