Abstract
CSF-1 and IL-34 share the CSF-1 receptor and no differences have been reported in the signaling pathways triggered by both ligands in human monocytes. IL-34 promotes the differentiation and survival of monocytes, macrophages and osteoclasts, as CSF-1 does. However, IL-34 binds other receptors, suggesting that differences exist in the effect of both cytokines. In the present study, we compared the differentiation and polarization abilities of human primary monocytes in response to CSF-1 or IL-34. CSF-1R engagement by one or the other ligands leads to AKT and caspase activation and autophagy induction through expression and activation of AMPK and ULK1. As no differences were detected on monocyte differentiation, we investigated the effect of CSF-1 and IL-34 on macrophage polarization into the M1 or M2 phenotype. We highlighted a striking increase in IL-10 and CCL17 secretion in M1 and M2 macrophages derived from IL-34 stimulated monocytes, respectively, compared to CSF-1 stimulated monocytes. Variations in the secretome induced by CSF-1 or IL-34 may account for their different ability to polarize naïve T cells into Th1 cells. In conclusion, our findings indicate that CSF-1 and IL-34 exhibit the same ability to induce human monocyte differentiation but may have a different ability to polarize macrophages.
Introduction
Monocytes are circulating blood leukocytes that play important role in tissue homeostasis and in the inflammatory response which is essential for the innate response to pathogens1. They have the unique property among peripheral blood cells to migrate into tissues where they are subjected to differentiation into morphological and functionally heterogeneous cells that include macrophages, myeloid dendritic cells, and osteoclasts, depending on the stimulus2. The differentiation of peripheral blood monocytes into resident tissue macrophages can be recapitulated ex vivo by incubation in the presence of colony-stimulating factor-1 (CSF-1)3. The biologic effects of CSF-1 are mediated by a unique receptor, the CSF-1R, which is encoded by the c-fms proto-oncogene4. Downstream signaling pathways activated by CSF-1R upon ligand binding include PI3K-AKT and AMPK pathways, which are implicated in the respective activation of caspases and autophagy, two key processes required for CSF-1-induced macrophage differentiation5. Our previous studies have established that physiological monocyte differentiation triggered by CSF-1R engagement is critically dependent on the oscillatory activation of the kinase AKT, which within 2–3 days leads to the formation of a multi-molecular platform that includes the adaptor Fas-associated death domain (FADD), the serine-threonine kinase RIP1, the long and short isoforms of FLIP, and procaspase-86. Caspase-8 activation in this platform provokes a limited activation of several downstream caspases that cleave specific intracellular proteins7,8. The contribution of these cleavages to the CSF-1–driven monocyte-to-macrophage differentiation remains poorly understood. More recently, we have also established that autophagy plays a crucial role during macrophage differentiation of monocytes9. We found that CSF-1 increases the expression of the purinergic receptor P2RY6 that in turn activates the CAMKK2-AMPK-ULK1 pathway leading to autophagy induction10. Notably, inhibition of this pathway abrogated both CSF-1-mediated induction of autophagy and differentiation.
IL-34 is a newly identified cytokine with only partially understood functions. IL-34 has been recently identified as the second ligand for CSF-1R through comprehensive proteomic analyses11. Although it lacks appreciable similarity with CSF-1 or any other proteins, IL-34 tightly binds to CSF-1R and promotes the differentiation, proliferation and survival of monocytes, macrophages and osteoclasts as CSF-1 does12,13. IL-34 actions have been rendered more complex by the discovery of two other distinct receptors: the receptor type protein-tyrosine phosphatase zeta (PTP-ζ)14 and CD138 (Syndecan 1)15, suggesting additional roles for IL-34, compared to CSF-1. Recently, IL-34 was found to be associated with the inflammation process seen in diseases such as rheumatoid arthritis (RA)16, inflammatory bowel disease17 and Sjogren’s syndrome18. Interestingly, emerging findings indicate that IL-34 levels are abnormally increased in serum and synovial fluid in patients with reactive rheumatoid arthritis19,20.
Here, we used human primary monocytes to characterize in details IL-34 and CSF-1-driven macrophage differentiation and polarization into the M1 or M2 phenotype. We demonstrate that IL-34, like CSF-1, induced caspase and autophagy activation and that both processes are required to induce differentiation of monocytes into macrophages in response to IL-34. Moreover, we report that IL-34 and CSF-1 macrophages display a different polarization potential when polarized by pro or anti-inflammatory stimulus, since we found some differences in the mRNA and protein expression profiles of some cytokines/chemokines in CSF-1 and IL-34 differentiated cells polarized into the M1 or M2 phenotype.
Results
CSF-1 and lL-34 exhibit similar signaling and differentiation properties in primary human monocytes
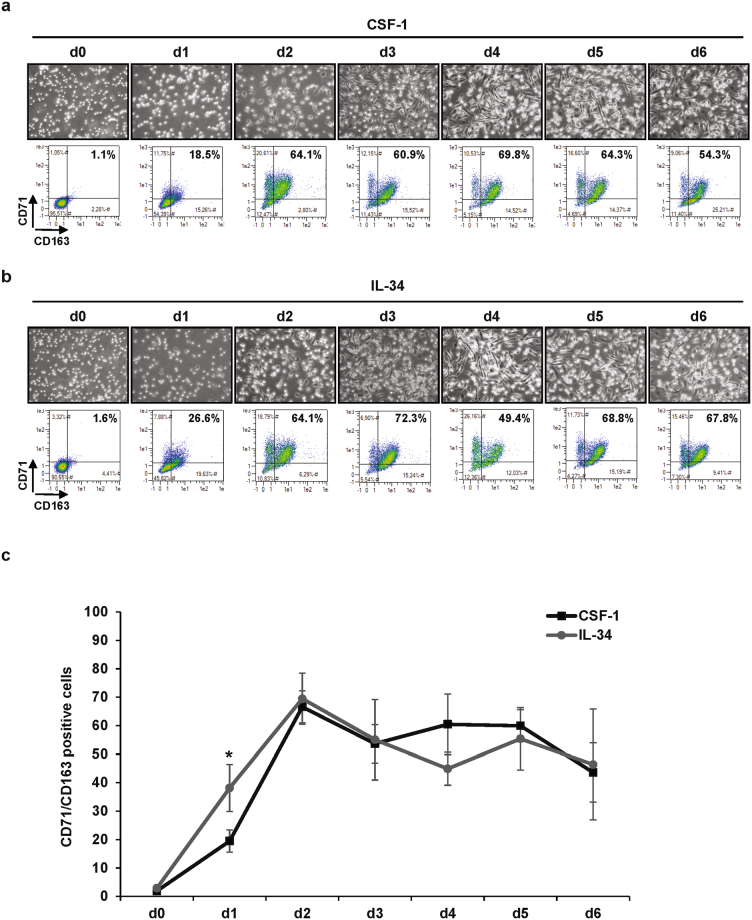
When stimulated with 100 ng/mL CSF-1, human monocytes differentiate into macrophages as shown by an increase in cell adherence and the acquisition of specific markers such as TFRC/CD71 and CD163. At day 2, 60–70% of myeloid cells were found to be positive for both CD71 and CD163 expression (Fig. 1a). This high rate of differentiation was maintained up to 6 days. The kinetic of macrophage differentiation induced by 100 ng/mL lL-34, the second known ligand of the CSF-1R, was nearly indistinguishable from that of CSF-1 (Fig. 1b and c, Sup Fig. 1a and b). As CSF-1 and IL-34 bind the CSF-1R with differential affinities, we performed a dose-response curve for each cytokine on monocyte differentiation (Sup Fig. 1c). We confirmed that for each cytokine, a 100 ng/mL concentration triggers maximal differentiation capacity.
