Abstract
Aim:
In this study, we aimed to assess the level of good glycemic control, to determine association between adherence to antidiabetic medications and glycosylated hemoglobin (HbA1c) and to examine factors influencing good glycemic control.
Materials and methods:
A cross-sectional design was employed among 369 patients with type 2 diabetes mellitus (T2DM) from four Ministry of Health health centers in 2016. A sample of 3 ml blood was taken to measure the HbA1c, and patients were asked to fill out a pretested questionnaire. Univariate and multivariate logistic regressions, to identify independent factors associated with good glycemic control, were conducted using SPSS software version 22 (IBM Corp, Armonk, NY, USA).
Results:
Mean [±standard deviation (SD)] of HbA1c was 8.97 (2.02) and one fifth of patients had good glycemic control (HbA1c ⩽ 7%). Factors associated with good glycemic control were: older age [odds ratio (OR) = 0.96, 95% confidence interval (CI): 0.933–0.988), high medication adherence (OR: 2.757, 95% CI: 1.308–4.693), and better health literacy (OR= 2.124, 95% CI: 1.917–4.921). Duration of diabetes mellitus (DM > 7 years) was inversely related to good glycemic control (OR = 2.255, 95% CI: 1.189–4.276).
Conclusion:
Our study showed that glycemic control was suboptimal, and factors associated with that were: older age, high medication adherence, and better health literacy. Knowledge of these factors could be an entry toward helping patients and targeting interventions to improve glycemic control and prevent diabetes-related complications.
Keywords: Gaza Strip, glycemic control, HbA1c, medication adherence, type 2 diabetes mellitus
Introduction
Diabetes mellitus (DM) is a rapidly growing public health problem that affects millions of people worldwide, leading to disastrous consequences. DM is responsible for three quarters of morbidity and 88% of mortality, mostly in developing countries.1,2 In Palestine, the prevalence of DM reached 9% of the general population in which type 2 DM (T2DM) is the most prevalent type (>87% of cases).3 Routine data gathered by the United Nations for Relief and Working Agency (UNRWA) showed the prevalence as 10.5% and 11.8% among registered Palestinian refugees in the West Bank and Gaza Strip, respectively.4 It is projected to reach 20.8% and 23.4% in 2020 and 2030, respectively.5
The Palestinian healthcare system had shown a significant improvement after the Oslo agreement and establishment of the Palestinian National Authority. However, the continuous threat posed by the political situation, the blockade around the Gaza Strip, which has been in place since 2006, and the political divide between the West Bank and the Gaza Strip posed challenges to unity of the Palestinian healthcare system by altering the health services delivered to the Gazan population. The Palestinian healthcare system is mainly a public health system and services are offered by many providers. The Ministry of Health (MoH) is the main player that provides both primary, secondary and some tertiary health services and is the stewardship body for health improvement. The United Nations for Relief and Working Agency (UNRWA) is the second largest provider of healthcare and offers free of charge, preventive, primary and community health services to registered Palestinian refugees in the eight refugee camps that represent 67.5% of the Gazan population. Nongovernmental organizations in the Gaza Strip provide almost the same range of MoH primary healthcare services, except immunization.
Diabetes management and follow up is provided in the primary health centers (PHCs). The PHCs belong to MoH and are divided into four levels, based on the capacity building of PHCs. The level IV PHC provides extensive lab services, X-ray services, dental care and consultation from specialized physicians.
Diabetes control is not restricted to taking medications. It comprises practices and a comprehensive management approach to prevent or delay possible complications.6 These practices are: self-monitoring of blood glucose, dietary management, ophthalmic follow up, foot care and biochemical monitoring of renal function tests.7 Poor glycemic control is significantly associated with clinical complications,8 and is triggered by factors including, but not limited to, age, dietary habits, exercise behavior, body mass index (BMI), duration of DM, adherence to prescribed medications and knowledge of the glycosylated hemoglobin (HbA1c) target.9
Many old studies have shown the strong correlation between good glycemic control and reduction in the risk of T2DM-related complications,10,11 in which 1% reduction in the HbA1c results in a 35% reduction in the risk of microvascular complications and 25% reduction in diabetes-related mortality.11 Optimal HbA1c control is suggested to be <7%12 or <6.5%.13 Despite this fact, the majority of patients with DM still have poor glycemic control14,15 and several international studies were conducted to identify the influencing factors.16–20 These factors are not alike, from one population to another due to cultural, educational, religious and economic variations. High adherence to prescribed medications was significantly a strong predictor for good glycemic control.21–26 Moreover, duration of DM showed a significant association with better HbA1c status.24,27,28 Age and sex have demonstrated contradicting associations. Age < 65 years was an important factor for good glycemic control,29 whereas it was not, in other studies.24,25,28 Female sex was shown to be a predictor for a good glycemic control,28 while Kautzky-Willer and colleagues,30 and Kamuhabwa and Charles25 found men have significantly greater HbA1c reduction than women. Other influencing factors are family support, good physician–patient relationship,15,26 knowledge about diabetes,31 educational level21 and mono- or multitherapy.21,25
Adherence to antidiabetes therapies is a key element in the quality of diabetes management. It is often suboptimal,32 but remains vague regarding prediction of glycemic control among T2DM.33 Previous studies supported the relationship between adherence to antidiabetes medications and HbA1c level.34,35 In contrast, finding from Blonde and colleagues36 did not support this association.
Studies on glycemic control and its association with medication adherence among T2DM in Palestine are lacking. Therefore, we conducted this study among primary care patients with T2DM in the Gaza Strip to: (a) assess the level of good glycemic control; (b) determine the association between adherence to diabetes medications and HbA1c; and (c) examine factors influencing good glycemic control.
