The clinical benefits of continuous glucose monitoring (CGM) in adults with type 1 diabetes is well known.1 However, the benefits of CGM initiation early after type 1 diabetes onset are not known.
In this retrospective, proof of concept, pilot study, we analyzed the electronic health records of adults (age ≥18 years) diagnosed with type 1A diabetes (T1D) between June 2013 and June 2015 who had at least 1 year of follow up at the Barbara Davis Center for Diabetes Adult Clinic. T1D is defined by at least two positive islet autoantibodies. Adults with other types of diabetes, fewer than three glycosylated hemoglobin (A1C) values during study, antidiabetic medications beside insulin, CGM initiation after 6 months or discontinuation within 3 months, previous participation in immune intervention studies, and pregnant women were excluded. Patients who initiated CGM within 6 months of their diagnosis of T1D were included as the “CGM group” and those who did not use CGM from T1D diagnosis to the study end served as “controls.” Baseline was defined as CGM initiation for CGM group and 3-4 months after diagnosis for controls. The differences in the A1C between CGM and control groups were assessed at diagnosis, baseline, 3, 6, and 12 months after baseline using Student’s t-test. Chi-square test was used for the comparison of discrete data.
A total of 19 adults (6 CGM group and 13 controls) with T1D were included in the present analysis. CGM was initiated within a mean of 3.8 months of diagnosis in the CGM group.
There were no differences in age (24.8 ± 4.9 vs 21.3 ± 3.9, P = .1), gender (50% vs 76% males, P = .3), body mass index at diagnosis (22.9 ± 5.9 vs 23.8 ± 3.8, P = .7), insurance type (100% vs 77% private insurance, P = .5), or insulin delivery methods (50% vs 85% multiple daily injection, P = .3) between the CGM group and controls.
Mean A1C at diagnosis (12.4 ± 1.5 vs 10.6 ± 2.8, P = .15), baseline (8.1 ± 3.0 vs 7.4 ± 1.9, P = .55), and 3 months (6.3 ± 0.6 vs 7.6 ± 1.7, P = .17) was similar between the groups. However, mean A1C was lower at 6 months (6.7 ± 1.3 vs 8.3 ± 1.5, P = .047) and 1 year (6.7 ± 1.0 vs 8.2 ± 1.6, P = .04) in the CGM group compared to controls (Figure 1). At 1 year, four patients in the CGM group (67%) achieved A1C below 7% compared to one patient in the control group (8%).
Figure 1.
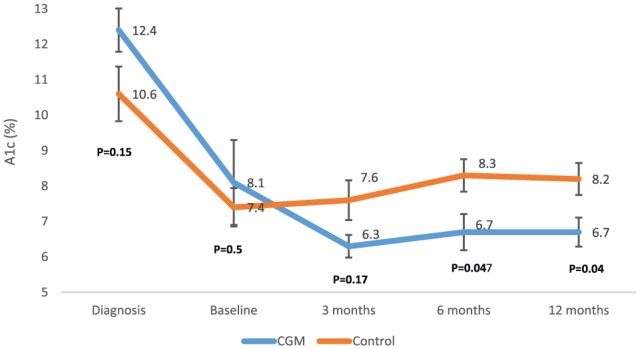
Mean A1c at diagnosis, baseline, and over 1 year between CGM group and controls.
This pilot study suggests that CGM initiation within 6 months of T1D diagnosis results in better glycemic control. Though self-monitoring of blood glucose is an integral part of T1D management and has been shown to improve glycemic control,2 it does not provide information on glucose trends and multiple finger sticks daily is cumbersome to newly diagnosed patients with T1D. Recent studies have shown that CGM is safe for insulin administration without confirmatory fingerstick3 and it is effective regardless of mode of insulin delivery.4 Therefore, CGM may be helpful for newly diagnosed patients and provide greater understanding of the effects of insulin, food, exercise, and stress on glucose fluctuations. Its use may ease management of diabetes. An adequately powered randomized control trial is needed to confirm the findings of our study.
Footnotes
Abbreviations: AIC, glycosylated hemoglobin; CGM, continuous glucose monitoring; TID, type 1A diabetes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: VNS’s employer has received research funding from T1D Exchange and Sanofi. VNS received speaking fees from the Dexcom Inc. TLG, MM, and JKS report no conflicts of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by the Dexcom Inc. However, the sponsor had no role in devising the study concept, data collection, analysis, and interpretation.
References
- 1. Ruedy KJ, Tamborlane WV, Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. The landmark JDRF continuous glucose monitoring randomized trials: a look back at the accumulated evidence. J Cardiovasc Transl Res. 2012;5(4):380-387. [DOI] [PubMed] [Google Scholar]
- 2. Garg S, Hirsch IB. Self-monitoring of blood glucose. Int J Clin Pract Suppl. 2010;166:1-10. [DOI] [PubMed] [Google Scholar]
- 3. Aleppo G, Ruedy KJ, Riddlesworth TD, et al. REPLACE-BG: a randomized trial comparing continuous glucose monitoring with and without routine blood glucose monitoring in adults with well-controlled type 1 diabetes. Diabetes Care. 2017;40(4):538-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beck RW, Riddlesworth T, Ruedy K, et al. Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial. JAMA. 2017;317(4):371-378. [DOI] [PubMed] [Google Scholar]


