Abstract
Background
Varicella zoster virus (VZV) causes both varicella (chickenpox) and herpes zoster (shingles) and is associated with significant global morbidity. Most epidemiological data on VZV come from high-come countries and to date there are limited data on the burden of VZV in Africa.
Methods
We assessed the seroprevalence of VZV antibodies among children in the Democratic Republic of Congo in collaboration with the 2013–2014 Demographic and Health Survey (DHS). Dried blood spot samples collected from children 6–59 months of age were run on Dynex™ Technologies Multiplier FLEX® chemiluminescent immunoassay platform to assess serologic response. Multivariate logistic regression was then used to determine risk factors for VZV seropositivity.
Results
Serologic and survey data were matched for 7,195 children 6 to 59 months of age, among whom 8% were positive and 2% indeterminate for VZV antibodies in weighted analyses. In multivariate analyses, the odds of seropositivity increased with increasing age, increasing socioeconomic status, mother’s education level, rural residence, and province (South Kivu, North Kivu, Bandundu, Bas Congo had the highest odds of a positive test result compared to Kinshasa).
Conclusion
Our data suggest that VZV is circulating in DRC and seropositivity is low among children 6 to 59 months. The with prevalence of seropositivity increased with age and varied by other sociodemographic factors, such as geographic location. This study provides the first nationally representative estimates of varicella zoster virus infection among children in the DRC.
Keywords: varicella zoster virus, varicella, herpes zoster, immunization, vaccine-preventable diseases, Democratic Republic of the Congo
Introduction
Varicella zoster virus (VZV) is the causative agent of both varicella (chickenpox) and herpes zoster (shingles), both of which occur worldwide (1). Primary varicella infection is characterized by a vesicular rash and fever, usually presenting as a mild, self-limiting illness in children (2). The most common complication in young children is secondary bacterial infection (3, 4); however, complications are more likely to occur in infants and adults, including pregnant women and immune-compromised individuals (5, 6). VZV is highly contagious with secondary attack rates in susceptible populations ranging from 61 to 100 percent (7–11) and is typically transmitted person-to-person by direct contact with lesions or inhalation of aerosolized droplets (1, 12).
Varicella is reported worldwide, however, population-based data are generally available from high-income countries (13–16). Studies conducted before widespread usage of the varicella vaccine in temperate regions suggest more than 90% of children are immune to VZV by adolescence due to natural infection (17–20). Varicella remains a public health concern among countries that do not have widespread vaccination coverage: contrary to findings in developed countries with temperate climates, limited data from the developing world including Thailand (21, 22) and India (16) suggest that varicella infection is less common in young children as infection tends to occur at a later age (13). This shift in the age of infection in tropical regions is also associated with markedly increased severity and complications such as skin infections, encephalitis, pneumonia, meningitis and death (16, 22, 23). On the other hand, Guinea Bissau, a developing, tropical country, has a median age of infection of 4 years (24) and by 10 years of age, 90% of the population is infected (25).
The reasons for the differing age epidemiology in various climates remain poorly understood (24); possible reasons include properties of VZV, climate, population density and the risk of exposure (22, 26).
In the Democratic Republic of the Congo (DRC), varicella is not a reportable disease, thus the burden of infection remains unknown (27). Therefore, in collaboration with the 2013–2014 DRC Demographic and Health Survey (DHS), we set out to obtain nationally representative, age-specific estimates of varicella infection among children 6 to 59 months of age.
Methods
Study Population and Design
The DRC is the largest country in sub-Saharan Africa and the fourth most populous nation on the continent with an estimated 77.8 million inhabitants, 11.9 million of which are under the age of five (28). At the time of this study, the DRC was administratively divided into 11 provinces. The country lies directly on the equator with one-third of the country to the north and two-thirds to the south. In the equatorial climate of Equateur, Orientale and Maniema provinces, the climate is generally tropical and moist, whereas in Kinshasa, Bas Congo, Bandundu, Kasai Oriental, and Kasai Occidental provinces, the climate is considered tropical savanna. In the southern highlands of Katanga, the climate is humid and subtropical. The eastern highlands of North and South Kivu generally have a cooler, alpine climate. North and South Kivu have also experienced the largest security difficulties and attacks by rebel groups, but have received more humanitarian interventions (29).
From November 2013 to February 2014, the second DHS was conducted in the DRC. Using a 2-stage stratified cluster design, the survey generates nationally representative data on population health and social indices. Details on the sampling design and data collection procedures are described elsewhere (30). Interviews were conducted among a nationally representative sample of 18,141 households. After parental consent, dried blood spots (DBS) were collected from children aged 6 to 59 months in 50% of the households selected.
All survey data were double entered from paper questionnaires to an electronic format, using the Census and Survey Processing System (U.S. Census Bureau, ICF Macro), and verified by comparison. Ethical approval was obtained at UCLA Fielding School of Public Health, the Kinshasa School of Public Health and the Centers for Disease Control and Prevention.
