Abstract
Objectives
As part of a series of Patient‐Centered Outcomes Research Institute‐funded large‐scale retrospective observational studies on bipolar disorder (BD) treatments and outcomes, we sought the input of patients with BD and their family members to develop research questions. We aimed to identify systemic root causes of patient‐reported challenges with BD management in order to guide subsequent studies and initiatives.
Methods
Three focus groups were conducted where patients and their family members (total n = 34) formulated questions around the central theme, “What do you wish you had known in advance or over the course of treatment for BD?” In an affinity mapping exercise, participants clustered their questions and ranked the resulting categories by importance. The research team and members of our patient partner advisory council further rated the questions by expected impact on patients. Using a Theory of Constraints systems thinking approach, several causal models of BD management challenges and their potential solution were developed with patients using the focus group data.
Results
A total of 369 research questions were mapped to 33 categories revealing 10 broad themes. The top priorities for patient stakeholders involved pharmacotherapy and treatment alternatives. Analysis of causal relationships underlying 47 patient concerns revealed two core conflicts: for patients, whether or not to take pharmacotherapy, and for mental health services, the dilemma of care quality vs quantity.
Conclusions
To alleviate the core conflicts identified, BD management requires a coordinated multidisciplinary approach including: improved access to mental health services, objective diagnostics, sufficient provider visit time, evidence‐based individualized treatment, and psychosocial support.
Keywords: bipolar disorder, operational excellence, patient priorities, patient‐centered, systems thinking, Theory of Constraints
1. INTRODUCTION
Challenges in bipolar disorder (BD) management shared by psychiatrists and patients across the USA include poorly controlled mood episodes, incomplete remission with cognitive decline, social dysfunction, and diminished quality of life.1, 2, 3 The problems faced by patients are broader than a range of symptoms targeted by available pharmacologic and psychosocial treatments, and, for many, reflect the lived negative experience of low self‐esteem, impaired sense of identity, isolation, and social stigma, all of which can be exacerbated by inadequate mental health care.4, 5 Many of these aspects have not been fully investigated since research priorities are traditionally based on factors such as disease burden, health costs, feasibility of approach and its novelty, interests of donors and advocacy groups, and experts’ opinions, rather than on patients’ perspectives and concerns.6, 7 The gap between research objectives and the real needs expressed by patients is emphasized by many authors,8, 9 and this bias has been identified as a major shortcoming of previous research.10 The value of stakeholder engagement in research is now commonly recognized, and extensive analysis of its practical implementation, methodology and evaluation has been performed.11, 12 Involvement of patients in research agendas is increasingly implemented on a legislative basis in developed countries,13 making patients not just “passive beneficiaries” but active participants in planning, designing, and evaluating research, as well as dissemination of its results. Three major justifications underlie this approach: (i) unique experiential knowledge brought by patients and their caregivers can elevate the quality and practical relevance of performed research; (ii) shared involvement of patients as consumers, taxpayers, voters and citizens increases trust in research findings and the legitimacy of decision‐making; and (iii) mutual learning between all stakeholders is conducive to a shared and more objective view of the disease phenomena.14, 15
New initiatives have been launched in Europe, North America, and Australia15, 16 stressing multi‐stakeholder engagement in research, with mental health being the second leading sphere following oncology.13 Efforts within the USA include the Patient‐Centered Outcomes Research Institute (PCORI), the Depression and Bipolar Support Alliance (DBSA), the Clinical Trials Transformation Initiative, the Patient Engagement Advisory Committee of the Food and Drug Administration's Center for Devices and Radiological Health, and the Center for Patient & Consumer Engagement at the American Institutes for Research.
The most extensive assessment of the concerns of patients with BD can be found in the Priority Setting Partnership (PSP) model of the James Lind Alliance (JLA), in the UK. The study focused on priorities in BD research related to causes, diagnosis, treatment, support and prognosis in 3283 patients, caregivers and health care professionals who, through surveys, submitted 14 492 questions targeting these categories. The resulting list of “top 10” priorities for BD research included BD causality, individualized treatment, and a combination of self‐management approaches, therapy and medication.17
A study addressing US patients’ greatest BD treatment concerns showed that major unmet needs include treatment of depression, followed by treatment access, affordability, relapse prevention, and treatment of mania and hypomania.18 Top issues in a DBSA survey on patient−provider relationships were lack of: communication, collaboration, and recovery‐oriented treatment that instills hope.4 A patient‐centered Canadian study on quality of life found that BD patients consider social support as the most important factor, followed by mental health, financial status, vocation and independence.5
Despite the abovementioned impressive efforts to build and prioritize large lists of BD patient concerns, and the growing use of systems approaches in psychiatric practice and research,19, 20, 21 we have not found published attempts to: (i) integrate patient concerns into a causal model, and (ii) involve patients in the model building. Systems thinking approaches illustrate that effects are often several steps removed from causes, and, because of interdependences, myriad “symptoms” can result from very few root causes which have the greatest leverage for system improvement once addressed. Thus, the objective of the study was to engage with our patient partners to understand the large “symptoms” in BD management, and to propose models that highlight root causes where limited resources can be deployed to achieve the highest impact.
2. PATIENTS AND METHODS
This study was conducted under a PCORI‐funded research project “Longitudinal comparative effectiveness of bipolar disorder therapies” (ClinicalTrials.gov identifier: NCT02893371)—a retrospective observational study of the long‐term effects of commonly used pharmacological treatment options for BD, using Truven Health Analytics MarketScan® (Ann Arbor, MI, USA) administrative claims data on over 1 million US BD patients.22 Patient‐engaged research was facilitated through a patient partner advisory council (PPAC), which included representatives of the National Alliance on Mental Illness (NAMI), patients with BD, and their advocates.
In order to elucidate patients’ perspectives on and concerns about BD management, and to elicit research questions of particular importance for them, three half‐day focus groups were conducted between October 2016 and February 2017 in Montana, New Mexico, and California. Recruitment of participants was conducted via NAMI in each state by means of social networks, emails, and phone calls. The inclusion criteria were diagnosis of BD or first‐degree relative with BD, age ≥18 years, and the ability to understand and speak English. The New Mexico and California focus groups each had one no‐show. All of the groups were conducted by the study principal investigator (CGL) and a second facilitator in the presence of a licensed mental health practitioner. In the Montana focus group, the second facilitator was an NAMI representative with BD (ANS). The study protocol was approved by the University of New Mexico Human Research Review Committee (Institutional Review Board number 16‐243); signed informed consent was obtained from each participant. Each individual received a $450.00 Amazon merchandise card for participation.
