Summary
Introduction
The nonunion rate has been reported between 0.1% and 15%. There are also several predisposing factors for the onset of complications: general factors connected with the patient and specific factors related to the fracture site. The purpose of our study is to review the etiology of nonunion of the clavicle in its atrophic form and investigate the outcomes of the revision treatment in a single step.
Materials and methods
Retrospective study on 71 patients suffering from nonunions due to the following treatments: conservative in 13 patients; plate fixation in 12; closed reduction and fixation with K-wire in 24; open reduction and fixation with K-wire. All patients were operated on in beach chair position and classic approach to the clavicle by incising the previous surgical scar. The clinical and radiographic criteria for evaluating the outcomes were: the Short Form (12) Health Survey (SF-12), the Constant Shoulder Score (CSS) and the Disability Disabilities of the Arm, Shoulder and Score (DASH) and radiographic Union Score (RUS) for bone healing. The evaluation endpoint was set at 12 months.
Results
Blood and culture tests showed 22 infected nonunions and 49 atrophic or oligoatrophic. In only 10 cases, before surgery, the inflammatory markers were positive. The isolated microorganisms were resistant to common antibiotics. In 70 out of 71 cases, plates and screws on the upper side and fibula allogenic splints at the bottom, associated with cancellous bone grafts taken from the patients’ iliac crests, were implanted. In one case, however, it was decided to implant the plate on the front edge of the clavicle and the fibula allogeneic splint on the posterior margin, also associated with a cancellous bone graft taken from the patient’s iliac crest. The radiographic bone healing was observed in 107.8 (range 82–160) days for the aseptic nonunions, while in 118.4 (range 82–203) days for the septic ones. The non-healing case was a serious failure that led to asubtotal excision of the clavicle.
Conclusions
The importance of classification and study of nonunions are essential to achieve positive outcomes. The guiding principle of our work is that aseptic nonunions heal in the operating room, while infected nonunions can be challenged and defeated on the operating table. Restoring the correct length of the clavicle interconnection between the sternum and the shoulder cingulum is indispensable to avoid functional deficits of the upper limb. The fibula splint and the tricorticale bone graft have both mechanical and strong biological values to quickly heal the nonunion. The return to pre-injury quality of life has to be our main goal.
Keywords: clavicle non union, bone allograft, outcomes, infection, biomechanical
Introduction
The fracture of the clavicle is a common injury due to its subcutaneous and relatively anterior position. Fractures affecting the middle third account for the majority of all clavicular fractures. Both non-operative and surgical methods have been described for the management of this injury. However, there is no unanimous consensus on the definite choice of treatment (1). Early primary fixation of comminuted shaft clavicular fractures results in improved patient-oriented outcomes, improved surgeon-oriented outcomes, earlier return to function and decreased rates of nonunion and malunion (2). Both plate fixation and intramedullary fixation are the most commonly used surgical treatment options for mid-shaft clavicle fractures; the latter method has shown better performance in some studies (3). The nonunion rate has been reported to be between 0.1 and 15%. There are also various predisposing factors for the onset of these complications: general factors linked to the patient (smoking, alcohol, diabetes, etc.) and the site of fracture (severe initial trauma, marked initial displacement and shortening, soft tissue interposition, primary open reduction and internal fixation, refracture, open fracture, polytrauma, and inadequate initial immobilization) (4). In the recent literature, the direct correlation between nonunions and infections is described (5). The aim of this study is to review the etiology of atrophic clavicle nonunions and to investigate the outcomes of a treatment with a single stage revision.
Materials and methods
This is a retrospective study: 71 middle clavicle shaft nonunions were treated.
The average age of the study population was 42.3 (range 16–82); the sex ratio was 1.84 in favor of males (Table 1). All previous fractures were classified according to Robinson Classification (6) (Table 1). All fractures were closed. Previous midshaft clavicle fractures were treated by: Conservative in 13 patients; Plate Fixation in 12; Closed Reduction and K Wire Fixation in 24; Open Reduction and K Wire Fixation in 22 (Table 1).
Table 1.