Laboratory Analysis
DBS samples were extracted using a modified extraction protocol (31) and processed at the UCLA-DRC laboratory housed at National Laboratory for Biomedical Research (INRB) in Kinshasa, DRC. A 0.25" DBS punch was extracted, shaken at room temperature in 1ml phosphate buffered saline, 0.05% Polysorbate 20, and 5% dried milk, which represents a 1:143 fold dilution assuming 7µl of serum per punch. The Dynex™ Technologies Multiplier FLEX® chemiluminescent immunoassay platform with a research use-only M² multiplex kit for measles, mumps, rubella, varicella-zoster virus, and tetanus (MMRVT) was used to test samples for IgG antibody response. Polystyrene beads coated separately with antigen to measles, mumps, rubella, varicella-zoster, and tetanus were immobilized within 54-well M² assay strips with 10 beads per well and processed using a modified Dynex DS2® automated ELISA system for IgG antibody detection.
Cut-offs were calculated via receiver operating characteristic (ROC) analysis to maximize agreement between 4 commercially available FDA-cleared ELISA kits (32) and categorization of serologic results were as follows: <0.18 IU/mL as negative; 0.18 to < 0.30 IU/mL as indeterminate; ≥0.30 IU/mL as positive. For analyses, the positive/negative cut-off for VZV IgG antibody detection was set at 0.30 IU/mL.
Statistical analysis
Chi-square analyses were performed on the weighted sample (using survey weights) to examine sociodemographic differences by serologic test results (positive and negative for varicella-zoster antibody). Univariate logistic regression models were used to identify independent predictors of seropositivity among variables included in Table 1. Multivariable regression models were initially run with all variables; using backward selection only significant predictors (alpha ≤ .05) were retained. Children for whom test results were indeterminate (n=125) were categorized as serologically positive and in sensitivity analyses these subjects were removed to assess the impact of their inclusion on findings. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC) and maps were created using ArcGIS software version 9.3 (ESRI, Redlands, CA).
Table 1.
Weighted demographic characteristics by varicella-zoster serosurvey result of 6–59 month old respondents of the 2013–2014 DRC-DHS.
| Negative (n=6,435) |
Positivea (n=815) |
Chi-square p-value |
|
|---|---|---|---|
| n (%) | n (%) | ||
| Child age | |||
| 6–11 monthsb | 798 (94) | 51 (6) | |
| 1 year | 1,578 (93) | 113 (7) | |
| 2 years | 1,468 (88) | 193 (12) | |
| 3 years | 1,350 (87) | 198 (13) | |
| 4 years | 1,241 (83) | 260 (17) | <0.0001 |
| Child sex | |||
| Male | 3,224 (89) | 410 (11) | |
| Female | 3,211 (89) | 405 (11) | 0.8888 |
| Children in householdc | |||
| 1 | 974 (92) | 85 (8) | |
| 2 | 1,357 (92) | 115 (8) | |
| 3 | 1,217 (88) | 168 (12) | |
| 4 | 1,067 (89) | 137 (11) | |
| 5 or more | 1,821 (85) | 310 (15) | <0.0001 |
| Mother's age at birth | |||
| ≤20 years | 1,209 (92) | 101 (8) | |
| 21–25 years | 1,699 (91) | 175 (9) | |
| 26–30 years | 1,644 (90) | 190 (10) | |
| 31–35 years | 1,040 (89) | 133 (11) | |
| >35 years | 906 (90) | 98 (10) | 0.0298 |
| Mother's highest level of education | |||
| No education | 1,274 (87) | 187 (13) | |
| Primary | 2,867 (91) | 293 (9) | |
| Secondary/higher | 2,295 (87) | 335 (13) | <0.0001 |
| Wealth indexd | |||
| Poorest | 1,503 (92) | 129 (8) | |
| Poorer | 1,555 (92) | 135 (8) | |
| Middle | 1,299 (88) | 172 (12) | |
| Richer | 1,158 (85) | 198 (15) | |
| Richest | 920 (84) | 181 (16) | <0.0001 |
| Province | |||
| Kinshasa | 415 (87) | 65 (13) | |
| Bandundu | 1,062 (86) | 170 (14) | |
| Bas-Congo | 271 (86) | 46 (14) | |
| Equateur | 1,032 (96) | 47 (4) | |
| Kasai-Occidental | 524 (93) | 38 (7) | |
| Kasai-Oriental | 743 (93) | 52 (6) | <0.0001 |
| Katanga | 646 (86) | 102 (14) | |
| Maniema | 245 (96) | 10 (4) | |
| Nord-Kivu | 508 (83) | 104 (17) | |
| Orientale | 569 (92) | 53 (8) | |
| Sud-Kivu | 421 (76) | 130 (24) | |
| Residence | |||
| Urban | 1,852 (85) | 315 (15) | |
| Rural | 4,583 (90) | 500 (10) | <0.0001 |
Includes those who tested positive and indeterminant on Dynex M2 multiplex for varicella-zoster virus.
Only children 6 months of age and older were invited to participate in the serosurvey.
Children in household is the sum of boys and girls that currently live in the household.