Figure 1.
IL-34 and CSF-1 induce equivalent macrophagic differentiation of primary monocytes. Human peripheral blood monocytes from healthy donors were exposed to 100 ng/mL CSF-1 or 100 ng/mL IL-34 for the indicated times. (a,b) Macrophage differentiation was examined morphologically (fibroblastic shape) and by 2-color flow cytometric analysis. The percentage indicates cells that express both CD71 and CD163. (c) Macrophagic differentiation of monocytes from 3 different healthy donors was followed by 2-color flow cytometric analysis. The percentage indicates cells that express both CD71 and CD163. *P < 0.05 according to a paired student t test.
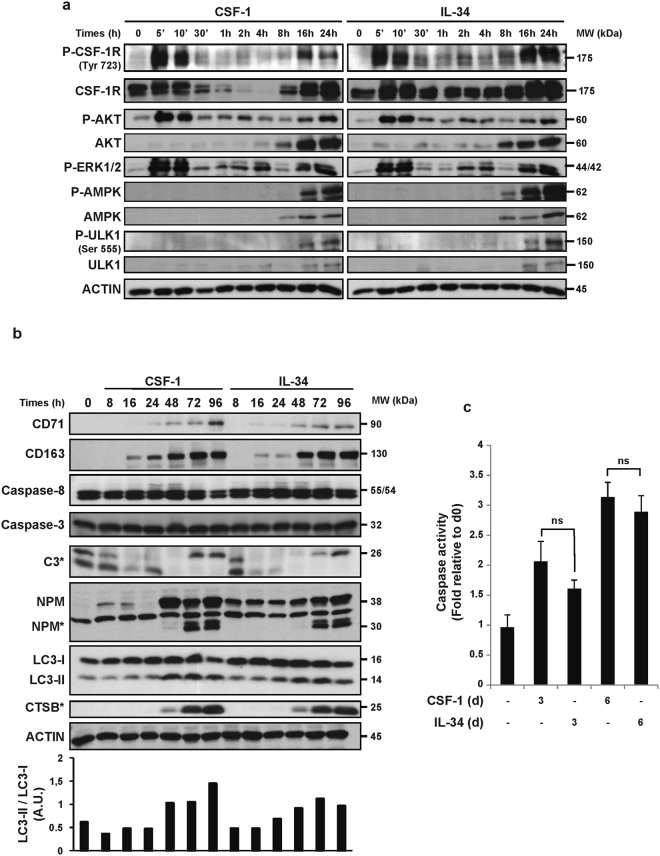
We next analyzed the early signaling pathways associated with the engagement of the CSF-1 receptor by either CSF-1 or lL-34 in human primary monocytes. We show that both CSF-1 and lL-34 triggered a transient first wave of CSF-1R phosphorylation at 5 and 10 min and a second one at 16 and 24 h (Fig. 2a). For both cytokines, the second wave of phosphorylation was associated with an increase in CSF-1R protein expression. The same waves of phosphorylation and activation of AKT and ERK 1/2 were also observed in CSF-1 and lL-34-stimulated monocytes. We have previously shown that CSF-1 triggered long term phosphorylation and activation of AMPK and ULK1 that correlated with increased autophagy in primary human monocytes10. This increased phosphorylation and activation of AMPK and ULK1 also correlated with an enhanced expression of both AMPK and ULK1 proteins (Fig. 2a). CSF-1-mediated phosphorylation and activation of AMPK and ULK1 were confirmed in the present study, but we further established for the first time that lL-34 increased AMPK and ULK1 phosphorylation at 16 and 24 h. This activation of phosphorylation was accompanied with increased expression of AMPK and ULK1 (Fig. 2a). In addition, we also investigated the effect of increasing concentrations of both cytokines on the early signaling events triggered by CSF-1R engagement and we confirmed a slightly higher sensitivity to CSF-1 (Sup Fig. 2a, please see also Sup Fig. 1c). Nevertheless, a 100 ng/mL concentration was maximal for both cytokines. We next compared the ability of CSF-1 and lL-34 to promote differentiation of monocytes. Both cytokines equivalently increased the protein expression of CD71 and CD163, two macrophage differentiation markers at 48 h (Fig. 2b). CSF-1 and IL-34 induced the activation of both caspases 8 and 3, which are a prerequisite for monocyte differentiation into macrophage and for NPM cleavage (Fig. 2b)21. We also analyzed the lipidation and cleavage of LC3-l into LC3-ll, a hallmark of autophagy induction in monocytes stimulated with CSF-1 or lL-34. Autophagy induction, that was increased after 48 h of stimulation, correlated with Cathepsin B (CTSB) activation in both CSF-1 and lL-34 treated monocytes (Fig. 2b)9. ln addition, caspase-3 activity at 3 and 6 days were found to be equivalent in CSF-1 or lL-34-treated monocytes (Fig. 2c). Furthermore, electron microscopy images of CSF-1 or lL-34 differentiated monocytes at day 3 showed accumulation of autolysosomes (Sup Fig. 2b), CTBS active fragment and increase in autophagic flux in the presence of Bafilomycin A1 (Sup Fig. 2c).
Figure 2.