The focus groups were all structured in the same way: a brief introduction of participants was followed by an overview of the project describing the observational study design and goals. Participants were then invited to perform an affinity mapping exercise23 to solicit questions of interest for BD patients and their family members. They were asked to independently formulate their questions, write them on sticky notes and place them on a wall. Questions were centralized around the theme “What do you wish you had known in advance or over the course of treatment for BD?” Examples of the questions that could be answered from the available research data were provided. Each person could generate as many questions as he/she wanted. Once the notes had been placed on the wall, participants were asked to manually cluster them into similar categories. They were encouraged to relocate the notes as needed to cluster the questions, but not to discuss the process verbally. Next, participants were encouraged to suggest descriptive titles to name each category in a group discussion format; some of the categories were united under a common header as a super‐category. As a final step, each participant was asked to score his/her perceived top three categories by importance from 1 (minimal) to 3 (maximal) by placing a sticky note with the relevant number next to the category. The category scores were summed, and, prior to closing the focus group, participants discussed the overall rankings and were encouraged to share their thoughts about their experience with the focus group. The detailed procedure with structured questions can be found in DataS1.
The resulting list of 369 questions and statements was shortened to 312 items with interrogative content to enable further prioritization of research questions. The research team assessed each item to determine if the Truven Health Analytics MarketScan® administrative claims data could provide insight into patients’ concerns. Each researchable question in the final data set was further independently scored on a five‐point Likert scale by eight patient stakeholders (PPAC members and one researcher with BD) and eight members of the research team (referred to as researcher stakeholders), based on the expected impact of answering the questions on individuals with BD and their families. Questions that were similar and had a common approach to answering were grouped together and rated with a single score. The top 10 questions were selected for research stakeholders, patient stakeholders and for both groups of raters based on the average score.
During a videoconference, research team and PPAC members collaboratively reviewed the original list of 369 focus group questions and statements and distilled 47 patient concerns or undesirable effects (UDEs) of BD management behind each of the focus group item clusters. Each of the UDEs served as concepts for building causal models of BD management challenges and their solution using the Theory of Constraints logical thinking process.24, 25, 26 This process allows concomitant analysis of many systems/organizational problems to identify the few common causes to most or all of the identified UDEs, where interventions will produce the greatest improvement in the symptoms.
The Theory of Constraints thinking process for system improvement follows several steps.24 First, a current reality tree (CRT) is built by: (i) connecting all UDEs within a single tree with arrows, reflecting cause−effect relationships; (ii) inserting additional entities to support the causal relationships with facts from reality; (iii) scrutinizing the logic; and (iv) identifying the root cause(s) that lead(s) to the majority of UDEs. Then, a CRT is transformed into a communication current reality tree (CCRT) diagram by forming a core conflict between a root cause and its mutually exclusive alternative, and simplifying the tree to its essential elements. A future reality tree (FRT) is then created as an action plan to resolve the conflicts by introducing hypothesized interventions that are expected to invert the negative UDEs into positive results.
Using this process, a CRT model was drafted by the joint efforts of the research team and PPAC members, refined and simplified to two CCRTs and corresponding FRTs by researchers, and finalized through PPAC feedback.
3. RESULTS
A total of 34 individuals participated in the focus groups; 24 of them had BD and 11 had a close family member with BD. The characteristics of the participants are shown in TableS1. Consistent with BD heterogeneity and complexity, 12 participants also reported comorbid mental disorders, including obsessive‐compulsive disorder, major depressive disorder, social phobia, post‐traumatic stress disorder, adjustment disorder, schizoaffective disorder, alcohol and substances abuse, epilepsy and Tourette's syndrome.
A total of 369 questions and statements resulted from the affinity mapping exercise, which were grouped into 33 categories across the three focus groups (TableS2). The top‐ranked categories were Medications in the Montana focus group, Education in the New Mexico group and Doctor communication/collaboration in the California group. The second most highly ranked categories were represented by Other Treatments, Diagnosis and research and Holistic options, respectively. Given that many of the 33 categories had overlapping content and similar names, they were subsequently grouped by researchers into 10 broader “themes”, which were ranked by summing the constituent patient category scores. The top three themes were Alternatives and adjuncts to pharmacotherapy, Pharmacotherapy and Provider relations (Table 1). We found that 176 out of the 312 items with interrogative content (56%) were at least partly answerable with the available data, all of which were categorized into one of the 10 newly defined broad themes.
Table 1.
The highest rated research questions (and interrogative statements) for each theme. The questions were scored by patient and researcher stakeholders based on the potential impact of their answering on individuals with bipolar disorder (BD). For groups of similar questions that have a common approach to answering, only one question is shown, most precisely reflecting the inquiry content. One theme might have several top‐rated questions with equal average score
| Theme rank and (summary score) | Theme | Top question (Q) for researcher stakeholders (average score) | Top question (Q) for patient stakeholders (average score) |
|---|---|---|---|
| 141 | Alternatives and adjuncts to pharmacotherapy | Q: “What are the risks of takings medications or not?” (4.6) | Q: “What are the risks of takings medications or not?” (4.8) |
| 235 | Pharmacotherapy | Q: “What can be done to eliminate suicidal thoughts with some medications?” (4.8) |
Q: “Medications: how do you get the right cocktail?” (5.0) Q: “What are the safest medications to take first?” (5.0) |
| 324 | Provider relations | Q: [To doctor:] “How can you better understand my condition and what information will help you in ‘fine tuning’ my treatment?” (4.0) | Q: [To doctor:] “How can you better understand my condition and what information will help you in ‘fine tuning’ my treatment?” (4.6) |
| 423 | Understanding BD | Q: “Would have been good to know severity of symptoms, especially dangers.” (4.5) |
Q: “Would have been good to know severity of symptoms, especially dangers.” (4.6) Q: “What will happen to me?” (4.6) Q: “Education at the start of treatment structured, i.e. NAMI etc., for patient/consumer.” (4.6) |
| 521 | Support | Q: “I wish they would've shown me where to find support when suicidal.” (3.9) | Q: “I wish they would've shown me where to find support when suicidal.” (4.3) |
| 614 | Health care system navigation | Q: “How do I find the right doctor?” (3.3) |
Q: “How do I find the right doctor?” (4.3) Q: “How often should bipolar patients talk to their psychiatrist?” (4.3) |
| 713 | Diagnosis | Q: “Diagnosed earlier.” (4.1) | Q: “How do you know I'm [this] diagnosis?” (4.0) |
| 88 | BD coping/management |
Q: “How should I manage a manic episode?” (4.3) Q: “How to stop bad thoughts and dreams?” (4.3) |
Q: “How should I manage a manic episode?” (4.8) |
| 98 | Social bias and stigma | Q: “I would have asked for more education for all family members including siblings (under 18).” | Q: “I would have asked for more education for all family members including siblings (under 18).” |
| 106 | Other (“Big ideas” and “Children”) | Q: “[Are] side effects different for young children?”/”I want to know how puberty affects medication efficacy.” (4.4) |
Q: “[Are] side effects different for young children?”/”I want to know how puberty affects medication efficacy.” (4.6) Q: “Would have asked about alternative treatments for children.” (4.6) Q: “What are the early warning signs for bipolar for teenagers?” (4.6) |
NAMI, National Alliance on Mental Illness.