Wealth index is a composite measure of a household's cumulative living standard, calculated from household ownership of selected assets (such as televisions and bicycles), materials used for housing construction, and types of water access and sanitation facilities. Using principal components analysis, the DHS separates all interviewed households into five wealth quintiles.
Results
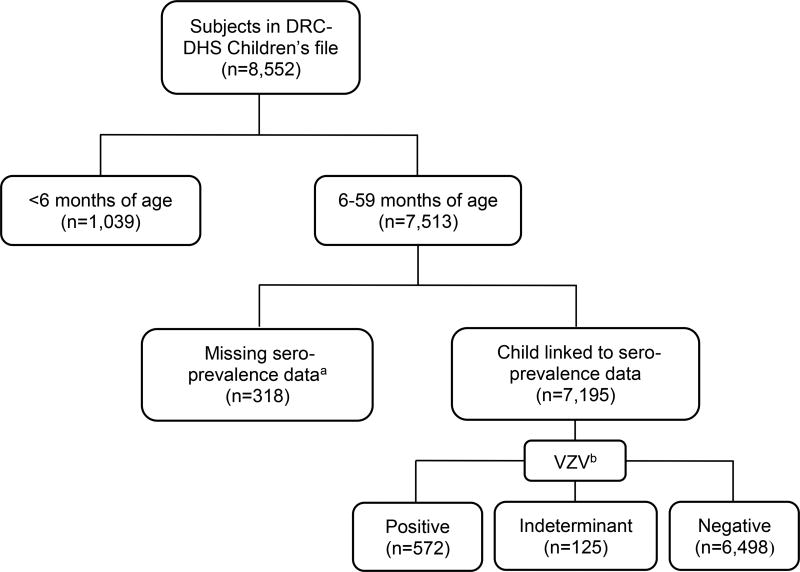
Among the 7,513 eligible 6–59 month olds, approximately 96% (n=7,195) were linked to seroprevalence data and included in analyses. Among these children, 572 (8%) were positive, 6,498 (90%) were negative, and 125 (2%) were indeterminate for varicella-zoster antibody (Figure 1). Categorizing children with indeterminate results as positive and accounting for population sampling methods through the application of DHS sampling weights, a total of 815 children (11%) were positive and 6,435 (89%) negative (Table 1). Overall, children born to higher socioeconomic status (SES), and older mothers living in urban environments were more likely to test positive for varicella zoster virus IgG compared to their younger, lower SES, rural counterparts.
Figure 1.
Study inclusion for assessment of varicella-zoster virus seroprevalence among children 6–59 months of age, 2013–2014 Demographic and Health Survey, Democratic Republic of Congo (unweighted)
a Those with missing seroprevalence data include: 18 who were not present, 129 who refused participation, 120 for whom the DBS sample was not found in the database, 20 for whom the barcode to match DBS sample was not known, and 31 “others”; b VZV stands for varicella-zoster virus
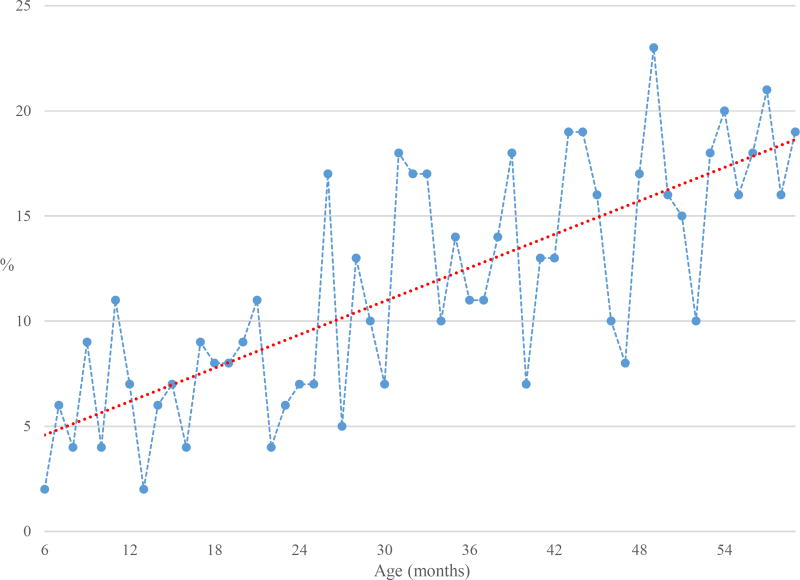
Furthermore, assessment of the assay response reveals an increase in seropositivity with increasing age: from 2% of 6 month olds to 19% of 59 month olds (range: 2%–23%) (Figure 2). Among all children, those living in North and South Kivu had the highest prevalence of seropositive children (17% and 24%, respectively), while Equateur and Maniema had the lowest (4% for both) (Figure 3). This pattern in serologic response according to geographic region persisted in those ≥1 year of age. However, among those 6–11 months of age, South Kivu and Kinshasa had the highest prevalence of positive results (18% and 11%, respectively) while North Kivu and Katanga had the lowest (<1% and 1%, respectively). In multivariate analyses, the odds of seropositivity increased with increasing age, number of children residing in the household, wealth index, and province (Table 2). Sensitivity analyses excluding indeterminate serologic results did not impact findings (data not shown).