Materials and methods
Study design
This was a cross-sectional design employed among T2DM patients seeking care in the PHCs.
Ethical consideration
This study was approved by the Palestinian Ethical Committee (No: PHRC/HC/118/16). Permission was also obtained from the Palestinian MoH for conducting the study in its PHCs. A consent form was signed by the patients and providing a confirmation that the study is voluntary based, and rights are preserved if withdrawals occur. The consent form also contained a statement of agreement by the patients themselves to collect a 3 ml sample of blood for establishing HbA1c status. The study was conducted from October to December 2016.
Study setting, sample and sampling
Patients with T2DM who had the willingness to be involved in the study, give patient-signed informed consent, were under antidiabetes treatment ⩾ 6 months, aged ⩾ 26 years and were on regular follow up for at least three visits were eligible for the study. Patients with mental diseases, pregnant women and gestational diabetes were excluded. Nine level IV PHCs belonging to MoH, serve 6486 T2DM patients, are distributed across four Gaza Strip governorates. One PHC had been randomly selected (cluster sample) to ensure equal representativeness of the sample. They were the Jabalia Health Center, Al Rimal Health Center, Dier Al Balah Health Center and Khan Younis Health Center located in the north, Gaza, middle zone and south governorate, respectively.
We used the traditional formula to calculate the sample size: n = [(Z – a/2)2 p(1 – p)/d2], in which p = 10%,5 d = margin error 5%. The sample size was 338 plus 10% nonresponse rate, giving a total sample size equal to 371. A proportionate systematic sampling was followed to select T2DM patients and the kth interval was 17.
Measures
Data were collected by three health professionals who received one-day training on understanding questionnaire content, verbal communication and facial expressions. At the end of the training day, data collectors provided an actual demonstration of data collection using a face-to-face interviewed approach. A pilot study was performed among an eligible group of 15 T2DM patients in the Al Rimal Health Center. Internal consistency of the whole questionnaire measured with Cronbach’s alpha coefficient was >0.83.
Medication adherence: Adherence to medications was measured using the self-report Morisky Medication Adherence Scale (MMAS-4). It comprises four questions measured with answers ‘Yes’ or ‘No’ and the score is ranged from 0 to 4. Because questions are negatively worded, a score of 4 reflects poor adherence and a score of 0 reflects a high adherence. This tool has shown a strongly predictive and concurrent validity, and internal consistency.37 The questionnaire was translated into Arabic and internal consistency was examined through Cronbach’s coefficient alpha, which equalled 0.76.
Health literacy: We used the Brief Health Literacy Screening Tool (BRIEF)38 which has four questions and are measured on a five-point Likert scale (1 = never to 5 = always). Answers were collapsed into two choices: Yes (scores 4 and 5) and No (scores 1, 2 and 3). The internal consistency of the Arabic BRIEF, measured by Cronbach’s coefficient alpha, was 0.71.
Laboratory measure: Glycemic control was examined through determination of HbA1c using the Bio-Rad D-10 (United States, Bio-Rad Laboratories, Inc., Hercules, CA 94547 FRANCE, Bio-Rad, Marnes-la-Coquett) [high-performance liquid chromatography (HPLC) instrument]. The HbA1c is an accurate marker of glycemic control over a preceding 3-month period. The HPLC instrument complies with latest Diabetes Control and Complications Trial (DCCT) according to the National Glycohemoglobin Standardization Program (NGSP).39 HbA1c > 7% represents poor glycemic control.12 A 3 ml venous blood sample was taken from patients, by a trained nurse, and put in ethylenediaminetetraacetic acid (EDTA)-filled tubes of 5 ml size (EDTA blood was used for HbA1c determination). The samples were immediately transferred to one laboratory and analysis was performed on the same day, not exceeding 24 h. Quality control and calibration were performed every day before started the analysis.
Baseline characteristics: Socio-demographic (age, sex, marital status) and clinical characteristics of participants (duration of having DM, complications, HbA1c values) were included in the beginning of questionnaire.
Data analysis
During the data entry phase, data were checked for errors and outliers. Descriptive analysis was used, with means (standard deviations) and frequencies (percentages) for continuous and categorical variables, respectively. Bivariate analysis of independent variables with glycemic control (good versus poor) was applied and the crude odds ratio (OR) [95% confidence interval (CI)] was used to determine the association between independent variables and the dependent variable (glycemic control). Independent variables with p value ⩽ 0.25 were selected for multiple logistic regression to determine independent factors associated with good glycemic control. Analyses were conducted using the Statistical Package for Social Sciences (IBM Corp, Armonk, NY, USA) version 22.
Results
Patients’ baseline and clinical characteristics are shown in Table 1. Mean [± standard deviation (SD)] age and mean (±SD) duration of DM was 56.38 (10.36) and 10.48 (8.12), respectively. A total of 55.8% (206) were females and 13% (48) had previous history of hospitalization due to DM. One third (126) were aged more than 61 years and 97 (26.3%) were under 50 years, and more than half (54.3%) had DM for 7 years and more. A total of 200 (54.2%) reported having complications including hypertension (13.6%), diabetic nephropathy (36%), diabetic retinopathy (3.5%), and cardiac problems (7.6%).
Table 1.
