Abstract
Introduction:
Hand hygiene (HH) prevents the transmission of healthcare-associated infections. Electronic HH monitoring and prompt devices have been developed to overcome problems with monitoring HH and to improve compliance. Devices monitor room entry and exit and soap use through communication between ceiling sensors and badges worn by practitioners and the badges sense alcohol rub.
Objectives:
To investigate (1) the impact of devices on HH compliance, (2) how devices influence behaviour and (3) the experience and opinions of practitioners on the use devices.
Methods:
HH compliance was monitored (before, during and after system installation) by observations and alcohol rub usage. Compliance during installation was also monitored by the device. Healthcare practitioner interviews (n = 12) explored how the device influenced behaviour and experiences and opinions of wearing the device.
Results:
HH compliance improved during the period the device was installed. Practitioners reported the device increased their awareness, enhancing their empathy for patients and encouraged patients and colleagues to prompt when HH was needed. Practitioners’ reported better HH, gaming the system and feelings of irritation.
Conclusion:
HH prompt and monitoring systems seem to improve compliance but improvements may be undermined by practitioner irritation and system gaming.
Keywords: Hand hygiene, behaviour change, compliance, electronic monitor and prompt, healthcare-associated infections, infection control, qualitative research
Introduction
Healthcare practitioner (HCP) compliance with hand hygiene (HH) is considered the primary measure of preventing the transmission of healthcare-associated infections (HCAIs) with research suggesting that up to 50% of such infections could be avoided with improvements in HH (Pittet et al., 2009). Observation is considered the current gold standard for assessing compliance with HH but has a number of limitations particularly the Hawthorne effect (Kohli et al., 2009; Kovace-Litman et al., 2016). As a result of this, electronic real-time locating systems have been developed which, as well as monitoring HH, may also improve HH by giving prompts (e.g. a badge worn may change colour or emit a sound). There have been three recent systematic reviews that report system impact, reliability, implementation challenges and staff design preferences. Srigley et al. (2014) reviewed impact on compliance and found an improvement in HH on entry to or exit from an area. Ward et al. (2014) reviewed all published material relating to HH monitoring and prompt systems and reported challenges to implementation including cost and the need to protect privacy. This review also considered staff preferences relating to systems and found (for example) a preference for vibration rather than audible prompts. The extent of coverage of monitoring systems was also considered in this review Based on Pittet et al. (2009) five moments of hand hygiene and the authors found coverage was largely restricted to moments 1 and 4 (before and after touching a patient). Finally, with regard to reliability, the authors found the accuracy of systems variable. Dawson and Mackrill’s (2014) review also investigated the extent of coverage of systems and found that no available system was able to measure moments 2 and 3 (before and after a procedure). These authors cite Vicente (2006) and suggest, when developing optimal HH monitor and prompt systems, we need to: (1) understand what governs human behaviour and (2) understand how HCPs want to be monitored and the personal acceptance of technology.
In relation to understanding what governs human behaviour, there is substantial evidence to suggest strategies to enhance clinical practice need to be according to behavioural determinants (Baker et al., 2010) and theoretically underpinned if they are to be effective (Bonetti et al., 2005; Davies et al., 2010; Grol et al., 2005). A recent systematic review of the theoretical underpinnings of HH improvement strategies found addressing behavioural determinants such as knowledge, awareness, action control and facilitation is not enough to improve HH; addressing combinations of different determinants leads to better results (Huis et al., 2012). Electronic HH prompt and monitor devices are reported to influence by means of reminders or even by way of the Hawthorne effect (Srigley et al., 2014) but there is no evidence of investigation to establish whether this is the case or which behavioural determinants these systems might address.
As for understanding how HCPs want to be monitored and the personal acceptance of technology, only three relevant studies were identified in the literature that investigate this. Boscart et al. (2008) conducted focus groups to explore the experience of wearing a prototype version of the technology and although practitioners were positive they expressed concerns about who could access the HH data and their intended use. Ellingson et al. (2011) conducted focus groups of practitioners who identified concerns about the accuracy of systems, potential punitive use of the data and they suggested the system indicated a lack of trust in their standards. Levchenko et al. (2010) conducted interviews with nurses who were prompted when they considered it was not necessary.
Aim
Our aims were to investigate:
Whether a monitoring device improves HH compliance,
How devices influence HH (that is, what governs human behaviour within this context?),
The experiences and opinions of HCPs of devices (that is, how do practitioners want to be monitored?).