The top 10 jointly rated questions/interrogative statements were placed in the following order by descending average score: “What can be done to eliminate suicidal thoughts with some medications?” (4.8), “What are the risks of taking medications or not?” (4.7), “Medications: how do you get the right cocktail?” (4.7), “Which are the safest medications to take first?” (4.7), “When it is too much medication” (4.6), “What is the efficacy of my treatment?” (4.6), “Would have been good to know severity of symptoms, especially dangers” (4.6), “How should I manage the manic episode?” (4.5), “Which antipsychotic works best for me [in combination with other drugs that I am taking]?” (4.5), and “How will the drugs interact with each other?” (4.5). Comparison of the top 10 questions of research stakeholders vs those of patient stakeholders showed that there were six in common. The unique questions stressed by patient stakeholders were related to polypharmacy, optimal drug dosage, manic episode management and head‐to‐head comparison of individual drugs; the unique questions stressed by researcher stakeholders were related to BD treatment efficacy in general, BD “dangers”, interaction of BD drugs with psychoactive substances, and pharmacotherapy in children (see TableS3).
Questions that scored the highest within each of the 10 broad themes are provided in Table 1 (separately for patient and researcher stakeholders). Eight out of 10 top‐rated questions matched for patient and researcher stakeholders, although in some cases they were accompanied by other questions with an equal average score. The full list of scored questions can be found in TablesS4–S13.
To analyze the systemic challenges experienced by BD patients and their family members, we built two CCRT diagrams and corresponding FRT diagrams as described in the Patients and Methods section. The first CCRT identified a central conflict between two mutually exclusive behaviors: seeking vs avoiding pharmacological treatment (Figure 1). A corresponding FRT (“Treatment leads to wellness”) was then constructed to convert the negatives into positives as a consequence of removing or alleviating root causes (Figure 2). In Figure 1, we created three major groupings of UDEs, shown in red, that were reported by the focus group participants. Two of them result from patients’ treatment choice and associated risks, and the third (dashed red lines) reflects the deleterious contribution of mental health care not addressing patients’ needs, which is expanded into a second CCRT (Figure 3) and associated FRT (Figure 4).
Figure 1.
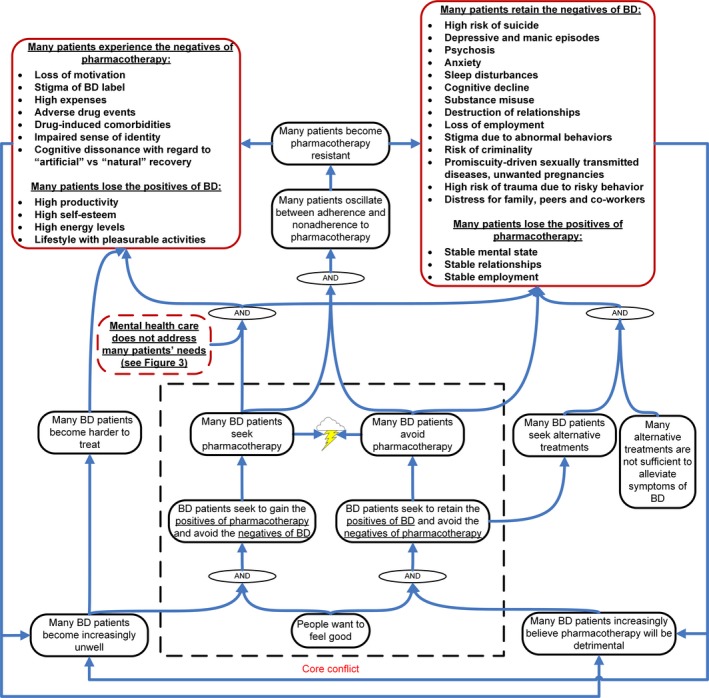
Seeking vs avoiding pharmacotherapy. A communication current reality tree (CCRT) reflecting bipolar disorder (BD) management challenges experienced by patients with BD and their family members is shown. Undesirable effects (UDEs) are framed in red rounded rectangles, and additional entities in black rounded rectangles. The red rounded rectangle with dashed lines represents a cluster of UDEs that are further expanded in Figure 3. Arrows signify direct causal relationships; arrows directed to “AND” operators imply that the combination of causes is needed to produce the resulting effect. The lightning sign reflects a conflict between mutually exclusive alternatives [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 2.
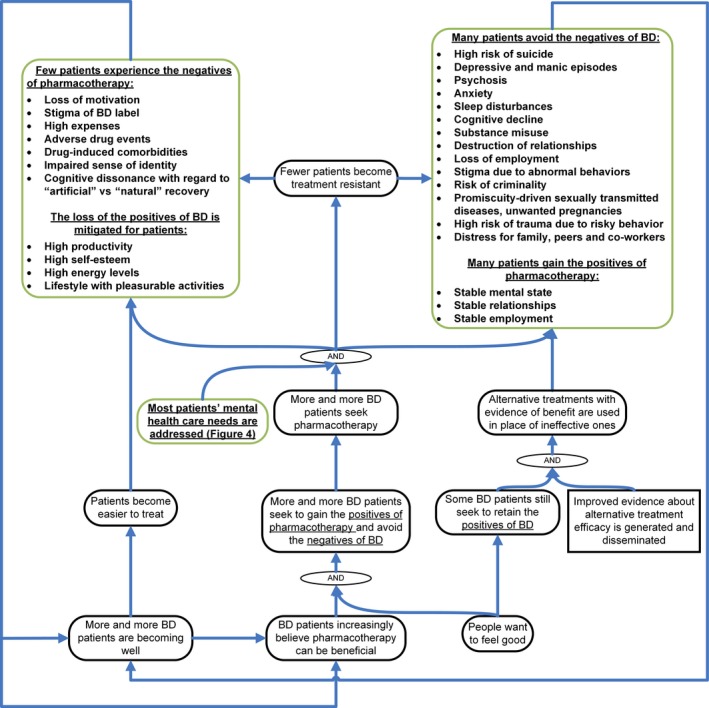
Treatment leads to wellness. A future reality tree (FRT) reflecting potential improvements in bipolar disorder (BD) care management is shown. Positive changes are framed in green rounded rectangles, additional entities in black rounded rectangles, and system interventions in square rectangles. Arrows signify direct causal relationships; arrows directed to “AND” operators imply that the combination of causes is needed to produce the resulting effect [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 3.