Description of clavicular shaft non unions.
| Number of patients | 71 |
| Average age (years) | 42.3 |
| Range of age (years) | 16–82 |
| Gender (M:F) | 46:25 |
| Male/Female ratio | 1.84 |
| Type of fracture according Robinson Classification (%) | IIA2: 4 (5.63%) IIB: 22 (30.99%) IIB1: 25 (35.21%) IIB2:20 (28.17%) |
| Orthopedic device used and type of reduction in the surgery for the osteosynthesis of the first middle clavicular schaft fracture | Conservative Treatment: 13 (18.31%) Plate Fixation: 12 (16.90%) Closed K Wire Fixation: 24 (33.80%) Open K Wire Fixation: 22 (30.99%) |
| Results of reduction and osteosynthesis | Bad: 29 (40.84%) Sufficient: 22 (30.99%) Good: 15 (21.13%) Excellent: 5 (7.04%) |
| Type of Non Union according Weber-Cech classification | Oligotrophic: 22 (13.64%) Atrophic or Avascular: 49 (86.36%) |
| Average Point of Non Union Scoring System | 63.8 |
| Range of of Non Union Scoring System | 31–82 |
After the first 7 days, the reduction and osteosynthesis outcomes were: Bad in 29 (40.84%); Sufficient in 22 (30.99%); Good 15 (21:13%); Excellent in 5 (7:04%) (Table 1).
Oligotrophic nonunions in 22 (30.99%), and Atrophic or Avascular nonunions were present in 49 cases (69.01%) according to the Weber-Cech classification (7) (Table 1).
Retrospectively, the Non-Union Scoring System (NUSS) (8) was used to understand and study the type of nonunion. To assess the NUSS, information from the medical case history was used.
The comorbidity index was reported in Table 2. 33 (46.48%) out of 71 patients had one comorbidity Table 2.
Table 2.
Comorbidity in 71 patients.
| No Patients (%) | |
|---|---|
| Comorbidity | 106 (100%) |
| Cardiovascular disease | 16 (15.09%) |
| Respiratory disease | 13 (12.26%) |
| Renal disease | 8 (7.55%) |
| Diabetes | 10 (9.44%) |
| Miscellanea allergies | 4 (3.77%) |
| Antibiotics drugs allergies | 3 (2.83%) |
| Rheumatoid disease | 2 (1.89%) |
| Intensive therapy | 13 (12.26%) |
| Gastroenterla diseases | 2 (1.89%) |
| Transplant | 2 (1.89%) |
| HIV | 1 (0.94%) |
| Current smokers | 30 (28.30) |
| Enteral steroids | 2 (1,89%) |
| No of patients with comorbidities: | |
| 0 | 12 (16.90%) |
| 1 | 33 (46.48%) |
| 2 | 15 (21.13%) |
| ≥3 | 11 (15.49%) |
The average point of the Non-Union Scoring System was 63.8 (range 31–82).
The average time from the first to the second surgery was 1.8 (range 1–3) years (Table 1).
Preoperative values of inflammatory markers were taken on all patients: erythrocyte sedimentation rate (ESR), C Reactive Protein (CRP) and White Blood Cell Count (WBC).
All patients were operated on in the beach chair position and the classic approach to the clavicle by incising the previous surgical scar, treated with ORIF. In 70 out of 71 cases, plates and screws on the upper side and fibula allogenic splints at the bottom, associated with cancellous bone grafts taken from the patients’ iliac crests, were implanted. In one case, however, it was decided to implant the plate on the front edge of the clavicle and the fibula allogeneic splint on the posterior margin, also associated with a cancellous bone graft taken from the patient’s iliac crest.
All nonunion outbreaks were first removed and blooded and then sent for anatomic pathology examination and the laboratory for microbiological culture.
All patients received illustrated exhaustive descriptions of the type of treatment and asked to decide which treatment they preferred. Patients were treated according to Helsinki Declaration of ethical standards and were asked to read and understand the patient information sheet and sign the informed consent form.
All patients received the same physical therapy protocol: the first 4 weeks, arm-support protection; from the fifth week, Codman pendulum; from the eighth week, active and passive exercises against gravity; from the tenth week, active and passive exercises against progressive resistance.
