Summary
Osteoporotic fractures are associated with a significant increase in morbidity, mortality and medical costs. There is also a strong link between fractures and increased mortality. Among effective measures for the prevention of falls, instability treatment surely plays a crucial role. Several factors contribute to instability, many of which are ageing-related: visual spatial deficit, strength reduction, weight imbalance with COP lateralization sometimes favoured by LLD (leg length discrepancy). It seems useful to detect an heterometry which could be corrected, if present. The aim of our work is to assess the responses of individuals with heterometry diagnosis to the wedge positioning, using the balance board Lizard 3.0®. In the period between January 2013 and September 2013, 52 patients were recruited with clinical heterometry >5 mm among those that were treated in the Recovery and Rehabilitation Agency’s postural clinic of the Careggi Hospital Orthopedic Trauma Centre in Florence. Our measurements have revealed that there is a statistically significant correlation (p<0.5) between clinical limb shortening expressed in mm and location of the weight imbalance at the stabilometric examination at T0; our data shows that the majority of patients with clinical heterometry shows a weight imbalance on the longer limb. After heterometry correction, 21 patients showed a statistically significant reduction (p<0,01) in weight imbalance expressed in kg between T0 and T1 and have been assigned to group 1, the remaining 31 worsened and have been assigned to group 2. From the results of our study, it is clear that the correction of lower limbs heterometry shouldn’t be based only on clinical measuring of the limbs length discrepancy, even if very accurate.
Keywords: osteoporosis fractures, fall prevention, stabilometry
Introduction
Osteoporosis is one of the most common skeletal system pathology. World Health Organization (WHO) has described it as a bone metabolism disorder characterized by a bone mass reduction and a structural deterioration which leads to an increase in bones fragility and a consequent increased risk of fractures. Currently the gold standard among diagnostic tools is the BMD (bone mineral density) measured on lumbar spine and hip. BMD with T score ≤−2.5 SD (standard deviation) are considered suggestive of osteoporosis. Some Authors consider a low-energy trauma fracture to be sufficient for osteoporosis diagnosis, even with a T score >−2.5 SD. WHO has quantified low-energy trauma as forces equivalent to a fall from a standing height or less. It is estimated that approximately 50% of women and 20% of men will face an osteoporotic fracture (1). Osteoporotic fractures are associated with a significant increase in morbidity, mortality and medical costs. There is also a strong link between fractures and increased mortality (2). The two main causes of fractures are therefore low BMD and falls (3–6).
Among effective measures for the prevention of falls, instability treatment surely plays a crucial role. Several factors contribute to instability, many of which are ageing-related: visual spatial deficit (7), strength reduction, weight imbalance with COP lateralization (8) sometimes favoured by LLD (leg length discrepancy). Balance will be more precarious the more the COP will be projected to the edges of the base of support. A precious standing balance assessment tool is the balance board which also allows to quantify this COP displacement and the effectiveness of potential corrective actions (9).
It is therefore useful to detect an heterometry which could be corrected, if present. Lower limbs heterometry is a difficult and contrasting subject with several unclear aspects, also in literature (10–13). In fact a standardized measurement method, agreed on a global scale, doesn’t exist yet; not even treatment indications. The literature reports the distinction between “true” and “false” heterometry (14).
True heterometry is a real shortening of bone segments due to various causes; while false heterometry is a functional shortening caused by limb compensation. True heterometry can be congenital or acquired and it often implicates a number of postural compensations. Congenital heterometry may be due to a different growth of both limbs. Acquired heterometry is often caused by a traumatic event (e.g. outcome of a fracture) or by a surgery (e.g. hip replacement surgery). Even if real, heterometry is not always easily identified because the pelvis and the spinal column could bring in some compensating actions. False heterometry of lower limbs is the most common case. It can be caused by various conditions, such as abnormal pelvic ossification, pelvic bone tilt, muscle retraction of the psoas, pelvic rotation, lumbar scoliosis, piriformis syndrome, calcaneal valgus, knee valgus. Current literature agrees with the potential effects of lower limbs heterometry on global posture (15), but it is controversial on the diagnosis. Measurements can be carried out in different ways (16, 17). Some Authors divide measurement methods in direct and indirect methods.
Direct methods include measuring with tape the distance between SIAS (or navel) and medial malleolus (spina-malleolar distance) and spirit level measurement with patient in anterior bending. Indirect methods are palpation of the iliac crests and iliac spines in orthostatic position or difference of ankle bones height in clinostatic position.
For many Authors (i.e. Fisk and Baigent) the most accurate measurement is radiography measurement (18).
Pelvic and lower limbs radiography will have to be done under load in anteroposterior projection. According to Fisk and Baigent, 30% of clinical measurements differ from radiography measurements. However, not even radiographic study is free of errors, caused by the patient malposition during the exam. Limitations are an inherent inaccuracy in patients with hip or knee flexion contracture and the technique is subject to a magnification error. Other problems are electromagnetic radiation exposure, especially during developmental age, and the exam cost.
