ABSTRACT
Intrinsic cystic lesions in the optic chiasm are an uncommon cause of bitemporal hemianopia compared with compressive lesions extrinsic to the chiasm. A 40-year-old man presented with difficulty driving. Clinical assessment revealed a bitemporal hemianopia. Magnetic resonance imaging showed an unusual cystic appearance of the chiasm. The appearance was felt to be most likely secondary to previous infective or inflammatory disease, but biopsy was not undertaken given the very significant risk of further visual loss.
KEYWORDS: Bitemporal hemianopia, cyst, cystic lesion, intrinsic cystic lesion, optic chiasm
A 40-year-old Indian man presented with difficulty driving in unfamiliar surroundings. He had moved from India to Australia the year previously and noticed these symptoms only after immigration. He had had a routine ophthalmological assessment in India in 2014 and was told that he “had a lazy left eye”, but no other abnormality was reported.
His past medical history was significant for latent tuberculosis, but there was no history of any neurological or ophthalmological disease. He had not been treated with anti-mycobacterial or other medications in the past. His alcohol intake was only two standard drinks per week. His diet was predominantly, but not exclusively, vegetarian.
On examination, his best-corrected visual acuity was right 6/9.5 and left 6/38. Ishihara was right 14/15 and left 3/15. 30-2 threshold perimetry showed bitemporal visual field loss, more marked on the left (Figure 1).Ophthalmoscopy showed myopic discs with cup: disc ratios of around 0.8 and somewhat pale neuroretinal rims. Optical coherence tomography was significant for bilateral retinal nerve fibre layer thinning (right 50 µm and left 52 µm) in a pattern of relative bow-tie atrophy (Figure 2)—the nasal and temporal quadrants were more atrophic than the superior and inferior. Chest x-ray was unremarkable. Vitamin B12 level was 102 pmol/L (range: 138–652 pmol/L) and supplementation was commenced. Serology for human immunodeficiency virus (HIV), syphilis, and cysticercosis was negative. Other relevant blood tests such as full blood count, electrolytes, urea and creatinine levels, inflammatory markers, serum angiotensin-converting enzyme level, and iron studies were unremarkable. Given the clinical presentation and investigations, a nutritional or toxic/drug-induced cause was considered unlikely in his case.
Figure 1.
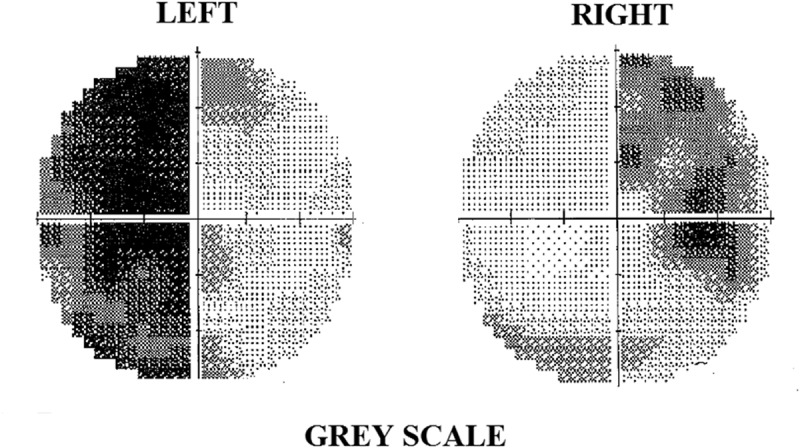
Automated perimetry showing left visual field on the left side and right visual field on the right side. There is bitemporal hemianopia (left worse than right).
Figure 2.
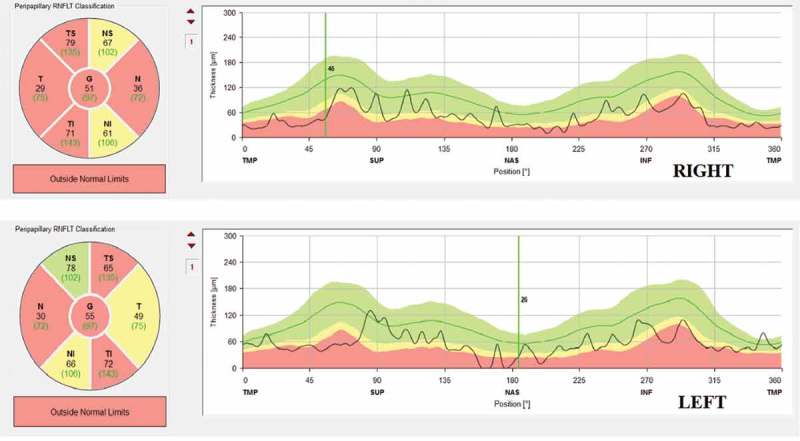
Optical coherence tomography (OCT): (top panel) right retinal nerve fibre layer (RNFL) measurements; (bottom panel) left RNFL measurements. Relative “bow-tie atrophy” pattern is noted bilaterally.
