Abstract
Study Design
Diagnostic study
Objectives
To evaluate the validity and reliability of a radiographic diagnosis of femoroacetabular impingement (FAI) by a non-radiologist.
Background
Symptomatic FAI is prevalent and thought to be a cause hip osteoarthritis (OA). However, the diagnosis is often delayed by 1 to 2 years, in large part because radiographic findings are often subtle and clinicians have been unaware of their significance. The purpose of this study was to evaluate the validity of a radiographic diagnosis of FAI by a non-radiologist.
Methods
A population-based sample of 701 subjects was recruited in Vancouver, Canada. For the current study, 50 subjects were selected - 40 randomly from the population sample and 10 from an orthopaedic practice with confirmed FAI. An anterior-posterior pelvis and bilateral Dunn radiographs were acquired and read by a fellowship-trained musculoskeletal radiologist and a 3rd year medical student who received basic training in radiographic signs of FAI. Three radiographic signs were evaluated: the lateral center edge angle (LCEA), alpha angle and cross-over sign. Validity was assessed using sensitivity and specificity, Bland-Altman limits of agreement and Kappa.
Results
The sample contained 65% women (n=31), was 62% Caucasian and 38% Chinese, and had a mean age of 38.3 years. For correctly diagnosing FAI, the non-radiologist reader had a sensitivity of 0.83 and specificity of 0.87. Intra-rater kappa value was 0.72, and prevalence-adjusted bias-adjusted Kappa 0.76.
Conclusion
This study provides evidence that a non-radiologist can accurately and reliably identify FAI on plain films.
Keywords: femoroacetabular impingement, hip radiography, validation, hip osteoarthritis
Introduction
There is emerging evidence that most hip pain in young active adults is caused by femoroacetabular impingement (FAI), a prevalent condition and proposed pre-cursor to hip osteoarthritis (OA) [1,2]. Despite its prevalence [3–5], and relatively consistent presentation [6,7], many patients with symptomatic FAI experience significant delays in diagnosis (1–2 years) [6]. This occurs despite consistent signs and symptoms and subtle but identifiable abnormalities on plain films [6,7]. As a result, many are misdiagnosed and receive inappropriate, ineffective or harmful treatment [8,6], including well-intentioned exercise to gain range of motion (ROM) and strength which may inadvertently lead to labral and chondral damage and accelerated onset of OA [9].
Earlier identification of FAI could substantially reduce the time to diagnosis and mitigate damage to the hip joint. Currently, consultation with experienced musculoskeletal (MSK) health care providers is often necessary, though not always sufficient, to receive an appropriate diagnosis and treatment [8]. The ability of those in the front lines to order the correct views and accurately read FAI signs could enhance early diagnosis and potentially allow patients to be appropriately triaged for a trial of conservative care and/or flagged for specialist referral before problems arise and hip arthroscopy and/or replacement is required.
The purpose of this study was to evaluate the validity and reliability of a radiographic diagnosis of FAI by a non-radiologist.
Materials and Methods
The Clinical Research Ethics Board at the University of British Columbia approved the study. All participants provided informed consent and the rights of the subjects were protected.
IMPAKT-Hip study sample
This study was performed as part of a larger Canadian longitudinal study on the role of FAI and physical activity in hip pain, the IMPAKT-HiP study (Investigations of Mobility, Physical Activity and Knowledge Translation in Hip Pain). For IMPAKT-HiP, a random population-based sample of 700 subjects (500 Caucasian and 201 Chinese) was recruited through random digit dialing in Metro Vancouver, Canada. Inclusion criteria included individuals that were between the ages of 20 and 49, reported that both parents were of Caucasian or Chinese descent, and could attend a two-hour assessment session, consisting of physical assessment, hip radiographs and a questionnaire. Subjects were excluded if they were pregnant, or reported previous hip surgery, fibromyalgia or inflammatory arthritis, severe low back or knee pain, or had an acute hip injury within the previous 6 months.
Study sample
For the current study, 50 subjects were selected - 40 randomly from the above population-based sample and 10 with clinically, imaging, and arthroscopically confirmed FAI to enrich the sample with an adequate number of positive test findings. The 10 with FAI were drawn from an orthopaedic practice in Vancouver, met study criteria for IMPAKT-HiP and an orthopedic surgeon specializing in FAI confirmed the diagnosis.
