Abstract
The global epidemic of diabetes, with increasing prevalence of type 2 diabetes (T2D), is placing a huge burden on health care management and financial systems. Unless new strategic solutions are developed, the increasing prevalence of T2D will result in a significant rise in morbidity, health care costs, and complications associated with diabetes. The introduction of smart devices in diabetes management may provide meaningful improvements in clinical outcomes, patient engagement, as well as potential cost reductions for the health care system. Future research may be capable of providing new smart and interactive solutions to the growing multidisciplinary diabetes team and, most important, to reduce the morbidity associated with T2D.
Keywords: blood glucose level, exercise, mobile app, physical activity, smart device, type 2 diabetes
Possible New Management Approach to Type 2 Diabetes
The recent introduction of wearable new smart devices may provide meaningful and reliable physical activity data, which, if used appropriately, may have the potential to offer new clinical management approaches to patients diagnosed with T2D. The ability of these smart devices to display visual goals and offer motivational graphics upon completion should not be underestimated. In addition to the exercise targets set for the user, the majority of these cost-effective devices can also be wirelessly connected to smartphones, which could be automatically synchronized with the freely available and password-protected cloud network. This network could become accessible live at anytime and anywhere by the patient, family members, and the clinicians, allowing potential multidisciplinary clinical decisions to be made in a much more informed and prompt manner. These interactive technologies could potentially offer valuable support in the treatment of T2D patients by providing real-time exercise duration, intensity, and energy expenditure data.
Some smart devices already available in the market are programmable even remotely to tailor a safe exercise program that can be adapted for each patient’s physical requirements. These intuitive devices that are already worn and used daily have inbuilt sensors that can measure exercise duration and intensity by using reliable accelerometers, tracking heart rate, and using GPS to precisely acquire the physical activity profile of the patient throughout the day. As an increase in adiposity has become one of most significant contributors to the development of T2D, a smart device could become a cost-effective and not invasive intervention prescribed by clinicians with the aim of improving self-motivation in regular exercise and to promote a more active and healthy lifestyle. For the T2D patient of having a tested and tailored physical activity program together with prompts and a reward gaming scheme, this could become a powerful new smart tool in diabetes lifestyle management. Further research is required to test the effectiveness and acceptability for such smart device specifically in T2D patients.
Blood Glucose Monitoring
Poor adherence to regular blood glucose testing, especially in younger adults with T2D is a constant concern for clinicians.1 Regular blood glucose testing is a key factor in determining the correct management of T2D and, as such, it should be considered a vital component of a patient’s daily routine. Already available smart devices could provide user-friendly visual interface data related to blood glucose level (BGL) concentrations, by connecting with existing validated portable devices via Bluetooth or wirelessly. Patients could benefit from increase of awareness of their BGL during specific time of the day, before or after food intake and even during physical activity.
Open access to specially designed online platforms that can be delivered by many already existing IT companies could possibly enable clinicians and other members of the multidisciplinary diabetes team to remotely monitor daily, weekly, and/or monthly BGL trends of their patients. By investing in improving the connectivity between the BGL monitoring devices, smartphones, and online platforms, all parties involved could potentially have access to “live” synchronized BGL data (Figure 1).
Figure 1.
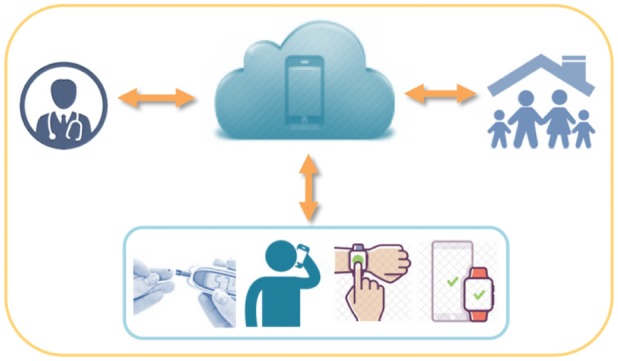
The device would be capable of capturing physical activity and BGL data, then automatically synchronize these outcomes to a secure cloud network and make results and information instantly available remotely to the multidisciplinary clinical team and family members (if required) anytime and anywhere.
Modern technology now allows clinicians to easily set up personalized prompts during the day to inform the patient with T2D that a BGL test is required at a specific time. Once taken, these BGL measurements can be automatically uploaded to the cloud network via password encryption, saving time and effort for the patients. Furthermore, severe hypoglycemic attacks occur in 25% of T2D patients who have been on insulin for more than 5 years,2 these cost-effective smart technologies could significantly help a patient’s engagement in their diabetes management care and potentially prevent severe complications. With this in mind, special logarithms could be developed to predict critical situations such as severe hypoglycemic attack, from which the smart device will automatically contact the emergency services, if required.