Methods
The technology was installed in two units of a large general hospital in the north of England. It was battery operated and therefore required no wiring or extensive installation and comprised of a badge, room sensors and a plug-in base station. The badge that was worn by practitioners was a small, light device (approximately 50 g) which they clipped to their tunic breast pocket. The badge could detect the infrared sensors that were installed above the doors and entrances to a patient’s bed space This was a proxy measure of ‘before touching a patient’ and ‘after touching a patient/a patient’s surroundings’ (HH moments 1 and 4/5) (Pittet et al., 2009). The units chosen had predominantly single bed spaces (separate rooms or a cubical system), but in both units there were curtain-separated areas within bays of several beds. The badges also contained in-built alcohol sensors and red, amber and green LEDs. When the HCPs cleaned their hands with gel, they could hold a hand near the badge and the badge would detect clean hands. If the HCPs chose to clean their hands with soap and water, this was recognised by a ceiling sensor over sinks so long as the practitioner was there for 2 min or more. In both instances, the badge would display a green light. If, however, the HCP failed to clean their hands within 10 s the badge would turn amber, after 15 s the badge would sound an audio alert, and after 20 s it turned red and gave a further audio alert. HH compliance information was communicated to the base station (which also acted as a unit to charge the badges between work shifts) and from here data were transferred securely to computer systems via the hospital’s wireless computer network. These data could be accessed at the level of individual practitioner by the infection prevention and control team.
HH compliance was measured in both units by observation as per usual practice, through recordings generated by the device and through monitoring the ordering of alcohol rub. Three HH measures were considered for triangulation purposes each having different strengths and limitations. To assess the possible mechanisms by which the system may influence HH and to establish experiences and opinions regarding the device, semi-structured interviews were conducted by an independent researcher with practitioners from both units who had experienced the badge. During the period of the study one unit experienced unexpected numbers of patients resulting additional beds being brought into the space after the technology was installed. This resulted in the misalignment of sensors with bed spaces and a potential increase in gel usage due to greater patient and temporary staff numbers. Due to these confounding factors, we ceased to monitor and do not report compliance data in this unit. Interviews, however, had taken place prior to this change and were therefore retained as part of the dataset.
Participants
Participants were HCPs on an emergency unit and a medical inpatient unit. HH opportunity (HHO) was according to usual practice. Observations by the infection prevention control team (IPCT) tended to be about 20 min each session and were conducted randomly on a daily basis. Observations could be anything from one upward (depending on what HCPs were doing at that time) with an average of 50 HHOs per month. Routine observations of HH involved all staff. Observations relating to nurses (registered and unregistered) and doctors were included in the study as these were the groups wearing electronic device.
Electronic monitoring involved all but one HCP from the medical inpatient unit (who declined to participate). The practicalities of wearing monitoring badges involved the practitioner taking their badge out of the docking station at the beginning of the shift and replacing it at the end of the shift. The IPCT visited the units twice daily to remind teams to wear their badges where necessary. Due to the changes in the environment of the emergency unit during the study period (described above), we were unable to use compliance data.
The medical inpatient unit (from which we present compliance data) consisted of 18 practitioners (mostly nurses, healthcare assistants and doctors). While there were visiting practitioners (allied health professionals, e.g. physiotherapists), they were not included in the study. Doctors wore the badge for the whole shift despite often working across more than one unit (for convenience).
Those interviewed were sampled from both units, purposively selected from three key job roles: doctors, registered nurses and healthcare assistants; as these represent the largest proportion of HCPs who had contact with patients. Unit selection was according to convenience due to ward layout (predominantly single rooms or cubicles which worked better with the electronic system) and range (an emergency and a routine care unit). Ethical approval was obtained from the University of Hull, Faculty of Health and Social Care Research Ethics Committee (ref: FHSC-170), Research Governance approval was obtained from the NHS trust involved in the study; participants gave written informed consent to participate.
Interviews with staff
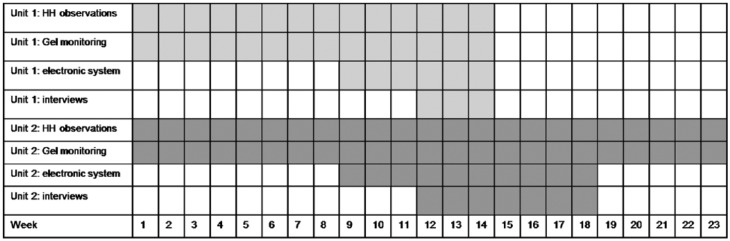
HH monitoring was as described above. Semi-structured interviews were undertaken over a seven-week period from January 2015. Purposive sampling identified a range of participants according to professional role. Recruitment took place through ward managers in each of the two areas. Participants were interviewed in the work place in a private room away from the practice area. We conducted interviews after the system had been installed for three weeks to allow for any system glitches to be resolved. We conducted interviews at a range of times during the installation period to accommodate for any initial novelty reaction and to accommodate any desensitisation to the presence of the badge. Figure 1 shows the study timings with regard to HH monitoring and interviews.