Socio-demographic and clinical characteristics of patients.
| Variables | Total (n = 369) |
North PHC (n = 109) |
Gaza PHC (n = 108) |
Middle PHC (n = 65) |
South PHC (n = 87) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| M (SD) | n (%) | M (SD) | n (%) | M (SD) | n (%) | M (SD) | n (%) | M (SD) | n (%) | |
| Sex | ||||||||||
| Male | 163 (44.2) | 46 (42.2) | 45 (41.7) | 29 (44.6) | 40 (46) | |||||
| Female | 206 (55.8) | 63 (57.8) | 63 (58.3) | 36 (55.4) | 47 (54) | |||||
| Marital status | ||||||||||
| Single | 28 (7.3) | 11 (10) | 11 (10.2) | 5 (7.6) | 1 (1.1) | |||||
| Married | 341 (92.7) | 98 (89.9) | 97 (89.8) | 60 (92.3) | 86 (98.9) | |||||
| Hospital admission | ||||||||||
| Yes | 48 (13) | 4 (3.7) | 9 (8.3) | 12 (18.5) | 23 (26.4) | |||||
| No | 321 (87) | 105 (96.3) | 99 (91.7) | 53 (81.5) | 64 (73.6) | |||||
| Age | 56.38 (10.36) | 56.07 (8.96) | 57.32 (11.67) | 54.66 (11.07) | 56.9 (9.69) | |||||
| ⩽50 | 42.96 (6.21) | 97 (26.3) | 44.5 (5.5) | 27 (24.8) | 41.6 (7.5) | 29 (26.9) | 40.9 (8.9) | 19 (29.2) | 42.2 (7.1) | 22 (25.3) |
| 51–60 | 56.07 (2.92) | 146 (39.6) | 56.1 (3.0) | 52 (47.7) | 55.5 (2.8) | 33 (30.6) | 56.3 (3.1) | 28 (43.1) | 56.5 (2.7) | 33 (37.9) |
| ⩾61 | 67.07 (4.61) | 126 (34.1) | 66.5 (4.2) | 30 ( 27.5) | 68.1 (5.5) | 46 (42.6) | 66.4 (4.1) | 18 (27.7) | 66.5 (3.6) | 32 (36.8) |
| Duration of having DM | 10.48 (8.12) | 8.51 (6.95) | 12.24 (8.85) | 10.07 (7.75) | 11.09 (8.37) | |||||
| ⩽7 years | 3.8 (2.0) | 169 (45.8) | 3.8 (2.1) | 63 (57.8) | 4.1 (1.9)17. | 40 (37.0) | 3.7 (1.7) | 31 (47.7) | 3.3 (2.0) | 35 (40.2) |
| >7 years | 16.2 (6.9) | 200 (54.2) | 15.0 (6.0) | 46 (42.2) | 0 (7.8) | 68 (63.0) | 15.9 (6.5) | 34 (52.3) | 16.3 (6.8) | 52 (59.8) |
| Consultation time | 7.09 (3.46) | 6.50 (2.71) | 7.40 (3.87) | 8.61 (3.12) | 6.33 (3.67) | |||||
| ⩽5 min | 4.83 (0.7) | 233 (63.1) | 4.9 (0.3) | 78 (71.6) | 4.5 (1.2) | 60 (55.6) | 5 (0) | 24 (36.9) | 4.9 (0.5) | 71 (81.6) |
| >5 min | 11.09 (2.7) | 132 (35.8) | 10.5 (1.9) | 31 (28.4) | 11.4 (2.5) | 44 (40.7) | 10.7 (1.8) | 41 (63.1) | 12.5 (5.2) | 16 (18.4) |
| Doctor consultation | ||||||||||
| Yes | 365 (98.9) | 109 (100) | 105 (97.2) | 65 (100) | 86 (98.9) | |||||
| No | 2 (0.5) | – | 1 (.9) | – | 1 (1.1) | |||||
| Previous complications | 200 (54.2) | 61 (56) | 52 (48.1) | 37 (56.9) | 50 (57.5) | |||||
| Hypertension | 50 (13.6) | 28 (25.7) | 1 (0.9) | 14 (21.5) | 7 (8) | |||||
| Retinopathy | 133 (36.0) | 38 (34.9) | 43 (39.8) | 21 (32.3) | 31 (35.6) | |||||
| Nephropathy | 13 (3.5) | 1 (0.9) | 6 (5.6) | 0 (0) | 4 (4.6) | |||||
| Cardiac | 28 (7.6) | 11 (10.1) | 3 (2.8) | 3 (4.6) | 11 (12.6) | |||||
| Nothing | 169 (45.8) | 48 (44) | 56 (51.9) | 28 (43.1) | 37 (42.5) | |||||
| Medications | ||||||||||
| Tablets | 241 (65.3) | 75 (68.8) | 64 (59.3) | 42 (64.6) | 60 (69) | |||||
| Insulin | 85 (23) | 19 (17.4) | 32 (29.6) | 12 (18.5) | 22 (25.3) | |||||
| Both | 43 (11.7) | 15 (13.8) | 12 (11.1) | 11 (16.9) | 5 (5.6) | |||||
| HbA1c | ||||||||||
| ⩽7% | 6.3 (0.5) | 72 (19.5) | 6.2 (0.5) | 19 (17.4) | 6.4 (0.5) | 22 (20.4) | 6.2 (0.6) | 14 (21.5) | 6.2 (0.5) | 17 (19.5) |
| >7.1% | 9.6 (2.0) | 297 (80.5) | 9.7 (1.5) | 90 (82.6) | 9.4 (1.7) | 86 (79.6) | 9.4 (1.7) | 51 (78.5) | 10.0 (1.8) | 70 (80.5) |
M, mean; SD, standard deviation; PHC, primary health centers; DM, diabetes mellitus; HbA1c, glycosylated hemoglobin.