Radiography
An anterior-posterior (AP) pelvis (weight-bearing, hips IR 15 ) and bilateral Dunn projection radiographs were acquired using standardized protocols. For the AP pelvis view, the subject was in a weight-bearing position, with the legs internally rotated 15° to allow better visualization of the contour of the lateral femoral head-neck junction [10]. The film-focus distance was 120 cm and the central beam was directed to a midpoint between a line connecting both anterior-superior iliac spines and the superior border of the symphysis.
For the Dunn view, the subject was supine and the hip was positioned in 45° flexion and 20° abduction while maintaining neutral rotation (defined as the tip of the coccyx pointing toward the midpoint of the superior aspect of the symphysis pubis). The x-ray beam was directed perpendicular to the table at the point midway between the anterior superior iliac spine and the symphysis pubis. Standard radiographic technique was followed [11].
FAI radiographic signs
Three radiographic signs were evaluated: the lateral center edge angle (LCEA) [12], and cross-over sign[13](pincer FAI), and the alpha angle [14] (cam FAI) (Figures 1, 2, and 3). FAI was defined radiographically as any one of LCEA > 40, alpha angle > 55 and presence of a cross-over sign. Description and definitions for a positive test are given in Table 1.
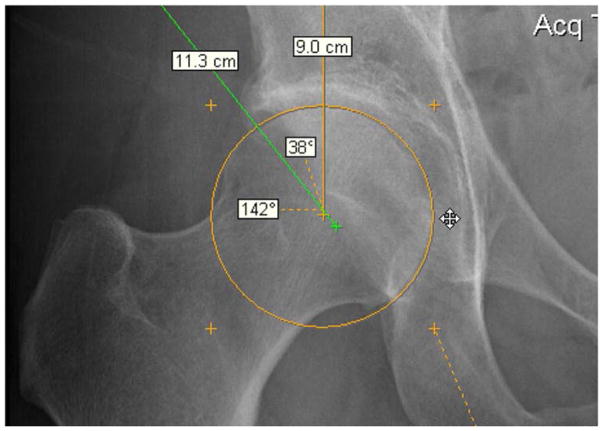
Fig. 1.
Lateral center edge angle of 38°. An angle >40° indicates pincer impingement
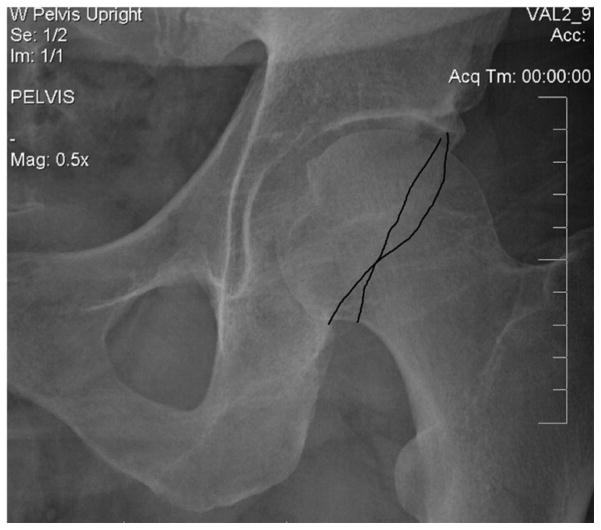
Fig. 2.
Radiographic appearance of the crossover sign
Fig. 3.