Caspases and autophagy are activated upon IL-34 or CSF-1 treatment. Human peripheral blood monocytes from healthy donors were exposed to 100 ng/mL CSF-1 or 100 ng/mL IL-34 for the indicated times. (a) Immunoblot analysis of indicated proteins in monocytes following CSF-1 or IL-34 stimulation. P indicate phosphorylated proteins. Each panel is representative of at least 3 independent experiments. (b) Immunoblot analysis of indicated proteins in monocytes following CSF-1 or IL-34 stimulation. The ratio of the LC3-II protein level to that of LC3-I protein level was determined using ImageJ software. Actin was detected as the loading control. Asterisks indicate cleavage fragments. Each panel is representative of at least 3 independent experiments. (c) Caspase activity was quantified by flow cytometry analysis using DEVD-FITC. The results are expressed as the fold induction compared with untreated cells and represent the mean ± SD of 3 independent experiments performed in duplicate. n.s. denotes non-significant according to a paired student t test.
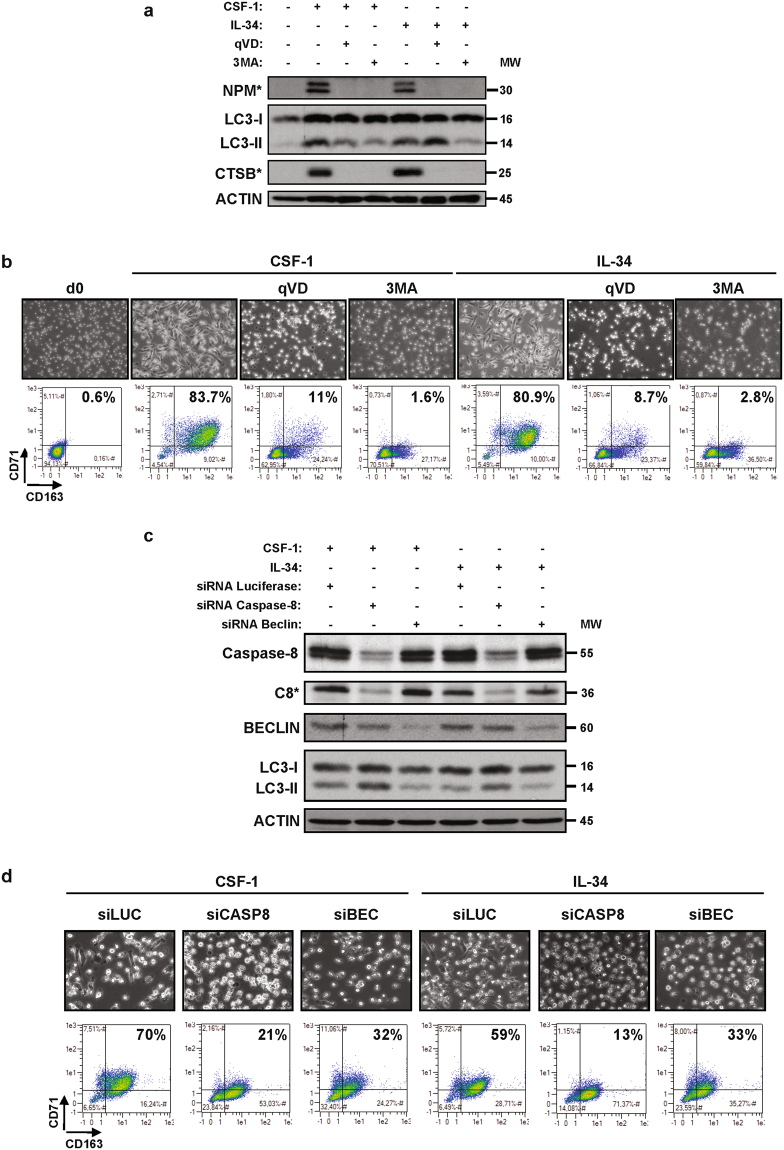
Finally, CSF-1 and lL-34 both triggered NPM cleavage, LC3-ll accumulation and CTSB activation at 2 days (Fig. 3a). Caspases or autophagy inhibition by qVD or 3MA, respectively, abolished NPM and LC3-l cleavage, CTSB activation and macrophage differentiation (Fig. 3a and b). Knock-down of caspase 8 was found to increase CSF-1 and lL-34-mediated LC3-ll accumulation while knock-down of BECLIN1 inhibited it (Fig. 3c). Importantly, caspase-8 or BECLIN1 knock-down both impaired macrophage differentiation of monocytes as shown by a reduction of the double positive CD71/CD163 population that corresponds to differentiated macrophages (Fig. 3d). In conclusion, we show that the signaling pathways involved in monocyte differentiation by CSF-1 or IL-34 are strictly identical.
Figure 3.
Caspases and autophagy are required for CSF-1 or IL-34 induced macrophagic differentiation. (a) Human monocytes were exposed for 2 days to 100 ng/mL CSF-1 or 100 ng/mL IL-34 alone or in combination with either 50 µM qVD or 3 mM 3MA (3-MethylAdenine), which were added 30 min before CSF-1 or IL-34 treatment. The expression of cleaved NPM (NPM*), LC3B and cleaved cathepsin B (CTSB*) was analyzed by immunoblotting. (b) Human monocytes were treated as in Fig. 3a. (c,d) Monocytes were transfected with siRNA targeting LUCIFERASE (LUC), CASPASE-8 (CASP8) or BECLIN (BEC) and exposed for 2 days to 100 ng/mL CSF-1 or 100 ng/mL IL-34. (c) Expression of Caspase-8, Beclin and LC3B was analyzed by immunoblotting. Actin is used as a loading control. Asterisk indicates a cleavage fragment. (d) Differentiation was examined as previously described.
CSF-1 and lL-34 macrophages exhibit differences in their ability to polarize into M1 or M2 macrophages
Globally, the results described above indicate that CSF-1 and lL-34-mediated intracellular signaling pathways, including auto-phosphorylation of the CSF-1R, activation of AKT, ERK 1/2, AMPK and ULK1 and induction of caspase activities and autophagy are similar in human primary monocytes induced to differentiate into macrophages, suggesting that the effects of lL-34 are mediated via the CSF1-R. As no obvious differences have been reported so far in the effects of CSF-1 and IL-34 on monocyte differentiation (Figs 1–3), we investigated the effects of both cytokines on macrophage polarization. Macrophages are categorized as “classically activated” pro-inflammatory M1-macrophages or an “alternatively activated” anti-inflammatory M2-macrophages22. They can differentiate into various activation states owing to the cytokine balance in their microenvironment. M1 phenotypic activation (pro-inflammatory), in response to interferon gamma (lFNγ) and lipopolysaccharide (LPS), is characterized by up-regulation of interleukin lL-6 and enhancement of the Th1 immune response. M2 phenotypic activation (anti-inflammatory) is stimulated by lL-4 and characterized by increased expression of lL-1023.