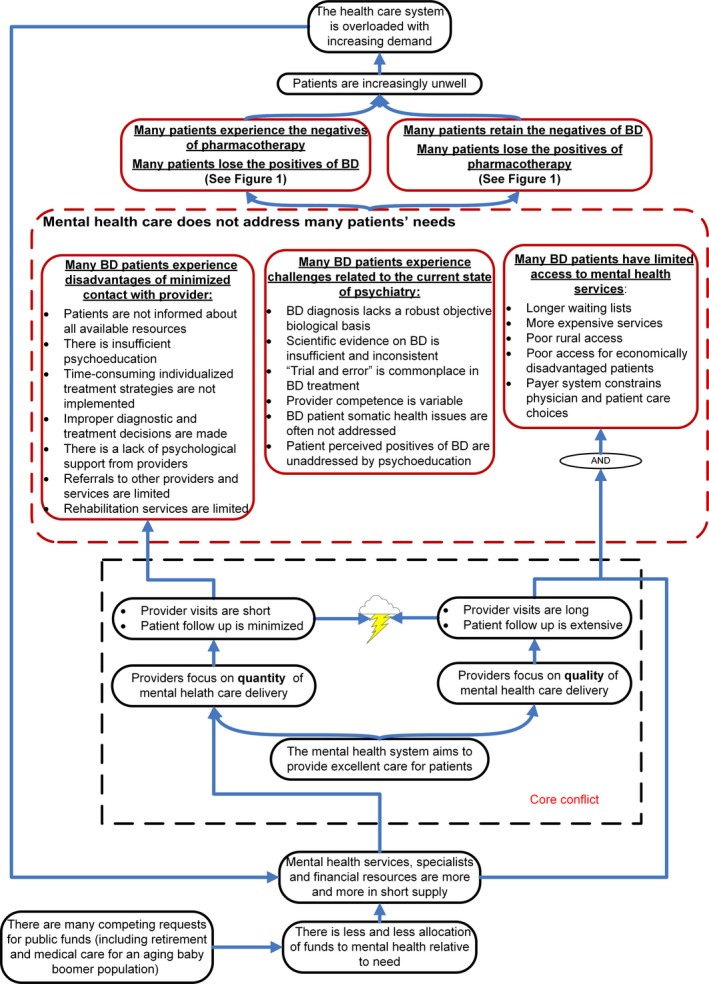
Quality vs quantity. A communication current reality tree (CCRT) reflecting causal relationships underlying patients’ experience that mental health care does not address their needs is shown. Undesirable effects (UDEs) are framed in red rounded rectangles, and additional entities in black rounded rectangles. Arrows signify direct causal relationships; arrows directed to “AND” operators imply that the combination of causes is needed to produce the resulting effect. The lightning sign reflects a conflict between mutually exclusive alternatives. The UDEs at the top of the tree are the same as in Figure 1, but represented in shortened form [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 4.
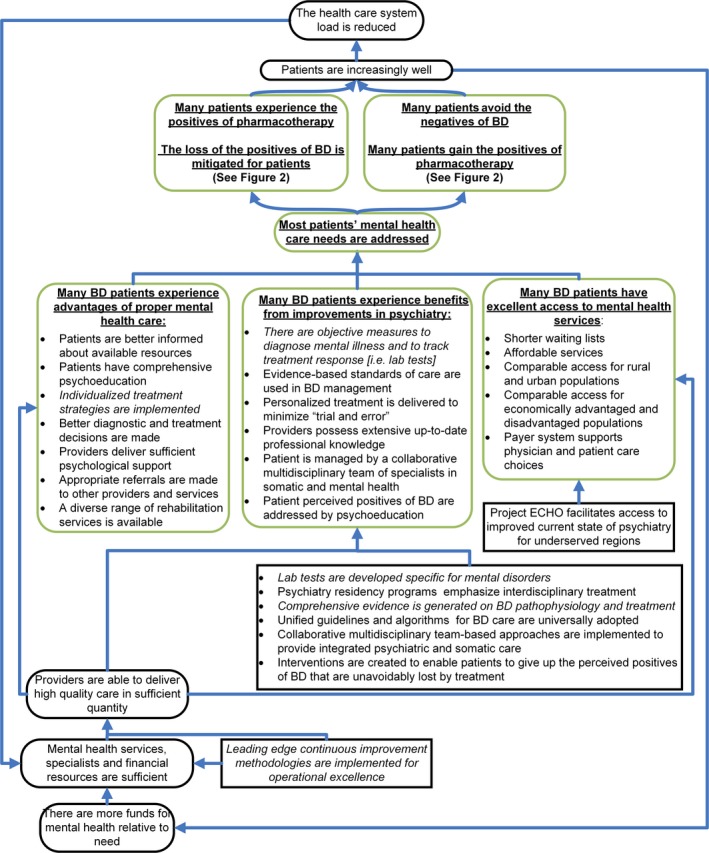
System overhaul. A future reality tree reflecting potential interventions to produce bipolar disorder (BD) management success is shown. Positive changes are framed in green rounded rectangles, additional entities in black rounded rectangles, and system interventions in square rectangles. Interventions shown in italics are being developed but are not yet ready for practical implementation. Arrows signify direct causal relationships; arrows directed to “AND” operators imply that the combination of causes is needed to produce the resulting effect. ECHO, Extension for Community Healthcare Outcomes [Colour figure can be viewed at wileyonlinelibrary.com]
The base of Figure 1 starts with the basic need, “People want to feel good”. In that context, three alternative modes of goal‐directed behavior emerge. The first two modes—seeking vs avoiding pharmacotherapy—constitute the central conflict in decision‐making which arises from weighing the positives and negatives of either strategy. It causes many patients to oscillate between adherence and nonadherence to prescribed treatment. Discontinuous use of medications is known to increase the risk of drug resistance, which might worsen disease outcomes.27 The third mode is to seek alternative nonmedicamentous remedies, many of which have limited efficacy in alleviating BD symptoms, resulting in the loss of pharmacotherapy benefits and retaining the negatives associated with BD.28 Given that, from our patients’ perspective, mental health care often does not meet their needs, choosing pharmacotherapy can lead to additional negative consequences, including the UDEs of both medications and BD without the advantages from either. A negative experience with medication could reinforce a patient's belief that pharmacotherapy will be detrimental, which fosters the medication‐free behavioral strategies. On the other hand, BD untreated or treated with ineffective drugs tends to progress, which motivates patients to seek pharmacotherapy, but makes the disorder harder to treat.