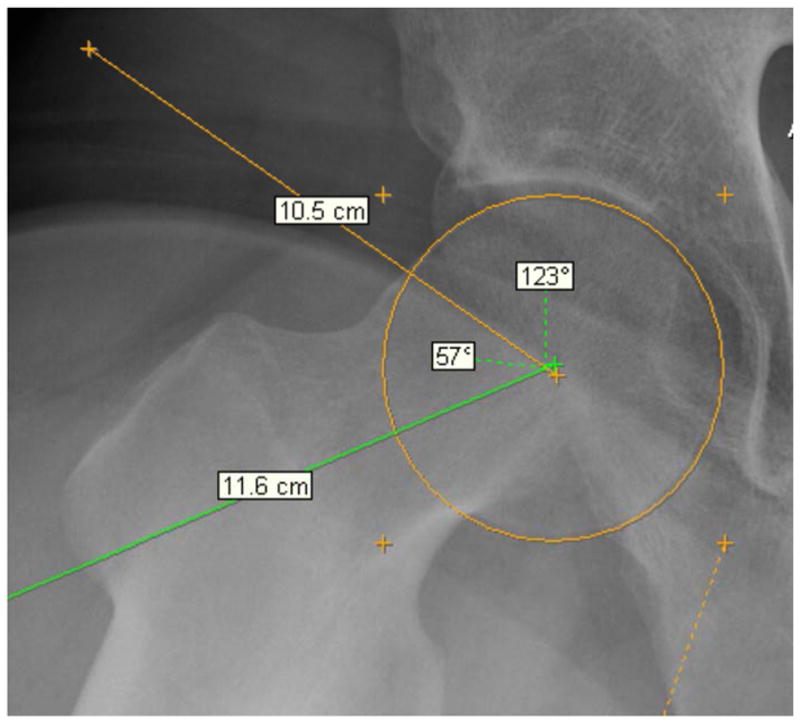
Alpha angle of 57° (>55° indicates cam impingement)
TABLE 1.
Description and definition of radiographic FAI signs evaluated
| Radiographic sign | Description | Definition of positive test |
|---|---|---|
| Alpha angle | Angle formed by 1) the axis of the femoral neck, and 2) a line connecting the center of the femoral head to the point where the contour begins to stray from a spherical radius | >55° on Dunn view |
| Lateral Center Edge Angle | Angle between 1) a line through the center of the femoral head, perpendicular to the transverse axis, and 2) a line through the center of the femoral head, passing through the most superolateral point of the sclerotic weight-bearing zone of the acetabulum | >40° on AP radiograph |
| Crossover sign, focal acetabular retroversion | Anterior acetabular rim lies lateral to posterior rim in the cranial part of acetabulum, then crosses the posterior rim in the distal part of the acetabulum. Considered negative if the cross happens superior to the femoral head. | Present on AP radiograph |
Image Evaluation
Reader training
A fellowship-trained MSK radiologist (JK) instructed a 3rd year medical student (CZ) (no prior experience with hip radiographs or clinical FAI) on scoring of the above radiographic signs of FAI. The medical student then evaluated the digital radiographs of 25 hips (AP and Dunn views) obtained in subjects not from the study cohort, reviewed results with the radiologist and formed final consensus for definitions for each FAI variable.
After blinding all demographic and clinical information, the 50 hips were randomized and read by the fellowship-trained MSK radiologist experienced in FAI, and the 3rd year medical student. The medical student re-read all films 8 weeks later in a new randomized order.
Analysis
Validity was assessed using sensitivity and specificity of the readers scores against the MSK radiologists standard. To examine agreement for the alpha angle and LCEA measurements obtained from the two readers, Bland and Altman plots were used. This plot included horizontal lines at the mean and 2 standard deviations of the differences between the two readers, depicting the level of bias and the limits of agreement [15].
For intra-reader reliability of the medical student, overall agreement (FAI/no FAI) was examined using Cohen’s Kappa, as well as the prevalence-adjusted bias-adjusted Kappa (PABAK). PABAK measures agreement beyond chance while taking into account both the prevalence of a positive finding and the bias of each measurement for reporting a positive finding. A PABAK of >0.60 was considered to indicate adequate reliability.
Results
The sample contained 65% women (n=31), was 62% Caucasian and 38% Chinese, and had a mean age of 38.3 years (SD=8.0). Hip pain in the past 12 months was reported by 42%. One hip had a fracture and was excluded, leaving 49 hips. The results are given in Table 2. When combining all three tests, the sensitivity was 0.83 and specificity was 0.87. For the individual tests, only the sensitivity for the cross-over sign was below 0.85 (0.50). There were 6 cases of cross-over; otherwise there was a balanced prevalence of positive and negative findings allowing for a more precise assessment.
TABLE 2.