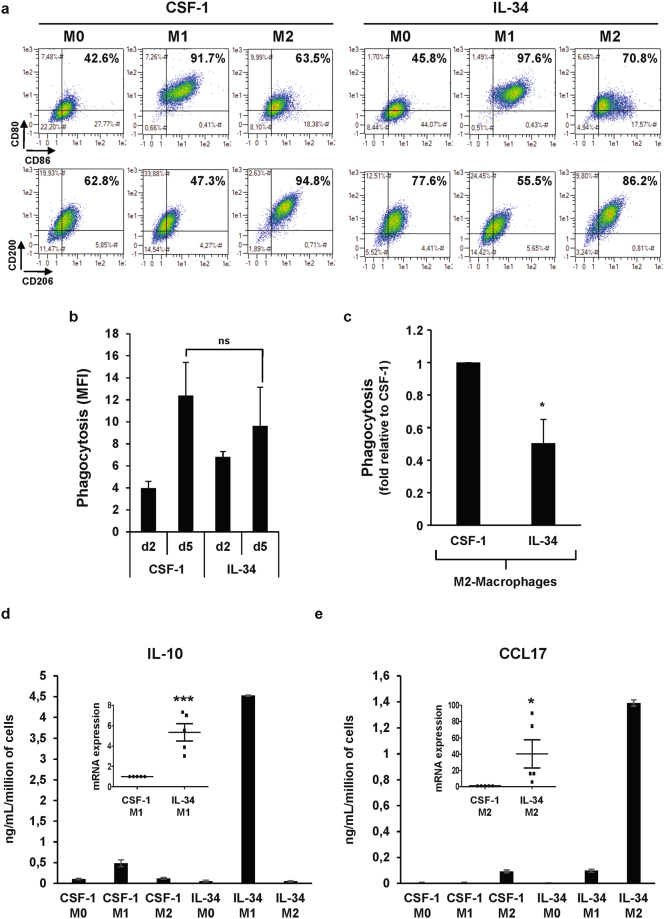
M1 or M2 polarization was initiated after 7 days of differentiation with either CSF-1 or lL-4 and next evaluated after a 2-day stimulation period with LPS + lNFγ or lL-4, respectively. ln a first series of experiments, the M1/M2 macrophage phenotype induced by lFNγ and LPS (M1 inducer) or IL-4 (M2 inducer) was analyzed by flow cytometry in macrophages differentiated with CSF-1 or lL-34. ln CSF-1 differentiated macrophages, LPS + lNFγ induced M1 polarization with both an increase in CD80 and CD86 expression and a decrease in CD200R and CD206 expression, whereas lL-4 promoted M2 polarization with an inhibition in CD80 and CD86 expression and an increase in CD200R and CD206 expression (Fig. 4a). Interestingly, whereas there was no difference in the ability of CSF-1 and lL-34 differentiated macrophages to phagocyte bacteria (Fig. 4b), M2-macrophages derived from CSF-1-stimulated monocytes exhibited a higher capacity to phagocyte bacteria than M2-macrophages derived from lL-34 differentiated macrophages (Fig. 4c).
Figure 4.
IL-34 macrophages have a different polarization potential as compared to CSF-1-macrophages. (a) Human monocytes were differentiated during 7 days with 100 ng/mL CSF-1 or 100 ng/mL IL-34 and then polarized into M1-macrophages (LPS + IFNγ) or M2-macrophages (IL-4) for 2 days. Macrophage polarization was evaluated by 2-color flow cytometric analysis. (b) Functional assay of monocytes exposed for 2 or 5 days to 100 ng/mL CSF-1 or 100 ng/mL IL-34. The results are expressed as MFI and represent the mean ± SD of 3 independent experiments performed in duplicate. n.s. denotes not statistically significant according to a paired student t test. (c) Functional assay of monocytes exposed for 7 days with 100 ng/mL CSF-1 or 100 ng/mL IL-34 and then polarized into M2-macrophages (IL-4) for 2 days. The results are expressed as the fold induction compared to CSF-1 macrophages and represent the mean of 3 independent experiments performed in duplicate. *P < 0.05 according to a paired student t test (versus CSF-1-macrophages). (d,e) Human monocytes were differentiated during 7 days with 100 ng/mL CSF-1 or 100 ng/mL IL-34 and then polarized into M1-macrophages (LPS + IFNγ) or M2-macrophages (IL-4) for 24 hours. The expression of the indicated mRNA was analyzed by qPCR (mean ± SEM of 5 independent experiments). *P < 0.05, ***P < 0.001 according to a paired student t test (versus CSF-1 macrophages). The production of IL-10 and CCL17 was analyzed using Multi-Analyte ELISArray kit as described in Material and Methods section. The results are expressed as ng/mL per million of cells and represent the mean ± SD of 2 independent experiments performed in duplicate.
To identify the cytokines that could be important for the polarization of macrophages in lL-34 stimulated monocytes, we analyzed by both real time RT-PCR and Elisa the expression level of some cytokines/chemokines known to be modulated during the M1 or M2 polarization process24–26. Regarding M1 polarization, we found a significant increase in IL-10 and CXCL11 mRNA and protein levels when IL-34 macrophages were polarized in response to LPS + IFNγ compared to CSF-1 polarized macrophages (Fig. 4d and Sup Fig. 3a). Some differences were also observed between macrophages polarized into the M2 phenotype by CSF-1 or IL-34. The most noticeable one were a very strong induction of CCL17, and CCL22, together with a decrease of IL-10 which was observed only when IL-34 differentiated monocytes were polarized into the M2 phenotype (Fig. 4e and Sup Fig. 3b). To investigate whether these differences in cytokine expression may be physiologically relevant, we analyzed the ability of M1 or M2 polarized macrophage secretomes (i.e from CSF-1 or IL-34 treated monocytes) to induce polarization of purified naïve T cells from two donors into the Th1 or Th2 phenotype. As no obvious differences were observed for Th2 polarization (not shown), we next focused on Th1 polarization. Therefore, we followed by flow cytometry the intracellular expression of IFNγ (Sup Fig. 3c and d) which is representative of Th1 cells. Of note, T cell polarization was higher in the presence of the secretome derived from M1-polarized CSF-1 macrophages as compared to M1-polarized IL-34 macrophages. Finally, the secretome derived from M2-polarized IL-34 macrophages strongly increased Th1 polarization compared to M2-polarized CSF-1 macrophages. In conclusion, although IL-34 and CSF-1 display an equivalent macrophage differentiation ability, the functionality of IL-34 and CSF-1 macrophages following polarization into the M1 or M2 phenotype is different, more specially regarding Th1 cell polarization.