Glycosylated hemoglobin
Mean (±SD) of HbA1c was 8.97 (2.02) and 19.5% had HbA1c ⩽7%. HbA1c values are shown in Figure 1. Unadjusted mean HbA1c for patients with MMAS-4 scores of 0, 1, 2, and 3 are shown in Figure 2. The more that patients adhere to medications (MMAS-4 = 0), the lower the mean HbA1c compared with another group with an MMAS-4 score of 1, 2 or 3, but the mean HbA1c remained above average (mean ± SD of HbA1c for MMAS-4 score 0 was 8.8 ± 2.0). Mean HbA1c (±SD) for patients receiving Oral Hypoglycemic Agents (OHA), insulin, and on both regimens, was 8.8 (2.1), 9.4 (1.8), and 9.1 (1.7), respectively. Statistical significance was shown between DM patients with and without previous medical complications (p < 0.05).
Figure 1.
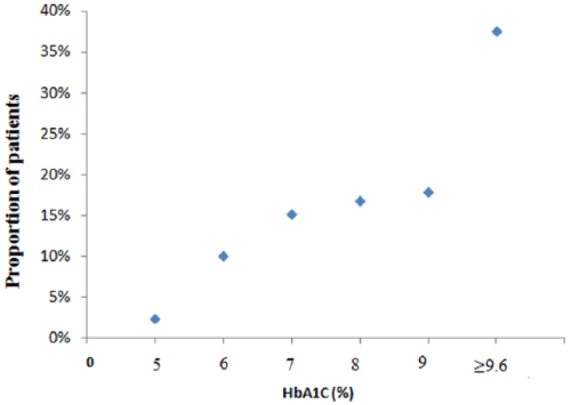
Distribution of glycosylated hemoglobin values.
HbA1c, glycosylated hemoglobin.
Figure 2.
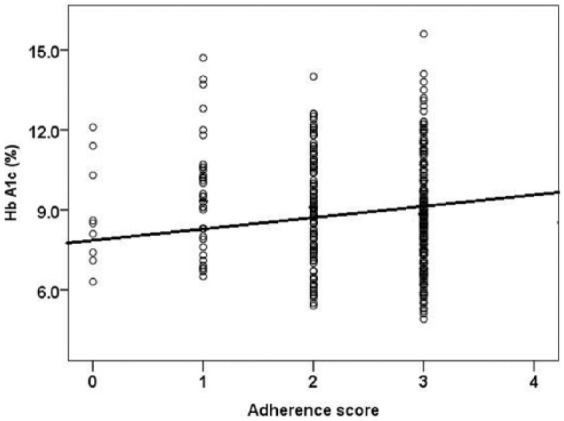
Relationship between adherence to medications and glycosylated hemoglobin (Morisky Medication Adherence Scale score = 4 means higher adherence).
HbA1c, glycosylated hemoglobin; MMAS-4, Morisky Medication Adherence Scale.
Adherence to medications
Out of the 369 participants, 58% (214) reported having high adherence (MMAS-4 = 0), 39.6% (146) and 2.4% (9) reported to have medium and low adherence, respectively (MMAS-4 = 1–2 and ⩾3, respectively). Correlation between HbA1c and MMAS-4 was moderately positive (r = 0.496, p < 0.05).
Bivariate associations
Patients were divided into two groups: good glycemic control (⩽7%) and poor glycemic control (>7%). Using the univariate analysis of independent variables, six independent factors were chosen for logistic regression (p ⩽ 0.25): age (OR = 0.97, 95% CI: 0.945–0.995), female sex (OR = 1.538, 95% CI: 0.917–2.579), duration of DM (OR = 1.874, 95% CI: 1.112–3.158), types of medication (OR = 2.676, 95% CI: 1.262–5.674), better health literacy (OR = 1.681, 95% CI: 0.771–3.666), and high adherence score (OR = 2.313, 95% CI: 0.282–4.557) (Table 2).
Table 2.
Univariate analysis of factors associated with good glycemic control.
| Variable | Total n = 369 |
Good control n = 72 |
Poor control n = 297 |
Odds ratio with 95% CI |
p value |
|---|---|---|---|---|---|
| Age | M ± SD 56.38 (10.36) |
M ± SD 58.9 ± 10.6 |
M ± SD 55.5 ± 11.0 |
0.97 (0.945–0.995) | <0.05 |
| Sex | |||||
| Male | 163 (44.2) | 38 (52.8) | 125 (42.1) | Reference | |
| Female | 206 (55.8) | 34 (47.2) | 172 (57.9) | 1.538 (0.917–2.579) | 0.103 |
| Marital status | |||||
| Single | 28 (7.3) | 12 (16.6) | 16 (5.4) | 0.537 (0.12–2.404) | 0.416 |
| Married | 341 (92.7) | 60 (83.3) | 281 (94.6) | ||
| Duration of DM | |||||
| ⩽7 years | 169 (45.8) | 42 (58.3) | 127 (42.8) | Reference | |
| >7 years | 200 (54.2) | 30 (41.7) | 170 (57.2) | 1.874 (1.112–3.158) | <0.05 |
| Complications | |||||
| No | 169 (45.8) | 33 (45.8) | 136 (45.8) | Reference | |
| Yes | 200 (54.2) | 39 (54.2) | 161 (54.2) | 1.002 (0.597–1.679) | 0.995 |
| Type of medication | |||||
| Oral | 241 (65.3) | 58 (80.6) | 183 (61.6) | Reference | <0.05 |
| Insulin | 85 (23) | 9 (12.5) | 76 (25.6) | 2.676 (1.262–5.674) | <0.05 |
| Both | 43 (11.7) | 5 (6.9) | 38 (12.8) | 2.409 (0.906–6.406) | 0.078 |
| Previous hospitalization | |||||
| No | 321 (87) | 65 (90.3) | 256 (86.2) | Reference | |
| Yes | 48 (13) | 7 (9.7) | 41 (13.8) | 0.672 (0.288–1.568) | 0.358 |
| Health literacy | |||||
| Yes | 353 (95.7) | 67 (93.1) | 286 (96.3) | 1.9 (0.7–5.8) | 0.183 |
| No | 16 (4.3) | 5 (6.9) | 11 (3.7) | Reference | |
| Morisky score | |||||
| 0 | 214 (58) | 48 (66.7) | 166 (55.9) | 2.313 (0.282–4.557) | 0.120 |
| 1–2 | 146 (39.6) | 23 (31.9) | 123 (41.4) | 1.546 (0.893–2.678) | 0.235 |
| 3–4 | 9 (2.4) | 1 (1.4) | 8 (2.7) | Reference | 0.242 |
M, mean; SD, standard deviation; DM, diabetes mellitus; CI, confidence interval.