Criterion validity of 3 radiographic FAI signs (n=49 hips) for a trained non-radiologist reader (medical student) versus gold standard (Fellowship-trained MSK radiologist)
| Alpha Angle > 55 (CAM) | Lateral Centre Edge Angle > 40° (Pincer) | Cross-over Sign (Pincer) | 3 FAI signs combined | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Fellowship-trained MSK radiologist | Fellowship-trained MSK radiologist | Fellowship-trained MSK radiologist | Fellowship-trained MSK radiologist | ||||||||||
| Yes | No | Total | Yes | No | Total | Yes | No | Total | Yes | No | Total | ||
|
|
|||||||||||||
| Non-radiologist | Yes | 20 | 4 | 24 | 12 | 5 | 17 | 3 | 5 | 8 | 35 | 14 | 49 |
| No | 3 | 22 | 25 | 1 | 31 | 32 | 3 | 38 | 41 | 7 | 91 | 98 | |
| Total | 23 | 26 | 49 | 13 | 36 | 49 | 6 | 43 | 49 | 42 | 105 | 148 | |
|
|
|||||||||||||
| Sensitivity | 0.87 | 0.92 | 0.50 | 0.83 | |||||||||
| Specificity | 0.85 | 0.86 | 0.88 | 0.87 | |||||||||
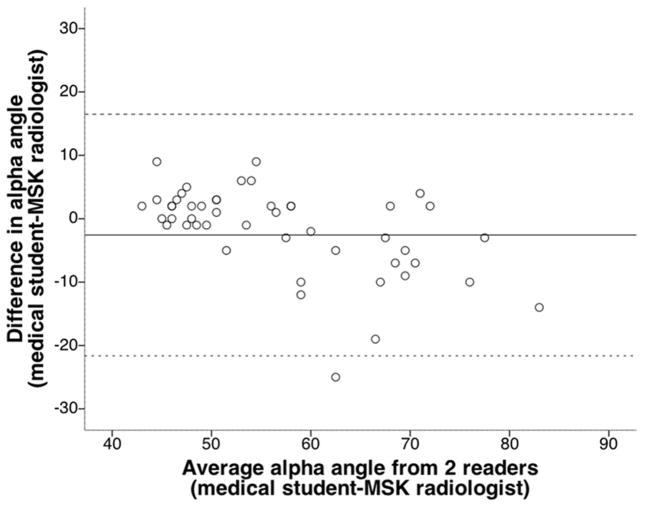
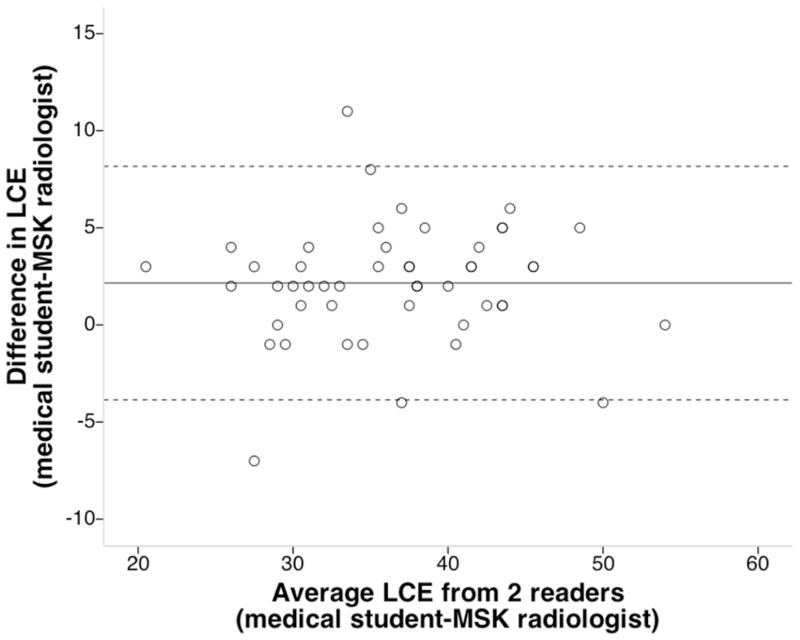
The Bland-Altman plots show the average value of the alpha angle (Figure 4) and LCEA (Figure 5) between the two readers for each subject, i.e., the theoretical true value, (x axis) against the difference between them. The dotted lines represent two SDs from the mean and the majority of the results in the study fall well within these lines.
Fig. 4.