Figure 2.
Varicella-zoster seropositivity according to age (in months) among 6–59 months old 2013–2014 DRC-DHS respondents (linear trend line in red).
Figure 3.
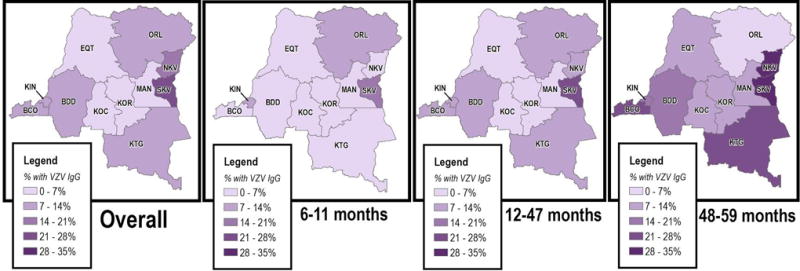
Varicella-zoster seropositivity by province and age among 6–59 months old 2013–2014 DRC-DHS respondents.
a BCD stands for Bas Congo; KIN stands Kinshasa; BDD stands for Bandundu; KOC stands for Kasai Occidental; KOR stands for Kasai Oriental; EQT stands for Equateur; ORL stands for Orientale; MAN stands for Maniema; NKV stands for North Kivu; SKV stands for South Kivu; KTG stands for Katanga
Table 2.
Weighted logistic regression of sociodemographic factors associated with varicella-zoster seropositivity of 6–59 month old 2013–2014 DRC-DHS respondents.
| ORcrude (95%CI) | ORadjusteda (95%CI) | |
|---|---|---|
| Child age | ||
| 6–11 monthsb | ref | ref |
| 1 year | 1.11 (0.79, 1.57) | 1.51 (0.81, 1.63) |
| 2 years | 2.06 (1.49, 2.83) | 2.12 (1.53, 2.94) |
| 3 years | 2.28 (1.66, 3.14) | 2.41 (1.74, 3.35) |
| 4 years | 3.27 (2.39, 4.47) | 3.19 (2.31, 4.41) |
| Children in householdc | ||
| 1 | ref | ref |
| 2 | 0.97 (0.72, 1.30) | 0.77 (0.57, 1.05) |
| 3 | 1.58 (1.20, 2.08) | 1.20 (0.90, 1.60) |
| 4 | 1.47 (1.10, 1.95) | 1.15 (0.85, 1.55) |
| 5 or more | 1.95 (1.51, 2.51) | 1.49 (1.14, 1.96) |
| Mother's highest level of education | ||
| No education | ref | ref |
| Primary | 1.01 (0.83, 1.22) | 0.71 (0.57, 0.87) |
| Secondary/higher | 0.70 (0.59, 0.83) | 0.87 (0.69, 1.11) |
| Wealth indexd | ||
| Poorest | ref | ref |
| Poorer | 1.01 (0.79, 1.30) | 0.84 (0.64, 1.08) |
| Middle | 1.55 (1.22, 1.97) | 1.23 (0.95, 1.59) |
| Richer | 1.99 (1.58, 2.52) | 1.31 (1.00, 1.73) |
| Richest | 2.30 (1.81, 2.93) | 1.54 (1.06, 2.23) |
| Province | ||
| Kinshasa | ref | ref |
| Bandundu | 1.03 (0.76, 1.40) | 1.95 (1.32, 2.89) |
| Bas-Congo | 1.09 (0.72, 1.64) | 1.80 (1.15, 2.84) |
| Equateur | 0.29 (0.20, 0.43) | 0.56 (0.35, 0.88) |
| Kasai-Occidental | 0.46 (0.30, 0.70) | 0.81 (0.50, 1.30) |
| Kasai-Oriental | 0.45 (0.31, 0.66) | 0.72 (0.47, 1.11) |
| Katanga | 1.02 (0.73, 1.42) | 1.48 (1.02, 2.14) |
| Maniema | 0.26 (0.13, 0.52) | 0.44 (0.21, 0.92) |
| Nord-Kivu | 1.32 (0.94, 1.85) | 1.97 (1.33, 2.92) |
| Orientale | 0.60 (0.41, 0.88) | 1.17 (0.76, 1.82) |
| Sud-Kivu | 1.98 (1.43, 2.75) | 3.41 (2.28, 5.10) |
| Residence | ||
| Urban | 1.56 (1.34, 1.81) | 1.46 (1.15, 1.85) |
| Rural | ref | ref |
Using backwards selection, only significant predictors (alpha ≤0.05) were retained in the final model; predictors in adjusted model include all variables in table 2.
Only children 6 months of age and older were invited to participate in the serosurvey.
Children in household is the sum of boys and girls that currently live in the household.