The next step was to propose transformations to the CCRT where some of the root causes are eliminated or alleviated and new actions are introduced to convert the negatives into positives, forming an FRT (Figure 2). Assuming that significant systemic improvements are made (see the relevant conflicts and their solutions in Figures 3 and 4) so that mental health care addresses patients’ needs, improved pharmacotherapy outcomes are more probable. A positive experience with psychiatric care would lead patients to be more likely to continue to seek professional help in order to gain the benefits of pharmacotherapy and avoid the negative consequences of BD. However, some patients will still be inclined to keep the benefits of BD and try to seek alternative treatments. With better evidence on the alternative strategies, more efficacious ones could be employed, either alone or adjunctively with pharmacotherapy. As a result, more patients will gain the benefits of pharmacotherapy than will experience its undesirable effects, and the adverse consequences of being untreated will be reduced or eliminated. Even without a guaranteed adequate response to treatment, optimal management of BD would promote patient well‐being and diminish the risk of complications or drug resistance, improving outcomes. An increased rate of favorable outcomes leads to a positive reinforcement of perceptions that pharmacotherapy is worthwhile, leading to a virtuous cycle of improved health for BD patients.
Causes for the cluster of UDEs “Mental health care does not address many patients’ needs” in Figure 1 were elucidated in a second CCRT (Figure 3). The model in Figure 3 shows how resource limitations give rise to a conflict for providers over the quality vs quantity of mental health care.29 Mutually exclusive standards of service related to physician visit time lead to two major negative outcomes: the disadvantages of minimized contact with a specialist and lack of specialist access. This conflict, as well as a cluster of factors related to shortcomings of the current state of psychiatry, contribute to both the detrimental outcomes and lack of benefits reported by patients, as detailed in Figure 1. Uncontrolled BD symptoms result in increased demand from the mentally ill population for mental health services, system overload and further reinforcement of the efficiency‐focused strategy to cope with the increased consumption of services.
A need for systemic reformation of mental health care services was explicitly stated by the focus group participants during closing discussions. Focus group participants indicated difficulties with lack of comprehensiveness of care, and the need for a coordinated approach to address the problems identified. When the CCRT (Figure 3) was transformed into the FRT (Figure 4), interventions were proposed to improve the overall performance of mental health care for individuals with BD and their families. These included multi‐level solutions ranging from biomarker development to reforms in education, standardization of diagnostic and treatment algorithms, and implementation of continuous improvement processes to achieve operational excellence.
4. DISCUSSION
The major contribution of this paper is the proposal of causal models that integrate patient‐driven research priorities into a comprehensive framework for focused intervention. While it is useful, for example, to discover that a top priority for focus group participants is alternative nonmedicamentous treatments, a deeper understanding that this effect may be explained by a core conflict over seeking vs avoiding pharmacotherapy, in the context of unsatisfactory care and disappointing therapeutic results, opens up avenues for new research and productive dialog.
Prioritization of research questions generated from the focus groups showed that major concerns expressed by individuals with BD and their family members are largely held in common with other patients, patient advocates and researchers. Seven out of ten major priorities of patient and researcher stakeholders fell under Pharmacotherapy, one of the two themes marked as most important by participants. The importance of BD pharmacotherapy is supported not only by the high burden of patients’ suffering from drugs’ unwanted effects and failure to bring expected relief, but also by its fundamental causal input into the majority of reported UDEs covering social, occupational, physical and psychological spheres of the patient's life not overtly linked to drug exposure (Figure 1). The detrimental potential of BD medication has two modes: on the one hand, it can cause adverse events and change perception of self‐identity; on the other hand, lack of efficacy exposes patients to the risks associated with depressive and manic episodes and deprives them of the expected benefits that could otherwise be obtained with another drug. Both types of negative outcome are driven by mental health care not addressing patient needs due to insufficient provider contact, poor access and/or deficiencies in the field of psychiatry. Concerns related to lack of individualized treatment and polypharmacy stem from unsuitable treatment decisions which, in turn, are driven by incomplete evidence, and insufficient patient contact. Concerns regarding drug interactions, safety and efficacy, dosage, antisuicidal and age‐specific properties require improvements in the current state of psychiatry, where scientific evidence is still insufficient and inconsistent, and existing pharmacological agents have limited efficacy and numerous side effects.30
Another top priority shared among patient stakeholders and focus group participants was Alternatives and adjuncts to pharmacotherapy. Being unsatisfied with their pharmacotherapy experience, many patients seek to gain the perceived benefits of exercise, nutrition, mindfulness, and psychoactive substances (e.g., alcohol, cannabinoids and lysergic acid diethylamide [LSD]), as well as a host of nontraditional medicine approaches. This represents one of the three behavioral strategies leading to negative BD outcomes (Figure 1). Patient stakeholders expressed the need for more evidence on the full range of available options and their comparative safety and efficacy.
Our findings regarding the top priorities in BD research are consistent with those of the JLA study,17 where six of their top 10 questions were related to individualized pharmacotherapy, its effectiveness and safety, its combination with other treatments and alternative options to address drug resistance. Similar results were obtained in an Australian study on patients with depression and BD, which identified medication as the most important topic for research.16
Patients’ concerns related to “Provider relations”, “Understanding BD”, “Support”, “Diagnosis” and “Social bias and stigma” can be traced to a common cause of the provider's focus on care quantity (Figure 3), where short visit times compromise comprehensive examination, patient and family psychoeducation, psychological support and appropriate referrals. Unproductive dialog with physicians drives patient inquiries about finding an appropriate provider, which represents a major concern under the “Health care navigation” theme.
In order to improve BD management, it is important not only to prioritize UDEs, but also to analyze their complex causal interrelationships as a system. The majority of concerns reported in the focus groups converge to two major conflicts between alternative action strategies for the provider and patient. The downstream consequences of the provider's conflict contribute crucially to the negative outcomes of the patient decision to receive pharmacotherapy, reinforce nonadherence and drive the demand for alternative BD treatments. Thus, the provider's conflict of quality vs quantity (Figure 3) sustains the patient's conflict of seeking vs avoiding pharmacotherapy (Figure 1).
When deciding on treatment involvement and collaboration with mental health services, the patient weighs the pros and cons of both BD and pharmacotherapy (Figure 1). Subjectively perceived BD advantages may be an important argument for patients to avoid medications; that is, treatment jeopardizes an individual's positive image of “self” supplemented by a sense of empowerment, high energy levels and high productivity, compounded by a lack of insight that these “benefits” are symptoms of disease.31 This rationale behind medication nonadherence is often unrecognized, and patient noncompliance is commonly attributed to ignorance, lack of insight and motivation, negative memories bias, or focus on short‐term needs.32, 33 We suggest that this particular aspect of decision‐making should become an important target of education for patients with BD and their families. However, additional research is needed to elucidate its role in BD outcomes, and additional psychosocial interventions should be developed in order to alleviate the loss of the perceived positives of BD.