As can be easily imagined, a wrong diagnosis can lead to errors in prescribing possible remedies. The correction of a false dysmetria could be totally useless or, in the worst of cases, even harmful (19). Not all patients with lower limbs heterometry develop overload painful symptoms, it is therefore conceivable that not all heterometry need treatment. In current literature the standard treatment consist of locating a wedge on the shorter leg side. Some Authors (14) consider to be significative, and therefore treatable, heterometry above 12 mm, some others the ones above 2 cm.
In literature a surgical treatment is recommended for significative heterometry (≥3 cm) (Ilizarov system, 1969). However, prior to undertaking any corrective treatment, it is fundamental to be sure of the differential diagnosis between true and false heterometry.
According to us it is not heterometry in itself that has to be treated, but the possible weight imbalance that could ensue, also assessing the individual response to the wedge positioning.
Aim of the study
The aim of our work is to assess the responses of individuals with heterometry diagnosis to the wedge positioning, using the balance board Lizard 3.0®.
Materials and methods
In the period between January 2013 and September 2013, 52 patients were recruited (22M, 30F), average age 38,02 (range 10–89), with clinical heterometry >5mm among those that were treated in the Recovery and Rehabilitation Agency’s postural clinic of the Careggi Hospital Orthopedic Trauma Centre in Florence. 25 patients showed (48.07%) a right clinical shortening and 27 a left clinical shortening (51.92%).
Clinical measurements
After an accurate examination of the patient’s history and physical state, the patients have been clinically assessed for any lower limbs heterometry.
Initially the difference in height between iliac crests has been measured in orthostatic position and anterior bending, using the spirit level and the rule.
The plantar stance and rearfoot axis have been measured on the podoscope, also in orthostatic position.
Subsequently the spina-malleolar distance measurement of the two limbs has been compared in clinostatic position, with the centimetric tape, from the anterior superior iliac spine to the medial malleolus.
Stabilometry
The patient has been positioned on a balance board Lizard 3.01. type. The board consists of two separated platforms for the bipodal support and it is provided with piezoelectric transducers which are able to assess the vertical component of the forces exerted upon the platform, therefore allowing to identify the body centre of pressure (CoP) on the supporting surface.
Using the balance board it is possible to graphically and numerically measure the body barycentre projection and its fluctuations. The CoP represents the point where the resultant of the forces exchanged between the foot and the ground applies; that is to say the barycentre of the support reactions to the ground applied to every point of the foot surface touching the support base.
The balance board interfaces with a computer using the software Lizard® which elaborates the measurements. In order to obtain some reproducible data, it was necessary to standardize the patient positioning, using anatomical reference marks (calcaneal bisection, lateral malleolus, second metatarsal) corresponding to the same amount of points on the board surface.
Patients were instructed to maintain a natural position during the examination, with arms straight along sides. The registration is always carried out in the same way: patient without shoes, with open eyes, quiet environment, duration 51.2 sec. During the first registration (T0) the patient is assessed in basal conditions. In case of weight imbalance, the exam would be repeated after heterometry correction by locating a wedge under the hypometric limb heel (T1). This wedge consists of 0.5 cm and 1 cm plywood spacers.
The graphic elaboration is completed by the displaying of the variations in position of the general barycentre and feet. In ideal conditions the load should be symmetrically distributed between the two limbs.
Results
In the period between January 2013 and September 2013, 52 patients with clinical heterometry >5 mm were included in the study (22M, 30F), average age 38,02 (range 10–89). 25 patients showed (48.07%) a right clinical shortening and 27 a left clinical shortening (51.92%). The clinical shortening was 6.41 mm on average (range 5–15 mm). Heterometry level measurements performed with the spirit level and the rule, compared to those performed with the centimetric tape were found to be homogeneous with Chi-Square (Χ2) < 0.05 (0.032) and a statistical error of 2.25 mm.
Regarding the location of weight imbalance correlated with the clinical shortening, in T0 we found that among the 25 patients with right clinical shortening, 9 (36%) showed a weight imbalance on the ipsilateral limb and 16 (64%) on the contralateral one. Whereas, among the 27 patients with left clinical shortening, 7 (25.93%) showed weight imbalance on the ipsilateral limb and 20 (74.07%) on the contralateral one. Our measurements have revealed that there is a statistically significant correlation (p<0.5) between clinical limb shortening expressed in mm and location of the weight imbalance at the stabilometric examination at T0; our data shows that the majority of patients with clinical heterometry shows a weight imbalance on the longer limb.