Wealth index is a composite measure of a household's cumulative living standard, calculated from household ownership of selected assets (such as televisions and bicycles), materials used for housing construction, and types of water access and sanitation facilities. Using principal components analysis, the DHS separates all interviewed households into five wealth quintiles.
Discussion
These findings suggest that VZV is circulating in DRC with an overall seroprevalence of 8% among children 6–59 months of age. We also observed a trend of increasing seropositivity with older age and varying serologic response by geographic region (North and South Kivu have the highest prevalence of VZV-positive children). These findings provide the first nationally representative estimates of varicella zoster virus infection among young children in the DRC.
Our findings of low infectivity among young children and increasing seroprevalence with older age are consistent with other studies (16, 33). Between 2001–2004, the monkeypox active disease surveillance system estimated the average age of VZV infection to be 20.6 years among the 61 positive participants(33). While the study was not nationally representative, it does suggest VZV exposure occurs at older ages. Our estimate of VZV seroprevalence among children less than 5 years of age in the DRC is lower than other studies in tropical regions (16). However, estimates of seropositivity among young children differ significantly by country: estimates range from 16% of children 1–4 years of age in India (34); 24% of children 1–4 years of age in Thailand (21); 26% of children 1–5 years of age in Malaysia (35); 30% of children under 5 years of age in the Philippines (23); and 35% of children 1–6 years of age in Singapore (36). In a prospective study conducted in Guinea Bissau, the proportion of index cases was highest among children aged 2 to 9 years (24). The lower seroprevalence in our study may be attributable to the younger study population, which includes children 6 months to <5 years of age.
The overall trend in tropical regions may suggest that the greatest rate of seroconversion occurs in adolescence and adulthood (37), which is concerning as infection in older ages is associated with increased rates of severe disease and complications (including skin infections, pneumonia, and encephalitis) and mortality (13, 16, 38, 39). Furthermore, as seroconversion more commonly occurs in adolescence or adulthood in tropical countries, a large proportion of reproductive age women may remain susceptible to VZV in pregnancy. VZV infection during pregnancy results in intrauterine infection in 25% of the cases (40). Primary VZV infection in the first 20 weeks of gestation may result in congenital varicella syndrome, in which infected mothers pass on the virus to the fetus (41). An estimated 2% of fetuses are affected by the syndrome after maternal infection, resulting in outcomes ranging from low birth weight to more severe anomalies such as chorioretinitis, microcephaly, encephalitis, skin scarring and muscle wasting of the extremities severe anomalies (3, 41, 42). Infection during the third trimester and near delivery, in particular 5 days before or 2 days after birth, can cause severe and fatal infections in neonates (43). After delivery, in utero infection is also associated with herpes zoster (shingles) in childhood (3). Therefore, additional serologic studies in older age groups will be important to evaluate the burden of VZV infection in the population and age-specific trends in virus circulation to identify vulnerable subgroups.
Moreover, the underlying reasons for varying response across provinces, in particular the low seroprevalence observed in Maniema and Equateur and the high seroprevalence observed in North and South Kivu, remain unclear. Such low rates of seroconversion may be the result of reduced viral circulation in high ambient temperatures and humidity (44), or a combination of other factors such as cross reactivity to other herpes viruses (45). In South East Asia, outbreaks appear to be more common in cooler months and temperate regions (15, 46–48), which is similar to the mountainous environment of North and South Kivu in eastern DRC. However, it is also possible that other factors such as increased crowding in homes in a cooler climate may favor transmission due to larger inoculum (16). Moreover, political instability in the east has led to large groups of internally displaced persons and while densely populated and crowded environments facilitate VZV transmission (49), the influx of potentially seronegative subjects may artificially decrease the prevalence in such areas.
Additional limitations of our study include possible misclassification of serologic status. However, compared to four commercially available kits, the multiplex assay exhibited high validity for both sensitivity and specificity (sensitivity range: 89.5–100%; specificity range: 77.3–100%), making it unlikely that misclassification would significantly impact our findings. Furthermore, the cost-effectiveness of the multiplex assay was high as we were also able to evaluate the seroprevalence of antigens for mumps, measles, rubella, polio and tetanus. Additionally, we initially categorized serologically indeterminate children as positive; however, in sensitivity analyses, exclusion of these individuals did not change our results. Furthermore, the younger children in the study population may still have maternal antibodies
There exists a safe and effective varicella vaccine, but it is only used in high income countries (13). According to the WHO, varicella vaccine is not a high priority for routine introduction into a national vaccination program (50). While the morbidity and mortality associated with varicella is considerably lower than other VPDs, the virus still results in 140 million cases, 4.2 million hospitalizations, and 4,200 deaths annually in countries with limited access to health infrastructure (13). Complications can lead to significant healthcare and societal costs and cause a sizable burden for patients and caregivers; however, limited information exists on the health burden of varicella in developing countries and tropical climates where a higher proportion of cases may occur among adults. In these areas, varicella morbidity and mortality may be higher than that of developed countries (51).