Discussion
CSF-1 and IL-34 share the same receptor11, the so-called CSF-1R and no obvious differences in the downstream signaling pathways triggered by both ligands in monocytes have been reported so far27. However, some genetic evidence indicate that it could exist differences in the effect of both cytokines in myeloid cells and in the brain28,29. This is exemplified by the fact that CSF-1 deficient (CSF-1op/op) mice exhibit a less severe phenotype than their CSF-1R deficient counterpart suggesting that at least one part of the IL-34 effect could be triggered independently of the CSF-1R30. This has been recently confirmed following the identification of a second receptor for IL-34 in the brain. Indeed, IL-34 binds to and signals by an alternative receptor, namely PTP-ζ14. Moreover, it has also been reported minor differences in the production and secretion of some cytokines including eotaxin-2 in peripheral blood cells stimulated with CSF-1 or IL-3427. Although CSF-1 and IL-34 exert many redundant functions ex vivo, the profile of expression, the source and the kinetic of cytokine production are different in vivo. Indeed, in contrast to CSF-1, IL-34 shows specific expression by keratinocytes and neurons in mice and plays an important role in the development and maintenance of Langherans cells and microglia, respectively29,31. In human, IL-34 is more widely/differently expressed, albeit also highly expressed in neuronal tissues and skin (see FANTOM5 and GTEX databases). There is also increasing evidence that IL-34 expression is upregulated in pathological conditions and may play important functions in autoimmune disorders, infections, inflammation and cancer32. Regarding cancer, IL-34 promotes the recruitment of M2-polarized tumor-associated macrophages by a direct effect on CSF-1R in macrophages, promoting new vessel formation and extravasation of immune cells, as CSF-1 does33. However, clear evidence indicating different functions of both cytokines are still lacking.
In the present study, we scrutinized the effect of CSF-1 and IL-34 on human monocyte differentiation. We found that the early and late signaling pathways leading to the differentiation of monocytes into macrophages were strictly identical in both conditions. Moreover, we also described for the first time that IL-34 promotes caspase activation and the activation of the AMPK/ULK1 pathway in monocytes leading to LC3-I lipidation and cleavage into LC3-II, as CSF-1 does, confirming the similarity of action of both ligands on human monocyte differentiation and induction of autophagy.
Whereas monocyte differentiation proceeded similarly in CSF-1 and IL-34 stimulated human primary monocytes, we identified however, differences in the production of some cytokines/chemokines when cells were polarized into the M1 or M2 phenotype using LPS + IFNγ or IL-4 following macrophage differentiation by either CSF-1 or IL-34. The most noticeable examples, were increased production of IL-10 and CXCL11 at the mRNA and protein level in M1 polarized macrophages. Regarding M2 polarization, we also observed a striking induction of CCL17 and CCL22 and a decrease in IL-10 mRNA and protein expression, which were found exclusively in M2-polarized IL-34 macrophages. Therefore, despite a strictly identical profile of monocyte differentiation, the cytokines/chemokines produced by CSF-1 or IL-34 macrophages are somehow different, suggesting that macrophages generated in both conditions may have different role in pro or anti-inflammatory pathophysiological conditions.
CCL17 (TARC) was originally implicated in the selective attraction of Th2 lymphocytes and thus considered as a M2 cytokine. Recent findings in the literature have reported that human monocyte-derived macrophages grown in CSF-1 do induce CCL17 in response to IL-4 as do mouse bone-marrow-derived macrophages grown in CSF-125,26. It was also recently reported that GM-CSF drives CCL17 mRNA and protein expression in human and mice monocytes. Surprisingly, CCL17 seems to mediate at least some of the pro-inflammatory action of GM-CSF on arthritic pain and disease34. Several other cytokines including IL-435 and IL-1336 have been reported to be associated with upregulation of CCL17 mRNA and protein. The fact that CCL17 mRNA expression was selectively upregulated in macrophages differentiated in the presence of IL-34 and polarized into the M2 phenotype by IL-4 but not in their CSF-1 differentiated counterpart indicates that polarization rather than IL-4 itself is responsible for CCL17 mRNA induction in our experiments. Globally, these findings indicate that IL-34 could resemble more GM-CSF than CSF-1 in its ability to trigger M2 polarization.
IL-10 is produced by Th2 lymphocytes and is known to suppress the differentiation and effector function of Th137–39. We showed here, that IL-10 protein expression is strikingly increased in M1-polarized IL-34 macrophages compared to M1-polarized CSF-1 macrophages. This may explain the impairment of Th1 polarization observed with the secretome of M1-polarized IL-34 macrophages.
The reason for the differential effect of CSF-1 and IL-34 regarding the polarization into M1 or M2 phenotypes is currently unknown. However, a likely explanation could rely on the fact that IFNγR/TLR4 or IL-4 receptor expression is different in CSF-1 and IL-34 differentiated macrophages. We checked that it was not indeed the case (Sup Fig. 4). An alternative hypothesis would be that this specific effect of IL-34 is mediated independently of the CSF-1R. It has been described that IL-34 can bind CD138 and PTP-ζ that can act as putative IL-34 receptors. As monocytes and macrophages failed to express CD138 (syndecan 1) (Sup Fig. 4) and PTP-ζ expression seems restricted to neuronal tissues and skin, it would be interesting in future studies to investigate whether other proteoglycans such as serglycin, versican, perlecan or other syndecans40,41, including syndecan 4, could explain the differential effect of IL-34 regarding the polarization into M1 or M2 phenotypes.
In conclusion, the signaling pathways induced by CSF-1 and IL-34 downstream CSF-1R are undistinguishable. However, some differences in chemokines/cytokines production do exist when CSF-1 or IL-34 differentiated monocytes are induced to polarize into the M1 or M2 phenotypes following LPS + INFγ or IL-4 treatments. Variations in the secretome induced by CSF-1 or IL-34 may account for their different ability to polarize naïve T lymphocytes into Th1 cells. Strikingly, the increase in IL-10 production in M1-polarized IL-34 macrophages promoted a decrease in Th1 cell polarization while the increase in CCL17 and CCL22 in M2-polarized IL-34 macrophages favored an increase in Th1 cell polarization. These findings suggest that in an inflammatory context, IL-34 derived macrophages may behave differently than CSF-1 derived macrophages. Therefore, we conclude that IL-34 and CSF-1 display equivalent macrophage differentiation ability but different polarization potential.