Bland–Altman plot depicting agreement on alpha angle between radiographic alpha angle measurements by a trained medical student and MSK fellowship-trained radiologist (gold standard)
Fig. 5.
Bland–Altman plot depicting agreement on the lateral center edge (LCE) angle between radiographic lateral center edge angle measurements by a trained medical student and MSK fellowship trained radiologist (gold standard)
The intra-rater overall kappa value was 0.72 and overall PABAK value was 0.76. For the individual tests, intra-rater ICC for the alpha angle was 0.97 and for the LCEA was 0.87. For the crossover test, kappa was 0.58.
Discussion
This study provides evidence that a non-radiologist can accurately read FAI radiographic signs with minimal training. Symptomatic FAI is a prevalent problem seen by a variety of MSK clinicians. The diagnosis, often delayed by 1 to 2 years[6], hinges on the interpretation of the radiograph [16]. Early diagnosis of FAI and minimally invasive interventions could prevent progression to hip OA and the growing number of THR procedures, especially in those < 55 years.
The results are encouraging given that the FAI radiographic signs can be subtle and challenging to measure. The overall sensitivity for the presence or absence of FAI was 0.83 and specificity was 0.87. For the individual tests, the alpha angle and LCEA, the most commonly reported FAI signs for CAM and pincer, respectively had good validity. The crossover sign had acceptable sensitivity, but specificity was 0.50; precision may have been effected by low numbers (6 cases)
Repeated measurements will rarely agree exactly, therefore it is important to know by how much the new method is likely to differ from the established. If this is not enough to cause problems in clinical interpretation and effect decisions on patient management, the new method can replace the established [15]. The Bland-Altman plots which provide limits of agreement in the units of the measurement shed light on this. For the alpha angle, there is evidence that the mean alpha angle of normal hips (<50 degrees) is substantially lower (20–40 degrees [2,17]) than whose with symptomatic cam FAI. The Bland-Altman plots from our data for alpha angle (Figure 1) show that for the vast majority, the scores of the two readers are within 10 degrees of each other. The limits of agreement for the difference in readings for the LCEA are smaller, with the majority within 3–4 degrees, again likely sufficient to classify patients into pincer FAI or not.
Evaluation of the cross-over sign was not well-validated. There were only six cases of cross-over sign present, but of these, three were missed and were consequently false negatives. Technical challenges including susceptibility to poor image quality and inadequate standardization of patient positioning make the cross-over sign less reproducible [18], and may have effected results.
The study several strengths. We used standardized radiographic protocols and conducted them at the same institution. Technicians were trained in the standardized protocols. Second, we had a balanced prevalence of positive and negative signs, providing more robust, precise findings. A third strength was the blinded design, such that neither reader was aware of the clinical information for the patient, or of the readings of the other observer. Fourth, for cam FAI we used the Dunn view - the radiographic view and protocol which has been shown to have the best sensitivity, specificity, predictive values and accuracy for alpha angle [19].
This study has several limitations. We used a single MSK radiologist’s interpretation as a reference standard, rather than test inter-rater variability between two expert readers. However, numerous studies [8,18,16] have shown good reproducibility between such readers, hence this was not the thrust of our manuscript. Rather, our purpose was to use the best (most reliable and clinically common) radiographic signs of FAI from the previously published papers, and test the hypothesis that non-experts seeing patients with hip pain could be trained against the reference standard of an expert radiologist. Our results support the hypothesis that agreement between expert and non-expert readers can be acceptable, and furthermore, the non-expert medical student in this study also demonstrated good intra-rater reproducibility (kappa 0.72, PABAK 0.76).
We used one trained reader, which may limit the generalizability of the findings to other observers. However, we chose a 3rd year medical student to conservatively approximate the MSK readers who might be involved in the diagnosis of FAI patients, since he did not have clinical or radiographic experience in hip pain and FAI. We feel that experienced MSK clinicians familiar with both would likely perform as well or better[16].
We are not aware of another study evaluating the validity of a non-radiologist in evaluating radiographic features of FAI. One study [19] looked at validity of varying x-ray views for the alpha angle (by two readers, job title and training not specified) in comparison to multiplanar MRI (read by an experienced MSK radiologist) and found that the Dunn view had the best validity, supporting radiographs as an adequate substitute to MRI in the evaluation of cam FAI.