The chosen criteria to evaluate these 71 patients during clinical and radiological follow-ups were the quality of life measured by The Short Form (12) Health Survey (SF-12) (9), the clavicle function measured by the Constant Shoulder Score (CSS) (10), while general health status, pain, and cosmetic outcomes related to was measured by the Disability Disabilities of the Arm, Shoulder and Score (DASH) (10), bone healing measured by the modified Radiographic Union Score (RUS) (11) by only XR projections, and postoperative complications. Follow-ups were performed with clinical and radiographic controls at 15 days, 1 month, 3 months, 6 months, and 12 months and annually thereafter.
The evaluation endpoint was at 12 months.
Exclusion criteria included refractures caused by hematological or oncological pathologies, trauma, open fracture, and patients who did not adhere to a minimum follow-up of 12 months.
Results
Patients who during the visit received a nonunion diagnosis reported as predominant symptoms: pain in 34 cases; functional limitation in 7 cases; redness of the skin in 18 cases; in 12 cases feeling of mobilization of the means of synthesis. The other 37 cases were occasionally found during X-rays.
From ESR, CPR and WBC blood tests, 10 patients had values of the inflammatory markers of a possible infection. Blood culture results were the following: 3 patients were positive to Staphylococcus epidermidis (only sensitive to fluoroquinolones), 2 cases to E. coli sp. (Sensitive to carbapenem), 4 cases to Staphylococcus aureus (methicillin resistant, sensitive to teiclopanin), while 1 case was not positive. All patients received the most appropriate antibiotic treatment for the specific bacteria, while the patient who didn’t test positive was treated, instead, with a broad-spectrum therapy and the results of intra operating samples were negative to infection. Of these patients (7 males and 3 females), 6 were treated her with a plate, 2 with Open Reduction and K Wire and 2 with Closed Reduction and K Wire.
Excluding the patients treated conservatively, 12 additional cases of infection were found from samples taken during the second operation. 7 identified between the muscle fascia and the bone without signs of bone involvement and 5 were in open infected nonunions.
The 7 patients: 5 were Propionibacterium positive acnes (clindamycin-resistant and trimethoprim-sensitive), while 2 patients were Staphylococcus aureus positive (methicillin-resistant, vancomycin-sensitive).
The other 5 patients were positive in 1 case the Propionibacterium acnes (resistant to clindamycin and sensitive to trimethoprim), 2 cases of E. Coli (sensitive to Fluoroquinolones) and 1 case of Candida lusitaniae (sensitive to Itraconazole) in diabetic patients and 1 Staphylococcus epidermidis (only sensitive to Fluoroquinolones). Of the 12 infected patients (6 males and 6 females), 5 had been treated with a plates and screws, 4 with Open Reduction and K Wire and 2 with Closed Reduction and K Wire.
The 22 infected patients were classified according to the Cierny-Mader Classification (12), from which emerged that 10 cases belonged to the Class A and 12 to Class B. At this stage, 8 patients to Class I; 12 patients to Class II; 2 Patients with class III.
All infected patients had first received an empiric therapy with broad-spectrum antibiotics and then a specific therapy, once the microbiological examination was received. All patients after the removal of the focus of the infected nonunion and release and surgical debridement of soft tissue, the plate and screws were implanted at the top and the allogeneic fibula splint at the bottom, associated with an autologous cancellous iliac crest bone graft.
The remaining 49 cases of nonunion were due to mechanical failure of the means of synthesis (Figures 1, 2). In these 49 cases one aneurysm of the subclavian artery was found. In this case, an anterior plate and the posterior grafting of the fibula were implanted.
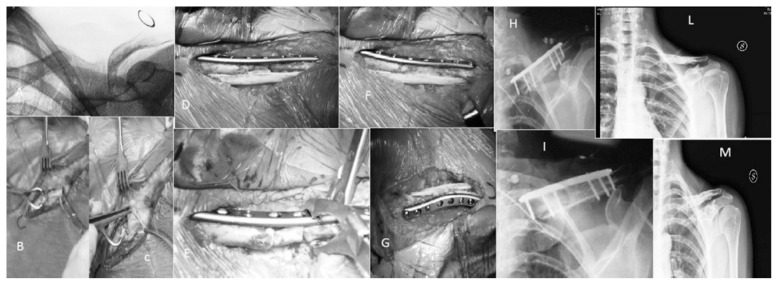
Figure 1.