Figure 1.
Data collection period.
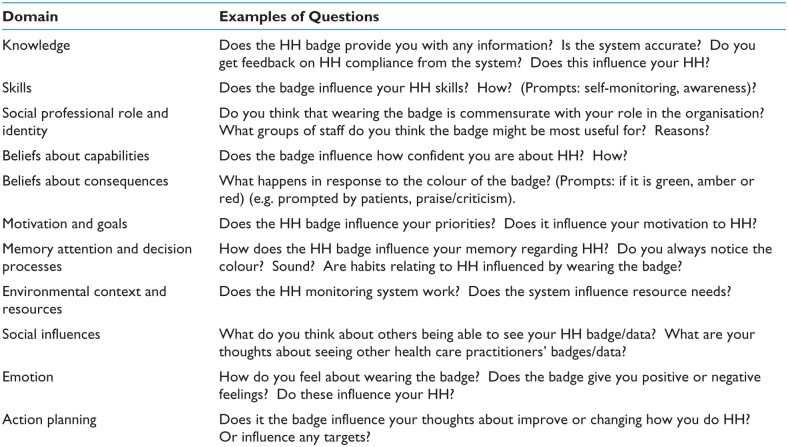
To understand how the system might influence HH behaviour, questions were designed using the 11 domains of the Theoretical Domains Framework (TDF) which offers a comprehensive set of potential behavioural determinants (Michie et al., 2005). The domains are: knowledge, skills, social professional role and identity, beliefs about capabilities, beliefs about consequences, motivation and goals, memory attention and decision processes, environmental context and resources, social influences, emotion and action planning. Figure 2 offers examples of questions asked according to these domains. By underpinning the interview question schedule with theory, we seek to achieve a deeper and more accurate understanding of how the system influences behaviour. To establish practitioners’ experience and opinions of the system they were simply asked their views and opinions about the system based on their experience of it.
Figure 2.
Examples of interview questions according to the Theoretical Domains Framework.
Data analysis
HH observations undertaken by the IPCT were recorded weekly and expressed as a percentage of HH completed as a proportion of HHOs. The HHOs included noting the role of the person being observed which enabled us to present data for only the groups wearing the HH badge. The HHOs were audited using a bespoke tool used by the NHS trust and consisted of: (1) before patient contact; (2) after patient contact; (3) after contact with the patient’s surroundings; and (4) after removing gloves. Electronic monitoring was recorded for all (enter/exit) HHOs during the period the system was installed and were also expressed as percentage of HH completed compared with HHO. The amount of hand gel ordered by the unit was recorded weekly. Interviews were digitally recorded and transcribed verbatim. A thematic analysis (Braun and Clarke, 2006) was conducted with themes identified according to the reported mode of influence of the system on HH behaviour and according to experience and opinion about the system.
Results
Participants
Six semi-structured interviews were conducted in each unit (n = 12) with four staff nurses, three charge nurses, two doctors and three nursing assistants. Participants had between three and 21 years of clinical experience. At the time of interview participants had engaged with the system for between three and ten weeks. Interview 9 appears to be the data saturation point (Miles and Huberman, 1994) as no new information was offered relating to how devices work or experiences and opinions of the system in the remaining three interviews.
Do devices influence HH compliance?
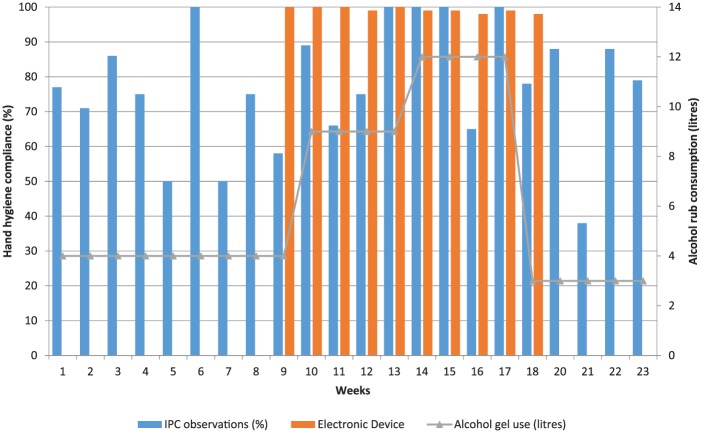
IPC observations were in the range of 38–100 HHOs per week. Electronic observations monitored 15–20 staff each week. According to IPC team observations, HH compliance went from a mean of 73% in the eight weeks before installation to 83% during the ten-week period the electronic device was installed and went back to 73% after the system was removed (measured over a period of four weeks). The electronic monitoring system recorded compliance at 98–100% throughout the period of its installation. The amount of alcohol hand gel ordered went from an average of 4 L before, 10 L during and 2.5 L after installation (Figure 3).