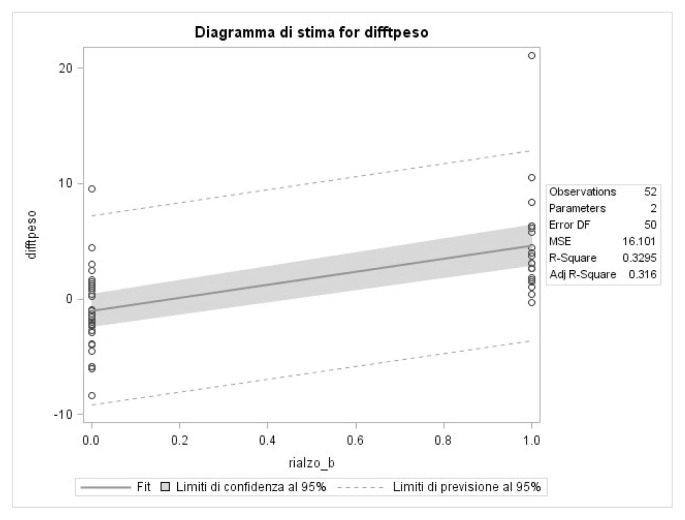
After heterometry correction, 21 patients showed a statistically significant reduction (p<0,01) in weight imbalance expressed in kg between T0 and T1 and have been assigned to group 1, the remaining 31 worsened and have been assigned to group 2 (Figure 1). The average of weight imbalance in kg at T0 in group 1 was 6,53 kg (range 1,8–21,6 kg). The average of weight imbalance in kg at T1 in group 1 was 1,30 kg (range 0,1–6,4 kg). The average of weight imbalance in kg at T0 in group 2 was 3,40 kg (range 0,2–11,7 kg). The average of weight imbalance in kg at T1 in group 2 was 4,42 kg (range 0,3–11,4 kg). The statistical correlations between T0 measurements and T1 measurements have been carried out solely in group 1.
Figure 1.
Statistically significant reduction (p<0,01) in weight imbalance between T0 and T1.
Discussion
Lower limbs heterometry treatment is still a controversial subject, both for the diagnostic approach (18, 20) and for the conservative treatment. The existing literature suggests to use the wedge based on clinically evaluated heterometry level, but there isn’t an agreed reference value on the wedge positioning (3 mm–22 mm) (19).
In our study we used a clinical and instrumental approach (balance board) which showed that lower limbs heterometry correction does not always require a wedge and that a reference value does not exist.
The first difficulty in the diagnostic process concerns the distinction between true and false heterometry, these latter deriving from compensations such as, for example, pelvic rotation or valgus knees.
Another controversial issue is the measurement of the heterometry real level and the most appropriate instruments. In our study we included only patients with real heterometry and we compared two measuring methods of lower limbs heterometry level: spirit level and rule versus centimetric tape measuring. From our measurements, the two methods were found to be pretty similar with a statistical error of 2,15 mm.
Our study confirms literature data (13) regarding the positive association between shortening location and weight imbalance location. Our study shows, indeed, a statistically significant correlation: weight imbalance is mostly on the longer limb side. The balance board used in our study allows to achieve some parameters not assessable with a clinical examination, such as weight imbalance expressed in kg in basal conditions (T0) and after heterometry correction (T1). It seems logical to think that high values of weight imbalance could lead to an overloading of some musculoskeletal structures involved in maintaining a standing position.
The postural examination using the balance board, therefore constitutes a tool supporting the clinical decision whether to correct an heterometry or not.
In consideration of the board results, it has been decided to correct heterometry with a wedge only in 21 (group 1) of the 52 patients recruited, since they showed a statistically significant reduction of weight imbalance between T0 and T1. The above mentioned wedge, non compressible, made with cork, leather or plastic, will be placed inside the shoe.
It was not prescribed a wedge to the remaining 31 patients (group 2) since the wedge positioning determined a weight imbalance worsening.
Osteoporosis is one of the most common skeletal system pathology. WHO has quantified low-energy trauma as forces equivalent to a fall from a standing height or less. The balance board allows to assess weight imbalance following the displacement of the real barycentre from the ideal one, causing an higher postural instability, less balance and an increased risk of falls. Correcting this imbalance, in a frail patient, may result in a reduced risk of falls and, consequently, in a reduced risk of fractures.
Conclusions
From the results of our study, it is clear that the correction of lower limbs heterometry should not be based only on clinical measuring of the limbs length discrepancy, even if very accurate. Each patient, indeed, has to be assessed considering also other parameters, outlining the patient in his entirety.
The balance board appears to be a reliable tool, easy to use and that allows to collect numerical data which can be evaluated over time.
After the wedge prescription, serial checks should follow to ascertain the benefit stability in terms of weight imbalance.