Considering the fast progression of modern technologies and the large investments in this priority research sector, dedicated health-IT companies should develop new user-friendly and interactive platforms. These should be capable of automatically filtering, processing and presenting (in user friendly reports) the large data input from T2D patient’s BGL and other key parameters, which may result in a significant reduction of time for clinicians to interpret data without the requirement of specialized staff or additional software. When BGL targets are met, the T2D patient can be informed with a gentle vibration on the wrist and discreetly notified of their glycemic achievements by displaying clear messages and “awards icons” directly on the watch screen. These “award icons” can be collected over a period of time and serve as an incentive and positive reinforcement for adhering to the customized diabetes management plan prescribed by the clinician. Future research should focus in testing the effectiveness of these technologies in stimulating positive behavioral changes with regular BGL monitoring. As more evidence will become available on the effectiveness of these smart technologies in helping T2D patients, it will also become possible to analyze the health cost savings for hospitals and diabetic departments. These savings could be proportionally reinvested to improve the care of T2D patients with severe complications and to compensate and incentivize clinicians for effectively adopting a new smart model of care.
Access to Interactive Technologies and Limitations
The number of worldwide smartphone owners is estimated to grow from 1.5 billion in 2014 to around 2.5 billion in 2019.3 Just over 36% of the world’s population is projected to use a smartphone by 2018, which has seen an unstoppable increase from 10% in 2011.3 Over the past decade, Internet cost and network provider charges have significantly reduced. Since 2005 the cost of transmitting one megabyte of data wirelessly has dropped from $8 to a few cents, and it is still falling.4 Evidence shows that in June 2013, there were 31.09 million mobile services in operation in Australia, up 3% since June 2012 In May 2013, up to 11.19 million people had a smartphone in Australia.5 Recent government statistics revealed that 14 million Australians used cloud computing services in the 6 months to May 2013, compared to 12.57 million in the 6 months to May 2012.5 It is expected that cloud network users will continue to increase in number in adults and in adolescent. Finally, the possible introduction of smart technology as part of their daily life for patients with T2D is likely to be welcomed by a growing modern Australian community that is already familiar with how to effectively use the cloud network.
Inevitably there are a few limitations that should be considered when wearing such interactive technologies. Regular software updates are usually required, which may impact the availability of synchronized data transfer. Missing physical activity data in T2D patients may occur during sporting activity such as swimming, as wearing smart watches and wristbands would damage the device, although the very latest devices are now safe to use while swimming. In addition to improved exercise regime and BGL control, technology should also facilitate patient’s awareness on important aspects such as nutrition intake and drug adherence.
Protecting patient privacy and confidentiality of data remains paramount; security protocols already exist among the major phone and Internet providers, such as Google6 and Apple7, to ensure constant system security, encryption and data protection, data backup and privacy, location services, password authentication, and intrusion detection. Access to smart device technology is not often supported by the health care service yet, although they are becoming more affordable, not all T2D patients may be able to purchase them. Finally, more evidence is also needed to establish the feasibility and willingness of T2D patients in interacting with health related technologies, especially among older age groups where patients may exhibit comprehension issues and reading impairments.
Conclusion
The introduction of smart devices in diabetes management may provide meaningful improvements in clinical outcomes, patient well-being and engagement, as well as cost reductions for the health care system. Future research may be capable of providing new solutions to the growing multidisciplinary diabetes team and, most important, to reduce the growing morbidity associated with T2D. The authors recommend further randomized control trials to determine the effectiveness and the affordability of these new devices and to assess several outcome measures ranging from physical activity to improved glycemic management in patients with T2D.
Footnotes
Abbreviations: BGL, blood glucose level; T2D, type 2 diabetes.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Diabetes: the silent pandemic and its impact on Australia has been supported by an unrestricted educational grant from Novo Nordisk. Baulkham Hills, NSW, Australia: Baker IDI Heart & Diabetes Institute; 2012. Available at: https://www.baker.edu.au/–/media/Documents/impact/diabetesthe–silent–pandemic.ashx?la=en [Google Scholar]
- 2. Noh RM, Graveling AJ, Frier BM. Medically minimising the impact of hypoglycaemia in type 2 diabetes: a review. Expert Opin Pharmacother. 2011;12(14):2161-2175. [DOI] [PubMed] [Google Scholar]
- 3. Number of smartphone users worldwide 2014-2020. Statista. June 2015. Available at: https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Accessed February 23, 2017.
- 4. Berkeley J. Planet of the phones. Economist. February 2015. Available at: http://www.economist.com/news/leaders/21645180-smartphone-ubiquitous-addictive-and-transformative-planet-phones. Accessed February 23, 2017.
- 5. Australia’s mobile digital economy—ACMA confirms usage, choice, mobility and intensity on the rise. ACMA. December 2013. Available at: http://www.acma.gov.au/theACMA/Library/Corporate-library/Corporate-publications/australia-mobile-digital-economy. Accessed November 20, 2016.
- 6. Google. Google cloud platform security. December 2016. Available at: https://cloud.google.com/security/. Accessed December 1, 2016.
- 7. Apple. iOS Security, report no.: 9.3 or later. 2016. Available at: https://www.apple.com/business/docs/iOS_Security_Guide.pdf. Accessed November 28, 2016.