Figure 3.
HH according to IPC observations, alcohol rub usage and electronic device before, during and after system installation.
How do devices influence HH behaviour?
Practitioners reported three ways in which they considered the badge influenced HH: (1) prompt (by the badge flashing and making a sound or by people referring to the badge); (2) empathy for the patients, how they might feel if they saw evidence of missed HH; and (3) by increasing awareness of HH frequency.
Prompt
The electronic system (badge) was reported to prompt HH through its change in colour, the noise it emitted or by other people referring to the badge.
‘It does prompt you, things like walking in and out of rooms. Definitely prompts then.’ (5: Nursing Assistant)
‘They probably prompt more than anything else.’ (9: Charge Nurse)
However, there was also some acknowledgement that people could become desensitised to the prompt.
‘They just get blind with it.’ (12: Nursing Assistant)
‘Desensitised they are. I saw a lot of people coming into the cubicle and just turning it off.’ (6: Doctor)
Not only did the badge prompt HH directly, practitioners also referred to comments made by patients or colleagues. People reported it easier to refer to a flashing or red badge than to ask someone to clean their hands.
‘It’s very visual good for patients and relatives because prior to this last year and the year before we had to wear a badge, please ask me if I have cleaned my hands which is a bit insulting actually. But this is better it gets people talking they say oh what’s that? Why is that flashing?’ (9: Charge Nurses)
‘They [patients] say, it is flashing, it is flashing.’ (1: Staff Nurse)
‘They do it in a jokey manner. You know, you might say, you are going in there to do a catheter and look at your badge, it is easier to do it like that.’ (7: Staff Nurse)
Empathy for the patient
The badge offered evidence to patients about whether practitioners had cleaned their hands. Practitioners wanted patient to feel confident in the care they were receiving.
“I think it does give them [patients] confidence that they know that you are doing it [HH].’ (7: Staff Nurse)
‘So it does show patients that we are compliant.’ (1: Staff Nurse)
‘It turns different colours and that can make a human-being, a patient, very anxious… You don’t want that. You clean your hands. Or you take it off. It is better to have a vibrator, it is better than the visual, the visual is a vehicle for other persons. It is not a vehicle for you.’ (6: Doctor)
Increased awareness
Practitioners reported the electronic system made them more aware of HH and, in particular, the frequency required.
‘I think we are all much more conscious of it [HH].’ (12: Nursing Assistant)
‘It does, perhaps it does open your eyes as to how often you go between patient environments.’ (5: Nursing Assistant)
‘I think it does work; you can see them thinking, oh, I should have probably done it a bit more before.’ (7: Staff Nurse)
What are the experiences and opinions of HCPs of devices?
Four themes were identified with regard to the experiences and opinions of the electronic device. These were relating to: (1) compliance with HH; (2) use of the data generated by systems; (3) system accuracy; and (4) HCPs emotion when using the system.
Compliance with hand hygiene
Most practitioners said although their HH practice was already good, it had improved since the system was installed. Responses were moderate when positive, but no practitioner suggested the system’s effect had been detrimental to HH.
‘We did it [HH] anyway; we are more aware of it now.’ (1: Staff Nurse)
‘We are pretty good here anyway, but that said, maybe there was room for improvement, there was a lot more flashing the first week than there is now.’ (10: Staff Nurse)
Use of data
This theme relates to how the compliance data generated from the system would or could be used. Some practitioners welcomed the opportunity to see their own data in order to consider their performance and some were concerned that sharing data would lead to criticism or other undesirable outcomes. There was agreement that group data would be more acceptable than individual data and that all data should be presented supportively.
‘We would use it [data] between ourselves to improve hand hygiene on the unit.’ (1: Staff Nurse)
‘People should not be able to see individual level data. If you do that you are singling out individuals.’ (6: Doctor)
‘They need to find the positives, say how good you are, tell them it that way. If anyone is really bad at hand washing, pull them aside and have a quiet word.’ (9: Charge Nurse)
System accuracy
There was a consensus from all practitioners interviewed that the system was not yet accurate. There were four reasons cited for this: the perception that the system was designed to better measure gel than soap; system failure; practitioners gaming or cheating; and the limited intelligence of the system. Each of these will be considered in turn.