We found only one study that reported intra-rater reliability finding for the alpha angle from the Dunn view, and it was reported at 0.98 [19] from the readings of an experienced MSK radiologist. Our findings for intra-rater ICC’s for the alpha angle were lower (0.87) but acceptable, and may reflect the difference between a 3rd year medical student and experienced radiologist. The intra-rater ICC for LCEA was 0.97, consistent with previous studies [16,20]. The intra-rater kappa for the crossover test has been reported at 0.69 [18], 0.73 [20] and Mast et al. [16] reported an adjusted kappa of 0.95. Ours was lower (0.58) likely for similar reasons that affected validity of the crossover sign (discussed above).
Conclusions
Knowledge that MSK clinicians seeing hip pain can accurately identify FAI on plain films, despite the subtlety of the findings, could shorten the current 1–2 year delay in diagnosis.
Key Points.
Findings: A non-radiologist demonstrated good validity (sensitivity 0.83, specificity 0.87) and reliability (PABAK 0.76) for a radiographic diagnosis of FAI.
Implications: MSK clinicians seeing hip pain can, with minimal training, accurately identify FAI on plain films, despite the subtlety of the findings. This knowledge could contribute to changes in practice shortening the current 1–2 year delay in diagnosis. The study also raises awareness about the importance of the optimal radiographic projections for cam FAI (Dunn view) and pincer FAI (AP pelvis).
Caution: There was only one non-radiologist reader, a 3rd year medical student and not an experienced MSK clinician. This may limit external validity, though an experienced MSK clinician is likely to perform equally as well or better.
Acknowledgments
The protocol for this study was approved by the Clinical Research Ethics Board at the University of British Columbia. This study was supported by the Canadian Institutes of Health Research (107513).
Footnotes
Conflict of Interest None
References
- 1.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Nicholls AS, Kiran A, Pollard TC, Hart DJ, Arden CP, Spector T, Gill HS, Murray DW, Carr AJ, Arden NK. The association between hip morphology parameters and nineteen-year risk of end-stage osteoarthritis of the hip: a nested case-control study. Arthritis Rheum. 2011;63(11):3392–3400. doi: 10.1002/art.30523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung KA, Restrepo C, Hellman M, Abdelsalam H, Parvizi J, Morrison W. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93(10):1303–1307. doi: 10.1302/0301-620X.93B10.26433. [DOI] [PubMed] [Google Scholar]
- 4.Ochoa LM, Dawson L, Patzkowski JC, Hsu JR. Radiographic Prevalence of Femoroacetabular Impingement in a Young Population with Hip Complaints Is High. Clin Orthop Relat Res. 2010;468(10):2710–2714. doi: 10.1007/s11999-010-1233-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92(5):1162–1169. doi: 10.2106/JBJS.H.01674. 92/5/1162 [pii] [DOI] [PubMed] [Google Scholar]
- 6.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638–644. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1041–1047. doi: 10.1007/s00167-007-0348-2. [DOI] [PubMed] [Google Scholar]
- 8.Carlisle JC, Zebala LP, Shia DS, Hunt D, Morgan PM, Prather H, Wright RW, Steger-May K, Clohisy JC. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52–58. [PMC free article] [PubMed] [Google Scholar]
- 9.Jaberi FM, Parvizi J. Hip pain in young adults: femoroacetabular impingement. J Arthroplasty. 2007;22(7 Suppl 3):37–42. doi: 10.1016/j.arth.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 10.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188(6):1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 11.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 12.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: With special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(suppl 58):1–135. [Google Scholar]
- 13.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81(2):281–288. doi: 10.1302/0301-620x.81b2.8291. [DOI] [PubMed] [Google Scholar]
- 14.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(4):556–560. doi: 10.1302/0301-620x.84b4.12014. [DOI] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 16.Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469(1):188–199. doi: 10.1007/s11999-010-1447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas GE, Hart DA, Spector T, Glyn-Jones S, et al. The association between hip morphology and end-stage osteoarthritis at 12-year follow up. Osteoarthritis Cartilage. 2012;20(Supp 1):S204. [Google Scholar]
- 18.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25(6):758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 19.Barton C, Salineros MJ, Rakhra KS, Beaule PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469(2):464–469. doi: 10.1007/s11999-010-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26(9):1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]