A 41-year-old woman, 19 years before the fall from the horse, in which she suffered the fracture of the left clavicle, treated with Open reduction and K wire. Wire removal after three months; then abandoned (asymptomatic). After 19 years (A), onset of paresthesia on left upper limb. B, C report the blooding of the aseptic nonunion outbreak. D, E report the synthesis with the upper plate and the lower fibular allograft without iliac crest autogenous bone grafting. F and G (taken from above) highlight the from the iliac crest autogenous grafting. The X-rays (H, I) at 6 months after surgery showed integration of the fibula and bone consolidation. The X-rays (L, M) at 1 year from the removal of the means of synthesis, 18 months after surgery, show the perfect integration of bone grafts.
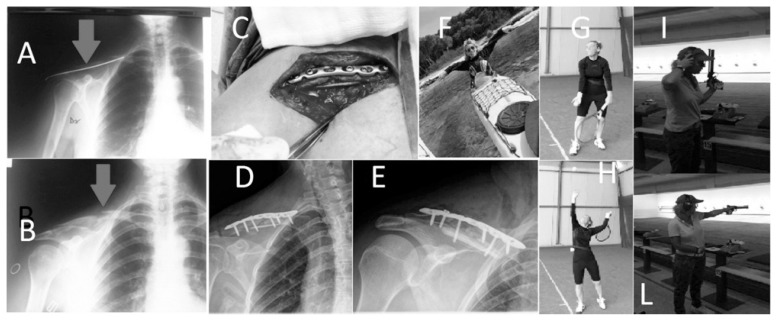
Figure 2.
Young sports woman, after a casual fall suffered the fracture of the right clavicle treated with Closed Reduction and K wire (A). K-wire removed after 6 months, showing outbreak of aseptic nonunion (B): osteosynthesis technique using plate and screws and cortical fibular allograft opposed inferiorly, and tricortical iliac crest autogenous grafting (C). X-rays (D, E) post operatively: functional recovery at 3 months after surgery (F–L).
All patients were asked if in the first three months after surgery had had infection complications in other organs or dental procedures. The results were: the dental procedures were the most common 25 (30.49%) of 82 complications; to follow: 19 urinary infections (23:17%) and in third place, 18 gastrointestinal infection (21.95%). There were no cases of infection of the surgical wound. For the complete index (Table 3).
Table 3.
Postoperative complications during the first 3 months after the surgery.
| No Patients (%) | |
|---|---|
| Complication | 82 (100%) |
| Chest infection | 3 (3.66%) |
| Skin infection | 2 (2.44%) |
| Upper airways infection | 15 (18.29%) |
| Urinary tract infection | 19 (23.17%) |
| Gastrointestinal infection | 18 (21.95%) |
| Wound infection | 0 (0%) |
| Dentestry surgery | 25 (30.49%) |
| No of patients with complications: | |
| 0 | 13 (18.31%) |
| 1 | 45 (63.38%) |
| 2 | 9 (12.68%) |
| ≥3 | 4 (5.63) |
In short, 63.38% of the patients, 45 of 71, had had a complication within the first 3 months from the initial treatment of the clavicle.
In the aseptic nonunion group, the XR bone healing occurred in about 107.8 (range 82–160) days after surgery.
In the infected nonunion group, the XR bone healing occurred in about 118.4 (range 82–203) days after surgery.
The Rus Score were the first year of follow-up (Figures 1, 2). Only one patient (IIIA Cierny-Mader) had a complication, a massive re-infection by Staphylococcus epidermidis, which forced the removal of the means of synthesis and the clavicle except the stump of the 3 lateral which was later merged with the acromion.