Gel use
The majority of participants identified that their use of gel had increased but that this was at the cost of using soap and water. Practitioners found that the badges were more responsive to gel than to the sensors by the soap. A small number of practitioners suggested that purpose of the system was to increase alcohol rub sales.
‘I am using more gel, a lot more gel, I am hand washing less. You have to do it or it won’t work [badge] so you have no choice you’ve got to do it. I am gelling more. Our gel use has gone up. Selling gel, that’s what this is.’ (4: Nursing Assistant)
‘I think that is this thing’s major flaw, the badge doesn’t really recognise the soap and water so well.’ (10: Staff Nurse)
‘Well it’s this. You think it’s [the badge] gonna flash so you gel. Even when you don’t need to. Even when I have washed. And look they are getting a bit sore. Doubling up. The nature of it [the work] you need to wash your hands with soap and water before… so it is just doubling up. Doing it twice.’ (3: Charge Nurse)
System failure
Participants identified problems with the sensors which sometimes failed to sense a practitioner had cleaned their hands, sometimes HH was prompted by the badges when a practitioner was not near a sensor and a great number of practitioners considered that the time from entering the room to the badge showing red was unreasonably short.
‘They go off without us doing anything at all. So if you are walking down the corridor, I don’t know why, it just goes off… every time I gelled, it was still flashing.’ (2: Staff Nurse)
‘When it flashes red and you have not done anything it does get a bit soul destroying. Things like that, it puts you off. You only get a minute and you’re feeling that you have to rush. Sometimes you can go red even when you have washed your hands.’ (3: Charge Nurse)
‘It bleeps randomly.’ (4: Nursing Assistant)
Gaming
Some practitioners had thought about manipulating the system, others reported having seen such manipulation and a minority of practitioners reported having engaged in gaming. Often this was linked with system errors or in situations where practitioners believed the system expected HH unnecessarily. Practitioners said they were unwilling to have inaccurate or unfair data recorded against them.
‘I want to leave it on top of the trolley. I was going to attach it to a gel dispenser.’ (2: Staff Nurse)
‘I put some gel on the badge for them.’ (4: Nursing Assistant)
‘People will just go and stand near a sink and not necessarily do anything.’ (11: Charge Nurse)
Intelligence
Practitioners reported having no faith in the accuracy of data recorded as the system at times expected HH when the practitioners themselves considered it unnecessary.
‘So you have to get your gloves on and your apron on. You have taken the urine bottle out and then you have to put it down on the floor to step out to gel and… this doesn’t think and it doesn’t let me think.’ (4: Nursing Assistant)
‘Even if you didn’t do anything, just because you enter an area… they are only sensors, it doesn’t have a brain.’ (6: Doctor)
Feelings about the system
Many emotions were expressed when practitioners discussed their experiences of the system; irritation and frustration were the most frequently mentioned. Practitioners acknowledged the value of the system but expressed reluctance in being monitored.
‘Sometimes it’s quite distracting this amber light flashing then starts flashing red, sometimes that is not appropriate. I know there is an emergency button but you get a bit frustrated.’ (1: Staff Nurse)
‘It’s like laser quest, you think, oh, stop it.’ (3: Charge Nurse)
‘It’s like the big brother show on the telly I am telling you.’ (4: Nursing Assistant)
‘It bleeps all of the time. It is a nuisance… irritating at the moment… it is irritating. It causes concern.’ (6: Doctor)
‘I feel positively about them, I think, overall [but] it causes yet another distraction in a stressful situation. When washing your hands is the least of your priorities.’ (8: Doctor)
Discussion
Do devices influence HH compliance?
During the period in which the electronic monitoring system was installed, HH practice was improved according to IPC team observations and hand gel usage. According to the electronic system, HH compliance was in the range of 98–100% during installation. Once the system was removed, HH compliance fell to pre-installation levels according to observations and gel usage. The findings relating to improved compliance are consistent with previous research (Edmond et al., 2010; Marra et al., 2014; Sahud et al., 2012; Swoboda et al., 2004; Venkatesh et al., 2008), though ours is the only study we are aware of that has taken place in the UK.
How do devices influence HH behaviour?
Of the badge systems that are reported in the literature, there is a general assumption that they may be effective through the process of prompt or the Hawthorne effect created by monitoring (Strigley et al., 2014). This study identified three ways the systems influenced HH behaviour: prompts; empathy for the patient; and increased awareness of the need for HH. Each of these will be discussed in turn.