Independent factors influencing glycemic control
Multivariate logistic analysis showed age, duration of DM, high adherence and better health literacy were significantly associated with good glycemic control (Table 3). The longer the patient lives with the disease, the less likely the glycemic status is controlled (OR = 2.255, 95% CI: 1.189–4.276). However, the more the patients are literate and knowledgeable about DM, the older they are, and adherent to their medications, the more likely their glycemic status is well controlled [(OR = 2.124, 95% CI: 1.917–4.921), (OR = 0.96, 95% CI: 0.933–0.988) and (OR: 2.757, 95% CI: 1.308–4.693)], respectively.
Table 3.
Multivariate analysis of factors associated with good glycemic control.
| Variable | B | SE | Wald | p value | Odds ratio with 95% CI |
|---|---|---|---|---|---|
| Constant | 2.046 | 0.943 | 4.703 | <0.05 | |
| Age | 0.041 | 0.015 | 7.745 | <0.05 | 0.96 (0.933–0.988) |
| Sex | 0.481 | 0.279 | 2.959 | 0.085 | 1.617 (0.935–2.797) |
| Duration of DM | −0.813 | 0.327 | 6.200 | <0.05 | 2.255 (1.189–4.276) |
| Medication | |||||
| Oral | 3.346 | 0.188 | Reference | ||
| Insulin | −0.667 | 0.422 | 2.496 | 0.114 | 1.948 (0.852–4.457) |
| Both | −0.643 | 0.528 | 1.480 | 0.224 | 1.901 (0.675–5.354) |
| Health literacy | 0.753 | 0.429 | 3.091 | < 0.05 | 2.124 (1.917–4.921) |
| Morisky score | |||||
| (3–4) | 3.767 | 0.096 | Reference | ||
| (1–2) | 0.489 | 0.294 | 0.822 | 0.365 | 0.917 (0.917–2.9) |
| (0) | 1.014 | 1.119 | 3.274 | < 0.05 | 2.757 (1.308–4.693) |
B, regression coefficient; SE, standard error; CI, confidence interval; DM, diabetes mellitus.
Discussion
The ultimate outcome of diabetes management is to achieve glycemic control and to prevent or delay complications related to diabetes. In this study, we assessed the glycemic status, determined by HbA1c, and factors associated with good glycemic control among patients with T2DM. Almost one fifth of patients were shown to have good glycemic control, which is consistent with previous reported studies from Africa,21,25 Australia,30 Asia,33 America18,26 and Arab countries.15,28 However, this prevalence is far lower than findings of Ali and colleagues,40 who reported 86.1%. The variations could be attributed to the presence or absence of a collection of practices that are necessary for the management of diabetes and are not only restricted to medications. The practices include self-management of diabetes, exercise behavior, dietary habits, knowledge, and awareness about the disease, uniform guidelines and not lastly, adherence to antidiabetes regimens.41
High adherence to antidiabetic medications was suboptimal (58%), which was previously documented among T2DM from Ethiopia,21 America,23,31 Tanzania,25 India42 and Palestine.43
The Morisky score was associated with HbA1c values. The more adherence to antidiabetic therapies, the better the HbA1c values, but the mean HbA1c value was above 7%, similar to findings of Al-Halaweh and colleagues.44 Reasons for poor glycemic control are difficult to identify. They could be attributed to lack of comprehensiveness of diabetes management which comprises a set of practices including, but not limited to, continuous glucose monitoring, dietary habits, physical exercise and awareness about DM, and also could be due to the disease process itself, as well as attitudes of physicians and patients. Patients themselves used to shop among endocrinologists and received different protocols for diabetes management. Moreover, the poverty status imposed by the current strict siege and bad economic status push this vulnerable group to prioritize medicines as a second choice after maintaining family life. Treatments are sometimes not available in PHCs after the middle of the month, so patients do not take the treatments unless purchased from pharmacies. Recent studies from Gaza revealed that adherence, of physicians and nurses in the PHCs, to Palestinian clinical practice guideline for DM is suboptimal (51.5%),45 and physicians and nurses perceive less trust-worth toward the guideline because of its poor quality compared with other international guidelines.46 So, glycemic control is not just by taking medications. High adherence (MMAS-4 score = 0) was significantly associated with 10% reduction in the HbA1c value, which is in line with findings of Krapek and his colleagues.23 This finding has practical and clinical implications in terms of preventing early microvascular complications associated with T2DM and therefore reduces healthcare-related costs. A previous study revealed that 1% reduction in HbA1c resulted in 35% reduction in the risk of complications from T2DM.11 In this study, 3.5% of patients reported having diabetic retinopathy, while we believe in reality, it is much higher because the estimation was based on self-report method. Microvascular complications of T2DM among Palestinians in the West Bank were 25.9%.44 We recommend further studies to determine the prevalence of diabetic complications among T2DM patients. Several studies showed no association between adherence and HbA1c. The prospective study conducted by Wooldridge and colleagues47 among 189 patients showed improvement in the metabolic control of intensive individual education, but no association was documented with self-reported adherence to antidiabetes medications. The MMAS-4 does not consider other factors influencing the metabolic control, including lifestyle factors (dietary habits and exercise), but it provides a meaningful information on use of drugs, which is a significant factor in diabetes management.