Many of the proposed interventions to improve mental health care identified in Figure 4 already exist, but from our patients’ experience are not implemented comprehensively. The current literature reports advances in development of BD biomarkers34 and evidence on alternative treatments such as circadian‐based therapies, vagus nerve stimulation, and omega‐3 fatty acid supplementation.35, 36, 37, 38 New evidence is available on BD‐specific psychological interventions,39, 40 psychoeducation41 and individualized treatment42optimized by E‐health applications43 and stage‐appropriate interventions.44, 45 A range of guidelines and practical algorithms have been produced for pharmacological treatment of BD,46, 47, 48 although none have been broadly adopted in the USA. Evidence‐based collaborative care models (CCMs) have been developed where a “care manager” mediates the interplay between patient, provider and community services. Such treatment delivery systems facilitate access to mental health services, support providers with guidelines, provide standardized patient education, and enable ongoing monitoring of the patient's state with timely reports to his/her treating physician. When tested in long‐term randomized controlled clinical trials, CCMs significantly reduced the length and severity of manic episodes, and improved patients’ social functioning, quality of life, and treatment satisfaction.49, 50
In the last decade, continuous improvement methodologies from manufacturing have begun to be adapted to health care systems, to alleviate the demand on health care services relative to supply. Methodologies such as Lean, Six Sigma, and Theory of Constraints have in many cases dramatically improved both quality and throughput of patient care by capitalizing on existing resources, reducing waste and variability, and locating rate‐limiting steps in operational performance.51, 52 By redesigning systems, changing policies, and redeploying resources, it is possible to significantly increase capacity with limited cost increases. Although operational excellence methodologies are in their early stages of implementation in the health care system, more evidence on their utility should be generated in mental health services where the literature is sparse.
An important insight from patient discussions is that BD management needs a coordinated approach that accounts for multiple aspects of patient−provider interaction, including policy making, standards of care, treatment alternatives, patient education, psychosocial support, objective diagnostics and individualized treatment. Psychiatric research should focus on matters of the greatest concern for patients and their caregivers, such as comparative efficacy and safety of existing BD medications and alternative treatments. Appropriate organizational decisions need to be made by providers to integrate the progress achieved in psychoeducation, psychosocial support and collaborative care into clinical practice and to adopt effective principles of operational excellence to improve both quality and quantity of care. An important leverage point for BD management improvement is increasing psychiatric visit time, which would require reimbursement policy change that currently favors 15‐minute medication management visits.53 In addition, a number of innovations appear to be crucial in the field of psychiatry. First, mental health needs to be placed on the same footing as internal medicine, where objective laboratory tests inform diagnosis and treatment response tracking. Second, psychiatric residency programs should provide more extensive training in somatic medicine and neuroscience, continually updated with modern advances. Third, an interdisciplinary approach for treatment should be taught and broadly implemented via collaborative teams of experts in both psychiatry and somatic medicine to ensure comprehensiveness of the care provided. Finally, unified evidence‐based protocols for BD diagnostics and treatment should be developed, which provide personalized patterns of BD care covering a diverse range of clinical situations. In order to achieve improved access, we point to one very successful model of care, Project ECHO (Extension for Community Healthcare Outcomes),54 which deploys scarce physician expertise to underserved areas by means of expert teams advising local providers through videoconferencing. We propose that interventions made in the directions mentioned will improve the quality of mental health care and access, leading to better outcomes for patients, family members, and society.
There are several limitations to this study, including the small sample of patients and concerns regarding their lack of representativeness. While “saturation” is a core principle for assessing sample size and sample adequacy in qualitative studies, its assessment is challenging and an active area of research. Several authors have found that code saturation (no new categories identified) can be achieved with seven to 16 qualitative interviews, but that meaning saturation (deep understanding of the categories) can take 25 or more interviews.55 Because our study participants could independently generate questions, code saturation was likely achieved in each focus group of 11−12 participants. This is corroborated by our observation that each focus group generated questions from all 10 of the broad themes.
In terms of representativeness, two of the three focus groups were based in rural locations which may be more affected by physician shortages and may not have deployed the same mental health advances as urban areas. The focus groups did not include imprisoned or hospitalized patients who may have different questions about their illness and different experiences with the mental health system. The patients who participated in the focus groups represented a relatively experienced and mentally stable part of the BD population, who were willing to interact and share their experiences. Due to our minimally intrusive institutional review board protocol, detailed medical records were not accessible to confirm detailed clinical characteristics of participants. Thus, the representation of viewpoints of patients with different BD subtypes and comorbidities is unclear. Also, this study was not focused specifically on ethnic or racial minorities among patients with BD who may have different experiences with the mental health system, although some minority groups were represented. These limitations are somewhat mitigated by the fact that numerous participants were experienced patient advocates who brought the viewpoints of hundreds of BD patients with whom they had interacted nationally.
Despite the small number of participants in our study, one principle of the Theory of Constraints is that deep root causes underlying studied phenomena tend to be universal, suggesting that the core conflicts revealed in our study can be extrapolated to a larger population of patients with BD. As our next initiative, we intend to communicate with more BD patients about the conflicts revealed, and explore their insights and expectations with regard to the challenges elucidated by our models on their BD management “journey”, in contrast with the expectations that were set by providers and by mental health brochures provided for BD patients.
5. CONCLUSIONS
In our study, the highest priority for BD patients is better evidence on individualized pharmacotherapy and its alternatives, with emphasis on management of suicidal thoughts and manic states.
The challenges in BD management appear to be driven by two interacting systemic core conflicts: for the patient, seeking vs avoiding pharmacotherapy; for the provider, quantity vs quality of care.
The conflicts underlying patient decision‐making should be investigated as a target for psychoeducational interventions, with particular emphasis on mitigating the loss of BD positives.
Implementation of advanced operational excellence approaches for health system improvement should be more fully investigated in the domain of mental health care, with an emphasis on maximizing the benefits to patients with limited visit time and resources.
BD management requires a “system overhaul” that supports patients in: accessing mental health services, obtaining sufficient provider visit time, having their condition diagnosed early and accurately by means of objective tools, and receiving personalized multidisciplinary care including psychosocial support.
DISCLOSURES
Dr. Tohen was a full time employee at Lilly (1997–2008). He has received honoraria from, or consulted for, Abbott, Actavis, AstraZeneca, Bristol Myers Squibb, GlaxoSmithKline, Lilly, Johnson & Johnson, Otsuka, Merck, Sunovion, Forest, Gedeon Richter, Roche, Elan, Alkermes, Allergan, Lundbeck, Teva, Pamlab, Wyeth and Wiley Publishing. His spouse was a full‐time employee at Lilly (1998–2013). Dr. Obenchain is a Lilly stockholder who performed BD outcomes research for Lilly before his retirement. Dr. Fawcett has received speaking fees from the American Psychiatric Association and the Nevada Psychiatric Association and serves on a data review board for Amgen, and he has received remuneration as co‐principal investigator of an NIMH‐funded study. Dr. Krall is a former employee and holds stock in GlaxoSmithKline, AstraZeneca, Abbott Labs, and Lorex Pharmaceuticals. Dr. Krall is a consultant to Takeda Pharmaceuticals and is Chairman of the Board of Pierian Biosciences. Dr. Young is a former employee of GlaxoSmithKline and Lilly.