Practitioners reported the system prompted directly through changing colour or emitting a sound or indirectly through practitioners or patients referring to or asking about the changed badge. Most practitioners were aware of being prompted when they entered or left a room (room entry and exit being proxy measures of HH moments 1 and 4/5). For other practitioners, the indirect prompt from HCPs or patient was what alerted them to the need to clean their hands. With regard to patient prompts, HCPs observed that it was easier for them to mention a badge changing colour than asking practitioners directly to clean their hands. The UKs National Patient Safety Agency ‘cleanyourhands’ campaign identified that 57% of the public were unlikely to question HCPs, 43% of patients considered practitioners should know to clean their hands and 20% would not want HCPs to think they were questioning their ability to do their job (Pittet et al., 2011) . It may be that referring to a changed badge mitigates reluctance to speak up. In terms of empathy for their patients, HCPs noted that a green badge was likely to offer reassurance whereas a red badge would cause some anxiety. Both the awareness of patient comfort in the case of a green badge (HH) and the risk of upset at seeing a red badge (failure to HH) resulted in greater intentions to clean hands. In one case, the option of removing the badge to prevent patient anxiety was suggested. It could be argued that there was indirect reference to the Hawthorne effect as patients observed compliance through the colour of the badge (versus direct observation of the behaviour). However, the data support practitioner behaviour being determined by caring for others rather than being judged by them. Practitioners reported being more aware or more conscious of their HH, in particular, the frequency. Indeed, during the study period there was an increase in HH compliance according to usual observations and gel usage. It is not possible to attribute the improvements in HH during the period the technology was installed to one or more of the modes by which practitioners suggest the badge worked (prompt, empathy or awareness). It is, however, clear from the data presented here that the influence of the system was not sustained after it was removed.
What are the experiences and opinions of HCPs of devices?
The themes identified from interview data compliance with HH, the use of the data generated by systems, system accuracy and HCP feelings when using the system will be discussed in turn. There was a consensus of opinion that the system generally led to improved compliance with HH (validated through usual HH observations) but these responses were modest in their emphasis and have to be considered against other data in particular with regard to system accuracy. Practitioners strongly questioned the accuracy of the system. One issue raised was the greater sensitivity of the system to gel use compared with soap usage. Although practitioners did not suggest failing to use soap when this was indicated (e.g. potential exposure to Clostridium difficile [Pittet et al., 2009]), they did talk about washing with soap and immediately following with alcohol gel to prevent the badge reacting as if HH had not taken place. This potentially undermined the positive impact of the badge with one practitioner suggesting the purpose of the system was to increase gel sales rather than to support patient care. The limits of system intelligence further undermined any positive impact of the system. Practitioners offered good reasons when they would not engage in HH but system expected it nonetheless. This led to practitioners questioning their own judgement (e.g. ‘it doesn’t let me think’) and indeed potentially guiding the wrong practice. This, along with system failures where, for example, the system failed to sense hands had been cleaned, left the practitioner with too little time to complete HH or the badge changed without a sensor being passed led in some cases to gaming the system to avoid inaccurate data being recorded against them. Despite a general perspective among participants that the system improved HH, feelings toward the system were generally negative. Despite acknowledging the override button (‘I know there is an emergency button’), practitioners found the system irritating, frustrating and distracting when it prompted unnecessarily (through error or lack of intelligence/system limitation) and resentment was expressed regarding their practice being monitored and guided in such a way; the judgement of a machine over that of human being. With regard to the use of data, some HCPs were interested to see their own data in order to improve their individual practice. They were also in favour of group data being shared (e.g. by professional group as per usual practice within this NHS trust). However, they were against individual level data being shared with others for fear of criticism believing that the management of poor performers should be a private matter between them and their line manager. There is little reported regarding the practitioners’ experiences and opinions of such systems with which to compare our findings. However, previous research reports of systems lacking the intelligence to judge the situational context (Boscart et al., 2008; Ellingson et al., 2011) and there is evidence of disparity between human with electronic observations to an extent of 38% (Sharma et al., 2012). Ellingson et al. (2011) also identified a reluctance in being monitored and concerns about compliance data being used unwisely. By contrast, none of the participants in the focus groups conducted by Boscart et al. (2008) expressed any such concerns. Audit and feedback is known means of enhancing clinical practice (Grimshaw et al., 2004) and is not new to the practice of HH (e.g. the aforementioned cleanyourhands campaign). Although we found no instance of individual electronic HH audit data being fed back to practitioners, there are cases whereby individual level data from HH observations are offered to practitioners by way of feedback to support improvement (Fuller et al., 2012). This would suggest that there may be a place for the use of individual level HH data as a means of improvement. Based on the reluctance and fears of the practitioners in this study, it is clear that this would need to be sensitively and supportively executed.