An inverse relationship was observed between age and HbA1c (p = 0.05); the higher the age, the more likely the HbA1c is controlled, similar to other studies.28,48 This could be attributed to ‘development effect’, in which glycemic control improves as cohorts mature by age. In fact, this is in contrast to a former concept that the glycemic control (HbA1c level) worsens with time. Other studies opposed our findings.25,49 The variation of the relationship between poor glycemic control and age could be due to dissimilarities of the studied population and age distribution in various studies. We recommend a prospective and a longitudinal study to explore the real relationship between age and glycemic control that gives clearer insight than the current cross-sectional study.
Poor glycemic control was significantly associated with duration of DM. This is congruent with other reported studies.18,20 A possible explanation, as given by Sampson and colleagues,50 is that the amount of carbohydrate attached to the HbA1c increases with increasing duration of DM. Also, DM is known as a progressive disease and insulin resistance increases with time due to progressive impairment of insulin secretion from beta cells.11
Health literacy is used to measure patients’ ability to comprehend, read and act on instructions given in the healthcare center. So, patients are able to understand elementary health information that helps them for a better decision on their health. Better health literacy was significantly associated with good glycemic control. This is consistent with findings obtained from Cavanaugh and colleagues.51 Successful glycemic control requires patients to know how to monitor and manage symptoms, carry out medical treatments on a daily basis, and self-monitoring of disease progression. Therefore, inadequate health literacy hampers these practices, leading to improper diabetes management and early occurrence of complications, including, but not limited to, kidney disease and neurological disorders.52
Females are more likely to have better glycemic control than males. Although this estimate did not reach statistical significance, it was in line with the Kautzky-Wille study,53 however, against the finding by Kamuhabwa and Charles25 that revealed women failed to achieve the targeted HbA1c in comparison with male counterparts. HbA1c differences in sex could not be explained by dissimilarities in body composition and therefore, there is a need for further investigation to examine sex-related distinction in efficacy/treatment response.
This study was strengthened by the tremendous response rate; therefore, generalization could possibly be applied to all T2DM patients seeking care in the PHCs. It also has some noteworthy limitations. First, there are other factors influencing glycemic control that were not examined in this study. These factors are dietary habits, physical activity index, patient education, and dieticians’ instructions. Second, adherence was measured by a self-report method and that was based on patients’ recall of their habits and medication-taking practices, and overestimation could occur. The direct method, counting pills, is a better way to estimate adherence to medications, but unfortunately, we couldn’t use it due to dual benefit of DM patients from MoH and UNRWA health services. Third, the nature of a cross-sectional design does not prove the causality.
Conclusion
Findings of this study indicate that diabetes management and glycemic control is a formidable challenge to the Palestinian healthcare system. The majority of participating patients in the Gaza Strip had poor glycemic control; and short duration of the disease, better health literacy, old age and high adherence to medications were significantly associated with the good glycemic control. Knowledge of these factors could be a start toward helping patients and targeting interventions to improve glycemic control and prevent diabetes-related complications. Poor glycemic control in Palestine indicates a need for more research and improvement, and highlights the need to review the existing guidelines and develop an awareness program around issues related to diabetes care.
Acknowledgments
This publication was made possible by award no: BMZ-2014.1819.3, from the Palestinian Medical Relief Society (strengthening resilience in healthcare and patients with noncommunicable diseases in the Gaza strip). We are grateful to head nurses of the selected PHCs who had supported and facilitated this work. Dr Aymen Elsous is the guarantor and has full access to all the data, and takes responsibility for the integrity and the accuracy of the data analysis.
Footnotes
Author contributions: AE and MR contributed to the design and concept of the study. AA was responsible for data analysis and data interpretation. HS wrote the first draft of the manuscript. AE, MR, AA and SH critically revised the manuscript and revision was done. All authors approved the final manuscript.
Funding: Palestinian Medical Relief Society (BMZ-2014.1819.3)
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Mahmoud Radwan, Department of Health Management and Economics, School of Public Health, Tehran University of Medical Sciences - International campus, Tehran, Iran Islamic Republic; and International Cooperation Department, Ministry of Health, Gaza Strip, Palestinian Territory, Occupied.
Aymen Elsous, Assistant Professor, Faculty of Health Sciences, Israa University, Gaza Strip, Palestinian Territory, Occupied; and Quality Improvement and Infection Control, Shifa Medical Complex, Gaza Strip, Palestinian Territory, Occupied.
Hasnaa Al-Sharif, Department of Chronic Diseases, Directorate of Primary Healthcare, Ministry of Health, Gaza Strip, Palestinian Territory, Occupied.