Additional epidemiologic information regarding VZV infection is of particular interest in DRC as the clinical presentation is similar to that of monkeypox virus (MPXV), a zoonosis endemic to the Congo basin, where a steady increase in incidence has been reported since the cessation of routine smallpox immunization in 1982 (52). Limited data available through MPX surveillance in DRC provide evidence that varicella is circulating (53, 54) and findings suggest VZV infection is commonly mistaken for MPX in central Africa (54–56).
To our knowledge, this is the first study to provide a national estimate of VZV exposure among children. Evidence of the burden of VZV remains incomplete and additional serologic studies in older populations will be required to better understand transmission and its public health significance in the DRC.
Acknowledgments
Funding Source: This work was supported by the Bill and Melinda Gates Foundation, Seattle, WA [grant number: OPP106668].
References
- 1.Gershon AA, Takahashi M, Seward JF. Varicella vaccine. In: Plotkin SA, Orenstin WA, Offit PA, editors. Vaccine. 6. Elsevier Saunders; 2013. pp. 836–869. [Google Scholar]
- 2.Heininger U, Seward JF. Varicella. Lancet. 2006;368:1365–1376. doi: 10.1016/S0140-6736(06)69561-5. [DOI] [PubMed] [Google Scholar]
- 3.Preblud SR. Varicella: complications and costs. Pediatrics. 1986;78(4):728–735. [PubMed] [Google Scholar]
- 4.Choo PW, Donahue JG, Manson JE, Platt R. The epidemiology of varicella and its complications. J Infect Dis. 1995;172:706–712. doi: 10.1093/infdis/172.3.706. [DOI] [PubMed] [Google Scholar]
- 5.Preblud SR. Age-specific risks of varicella complications. Pediatrics. 1981;68(1):14–17. [PubMed] [Google Scholar]
- 6.Fleisher G, Henry W, McSorley M, Arbeter A, Plotkin S. Life-threatening complications of varicella. Archives of Pediatrics & Adolescent Medicine. 1981;135(10):896. doi: 10.1001/archpedi.1981.02130340008004. [DOI] [PubMed] [Google Scholar]
- 7.Fairley CK, Miller E. Varicella-zoster virus epidemiology-a changing scene? Journal of infectious diseases. 1996;174(Supplement 3):S314–S319. doi: 10.1093/infdis/174.supplement_3.s314. [DOI] [PubMed] [Google Scholar]
- 8.Simpson RH. Infectiousness of communicable diseases in the household:(measles, chickenpox, and mumps) The Lancet. 1952;260(6734):549–554. doi: 10.1016/s0140-6736(52)91357-3. [DOI] [PubMed] [Google Scholar]
- 9.Ross AH, Lenchner E, Reitman G. Modification of chicken pox in family contacts by administration of gamma globulin. New England Journal of Medicine. 1962;267(8):369–376. doi: 10.1056/NEJM196208232670801. [DOI] [PubMed] [Google Scholar]
- 10.Seward JF, Zhang JX, Maupin TJ, Mascola L, Jumaan AO. Contagiousness of varicella in vaccinated cases: a household contact study. Jama. 2004;292(6):704–708. doi: 10.1001/jama.292.6.704. [DOI] [PubMed] [Google Scholar]
- 11.Asano Y, Nakayama H, Yazaki T, Kato R, Hirose S. Protection against varicella in family contacts by immediate inoculation with live varicella vaccine. Pediatrics. 1977;59(1):3–7. [PubMed] [Google Scholar]
- 12.Richardson M, Elliman D, Maguire H, Simpson J, Nicoll A. Evidence base of incubation periods, periods of infectiousness and exclusion policies for the control of communicable diseases in schools and preschools. Pediatr Infect Dis J. 2001;20(4):380–91. doi: 10.1097/00006454-200104000-00004. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Varicella and herpes zoster vaccines: WHO position paper, June 2014. Weekly Epidemiologic Record. 2014;25(89):265–288. [Google Scholar]
- 14.Somekh E, Dalal I, Shohat T, Ginsberg GM, Romano O. The burden of uncomplicated cases of chickenpox in Israel. Journal of Infection. 2002;45(4):233–236. doi: 10.1053/jinf.2002.1039. [DOI] [PubMed] [Google Scholar]
- 15.Balraj V, John T. An epidemic of varicella in rural southern India. The Journal of tropical medicine and hygiene. 1994;97(2):113–116. [PubMed] [Google Scholar]
- 16.Lee B. Review of varicella zoster seroepidemiology in India and South-east Asia. Tropical Medicine and International Health. 1998;3(11):886–890. doi: 10.1046/j.1365-3156.1998.00316.x. [DOI] [PubMed] [Google Scholar]
- 17.Alp H, Altınkaynak S, Ertekin V, Kılıçaslan B, Giiraksin A. Seroepidemiology of varicella-zoster virus infection in a cosmopolitan city (Erzurum) in the eastern Turkey. Health Policy. 2005;72(1):119–124. doi: 10.1016/j.healthpol.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Wutzler P, Färber I, Wagenpfeil S, Bisanz H, Tischer A. Seroprevalence of varicella-zoster virus in the German population. Vaccine. 2001;20(1):121–124. doi: 10.1016/s0264-410x(01)00276-6. [DOI] [PubMed] [Google Scholar]