Material and Methods
Reagents and antibodies
Human IL-34 was from Biolegend (BLE577906). Human CSF-1 was purchased from Miltenyi (130-096-493). Bafilomycin A1 was from Tocris (1334). qVD was from Clinisciences (A1901-5mg). 3-MethylAdenine was purchased from Sigma Aldrich (M9281). Phospho-CSF-1R (Tyr723), Phospho-AKT, AKT, Phospho-ERK1/2, ERK1/2, Phospho-AMPK (Thr172), AMPK, Phospho-ULK1 (Ser555), ULK1, Caspase-8, Caspase-3, Nucleophosmin, LC3-B, and Beclin antibodies were purchased from Cell Signaling Technology (catalog numbers were 3155, 4060, 9272, 4370, 4695, 2535, 2532, 5869, 8054, 9746, 9662, 3542, 2775, and 3738 respectively). CSF-1R, ACTIN, CD71, and CD163 antibodies were from Santa Cruz Biotechnology (catalog numbers were sc-692, sc-1616, sc-51829 and sc-33559 respectively). Cathepsin B was from MERCK (IM27L). HRP-conjugated rabbit anti-goat or mouse was purchased from Dako (P0449 and P0260) and HRP-conjugated goat anti-rabbit was from Cell Signaling (5127).
Human monocyte culture and differentiation
Human peripheral volunteers were obtained from healthy donors with informed consent following the Declaration of Helsinki according to the recommendations of an independent scientific review board. The project has been validated by The Etablissement Français du Sang, the French national agency for blood collection (protocol N°ALM/PLER/FO/001). Blood samples were collected using ethylene diamine tetra-acetic acid–containing tubes. Mononucleated cells were first isolated using Ficoll Hypaque (Eurobio, CMSMSL0101). Then, we used the autoMACS® Pro Separator (Miltenyi, France) to perform cell enrichment. An initial positive selection, which included antibody targeting CD14, was used for monocyte enrichment (Miltenyi, 130-050-201). Purified monocytes from human were grown in RPMI 1640 medium with glutamax-I (Life Technologies, 61870044) supplemented with 10% (vol/vol) foetal bovine serum (Life Technologies). Monocytes were seeded in tissue culture treated flasks or wells. Macrophage differentiation was induced by adding into the culture medium 100 ng/mL CSF-1 or 100 ng/mL IL-34 and was visualized using standard optics (20x/0.35 Ph1) equipped with an AxioCam ERc camera (Zeiss, France). Phase images of the cultures were recorded with the Zen 2 software (Zeiss).
Flow cytometry
To analyze the macrophagic differentiation of monocytes, cells were washed with ice-cold phosphate buffered saline (PBS, Life Technologies, 14190169), incubated at 4 °C for 10 min in PBS/bovine serum albumin (BSA 0.5%, Dutscher, 871002) with anti-CD71 and anti-CD163 or an isotype control (Miltenyi and BD Biosciences, catalog numbers were 551374 and 130-097-628). Finally, cells were washed and fixed in 2% paraformaldehyde (EMS, 15710). To detect caspase activity, we used FITC-DEVD-FMK according to the manufacturer’s instruction (Promokine, green caspase-3 staining kit, PK-CA577-K183). To perform macrophage polarization, purified monocytes were plated at 0.3 × 106 per mL in RPMI 1640 medium with glutamax-I supplemented with 10% (vol/vol) fetal bovine serum plus CSF-1 or IL-34 for 7 + 2 days to differentiate into M0 macrophages. 100 ng/mL lipopolysaccharide (LPS-EK Ultrapure, Invivogen, tlrl-peklps) and 20 ng/mL interferon gamma (Miltenyi, 130-096-484) were added after 7 days of differentiation for two days to polarize into M1-macrophages. M2-macrophages were obtained by addition of 20 ng/mL IL-4 (Miltenyi, 130-094-117) for two days. To analyze the macrophage polarization, cells were detached using PBS/EDTA/BSA, washed with PBS, and incubated at 4 °C for 10 min in PBS/ bovine serum albumin with anti-CD80 (Miltenyi, 130-097-204), anti-CD86 (Miltenyi, 130-094-877), anti-CD200R (Biolegend, 329308), and anti-CD206 (Miltenyi, 130-100-034) or isotype controls. Finally, cells were washed and fixed in 2% paraformaldehyde (EMS, 15710). Fluorescence was measured with a MACSQuant® Analyzer (Miltenyi, Paris, France). To analyze the ability of macrophages to phagocyte bacteria, we used Vybrant® Phagocytosis Assay Kit according manufacture’s instruction (ThermoFisher, V-6694). Briefly, macrophages were detached and incubated with fluorescein-labeled E. coli (K-12 strain) for 30 min. Next, cells were washed twice with PBS and resuspended in PBS. Fluorescence, that indicate the internalization of particles, was measured with a MACSQuant® Analyzers (Miltenyi, France). Trypan blue solution was used to quench the fluorescence from particles that were not internalized.
Immunoblot assays
Cells were lysed for 30 min at 4 °C in lysis buffer [50 mM HEPES pH 7.4, 150 mM NaCl, 20 mM EDTA, PhosphoSTOP (Sigma, 04906837001), complete protease inhibitor mixture (Sigma, 11836153001), 1% Triton X-100 (Sigma, T9284)]. Lysates were centrifuged at 20,000 g (15 min, 4 °C) and supernatants were supplemented with concentrated loading buffer (4X laemmli buffer). Fifty micrograms of proteins were separated and transferred following standard protocols before analysis with chemiluminescent detection kit (GE Healthcare, RPN2105).
siRNA knockdown
Small interfering (si) RNAs were introduced into monocytes by nucleoporation (Amaxa, VPA-1007) of 5 × 106 monocytes in 100 μL of nucleofector solution with 15 nmol of siRNA. Cells were incubated for 24 h with 5 mL of prewarmed complete medium, and CSF-1 or IL-34 was subsequently added. We used siRNAs (Life Technologies) targeting Caspase-8 (HSS141461), BECLIN1 (HSS112741) and LUCIFERASE as a negative control (Sense: 5′-CUUACGCUGAGUACUUCGAtt-3′).