Ayman Abu Mustafa, Palestine College of Nursing, Ministry of Health, Gaza Strip, Palestinian Territory, Occupied.
References
- 1. International Diabetes Federation. Diabetes atlas. 7th ed. International Diabetes Federation. http://www.diabetesatlas.org/ (2015, accessed 2 June 2017).
- 2. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3: e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ministry of Health. Health status in Palestine. Palestine, Gaza: Ministry of Health, 2006. [Google Scholar]
- 4. United Nations for Relief and Working Agency UNRWA. Annual report of the Department of Health. Amman: United Nations for Relief and Works Agency, 2007. [Google Scholar]
- 5. Abu-Rmeileh NME, Husseini A, O’Flaherty M, et al. Forecasting prevalence of type 2 diabetes mellitus in Palestinians to 2030: validation of a predictive model. Lancet 2012; 380: S21. [Google Scholar]
- 6. Ryden L, Standl E, Bartnik M, et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The task force on diabetes and cardiovascular diseases of the European Society of Cardiology (ESC) and European Association for the Study of Diabetes (EASD). Eur Heart J 2007; 28: 88–136. [DOI] [PubMed] [Google Scholar]
- 7. Aschner P, Beck-Nielsen H, Bennett P, et al. Diabetes and impaired glucose tolerance. 5th ed. Brussels: IDF Diabetes Atlas, 2012. [Google Scholar]
- 8. Selvin E, Ning Y, Steffes MW, et al. Glycated hemoglobin and the risk of kidney disease and retinopathy in adults with and without diabetes. Diabetes 2011; 60: 298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rogvi S, Tapager I, Almdal P, et al. Patient factors and glycaemic control-associations and explanatory power. Diabet Med 2012; 29: e382–e389. [DOI] [PubMed] [Google Scholar]
- 10. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 977–986. [DOI] [PubMed] [Google Scholar]
- 11. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet 1998; 352: 837–853. [PubMed] [Google Scholar]
- 12. Genuth S, Eastman R, Kahn R, et al. Implications of the United Kingdom prospective diabetes study. Diabetes Care 2003; 26: S28–S32. [DOI] [PubMed] [Google Scholar]
- 13. The American Association of Clinical Endocrinologists. AACE Medical Guidelines for the Management of Diabetes Mellitus. The AACE system of intensive diabetes self-management-2002 update. Endocr Pract 2002; 8: 40–82.11939758 [Google Scholar]
- 14. Del Prato S, Felton AM, Munro N, et al. Improving glucose management: ten steps to get more patients with type 2 diabetes to glycaemic goal. Int J Clinical Pract 2005; 59: 1345–1355. [DOI] [PubMed] [Google Scholar]
- 15. Badedi M, Solan Y, Darraj H, et al. Factors associated with long-term control of type 2 diabetes mellitus. J Diabet Res 2016; 2016: 2109542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khattab M, Khader YS, Al-Khawaldeh A, et al. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complicat 2010; 24: 84–89. [DOI] [PubMed] [Google Scholar]
- 17. Sanal TS, Nair NS, Adhikari P. Factors associated with poor control of type 2 diabetes mellitus: A systematic review and meta-analysis. J Diabetolo 2011; 3:1 [Google Scholar]
- 18. Juarez DT, Sentell T, Tokumaru S, et al. Factors associated with poor glycemic control or wide glycemic variability among diabetes patients in Hawaii, 2006–2009. Prev Chronic Dis 2012; 9: 120065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ferwana M, Abdulmajeed I, Madani WA, et al. Glycemic control and accompanying risk factors: 4-year primary care study. J Diabet Metabol 2015; 6: 523. [Google Scholar]
- 20. Chiu CJ, Wray LA. Factors predicting glycemic control in middle-aged and older adults with type 2 diabetes. Prev Chronic Dis 2010; 7: A08. [PMC free article] [PubMed] [Google Scholar]
- 21. Kassahun T, Eshetie T, Gesesew H. Factors associated with glycemic control among adult patients with type 2 diabetes mellitus: a cross-sectional survey in Ethiopia. BMC Res Notes 2016; 9: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aikens JE, Piette JD. Longitudinal association between medication adherence andglycaemic control in type 2 diabetes. Diabet Med 2013; 30: 338–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Krapek K, King K, Warren SS, et al. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother 2004; 38: 1357–1362. [DOI] [PubMed] [Google Scholar]
- 24. Schetman JM, Nadkarni MM, Voss JD. The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care 2002; 25: 1015–1021. [DOI] [PubMed] [Google Scholar]
- 25. Kamuhabwa AR, Charles E. Predictors of poor glycemic control in type 2 diabetic patients attending public hospitals in Dar es Salaam. Drug Healthc Patient Saf 2014; 6: 155–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ramirez LDH, Soto AF, Valenzuela CLC, et al. Factors influencing glycemic control in patients with diabetes type II in Mexican patients. J Fam Med 2016; 3: 1051. [Google Scholar]
- 27. Bruce DG, Davis WA, Davis TME. Glycemic control in older subjects with type 2 diabetes mellitus in the Fremantle Diabetes Study. JAGS 2000; 48: 1449–1453. [DOI] [PubMed] [Google Scholar]
- 28. Al-Lawati JA, Barakat MN, Al-Maskari M, et al. HbA1c levels among primary healthcare patients with type 2 diabetes mellitus in Oman. Oman Med J 2012; 27; 465–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kasznicki J, Głowacka A, Drzewoski J. Type 2 diabetic patients’ compliance with drugtherapy and glycaemic control. Diabetologia Doświadczalna i Kliniczna 2007; 7: 199–203. [Google Scholar]