The quality of life measured by SF12 has shown that aseptic or septic nonunions do not create big problems in the quality of life. However, the subcategories which produced the worst scores were mainly psychological, since the female patients saw the nonunion as an aesthetic damage. In cases of infected nonunion, the patients lived in a state of deep anguish, because they felt that the infection could have led to death within a short time.
The pain was the most disabling component in CSS and DASH.
From the Functional point of view there was a marked hypo-validity of the affected limb found in both CSS and DASH in patients who had a shortening of the clavicle more than 15 mm.
Discussion
The diagnosis of atrophic, oligotrophic or infected nonunion may be occasional (13). In over half of our cases, in fact, there was an incidental finding.
Already in 1983, Wilkins and Johnston (13) said that a nonunion may be asymptomatic especially in its typology. In their study, only 3 of 11 patients who had atrophic nonunions were symptomatic enough to require surgery, in comparison with 16 of 22 patients who had hypertrophic nonunions. They noticed that the absence of callous in an atrophic nonunion can diminish the grating and crepitation that may be responsible for pain at the site of the nonunion. They suggested that patients with atrophic nonunions be followed for at least 6 months before scheduling surgery, since they believe that many patients will become asymptomatic during that time period (13).
In 2013, Sirvent-Díaz et al. (14) reported about 40 patients, mean age 35 years (18–64) with a non-surgically treated clavicle fracture with a minimum follow-up of 15 years (the mean follow-up was more than 22 years and range 15–32). They performed the clinical evaluation with the Disability of DASH, CSS and their conclusions were: the presence of comminution and/or the shortening of 15 mm or more had the worst functional and radiographic results. Despite this, non-surgical treatment showed excellent functional and radiographic results, and a high personal satisfaction.
Most likely the aesthetic problem is interconnected with the mobilization of the means of synthesis, the psychological state of the patients and to the sensation of pain.
In 1995, Olsen et al. (15) just showed that atrophic nonunions do not become asymptomatic. Disability may result from pain at the site of nonunion, altered shoulder mechanics (either in response to pain or due to malposition of the fracture fragments), “ptosis” of the shoulder, or a compression lesion involving the underlying brachial plexus or vascular structures.
Liu et al. (16) reported in their meta-analysis the comparison of the CS and DASH scores between operative and non-operative treatment for clavicle fracture. Five studies (17–21) reported the CS scores after the treatment of clavicle fracture and the results showed that the CS scores of the operational group were higher than those of the non-operative group. Four studies (18–21) reported the DASH scores and those of the operational group were shown to be lower than those of the non-operative group.
The same Authors also assert that the operative treatment could significantly reduce the nonunion rate (16).
Two recent papers (22, 23) reveal that the reduction of the length of the clavicle may reduce shoulder function measured with the DASH and CSS.
According to this meta-analysis (24), the risk of septic nonunion is high if internal fixation is used; the same is for deep infection.
This may help us understand why there were 22 infections and many of them had an advanced stadiation according to Cierny Mader.
The latest work by Gausden et al. (5) showed us how the nonunions of the clavicle are very often related to a latent infection and to saprophytic microorganisms of the surgical site (25). Also from the data collected by us we saw that many patients in the preoperative had a high number of comorbidities and postoperatively had dental treatment or infections of other systems that may have been the source of contamination (26–28).
Therefore it is useful, before proceeding to a surgery for a nonunion, to do a careful history and physical examination to discern what type of symptoms and disability, if any, the patient is experiencing.
Unfortunately, as we know from prosthetic surgery, ESR, CRP, and WBC are not very valid to find all true positives (29).
The cultural examination of the anatomical nonunion pieces removed and the surrounding tissues may give us many more true positives (5). Empirical antibiotic therapy with broad spectrum must always be started before surgery even when there is no clear sign of infection; it can modified or continued once the laboratory results are available (30).
Surgical treatment of infected, aseptic or oligotrophic nonunions of the clavicle should be the same, since we cannot afford to create bone gaps and shortening of the clavicle, therefore compromising the upper limb function (22, 23).
The clavicles are long bones, so in nonunions it may be used the metal plate against the splint bone technique (31).