Strengths and limitations
One of the strengths of this study is the explicit investigation of the behavioural determinants addressed by HH monitor and prompt systems and the acceptability of such systems to practitioners. This study is also subject to some limitations. We were only able to report HH compliance from one of the two areas in which the system was installed. During the study period, in the second unit an unexpected high volume of admissions led to additional and temporary bed spaces being created causing misalignment of the ceiling sensors with the entrances with some bed spaces and having a potential confounding impact on gel usage. Interviews had taken place prior to this change and we therefore report these. It was not possible to unpick the HH compliance data sufficiently to report them. Another limiting factor, it was infeasible to measure alcohol rub actual usage and we therefore relied on the stock ordering data to estimate usage. While orders are made according to stock levels and anecdotal evidence dismisses stock-piling, it is not possible to be accurate in the amount of alcohol rub used. We did not measure soap usage during the study. Only through the practitioner views presented here do we understand that the system may support gel over soap; this was not predicted and we have found no other evidence in the literature to suggest this is the case. However, from the data here it is possible that where there were increases in gel usage there may have been concurrent reductions in soap usage. Gel usage in this study is therefore not a reliable indicator of increased HH.
Our interviews took place over a seven-week period to mitigate for any changes in the experience of the badge over time (e.g. the honeymoon effect or desensitisation to the intervention). Future research exploring practitioner experience and opinion where systems have been in situ for longer periods would be beneficial.
Recommendations
According to the findings of this study, further work is required to refine electronic HH monitoring systems. Our participants report irritation and frustration at system failure and lack of ‘intelligence’ (being prompted when HH is not necessary). The findings of this study suggest that electronic HH monitor and prompt systems may improve compliance and that systems appear to impact a range of behavioural determinants. This may be undermined if practitioners have no faith in the accuracy of the system. Consideration needs to be given to most effective and acceptable use of compliance data and the potential and rationale for ‘gaming’ the system. Finally, consideration need to be given to the suitability of systems within the current hospital environment. Curtain separated bed spaces allow practitioners to approach patients from all angles which means sensor placement in shared bed spaces will be not possible or not accurate.
Conclusion
HH prompt and monitoring systems appear to improve compliance but improvements are not sustained when systems are removed. Their mode of impact appears to be multifaceted in terms of prompting, enhancing empathy with patients and increasing awareness of the need for HH during the period of installation. However, systems are unable to recognise context and therefore prompt when HH is unnecessary. This may lead to practitioner irritation and gaming potentially undermining the positive impact of such systems.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, Robertson N. (2010) Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 3: CD005470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonetti D, Eccles M, Johnson M, Steen N, Grimshaw JM, Baker R, Walker A, Pitts N. (2005) Guiding the design and selection of interventions to influence the implementation of evidence based practice: an experimental simulation of a complex intervention trial. Social Science and Medicine 60: 2135–2147. [DOI] [PubMed] [Google Scholar]
- Boscart VM, McGilton KS, Levchenko A, Hufton G, Holliday P, Fernie GR. (2008) Acceptability of a wearable hand hygiene device with monitoring capabilities. Journal of Hospital Infection 70: 216–222. [DOI] [PubMed] [Google Scholar]
- Braun V, Clarke V. (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3(2): 77–101. [Google Scholar]
- Davies P, Walker AE, Grimshaw JM. (2010) A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implementation Science 5: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson CH, Mackrill JB. (2014) Review of technologies available to improve hand hygiene compliance–are they fit for purpose? Journal of Infection Prevention 15:222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmond MB, Goodell A, Zuelzer W, Sanogo K, Elam K, Bearman G. (2010) Successful use of alcohol sensor technology to monitor and report hand hygiene compliance. Journal of Hospital Infection 76: 364–365. [DOI] [PubMed] [Google Scholar]