AUTHOR CONTRIBUTIONS
Study concept and design: AN, NGH, ASC, BK, MJK, ANS, EV, QLS, JLD, DJP and CGL; acquisition, analysis, or interpretation of data: AN, NGH, SJN, ASC, BK, MJK, ANS, EV, QLS, JLD, SSY, RLO, RLK, KJ, JF, MT, DJP and CGL; drafting of the manuscript: AN and CGL; critical revision of the manuscript for important intellectual content: NGH, SJN, ASC, BK, MJK, SSY, RLO, RLK, JF, MT and DJP; obtaining of funding: CGL; administrative, technical, or material support: CGL and DJP.
Supporting information
ACKNOWLEDGEMENTS
Research reported in this publication was funded through a Patient‐Centered Outcomes Research Institute (PCORI) award (CER‐1507‐3160). The views in this publication are solely the responsibility of the authors and do not necessarily represent the views of PCORI, its Board of Governors or Methodology Committee.
Nestsiarovich A, Hurwitz NG, Nelson SJ, et al. Systemic challenges in bipolar disorder management: A patient‐centered approach. Bipolar Disord. 2017;19:676–688. https://doi.org/10.1111/bdi.12547
REFERENCES
- 1. Robinson LJ, Thompson JM, Gallagher P, et al. A meta‐analysis of cognitive deficits in euthymic patients with bipolar disorder. J Affect Disord. 2006;93:105‐115. [DOI] [PubMed] [Google Scholar]
- 2. Van Rheenen TE, Rossell SL. Objective and subjective psychosocial functioning in bipolar disorder: an investigation of the relative importance of neurocognition, social cognition and emotion regulation. J Affect Disord. 2014;162:134‐141. [DOI] [PubMed] [Google Scholar]
- 3. Sylvia LG, Montana RE, Deckersbach T, et al. Poor quality of life and functioning in bipolar disorder. Int J Bipolar Disord. 2017;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lewis L, Hoofnagle L. Patient perspectives on provider competence: a view from the depression and bipolar support alliance. Adm Policy Ment Health. 2005;32:497‐503. [DOI] [PubMed] [Google Scholar]
- 5. Michalak EE, Yatham LN, Kolesar S, Lam RW. Bipolar disorder and quality of life: a patient‐centered perspective. Qual Life Res. 2006;15:25‐37. [DOI] [PubMed] [Google Scholar]
- 6. Rudan I, Gibson J, Kapiriri L, et al. Setting priorities in global child health research investments: assessment of principles and practice. Croat Med J. 2007;48:595‐604. [PMC free article] [PubMed] [Google Scholar]
- 7. Wykes T, Haro JM, Belli SR, et al. Mental health research priorities for Europe. Lancet Psychiatry. 2015;2:1036‐1042. [DOI] [PubMed] [Google Scholar]
- 8. Fleurence R, Selby JV, Odom‐Walker K, et al. How the Patient‐Centered Outcomes Research Institute is engaging patients and others in shaping its research agenda. Health Aff. 2013;32:393‐400. [DOI] [PubMed] [Google Scholar]
- 9. Crowe S, Fenton M, Hall M, Cowan K, Chalmers I. Patients’, clinicians’ and the research communities’ priorities for treatment research: there is an important mismatch. Res. Involve. Engage. 2015;1:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet. 2009;374:86‐89. [DOI] [PubMed] [Google Scholar]
- 11. Concannon TW, Fuster M, Saunders T, et al. A systematic review of stakeholder engagement in comparative effectiveness and patient‐centered outcomes research. J Gen Intern Med. 2014;29:1692‐1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Esmail L, Moore E, Rein A. Evaluating patient and stakeholder engagement in research: moving from theory to practice. J Comp Eff Res. 2015;4:133‐145. [DOI] [PubMed] [Google Scholar]
- 13. Stewart RJ, Caird J, Oliver K, Oliver S. Patients’ and clinicians’ research priorities. Health Expect. 2011;14:439‐448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abma TA, Broerse JEW. Patient participation as dialogue: setting research agendas. Health Expect. 2010;13:160‐173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Raeymaekers P, Crowe S, Cowan K, Broerse J, Hertz‐Pannier L. Mind the gap! Multi‐stakeholder dialogue for priority setting in health research [Internet]. King Baudouin Foundation; 2016. Apr. Available from: https://www.kbs-frb.be/en/Activities/Publications/2016/20160426PP. Accessed June 29, 2017.
- 16. Banfield MA, Barney LJ, Griffiths KM, Christensen HM. Australian mental health consumers’ priorities for research: qualitative findings from the SCOPE for Research project. Health Expect. 2014;17:365‐375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. James Lind Alliance . Description of final workshop to set research priorities for bipolar [Internet]. 2016. Jun. http://www.jla.nihr.ac.uk/priority-setting-partnerships/bipolar/downloads/Bipolar%20PSP%20Workshop%20report%20FINAL.pdf. Accessed June 29, 2017.
- 18. Masand PS, Tracy N. Results from an online survey of patient and caregiver perspectives on unmet needs in the treatment of bipolar disorder. Prim Care Companion CNS Disord. 2014;16: doi: 10.4088/PCC.14m01655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hodges S, Ferreira K, Israel N. “If we're going to change things, it has to be systemic:” systems change in children's mental health. Am J Community Psychol. 2012;49:526‐537. [DOI] [PubMed] [Google Scholar]
- 20. Saxe GN, Statnikov A, Fenyo D, et al. A complex systems approach to causal discovery in psychiatry. PLoS ONE. 2016;11:e0151174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maier D. Applying systems medicine in the clinic. Curr Opin Syst Biol. 2017;3:77‐87. [Google Scholar]
- 22. Quint JB. Health Research Data for the Real World: the Marketscan Databases. Ann Arbor, MI: Truven Health Analytics; 2015. [Google Scholar]
- 23. Curedale R. Affinity Diagrams: the Tool to Tame Complexity. Topanga, CA: Design Community College Inc.; 2016:128. [Google Scholar]
- 24. Scheinkopf LJ. Thinking for a Change: Putting the TOC Thinking Processes to Use. Boca Raton, FL: St. Lucie Press; 1999. 268 p. [Google Scholar]
- 25. William Dettmer H. The Logical Thinking Process: A Systems Approach to Complex Problem Solving. Milwaukee, WI: ASQ Quality Press; 2007. 413 p. [Google Scholar]
- 26. Cox JF III, Schleier JG. Theory of Constraints Handbook. New York, NY: McGraw‐Hill; 2010. [Google Scholar]
- 27. Cakir S, Yazıcı O, Post RM. Decreased responsiveness following lithium discontinuation in bipolar disorder: a naturalistic observation study. Psychiatry Res. 2017;247:305‐309. [DOI] [PubMed] [Google Scholar]
- 28. Andreescu C, Mulsant BH, Emanuel JE. Complementary and alternative medicine in the treatment of bipolar disorder–a review of the evidence. J Affect Disord. 2008;110:16‐26. [DOI] [PubMed] [Google Scholar]
- 29. Nelson B. Quality over quantity. Hospitalist [Internet]. 2009. [cited 2017 May 19];12. http://www.the-hospitalist.org/hospitalist/article/123798/quality-over-quantity. Accessed June 29, 2017.