The surgical technique must be precise and accurate, starting from the surgical access to expose the superior and anteroinferiorsite of the clavicle. Remove previous implants with minimal dissection and in atrophic or septic nonunions, remove and send the tissue for culture examination. Use drill to open the medullary canal.
Prepare on the table the cortical fibular allograft of a length shorter than 1/3 of the plate used. The 1/3 tubular plate or an anatomical plate for clavicle may be used (32). The plate should be placed on the upper surface of the clavicle and the contrasting allograft should be placed internally to optimize the biomechanical stability of the construct (33). The plate anteriorly, then posteriorly, the contrasting fibula should be placed only in re-operations to decrease the risk of vascular lesions (34), as it was done for the patient with aneurysm of the subclavian artery.
Finally, the construct must be completely coated with the reinsertion of the muscles.
Schnetzke et al. (35) have shown that an additional clavicle bone graft accelerates healing of non-unions and improves long-term results after 8.9 years of follow-up. Furthermore, the autologous bone grafting was performed to provide the length of the segment.
Once the pathogen is isolated, a specific therapy should be prescribed for a long time. Unfortunately cases of reinfection exist and can be so tragic that only life-saving surgery can be done.
From the data reported in our study, we can say that the treatment of aseptic or infected nonunion based on our method is reliability, feasibility and value. The importance of the classification and the study of the nonunion is critical to obtain good outcomes.
Infections can be challenged and defeated on the operating table.
Restoring the correct length of the interconnection between the sternum and the scapular cingulum is indispensable to avoid functional deficits to the upper limb. The fibular bone graft strut and the tri-cancellous bone graft from the iliac crest not only have a mechanical value, but also a strong biological value to quickly heal the nonunion. The return to pre fracture quality of life of the patients should be our goal.
Acknowledgments
Conflict of interest statement
All Authors disclose any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work. Examples of potential conflicts of interest include employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations, and grants or other funding.
Human and animal right
For this type of study is not required any statement relating to studies on humans and animals. All patients gave the informed consent prior being included into the study. All procedures involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
References
- 1.Naveen BM, Joshi GR, Harikrishnan B. Management of mid-shaft clavicular fractures: comparison between non-operative treatment and plate fixation in 60 patients. Strategies Trauma Limb Reconstr. 2017 doi: 10.1007/s11751-016-0272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhakad RK, Panwar M, Gupta S. Plating versus conservative treatment in mid shaft fractures of clavicle: A comparative study. J Clin Orthop Trauma. 2016;7(Suppl 2):166–170. doi: 10.1016/j.jcot.2015.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gao Y, Chen W, Liu YJ, Li X, Wang HL, Chen ZY. Plating versus intramedullary fixation for mid-shaft clavicle fractures: a systemic review and meta-analysis. Peer J. 2016;4:e1540. doi: 10.7717/peerj.1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones GL, McCluskey GM, 3rd, Curd DT. Nonunion of the fractured clavicle: evaluation, etiology, and treatment. J South Orthop Assoc. 2000;9(1):43–54. [PubMed] [Google Scholar]
- 5.Gausden EB, Villa J, Warner SJ, Redko M, Pearle A, Miller A, Henry M, Lorich DG, Helfet DL, Wellman DS. Nonunion after clavicle osteosynthesis: High incidence of Propionibacterium acnes. J Orthop Trauma. 2016 doi: 10.1097/BOT.0000000000000770. [DOI] [PubMed] [Google Scholar]