Magnetic resonance imaging (MRI) of the brain and orbits (Phillips 3T) showed a non-enhancing 7.4 × 3.7 × 4.2 mm ovoid cystic lesion within the optic chiasm with signal intensity equivalent to that of cerebrospinal fluid (CSF) on all sequences. Cystic changes extended along both optic tracts for approximately 7 mm on the right and 11 mm on the left. There were also small T2-high-intensity foci in both optic nerves adjacent to the chiasm, likely to represent further cysts too small to resolve. There was no evidence of chiasmal compression (Figures 3–5).
Figure 4.
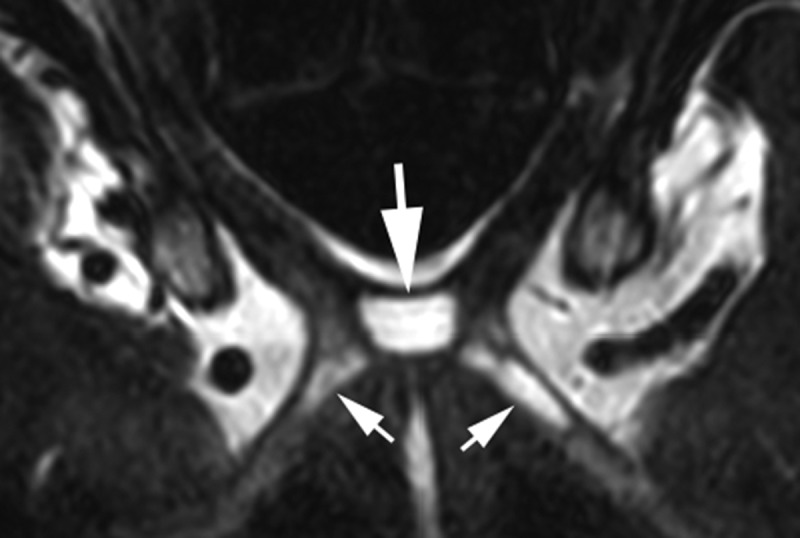
MRI axial T2 drive: As well as the cyst in the chiasm (large arrow), there are smaller cysts in both optic tracts (small arrows).
Figure 3.

MRI coronal T2: Cyst within the optic chiasm (arrow).
Figure 5.
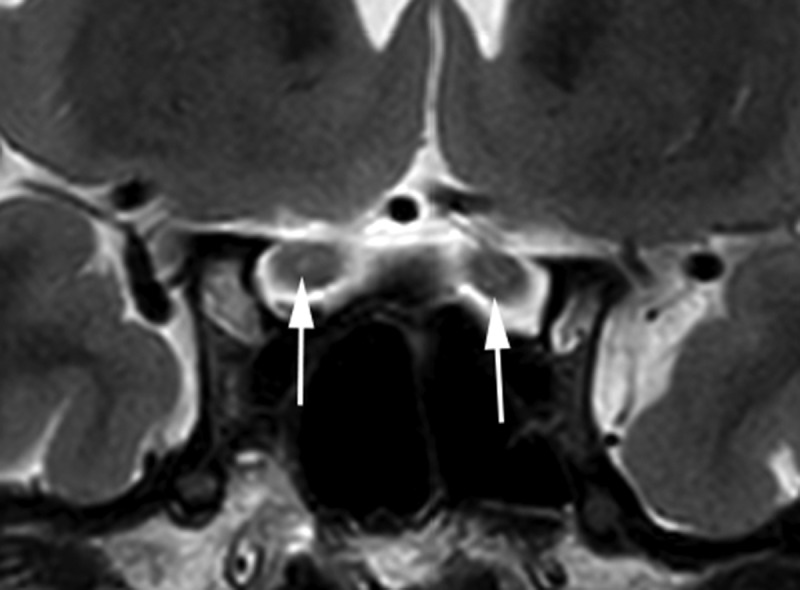
MRI coronal T2: Small, high-intensity foci in both optic nerves (arrows).
We cannot find a report in the literature of a similar case. The differential diagnosis for a cystic lesion of the chiasm includes arachnoid cyst, ganglioglioma, pilocytic astrocytoma, or sequelae of a prior inflammatory or infective disease.
Chowdhury first described an arachnoid cyst within the optic chiasm in 1976.1 Primary arachnoid cysts commonly occur as benign developmental anomalies, but, less frequently, there can be post-inflammatory accumulation of CSF in the subarachnoid space following intracranial haemorrhage, infection, or trauma.2 The characteristic appearance of an arachnoid cyst on MRI is that of a well-defined, non-enhancing mass that is isointense with the CSF signal.3,4 Occurrence of symptoms is rare and precipitated by mass effect or displacement of the surrounding structures following sudden enlargement.5 Our case was interesting as there were multiple cysts, the largest one within the chiasm (Figures 3–5). Such multiple cystic lesions with emergence of visual difficulties later in life suggested an acquired lesion rather than a primary arachnoid cyst.