- 30. Kautzky-Willer A, Kosi L, Lin J, et al. Gender-based differences in glycaemic control and hypoglycaemia prevalence in patients with type 2 diabetes: results frompatient-level pooled data of six randomized controlled trials. Diabet Obesity Metabol 2015; 17: 533–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hill-Briggs F, Gary TL, Bone LR, et al. Medication adherence and diabetes control in urban African Americans with type 2 diabetes. Health Psychol 2005; 24: 349–357. [DOI] [PubMed] [Google Scholar]
- 32. Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care 2004; 27: 1218–1224. [DOI] [PubMed] [Google Scholar]
- 33. Asche C, LaFleur J, Conner C. A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clin Ther 2011; 33: 74–109. [DOI] [PubMed] [Google Scholar]
- 34. Adams AS, Trinacty CM, Zhang F, et al. Medication adherence and racial differences in A1C control. Diabetes Care 2008; 31: 916–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rozenfeld Y, Hunt JS, Plauschinat C, et al. Oral antidiabetic medication adherence and glycemic control in managed care. Am J Manag Care 2008; 14: 71–75. [PubMed] [Google Scholar]
- 36. Blonde L, Wogen J, Kreilick C, et al. Greater reductions in A1C in type 2 diabetic patients new to therapy with glyburide/metformin tablets as compared to glyburide coadministered with metformin. Diabet Obes Metab 2003; 5: 424–431. [DOI] [PubMed] [Google Scholar]
- 37. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986; 24: 67–74. [DOI] [PubMed] [Google Scholar]
- 38. Haun J, Noland-Dodd V, Varnes J, et al. Testing the BRIEF health literacy screening tool. Fed Pract 2009; 26: 24–31. [Google Scholar]
- 39. Gebrehiwot T, Jemal H, Dawit T. Non-adherence and associated factors among type 2 diabetic patients at Jimma University specialized hospital, Southwest Ethiopia. J Med Sci 2013; 13: 578–584. [Google Scholar]
- 40. Ali MK, Bullard KM, Imperatore G, et al. Characteristics associated with poor glycemic control among adults with self-reported diagnosed diabetes—National Health and Nutrition Examination Survey, United States, 2007–2010. MMWR Morb Mortal Wkly Rep 2012; 61: 32–78. [PubMed] [Google Scholar]
- 41. Hailu E, Mariam WH, Belachew T, et al. Self-care practice and glycaemic control amongst adults with diabetes at the Jimma University specialized hospital in south-west Ethiopia: a cross-sectional study. Afr J Prim Health Care Fam Med 2012; 4: 311–316. [Google Scholar]
- 42. Sontakke S, Jadhav M, Pimpalkhute S, et al. Evaluation of adherence to therapy in patients of type 2 diabetes mellitus. J Young Pharm 2015; 7: 462–469. [Google Scholar]
- 43. Elsous A, Radwan M, Al-Sharif H, et al. Medications adherence and associated factors among patients with type 2 diabetes mellitus in the Gaza strip, Palestine. Front Endocrinol (Lausanne). 2017; 8: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Al-Halaweh A, Davidovitch N, Almdal TP, et al. Prevalence of type 2 diabetes mellitus complications among Palestinians with T2DM. Diabetes Metab Syndr 2017; pii: S1871-4021(17)30166-2. [DOI] [PubMed] [Google Scholar]
- 45. Radwan M, Akbari Sari A, Rashidian A, et al. Influence of organizational culture on provider adherence to the diabetic clinical practice guideline: using the competing values framework in Palestinian Primary Healthcare Centers. Int J Gen Med 2017; 10: 239–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Radwan M, Akbari Sari A, Rashidian A, et al. Appraising the methodological quality of the clinical practice guideline for diabetes mellitus using the AGREE II instrument: a methodological evaluation. JRSM Open 2017; 8: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wooldridge KL, Wallston KA, Graber AL, et al. The relationship between health beliefs, adherence, and metabolic control of diabetes. Diabet Educ 1992; 18: 495–500. [DOI] [PubMed] [Google Scholar]
- 48. Rothenbacher D, Rüter G, Saam S, et al. Younger patients with type 2 diabetes need better glycaemic control: results of a community-based study describing factors associated with a high HbA1c value. Br J Gen Pract 2003; 53: 389–391. [PMC free article] [PubMed] [Google Scholar]
- 49. Nyunt SW, Howteerakul N, Suwannapong N, et al. Self-efficacy, self-care behaviors and glycemic control among type-2 diabetes patients attending two private clinics in Yangon, Myanmar. Southeast Asian J Trop Public Health 2010; 41: 943–951. [PubMed] [Google Scholar]
- 50. Sampson MJ, Hughes DA, Carrier MJ, et al. Status of HbA1c during acute hyperglycemia in type 2 diabetes. Diabetes Care 2002; 25: 537–541. [DOI] [PubMed] [Google Scholar]
- 51. Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Ann Internal Med 2008; 148: 737–746. [DOI] [PubMed] [Google Scholar]
- 52. Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011; 15: 97–107. [DOI] [PubMed] [Google Scholar]
- 53. Kautzky-Willer A, Kamyar MR, Gerhat D, et al. Sex-specific differences in metabolic control, cardiovascular risk, and interventions in patients with type 2 diabetes mellitus. Gend Med 2010; 7: 571–583. [DOI] [PubMed] [Google Scholar]