- 6.Robinson CM. Fracture clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1198;80(3):476–84. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 7.Salomone C, Burastero G, Rita A, Felli L, Biasibetti A. Nonunions in diaphyseal fractures. Lo Scalpello. 2015;29:44–48. doi: 10.100/s11639-015-0102-3. [DOI] [Google Scholar]
- 8.Calori GM, Colombo M, Mazza EL, Mazzola S, Malagoli E, Marelli N, Corradi A. Validation of the Non-Union Scoring System in 300 long bone non-unions. Injury. 2014;45(Suppl 6):S93–7. doi: 10.1016/j.injury.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 9.El Haj M, Khoury A, Mosheiff R, Liebergall M, Weil YA. Orthogonal Bouble Plate fixation for long bone fracture nonunion. Acta Chir Orthop Traumatol Cech. 2013;80(2):131–7. [PubMed] [Google Scholar]
- 10.Woltz S, Stegeman SA, Krijnen P, van Dijkman BA, van Thiel TP, Schep NW, de Rijcke PA, Frölke JP, Schipper IB. Plate Fixation Compared with Nonoperative Treatment for Displaced MidShaft Clavicular Fractures: A Multicenter Randomized Controlled Trial. J Bone Joint AM. 2017;99(2):106–112. doi: 10.2016/JBJS.15.01394. [DOI] [PubMed] [Google Scholar]
- 11.Maiettini D, Bisaccia M, Caraffa A, Rinonapoli G, Piscitelli L, Bisaccia O, Rollo G, Meccariello L, Ceccarini P, Rebonato A. Feasibility and Value of Radiographic Union Score Hip Fracture after Treatment with Intramedullary Nail of Stable Hip Fractures. Acta Inform Med. 2016;24(6):394–396. doi: 10.5455/aim.2016.24.394-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cierny G, 3rd, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Clinic Orthop Relat Res. 2003;(414):7–24. doi: 10.1097/01.blo.0000088564.81746.62. [DOI] [PubMed] [Google Scholar]
- 13.Wilkins RM, Johnston RM. Ununited fractures of the clavicle. J Bone Joint Surg Am. 1983;65:773–778. [PubMed] [Google Scholar]
- 14.Sirvent-Díaz E, Calmet-García J, Capdevila-Baulenes J. Functional and aesthetic results of orthopaedic treatment of midshaft fractures of the clavicle. A 22 years follow-up study. Rev Esp Cir Ortop Traumatol. 2014;58(2):108–13. doi: 10.1016/j.recot.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Olsen BS, Vaesel MT, Sojbjerg JO. Treatment of midshaft clavicular nonunion with plate fixation and autologous bone grafting. J Shoulder Elbow Surg. 1995;4:337–344. doi: 10.1016/s1058-2746(95)80017-4. [DOI] [PubMed] [Google Scholar]
- 16.Liu GD, Tong SL, Ou S, Zhou LS, Fei J, Nan GX, Gu JW. Operative versus non-operative treatment for clavicle fracture: a meta-analysis. Int Orthop. 2013 Aug;37(8):1495–500. doi: 10.1007/s00264-013-1871-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Böhme J, Bonk A, Bacher G, Wilharm A, Hoffmann R, Josten C. Current treatment concepts for mid-shaft fractures of the clavicle-results of a prospective multicentre study. Z Orthop Unfall. 2011;149(1):68–76. doi: 10.1055/s-0030-1250334. [DOI] [PubMed] [Google Scholar]
- 18.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 19.Jubel A, Andermahr J, Prokop A, Lee J, Schiffer G, Rehm K. Treatment of mid-clavicular fractures in adults. Early results after rucksack bandage or elastic stable intramedullary nailing. Unfallchirurg. 2005;108(9):707–714. doi: 10.1007/s00113-005-0970-8. [DOI] [PubMed] [Google Scholar]
- 20.Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23(2):106–112. doi: 10.1097/BOT.0b013e318190cf88. [DOI] [PubMed] [Google Scholar]
- 21.Virtanen KJ, Paavola MP, Remes VM, Pajarinen J, Savolainen V, Bjorkenheim JM. Nonoperative versus operative treatment of midshaft clavicle fractures: a randomized controlled trial. The 75th Annual Meeting of the American Academy of Orthopaedic Surgeons. 2010;9–12:65–73. [Google Scholar]