- 19.Gil A, Gonzalez A, Dal-Re R, Ortega P, Dominguez V. Prevalence of antibodies against varicella zoster, herpes simplex (types 1 and 2), hepatitis B and hepatitis A viruses among Spanish adolescents. Journal of Infection. 1998;36(1):53–56. doi: 10.1016/s0163-4453(98)93126-7. [DOI] [PubMed] [Google Scholar]
- 20.Kang C-I, Choi C-M, Park T-S, Lee D-J, Oh M-d, Choe K-W. Incidence of herpes zoster and seroprevalence of varicella-zoster virus in young adults of South Korea. International Journal of Infectious Diseases. 2008;12(3):245–247. doi: 10.1016/j.ijid.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Migasena S, Simasathien S, Desakorn V, Phonrat B, Suntharasamai P, Pitisuttitham P, et al. Seroprevalence of varicella-zoster virus antibody in Thailand. International journal of infectious diseases. 1997;2(1):26–30. [Google Scholar]
- 22.Lolekha S, Tanthiphabha W, Sornchai P, Kosuwan P, Sutra S, Warachit B, et al. Effect of climatic factors and population density on varicella zoster virus epidemiology within a tropical country. The American journal of tropical medicine and hygiene. 2001;64(3):131–136. doi: 10.4269/ajtmh.2001.64.131. [DOI] [PubMed] [Google Scholar]
- 23.Barzaga N, Roxas J, Florese R. Varicella zoster virus prevalence in metro Manila, Philippines. JAMA (SE Asia) 1994;274:S633–S635. [Google Scholar]
- 24.Poulsen A, Cabral F, Nielsen J, Roth A, Lisse IM, Vestergaard BF, et al. Varicella zoster in Guinea-Bissau: intensitty of exposure and severity of infection. Pediatric Infectious Disease Journal. 2005;24(2):102–107. doi: 10.1097/01.inf.0000151034.15747.4a. [DOI] [PubMed] [Google Scholar]
- 25.Nichols RA, Averbeck KT, Poulsen AG, al Bassam MM, Cabral F, Aaby P, et al. Household size is critical to varicella-zoster virus transmission in the tropics despite lower viral infectivity. Epidemics. 2011;3(1):12–18. doi: 10.1016/j.epidem.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mandal BK, Mukherjee PP, Murphy C, Mukherjee R, Naik T. Adult susceptibility to varicella in the tropics is a rural phenomenon due to the lack of previous exposure. J Infect Dis. 1998;178(Supplement 1):S52–S54. doi: 10.1086/514262. [DOI] [PubMed] [Google Scholar]
- 27.Organization WH. Adding a vaccine to a national immunization programme: decision and implementation. Geneva: World Health Organization; 2005. Vaccine introduction guidelines. [Google Scholar]
- 28.Minister of Plan, Minister of Health, International I. Demograhic and Health Survey: Democratic Republic of Congo 2013–14. Supplementational Vaccine-Preventable Diseases; Rockville, Maryland: 2014. [Google Scholar]
- 29.Kandala N-B, Madungu TP, Emina JB, Nzita KP, Cappuccio FP. Malnutrition among children under the age of five in the Democratic Republic of Congo (DRC): does geographic location matter? BMC public health. 2011;11(1):261. doi: 10.1186/1471-2458-11-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.ICF International. Sampling and Household Listing Manual. Calverton, Maryland: 2012. [Google Scholar]
- 31.Mercader S, Featherstone D, Bellini WJ. Comparison of available methods to elute serum from dried blood spot samples for measles serology. Journal of Virological Methods. 2006;137(1):140–149. doi: 10.1016/j.jviromet.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 32.Higgins SG. Validations of Dynex multiplexed serology panel for Measles, Mumps, Rubella, Varicella Zoster Virus and Tetanus (unpublished work) 2016 [Google Scholar]
- 33.Rimoin AW, Kisalu N, Kebela-Ilunga B, Mukaba T, Wright LL, Formenty P, et al. Endemic human monkeypox, democratic Republic of Congo, 2001–2004. Emerging infectious diseases. 2007;13(6):934. doi: 10.3201/eid1306.061540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Venkitaraman AR, Seigneurin J-M, Lenoir GM, T Jacob J. Infections due to the human herpes-viruses in Southern India: a seroepidemiological survey. International journal of epidemiology. 1986;15(4):561–566. doi: 10.1093/ije/15.4.561. [DOI] [PubMed] [Google Scholar]
- 35.Malik YA, Baharin R. Prevalence of varicella zoster virus infection in Malaysia. Proceeding of the 5th International Congress on the Impact of Viral Diseases in the Developing World; 1995; Johannesburg, South Africa. 1995. [Google Scholar]