Gangliogliomas can also cause cystic lesions in the optic chiasm and tract.6–9 Although rare compared with other brain neoplasms, they represent the most common neuronal-glial neoplasm within the central nervous system. MRI characteristically shows a single, well-defined cystic mass with a solid mural nodule. The solid component shows low-to-intermediate T1-weighted and high T2-weighted signal intensity. Enhancement of the solid portion is variable, ranging from non-enhancement to ring-like enhancement or intense homogeneity. There is minimal associated mass effect or vasogenic oedema.10
Pilocytic astrocytomas are low-grade tumours that may exhibit both solid and cystic components that are typically hypointense to isointense on T1-weighted sequences and hyperintense on T2-weighted and FLAIR (fluid-attenuated inversion recovery) sequences. Contrast enhancement tends to be diffuse.11 Patients typically present in early childhood or teens. Although commonly localised to the cerebellum, they are well reported to occur in the optic pathway (especially in the hypothalamo-chiasmatic region) in children with neurofibromatosis type 1.12
The imaging characteristics of our case with multiple cysts and lack of enhancement were considered inconsistent with either pilocytic astrocytoma or ganglioglioma.
Rarely, CSF collections within the chiasm have been reported in the context of raised intracranial pressure secondary to intra-orbital or orbital apex lesions such as meningioma.13 There was no clinico-radiological evidence of raised intracranial pressure in our patient.
In neurocysticercosis, the vesicular larvae have CSF-like intensity signal on all MRI sequences. As the cyst dies, an inactive calcified nodule of low intensity on proton-weighted MRI appears.14 These cysts are located within the brain parenchyma. Bitemporal hemianopia has been reported in patients with neurocysticercosis because of compression from subarachnoid or parenchymal cysts rather than intrinsic chiasmal lesions.15 The radiological appearance of our case suggested that neurocysticercosis was unlikely and history and serological tests were negative.
In summary, the radiological appearances of the chiasmal cystic lesion (along with multiple smaller cysts in optic nerves and tracts) in our patient were unusual and we cannot find a previous similar report. We suspect that these cysts are the result of acquired/resolved disease of the chiasm, which may have been inflammatory or infective in nature but the precise cause remains unknown. A biopsy is not currently planned due to the significant risk of further visual deterioration.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- [1].Chowdhury AM. Cyst within the parenchyma of the optic chiasm. Br J Ophthalmol 1976;60:581–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Choi JU, Kim DS.. Pathogenesis of arachnoid cyst: congenital or traumatic? Pediatr Neurosurg 1998;29:260–266. [DOI] [PubMed] [Google Scholar]
- [3].Gosalakkal JA. Intracranial arachnoid cysts in children: a review of pathogenesis, clinical features, and management. Pediatr Neurol 2002;26:93–98. [DOI] [PubMed] [Google Scholar]
- [4].Osborn AG, Preece MT.. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology 2006;239:650–664. [DOI] [PubMed] [Google Scholar]
- [5].Rao G, Anderson RC, Feldstein NA, Brockmeyer DL.. Expansion of arachnoid cysts in children: report of two cases and review of the literature. J Neurosurg 2005;102(3 Suppl):314–317. [DOI] [PubMed] [Google Scholar]
- [6].Chilton J, Caughron MR, Kepes JJ.. Ganglioglioma of the optic chiasm: case report and review of the literature. Neurosurgery 1990;26:1042–1045. [PubMed] [Google Scholar]
- [7].Pant I, Suri V, Chaturvedi S, Dua R, Kanodia AK.. Ganglioglioma of optic chiasma: case report and review of literature. Childs Nerv Syst 2006;22:717–720. [DOI] [PubMed] [Google Scholar]
- [8].Shuangshoti S, Kirsch E, Bannan P, Fabian VA.. Ganglioglioma of the optic chiasm: case report and review of the literature. AJNR Am J Neuroradiol 2000;21:1486–1489. [PMC free article] [PubMed] [Google Scholar]
- [9].Liu GT, Galetta SL, Rorke LB, Bilaniuk LT, Vojta DD, Molloy PT, Phillips PC, Needle M, Duhaime AC, Sutton LN, Volpe NJ.. Gangliogliomas involving the optic chiasm. Neurology 1996;46:1669–1673. [DOI] [PubMed] [Google Scholar]
- [10].Shin JH, Lee HK, Khang SK, Kim DW, Jeong AK, Ahn KJ, Choi CG, Suh DC.. Neuronal tumors of the central nervous system: radiologic findings and pathologic correlation. Radiographics 2002;22:1177–1189. [DOI] [PubMed] [Google Scholar]
- [11].Collins VP, Jones DT, Giannini C.. Pilocytic astrocytoma: pathology, molecular mechanisms and markers. Acta Neuropathol (Berl) 2015;129:775–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Baker SJ, Ellison DW, Gutmann DH.. Pediatric gliomas as neurodevelopmental disorders. Glia 2016;64:879–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].McNab AA, Wright JE.. Cysts of the optic nerve three cases associated with meningioma. Eye 1989;3(Pt 3):355–359. [DOI] [PubMed] [Google Scholar]
- [14].Neurocysticercosis: Carpio A. an update. Lancet Infect Dis 2002;2:751–762. [DOI] [PubMed] [Google Scholar]
- [15].Chang GY, Keane JR.. Visual loss in cysticercosis: analysis of 23 patients. Neurology 2001;57:545–548. [DOI] [PubMed] [Google Scholar]