- 30. Fountoulakis KN, Vieta E, Young A, et al. The International College of Neuropsychopharmacology (CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP‐BD‐2017), part 4: unmet needs in the treatment of bipolar disorder and recommendations for future research. Int J Neuropsychopharmacol. 2016;20:196‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Landi P, Marazziti D, Rutigliano G, Dell'Osso L. Insight in psychiatry and neurology: state of the art, and hypotheses. Harv Rev Psychiatry. 2016;24:214‐228. [DOI] [PubMed] [Google Scholar]
- 32. Basco MR, Smith J. Faulty decision‐making: impact on treatment adherence in bipolar disorder. Prim psychiatry. 2009;16:53‐58. [Google Scholar]
- 33. Gibson S, Brand SL, Burt S, Boden ZVR, Benson O. Understanding treatment non‐adherence in schizophrenia and bipolar disorder: a survey of what service users do and why. BMC Psychiatry. 2013;29:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. de Jesus JR, de Campos BK, Galazzi RM, Martinez JLC, Arruda MAZ. Bipolar disorder: recent advances and future trends in bioanalytical developments for biomarker discovery. Anal Bioanal Chem. 2015;407:661‐667. [DOI] [PubMed] [Google Scholar]
- 35. Marangell LB, Suppes T, Zboyan HA, et al. A 1‐year pilot study of vagus nerve stimulation in treatment‐resistant rapid‐cycling bipolar disorder. J Clin Psychiatry. 2008;69:183‐189. [DOI] [PubMed] [Google Scholar]
- 36. Benedetti F, Riccaboni R, Locatelli C, Poletti S, Dallaspezia S, Colombo C. Rapid treatment response of suicidal symptoms to lithium, sleep deprivation, and light therapy (chronotherapeutics) in drug‐resistant bipolar depression. J Clin Psychiatry. 2014;75:133‐140. [DOI] [PubMed] [Google Scholar]
- 37. Crowe M, Beaglehole B, Inder M. Social rhythm interventions for bipolar disorder: a systematic review and rationale for practice. J Psychiatr Ment Health Nurs. 2016;23:3‐11. [DOI] [PubMed] [Google Scholar]
- 38. Saunders EFH, Ramsden CE, Sherazy MS, Gelenberg AJ, Davis JM, Rapoport SI. Omega‐3 and omega‐6 polyunsaturated fatty acids in bipolar disorder: a review of biomarker and treatment studies. J Clin Psychiatry. 2016;77:e1301‐e1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Swartz HA, Swanson J. Psychotherapy for bipolar disorder in adults: a review of the evidence. Focus. 2014;12:251‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Oud M, Mayo‐Wilson E, Braidwood R, et al. Psychological interventions for adults with bipolar disorder: systematic review and meta‐analysis. Br J Psychiatry. 2016;208:213‐222. [DOI] [PubMed] [Google Scholar]
- 41. Bond K, Anderson IM. Psychoeducation for relapse prevention in bipolar disorder: a systematic review of efficacy in randomized controlled trials. Bipolar Disord. 2015;17:349‐362. [DOI] [PubMed] [Google Scholar]
- 42. Salloum NC, McCarthy MJ, Leckband SG, Kelsoe JR. Towards the clinical implementation of pharmacogenetics in bipolar disorder. BMC Med. 2014;30:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Eiring Ø, Nytrøen K, Kienlin S, Khodambashi S, Nylenna M. The development and feasibility of a personal health‐optimization system for people with bipolar disorder. BMC Med Inform Decis Mak. 2017;17:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kupfer DJ, Frank E, Ritchey FC. Staging bipolar disorder: what data and what models are needed? Lancet Psychiatry. 2015;2:564‐570. [DOI] [PubMed] [Google Scholar]
- 45. Fernandes BS, Berk M. Staging in bipolar disorder: one step closer to precision psychiatry. Rev Bras Psiquiatr. 2017;39:88‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Castellani A, Girlanda F, Barbui C. Rigour of development of clinical practice guidelines for the pharmacological treatment of bipolar disorder: systematic review. J Affect Disord. 2015;15:45‐50. [DOI] [PubMed] [Google Scholar]
- 47. Fountoulakis KN, Yatham L, Grunze H, et al. The International College of Neuro‐Psychopharmacology (CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP‐BD‐2017), part 2: review, grading of the evidence, and a precise algorithm. Int J Neuropsychopharmacol. 2017;20:121‐179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Parker GB, Graham RK, Tavella G. Is there consensus across international evidence‐based guidelines for the management of bipolar disorder? Acta Psychiatr Scand. 2017;135:515‐526. [DOI] [PubMed] [Google Scholar]
- 49. Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder: part II. Impact on clinical outcome, function, and costs. Psychiatr Serv. 2006;57:937‐945. [DOI] [PubMed] [Google Scholar]
- 50. Simon GE, Ludman EJ, Bauer MS, Unützer J, Operskalski B. Long‐term effectiveness and cost of a systematic care program for bipolar disorder. Arch Gen Psychiatry. 2006;63:500‐508. [DOI] [PubMed] [Google Scholar]
- 51. Ronen B, Pliskin JS, Pass S. Focused Operations Management for Health Services Organizations. San Francisco, CA: John Wiley & Sons; 2006. [Google Scholar]
- 52. Kenney C, Berwick DM. Transforming Health Care: Virginia Mason Medical Center's Pursuit of the Perfect Patient Experience, 1st edn New York, NY: CRC Press; 2011:223. [Google Scholar]
- 53. Torrey WC, Griesemer I, Carpenter‐Song EA. Beyond “Med Management”. Psychiatr Serv. 2017;68:618‐620. [DOI] [PubMed] [Google Scholar]
- 54. Zhou C, Crawford A, Serhal E, Kurdyak P, Sockalingam S. The impact of project ECHO on participant and patient outcomes: a systematic review. Acad Med. 2016;91:1439‐1461. [DOI] [PubMed] [Google Scholar]
- 55. Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. 2017;27:591‐608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