- 36.Fatha N, Ang LW, Goh KT. Changing seroprevalence of varicella zoster virus infection in a tropical city state, Singapore. International Journal of Infectious Diseases. 2014;22:73–77. doi: 10.1016/j.ijid.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 37.Sloan D, Burlison A. Shift in age in chickenpox. The Lancet. 1992;340(8825):974. doi: 10.1016/0140-6736(92)92860-i. [DOI] [PubMed] [Google Scholar]
- 38.Guess H, Broughton D, Melton Lr, Kurland L. Population-based studies of varicella complications. Pediatrics. 1986;78(4):723–727. [PubMed] [Google Scholar]
- 39.Baren JM, Henneman PL, Lewis RJ. Primary varicella in adults: pneumonia, pregnancy, and hospital admission. Annals of emergency medicine. 1996;28(2):165–169. doi: 10.1016/s0196-0644(96)70057-4. [DOI] [PubMed] [Google Scholar]
- 40.Paryani SG, Arvin AM. Intrauterine infection with varicella-zoster virus after maternal varicella. New England Journal of Medicine. 1986;314:1542–1546. doi: 10.1056/NEJM198606123142403. [DOI] [PubMed] [Google Scholar]
- 41.Pastuszak AL, Levy M, Schick B, Zuber C, Feldkamp M, Gladstone J, et al. Outcome after maternal varicella infection in the first 20 weeks of pregnancy. New England Journal of Medicine. 1994;330:901–905. doi: 10.1056/NEJM199403313301305. [DOI] [PubMed] [Google Scholar]
- 42.Enders G, Miller E, Cradock-Watson J, Bolley I, Ridehalgh M. Consequences of varicella and herpes zoster in pregnancy: prospective study of 1739 cases. Lancet. 1994;343:1548–1551. doi: 10.1016/s0140-6736(94)92943-2. [DOI] [PubMed] [Google Scholar]
- 43.Sauerbrei A, Wutzler P. Neonatal varicella. J Perinatol. 2001;21(8):545–9. doi: 10.1038/sj.jp.7210599. [DOI] [PubMed] [Google Scholar]
- 44.Garnett G, Cox M, Bundy DA, Didier JM, Catharine JS. The age of infection with varicella-zoster virus in St Lucia, West Indies. Epidemiology and infection. 1993;110(02):361–372. doi: 10.1017/s0950268800068308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Edson CM, Hosler B, Respess R, Waters D, Thorley-Lawson D. Cross-reactivity between herpes simplex virus glycoprotein B and a 63,000-dalton varicella-zoster virus envelope glycoprotein. Journal of virology. 1985;56(1):333–336. doi: 10.1128/jvi.56.1.333-336.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Basu RN, Jezek Z, Ward NA. The eradication of smallpox from India: World Health Organization. South East Asia Regional Office; New Delhi, India: 1979. [Google Scholar]
- 47.White E, Organization WH. Chickenpox in Kerala. 1976. [Google Scholar]
- 48.Health MoP. Annual Epidemiological Surveillance Report. Ministry of Public Health; Bangkok: 1995. [Google Scholar]
- 49.Shimakawa Y, Camélique O, Ariyoshi K. Outbreak of chickenpox in a refugee camp of northern Thailand. Conflict and health. 2010;4(1):1. doi: 10.1186/1752-1505-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wkly Epidemiol Rec: World Health Organization. 1998. Varicella vaccines. [Google Scholar]
- 51.Plotkin Stanley, Orenstein Walter, Offit P. Vaccines. 6. Saunders; 2012. Varicella Vaccines. [Google Scholar]
- 52.Rimoin AW, Mulembakani PM, Johnston SC, Lloyd Smith JO, Kisalu NK, Kinkela TL, et al. Major increase in human monkeypox incidence 30 years after smallpox vaccination campaings cease in the Democratic Republic of Congo. PNAS. 2010;107(37):16262–16267. doi: 10.1073/pnas.1005769107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hutin Y, Williams RJ, Malfait P, Pebody R, Loparev VN, Ropp SL, et al. Outbreak of human monkeypox, Democratic Republic of Congo, 1996 to 1997. Emerging infectious diseases. 2001;7(3):434. doi: 10.3201/eid0703.010311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meyer H, Perrichot M, Stemmler M, Emmerich P, Schmitz H, Varaine F, et al. Outbreaks of disease suspected of being due to human monkeypox virus infection in the Democratic Republic of Congo in 2001. Journal of clinical microbiology. 2002;40(8):2919–2921. doi: 10.1128/JCM.40.8.2919-2921.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rimoin AW, Kisalu N, Kebela-Ilunga B, Mukaba T, Wright LL, Formenty P, et al. Endemic Human Monkeypox, Democratic Republic of Congo, 2001–2004. Emerging Infectious Diseases. 2007;13(6):934–937. doi: 10.3201/eid1306.061540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.MacNeil A, Reynolds MG, Carroll DS, Karem K, Braden Z, Lash R, et al. Monkeypox or varicella? Lessons from a rash outbreak investigation in the Republic of Congo. American Journal of Tropical Medicine and Hygiene. 2009;80(4):503–507. [PubMed] [Google Scholar]