Reverse-transcription and real-time polymerase chain reaction
RNA was prepared from 5 × 106 cells using the RNeasy Mini Kit according to manufacturer’s protocol (Qiagen, 74104). Each cDNA sample was prepared using AMV RT and random primers (Promega, M510F and C1181). Real-time polymerase chain reaction (PCR) was performed using the SyBR Green detection protocol (Life Technologies, 4367659). Briefly, 5 ng of total cDNA, 500 nM (each) primers, and 5 µL SyBR Green mixture were used in a total volume of 10 µL. Detection of multiple endogenous controls (ACTB, L32 and UBIQUITIN) were used to normalize the results. Specific forward and reverse primers are accessible upon request.
Cytokine production assay
To perform macrophage polarization, purified monocytes were plated at 0.3 × 106 per mL in RPMI 1640 medium with glutamax-I supplemented with 10% (vol/vol) fetal bovine serum plus CSF-1 or IL-34 for 7 + 1 days to differentiate into M0 macrophages. 100 ng/mL lipopolysaccharide (LPS-EK Ultrapure, Invivogen, tlrl-peklps) and 20 ng/mL interferon gamma (Miltenyi, 130-096-484) were added after 7 days of differentiation for one day to polarize into M1-macrophages. M2-macrophages were obtained by addition of 20 ng/mL IL-4 (Miltenyi, 130-094-117) for one day. Next, cells were washed and seeded in RPMI 1640 medium with glutamax-I supplemented with 10% (vol/vol) fetal bovine serum during one day. The cytokines productions were finally evaluated using MultiAnalyte ELISArray kit (Qiagen, MEH-004A and MEH-009A).
Statistical analysis
Statistical analysis was performed using a paired Student t test and significance was considered when P values were lower than 0.05. The results are expressed as the mean ± SEM.
Electronic supplementary material
Acknowledgements
This work was supported by Inserm, the Ligue Nationale Contre le Cancer, the foundation ARC (team labelled 2014–2017 and 2017–2019), the Fondation pour la Recherche Médicale, the Association Laurette Fugain and the French Government (National Research Agency, ANR) through the “Investments for the Future” Labex Signalife (ANR-11-LABX-0028-01). The authors are indebted to the Etablissement Francais du sang for providing us with human blood from healthy donors. We also thank the C3M facilities (ISO-9001 certified cytometry facility). S.B., A.P., and S.O. were supported by a fellowship from the Association pour la Recherche contre le Cancer, the Ligue Nationale Contre le Cancer, and the Fondation pour la Recherche Médicale, respectively.
Author Contributions
S.B. and A.P. designed and performed the experimental work; R.M., S.O., M.G., T.S., P.C., A.C. and N.F. contributed to some experiments; F.O. and S.L.G. realized the EM; L.B. performed functional assays; S.M., E.V., F.L., and G.R. participated in helpful discussion; and P.A. and A.J. designed the study, directed the work and wrote the paper.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Patrick Auberger and Arnaud Jacquel contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-017-18433-4.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Patrick Auberger, Email: auberger@unice.fr.
Arnaud Jacquel, Email: jacquel@unice.fr.
References
- 1.Ginhoux F, Jung S. Monocytes and macrophages: developmental pathways and tissue homeostasis. Nature reviews. Immunology. 2014;14:392–404. doi: 10.1038/nri3671. [DOI] [PubMed] [Google Scholar]
- 2.Jakubzick CV, Randolph GJ, Henson PM. Monocyte differentiation and antigen-presenting functions. Nature reviews. Immunology. 2017;17:349–362. doi: 10.1038/nri.2017.28. [DOI] [PubMed] [Google Scholar]
- 3.Sordet O, et al. Specific involvement of caspases in the differentiation of monocytes into macrophages. Blood. 2002;100:4446–4453. doi: 10.1182/blood-2002-06-1778. [DOI] [PubMed] [Google Scholar]
- 4.Stanley, E. R. & Chitu, V. CSF-1 receptor signaling in myeloid cells. Cold Spring Harb Perspect Biol6 (2014). [DOI] [PMC free article] [PubMed]
- 5.Jacquel A, Obba S, Solary E, Auberger P. Proper macrophagic differentiation requires both autophagy and caspase activation. Autophagy. 2012;8:1141–1143. doi: 10.4161/auto.20367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacquel A, et al. Colony-stimulating factor-1-induced oscillations in phosphatidylinositol-3 kinase/AKT are required for caspase activation in monocytes undergoing differentiation into macrophages. Blood. 2009;114:3633–3641. doi: 10.1182/blood-2009-03-208843. [DOI] [PubMed] [Google Scholar]
- 7.Cathelin S, et al. Identification of proteins cleaved downstream of caspase activation in monocytes undergoing macrophage differentiation. J Biol Chem. 2006;281:17779–17788. doi: 10.1074/jbc.M600537200. [DOI] [PubMed] [Google Scholar]
- 8.Rebe C, et al. Caspase-8 prevents sustained activation of NF-kappaB in monocytes undergoing macrophagic differentiation. Blood. 2007;109:1442–1450. doi: 10.1182/blood-2006-03-011585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacquel A, et al. Autophagy is required for CSF-1-induced macrophagic differentiation and acquisition of phagocytic functions. Blood. 2012;119:4527–4531. doi: 10.1182/blood-2011-11-392167. [DOI] [PubMed] [Google Scholar]
- 10.Obba S, et al. The PRKAA1/AMPKalpha1 pathway triggers autophagy during CSF1-induced human monocyte differentiation and is a potential target in CMML. Autophagy. 2015;11:1114–1129. doi: 10.1080/15548627.2015.1034406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin H, et al. Discovery of a cytokine and its receptor by functional screening of the extracellular proteome. Science. 2008;320:807–811. doi: 10.1126/science.1154370. [DOI] [PubMed] [Google Scholar]
- 12.Guillonneau C, Bezie S, Anegon I. Immunoregulatory properties of the cytokine IL-34. Cell Mol Life Sci. 2017;74:2569–2586. doi: 10.1007/s00018-017-2482-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baud’huin M, et al. Interleukin-34 is expressed by giant cell tumours of bone and plays a key role in RANKL-induced osteoclastogenesis. J Pathol. 2010;221:77–86. doi: 10.1002/path.2684. [DOI] [PubMed] [Google Scholar]