- 22.Figueiredo GS, Tamaoki MJ, Dragone B, Utino AY, Netto NA, Matsumoto MH, Matsunaga FT. Correlation of the degree of clavicle shortening after non-surgical treatment of midshaft fractures with upper limb function. BMC Musculoskelet Disord. 2015;16:151. doi: 10.1186/s12891-015-0585-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rasmussen JV, Jensen SL, Petersen JB, Falstie-Jensen T, Lausten G, Olsen BS. A retrospective study of the association between shortening of the clavicle after fracture and the clinical outcome in 136 patients. Injury. 2011;42(4):414–7. doi: 10.1016/j.injury.2010.11.061. [DOI] [PubMed] [Google Scholar]
- 24.Xiao H, Gao H, Zheng T, Zhao J, Tian Y. Plate fixation versus intramedullary fixation for midshaft clavicle fractures: Meta-analysis of complications and functional outcomes. J Int Med Res. 2016;44(2):201–15. doi: 10.1177/0300060515621638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ribeiro M, Monteiro FJ, Ferraz MP. Infection of orthopedic implants with emphasis on bacterial adhesion process and techniques used in studying bacterial-material interactions. Biomatter. 2012;2(4):176–94. doi: 10.4161/biom.22905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tigani D, Trisolino G, Fosco M, Ben Ayad R, Costigliola P. Two-stage reimplantation for periprosthetic knee infection: Influence of host health status and infecting microorganism. Knee. 2013;20(1):9–18. doi: 10.1016/j.knee.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Lockhart PB, Loven B, Brennan MT, Fox PC. The evidence base for the efficacy of antibiotic prophylaxis in dental practice. J Am Dent Assoc. 2007;138(4):458–74. doi: 10.14219/jada.archive.2007.0198. [DOI] [PubMed] [Google Scholar]
- 28.Ollivere BJ, Ellahee N, Logan K, Miller-Jones JC, Allen PW. Asymptomatic urinary tract colonization predisposes to superficial wound infection in elective orthopaedic surgery. Int Orthop J. 2009;33(3):847–50. doi: 10.1007/s00264-008-0573-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Falzarano G, Piscopo A, Grubor P, Rollo G, Medici A, Pipola V, Bisaccia M, Caraffa A, Barron EM, Nobile F, Cioffi R, Meccariello L. Use of Common Inflammatory Markers in the Long-Term Screening of Total Hip Arthroprosthesis Infections: Our Experience. Adv Orthop. 2017;2017:9679470. doi: 10.1155/2017/9679470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Korean Society for Chemotherapy; Korean Society of Infectious Diseases; Korean Orthopaedic Association. Clinical guidelines for the antimicrobial treatment of bone and joint infections in Korea. Infect Chemother. 2014;46(2):125–38. doi: 10.3947/ic.2014.46.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carta S, Fortina M, Riva A, Meccariello L, Manzi E, Di Giovanni A, Ferrata P. The Biological Metallic versus Metallic Solution in Treating Periprosthetic Femoral Fractures: Outcome Assessment. Adv Med. 2016;2016:2918735. doi: 10.1155/2016/2918735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gilde AK, Jones CB, Sietsema DL, Hoffmann MF. Does plate type influence the clinical outcomes and implant removal in midclavicular fractures fixed with 2.7-mm anteroinferior plates? A retrospective cohort study. J Orthop Surg Res. 2014;9:55. doi: 10.1186/s13018-014-0055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Endrizzi DP, White RR, Babikian GM, Old AB. Nonunion of the clavicle treated with plate fixation: a review of forty-seven consecutive cases. J Shoulder Elbow Surg. 2008;17(6):951–3. doi: 10.1016/j.jse.2008.05.046. [DOI] [PubMed] [Google Scholar]
- 34.Kloen P, Werner CM, Stufkens SA, Helfet DL. Anteroinferior plating of midshaft clavicle nonunions and fractures. Oper Orthop Traumatol. 2009;21(2):170–9. doi: 10.1007/s00064-009-1705-8. [DOI] [PubMed] [Google Scholar]
- 35.Schnetzke M, Morbitzer C, Aytac S, Erhardt M, Frank C, Muenzberg M, Studier-Fischer S, Helbig L, Suda AJ, Gruetzner PA, Guehring T. Additional bone graft accelerates healing of clavicle non-unions and improves long-term results after 8.9 years: a retrospective study. J Orthop Surg Res. 2015 Jan 9;10:2. doi: 10.1186/s13018-014-0143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]