References
- 1.Kanis JA, McCloskey EV, Johanson H, et al. European guidance for the diagnosis and management of the osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23–57. doi: 10.1007/s00198-012-2074-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanis JA, Oden A, Johnell O, et al. The components of excess mortality after hip fracture. Bone. 2003;32:468–473. doi: 10.1016/s8756-3282(03)00061-9. [DOI] [PubMed] [Google Scholar]
- 3.Gill T, Taylor AW, Pengelly A. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology. 2005 Sep-Oct;51(5):340–5. doi: 10.1159/000086372. [DOI] [PubMed] [Google Scholar]
- 4.Moylan KC, Binder EF. Falls in older adults: risk assessment, management and prevention. Am J Med. 2007;120(6):493.e1–6. doi: 10.1016/j.amjmed.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 5.Kannus P, Sievänen H, Palvanen M, et al. Prevention of falls and consequent injuries in elderly people. Lancet. 2005 Nov 26;366(9500):1885–93. doi: 10.1016/S0140-6736(05)67604-0. [DOI] [PubMed] [Google Scholar]
- 6.McClure R, Turner C, Peel N, et al. Population-based interventions for the prevention of fall-related injuries in older people. Cochrane Database Syst Rev. 2005 Jan 25;(1):CD004441. doi: 10.1002/14651858.CD004441.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kulmala J, Viljanen A, Sipilä S, et al. Poor vision accompanied with other sensory impairments as a predictor of falls in older women. Age Ageing. 2009 Mar;38(2):162–7. doi: 10.1093/ageing/afn228. [DOI] [PubMed] [Google Scholar]
- 8.Miko I, Szerb I, Szerb A, Poor G. Effectiveness of balance training programme in reducing the frequency of falling in established osteoporotic women: A randomized controlled trial. Clin Rehabil. 2016 Jan 29; doi: 10.1177/0269215516628616. pii: 0269215516628616. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Cultrera P, Pratelli E, Petrai V, Postiglione M, Zambelan G, Pasquetti P. Evaluation with stabilometric platform of balance disorders in osteoporosis patients. A proposal for a diagnostic protocol. Clin Cases Miner Bone Metab. 2010 May;7(2):123–5. [PMC free article] [PubMed] [Google Scholar]
- 10.Blustein SM, D’Amico JC. Limb Lenght discrepancy. Identification, clinical and menagement. I am Podoiatric Med Assoc. 1985;75(4):200–206. doi: 10.7547/87507315-75-4-200. [DOI] [PubMed] [Google Scholar]
- 11.Clarke GR. Unequal leg length: an accurate method of detection and some clinical results. Rheum Phys Med. 1972;11:385–390. doi: 10.1093/rheumatology/11.8.385. [DOI] [PubMed] [Google Scholar]
- 12.Danbert RJ. Clinical assessment and treatment of leg length inequalities. J Manipulative Physiol Ther. 1988;11(4):290–295. [PubMed] [Google Scholar]
- 13.Mahar RK, Kirby RL. Simulated leg-lenght discrepancy: its effect on mean center of pressure position and postural sway. Arch Phys Med Rehabil. 1985;66 [PubMed] [Google Scholar]
- 14.Gofton JP, Trueman GE. Studies in osteoarthritis of the hip. II. Osteoarthritis of the hip and leg-length disparity. Can Med Assoc. 1971;104(9):791–799. [PMC free article] [PubMed] [Google Scholar]
- 15.Rothenberg RJ. Rheumatic disease aspects of leg length Inequality. Seminars in arthritis and rheumatism. 1988;17(3):196–205. doi: 10.1016/0049-0172(88)90020-0. [DOI] [PubMed] [Google Scholar]
- 16.Mann M, Glasheen-Wray M, Nyberg R. Therapist agreement for palpation and observation of iliac crest heights. Phys ther. 1984;64(3):334–338. doi: 10.1093/ptj/64.3.334. [DOI] [PubMed] [Google Scholar]
- 17.Sanjeev Sabharwal MD, Ajay Kumar MD. Methods for Assessing Leg Length Discrepancy. Clin orthop relat res. 2008;466:2910–2922. doi: 10.1007/s11999-008-0524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fisk JW, Baigent ML. Clinical and radiological assessment of leg length. N Z Med J. 1975 May 28;81(540):477–80. [PubMed] [Google Scholar]
- 19.Brady RJ, Dean JB, Skinner TM, Gross MT. Limb length Inequality: clinical implications of assessment and intervention. J Orthop Sports Phys Ther. 2003;33(5):221–34. doi: 10.2519/jospt.2003.33.5.221. [DOI] [PubMed] [Google Scholar]
- 20.Woerman A, Binder-Macleod S. Leg length discrepancy assessment: accuracy and precision in five clinical in five clinical methods of evaluation. J Orthop Sports Phys Ther. 1984;5:230–239. doi: 10.2519/jospt.1984.5.5.230. [DOI] [PubMed] [Google Scholar]