- 14.Nandi S, et al. Receptor-type protein-tyrosine phosphatase zeta is a functional receptor for interleukin-34. J Biol Chem. 2013;288:21972–21986. doi: 10.1074/jbc.M112.442731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Segaliny AI, et al. Syndecan-1 regulates the biological activities of interleukin-34. Biochim Biophys Acta. 2015;1853:1010–1021. doi: 10.1016/j.bbamcr.2015.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Chemel M, et al. Interleukin 34 expression is associated with synovitis severity in rheumatoid arthritis patients. Ann Rheum Dis. 2012;71:150–154. doi: 10.1136/annrheumdis-2011-200096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zwicker S, et al. Interleukin 34: a new modulator of human and experimental inflammatory bowel disease. Clin Sci (Lond) 2015;129:281–290. doi: 10.1042/CS20150176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ciccia F, et al. IL-34 is overexpressed in the inflamed salivary glands of patients with Sjogren’s syndrome and is associated with the local expansion of pro-inflammatory CD14(bright)CD16 + monocytes. Rheumatology (Oxford) 2013;52:1009–1017. doi: 10.1093/rheumatology/kes435. [DOI] [PubMed] [Google Scholar]
- 19.Yang S, et al. Interleukin 34 Upregulation Contributes to the Increment of MicroRNA 21 Expression through STAT3 Activation Associated with Disease Activity in Rheumatoid Arthritis. J Rheumatol. 2016;43:1312–1319. doi: 10.3899/jrheum.151253. [DOI] [PubMed] [Google Scholar]
- 20.Fan Q, et al. IL-34 is associated with the presence and severity of renal dysfunction and coronary artery disease in patients with heart failure. Sci Rep. 2016;6:39324. doi: 10.1038/srep39324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guery, L. et al. Fine-tuning nucleophosmin in macrophage differentiation and activation. Blood (2011). [DOI] [PMC free article] [PubMed]
- 22.Murray PJ, et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity. 2014;41:14–20. doi: 10.1016/j.immuni.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Locati M, Mantovani A, Sica A. Macrophage activation and polarization as an adaptive component of innate immunity. Adv Immunol. 2013;120:163–184. doi: 10.1016/B978-0-12-417028-5.00006-5. [DOI] [PubMed] [Google Scholar]
- 24.Spiller KL, et al. Differential gene expression in human, murine, and cell line-derived macrophages upon polarization. Exp Cell Res. 2016;347:1–13. doi: 10.1016/j.yexcr.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 25.Martinez FO, et al. Genetic programs expressed in resting and IL-4 alternatively activated mouse and human macrophages: similarities and differences. Blood. 2013;121:e57–69. doi: 10.1182/blood-2012-06-436212. [DOI] [PubMed] [Google Scholar]
- 26.Martinez FO, Gordon S, Locati M, Mantovani A. Transcriptional profiling of the human monocyte-to-macrophage differentiation and polarization: new molecules and patterns of gene expression. Journal of immunology. 2006;177:7303–7311. doi: 10.4049/jimmunol.177.10.7303. [DOI] [PubMed] [Google Scholar]
- 27.Chihara T, et al. IL-34 and M-CSF share the receptor Fms but are not identical in biological activity and signal activation. Cell death and differentiation. 2010;17:1917–1927. doi: 10.1038/cdd.2010.60. [DOI] [PubMed] [Google Scholar]
- 28.Barve RA, et al. Transcriptional profiling and pathway analysis of CSF-1 and IL-34 effects on human monocyte differentiation. Cytokine. 2013;63:10–17. doi: 10.1016/j.cyto.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 29.Greter M, et al. Stroma-derived interleukin-34 controls the development and maintenance of langerhans cells and the maintenance of microglia. Immunity. 2012;37:1050–1060. doi: 10.1016/j.immuni.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dai XM, et al. Targeted disruption of the mouse colony-stimulating factor 1 receptor gene results in osteopetrosis, mononuclear phagocyte deficiency, increased primitive progenitor cell frequencies, and reproductive defects. Blood. 2002;99:111–120. doi: 10.1182/blood.V99.1.111. [DOI] [PubMed] [Google Scholar]
- 31.Wang Y, et al. IL-34 is a tissue-restricted ligand of CSF1R required for the development of Langerhans cells and microglia. Nat Immunol. 2012;13:753–760. doi: 10.1038/ni.2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baghdadi M, Endo H, Tanaka Y, Wada H, Seino KI. Interleukin 34, from pathogenesis to clinical applications. Cytokine. 2017;99:139–147. doi: 10.1016/j.cyto.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 33.Segaliny AI, et al. Interleukin-34 promotes tumor progression and metastatic process in osteosarcoma through induction of angiogenesis and macrophage recruitment. Int J Cancer. 2015;137:73–85. doi: 10.1002/ijc.29376. [DOI] [PubMed] [Google Scholar]
- 34.Achuthan A, et al. Granulocyte macrophage colony-stimulating factor induces CCL17 production via IRF4 to mediate inflammation. The Journal of clinical investigation. 2016;126:3453–3466. doi: 10.1172/JCI87828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liddiard K, et al. Interleukin-4 induction of the CC chemokine TARC (CCL17) in murine macrophages is mediated by multiple STAT6 sites in the TARC gene promoter. BMC Mol Biol. 2006;7:45. doi: 10.1186/1471-2199-7-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crapster-Pregont M, Yeo J, Sanchez RL, Kuperman DA. Dendritic cells and alveolar macrophages mediate IL-13-induced airway inflammation and chemokine production. J Allergy Clin Immunol. 2012;129:1621–1627 e1623. doi: 10.1016/j.jaci.2012.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang, X., Wong, K., Ouyang, W. & Rutz, S. Targeting IL-10 Family Cytokines for the Treatment of Human Diseases. Cold Spring Harb Perspect Biol (2017). [DOI] [PMC free article] [PubMed]
- 38.Fiorentino DF, Zlotnik A, Mosmann TR, Howard M, O’Garra A. IL-10 inhibits cytokine production by activated macrophages. Journal of immunology. 1991;147:3815–3822. [PubMed] [Google Scholar]
- 39.Mosser DM, Zhang X. Interleukin-10: new perspectives on an old cytokine. Immunol Rev. 2008;226:205–218. doi: 10.1111/j.1600-065X.2008.00706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chang MY, et al. Monocyte-to-macrophage differentiation: synthesis and secretion of a complex extracellular matrix. J Biol Chem. 2012;287:14122–14135. doi: 10.1074/jbc.M111.324988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wegrowski Y, et al. Cell surface proteoglycan expression during maturation of human monocytes-derived dendritic cells and macrophages. Clin Exp Immunol. 2006;144:485–493. doi: 10.1111/j.1365-2249.2006.03059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.