- Ellingson K, Polgreen PM, Schneider A, Shinkunas L, Kaldjian LC, Wright D, Thomas GW, Segre AM, Herman T, McDonald LC, Sinkowitz-Cochran R. (2011) Healthcare personnel perceptions of hand hygiene monitoring technology. Infection Control & Hospital Epidemiology 32: 1091–1096. [DOI] [PubMed] [Google Scholar]
- Fuller C, Michie S, Savage J, McAteer J, Besser S, Charlett A, Hayward A, Cookson BD, Cooper BS, Duckworth G, Jeanes A. (2012. _ The Feedback Intervention Trial (FIT)—improving hand-hygiene compliance in UK healthcare workers: a stepped wedge cluster randomised controlled trial. PLoS One 7: e41617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimshaw J, Thomas R, MacLennan G, Fraser CRRC, Ramsay CR, Vale LEEA, Whitty P, Eccles MP, Matowe L, Shirran L, Wensing MJP. (2004) Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technology Assessment 8: iii–iv, 1–72. [DOI] [PubMed] [Google Scholar]
- Grol R. (2005) Implementation of changes in practice. In: Grol R, Wensing M, Eccles M. (eds) Improving Patient Care: The Implementation of Change in Clinical Practice. London: Elsevier Butterworth Heinemann. [Google Scholar]
- Huis A, van Achterberg T, de Bruin M, Grol R, Schoonhoven L, Hulscher M. (2012) A systematic review of hand hygiene improvement strategies: a behavioural approach. Implementation Science 7: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohli E, Ptak J, Smith R, Taylor E, Talbot EA, Kirkland KB. (2009) Variability in the Hawthorne effect with regard to hand hygiene performance in high- and low-performing inpatient care units. Infection Control and Hospital Epidemiology 30: 222–225. [DOI] [PubMed] [Google Scholar]
- Kovacs-Litman A, Wong K, Shojania KG, Callery S, Vearncombe M, Leis JA. (2016) Do physicians clean their hands? Insights from a covert observational study. Journal of Hospital Medicine 11: 862–864. [DOI] [PubMed] [Google Scholar]
- Levchenko AI, Boscart VM, Fernie GR. (2011) The feasibility of an automated monitoring system to improve nurses’ hand hygiene. International Journal of Medical Informatics 80: 596–603. [DOI] [PubMed] [Google Scholar]
- Marra AR, Camargo TZS, Magnus TP, Blaya RP, dos Santos GB, Guastelli LR, Rodrigues RD, Prado M, da Silva Victor E, Bogossian H, Monte JCM. (2014) The use of real-time feedback via wireless technology to improve hand hygiene compliance. American Journal of Infection Control 42: 608–611. [DOI] [PubMed] [Google Scholar]
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. (2005) Making psychological theory useful for implementing evidence based practice: a consensus approach. Quality and Safety in Health Care 14: 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. (1994) Qualitative data analysis: A sourcebook. Beverly Hills, CA: Sage Publications. [Google Scholar]
- Pittet D, Allegranzi B, Boyce J. and World Health Organization World Alliance for Patient Safety First Global Patient Safety Challenge Core Group of Experts. (2009) The World Health Organization guidelines on hand hygiene in health care and their consensus recommendations. Infection Control and Hospital Epidemiology 30: 611–622. [DOI] [PubMed] [Google Scholar]
- Pittet D, Panesar SS, Wilson K, Longtin Y, Morris T, Allan V, Storr J, Cleary K, Donaldson L. (2011) Involving the patient to ask about hospital hand hygiene: a National Patient Safety Agency feasibility study. Journal of Hospital Infection 77: 299–303. [DOI] [PubMed] [Google Scholar]
- Sahud AG, Bhanot N, Narasimhan S, Malka ES. (2012) Feasibility and effectiveness of an electronic hand hygiene feedback device targeted to improve rates of hand hygiene. Journal of Hospital Infection 82: 271–273. [DOI] [PubMed] [Google Scholar]
- Sharma D, Thomas GW, Foster ED, Iacovelli J, Lea KM, Streit JA, Polgreen PM. (2012) The precision of human-generated hand-hygiene observations: a comparison of human observation with an automated monitoring system. Infection Control & Hospital Epidemiology 33: 1259–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srigley JA, Gardam M, Fernie G, Lightfoot D, Lebovic G, Muller MP. (2015) Hand hygiene monitoring technology: a systematic review of efficacy. Journal of Hospital Infection 89: 51–60. [DOI] [PubMed] [Google Scholar]
- Swoboda SM, Earsing K, Strauss K, Lane S, Lipsett PA. (2004) Electronic monitoring and voice prompts improve hand hygiene and decrease nosocomial infections in an intermediate care unit. Critical Care Medicine 32: 358–363. [DOI] [PubMed] [Google Scholar]
- Venkatesh AK, Lankford MG, Rooney DM, Blachford T, Watts CM, Noskin GA. (2008) Use of electronic alerts to enhance hand hygiene compliance and decrease transmission of vancomycin-resistant Enterococcus in a hematology unit. American Journal of Infection Control 36: 199–205. [DOI] [PubMed] [Google Scholar]
- Vicente K. (2006) The human factor: Revolutionizing the way people live with technology. Abingdon, Oxon, UK: Routledge. [Google Scholar]
- Ward MA, Schweizer ML, Polgreen PM, Gupta K, Reisinger HS, Perencevich EN. (2014) Automated and electronically assisted hand hygiene monitoring systems: a systematic review. American Journal of Infection Control 42: 472–478. [DOI] [PubMed] [Google Scholar]