Abstract
Comorbidity of internalizing and externalizing problems and its risk and protective factors have not been well incorporated into developmental research, especially among racial minority youth from high-poverty neighborhoods. The present study identified a latent comorbid factor as well as specific factors underlying internalizing and externalizing problems among 592 African American adolescents living in economically disadvantaged neighborhoods (291 male; M age = 15.9 years, SD = 1.43 years). Stressful life events and racial discrimination were associated with higher comorbid problems, whereas stressful life events and exposure to violence were associated with higher specific externalizing problems. Collective efficacy was associated with both lower specific externalizing problems and lower comorbid problems. Moreover, high collective efficacy buffered the risk effects of stressful life events and racial discrimination on comorbid problems. Our results demonstrated the advantages of latent variable modeling to understanding comorbidity by articulating impacts of risk factors on comorbid and specific components underlying internalizing and externalizing problems. They also highlighted the protective effect of collective efficacy in mitigating risks for these problems. These findings broadly call for more studies on comorbidities in developmental psychopathology among youth from diverse sociocultural backgrounds.
High comorbidity rates of internalizing and externalizing problems have been extensively documented among youth and adults (Angold, Costello, & Erkanli, 1999; Cerdá, Sagdeo, & Galea, 2008). Epidemiological evidence supports the notion that comorbidity, a condition where two unrelated types of problems co-occur with a rate that far exceeds chance (Caron & Rutter, 1991), is not a mere artifact of sampling or clinical referral bias (e.g., Angold et al., 1999; Cerda´ et al., 2008; Kessler et al., 1994, 2005). The prevalence of comorbidity across internalizing and externalizing problems highlights the need to reconceptualize psychopathology and its development (Eaton, Rodriguez-Seijas, Carragher, & Krueger, 2015; Eaton, South, & Krueger, 2010; Krueger & Markon, 2006). Traditional nosology has been challenged on the grounds that seemingly discrete symptoms may represent at least in part a common underlying pathology for internalizing and externalizing problems (Caron & Rutter, 1991). Moreover, risk and protective factors need to be investigated in light of comorbidity, because examining one type of problem in the absence of the other is likely to produce biased or incomplete results (Caron & Rutter, 1991; Liu, Bolland, Dick, Mustanski, & Kertes, 2016). Comorbidity may also indicate shared etiological factors, as well as direct reciprocal influences, between the two types of problems (e.g., Beyers & Loeber, 2003; Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011; Timmermans, van Lier, & Koot, 2010). However, the current research field lacks a strong methodology to represent comorbidity, let alone investigate its risk and protective factors.
Comorbidity is often assessed using DSM diagnoses (e.g., Ha, Balderas, Zanarini, Oldham, &Sharp, 2014; Kessler et al., 2014). Such a categorical approach to represent psychopathology has long been criticized, and a dimensional approach has been advocated (Boyle et al., 1996; Plomin, Haworth, & Davis, 2009; Widiger & Samuel, 2005). A dimensional approach is especially relevant for problems emerging during adolescence, as biological, psychological, and social changes during this developmental period blur the boundary between normal and abnormal behaviors (Cicchetti & Rogosch, 2002). One analytic approach to the “problem” of comorbidity in developmental research has been to control for comorbid problems in regression analyses (e.g., Sentse, Ormel, Veenstra, Verhulst, & Oldehinkel, 2011). This approach is useful for identifying unique risk and protective factors for a specific type of problem. However, it is less useful for identifying common risk and protective factors that predict comorbidity.
Efforts have been made recently to address this issue by identifying latent components underlying internalizing and externalizing problems using a structural equation modeling framework. Several latent models for comorbidity have been tested, reflecting different ways of conceptualizing psychopathology. The internalizing–externalizing two-factor model represents discrete symptoms, such as withdrawn/depressed and somatic symptoms, by an internalizing factor, and aggression and rule-breaking behavior by an externalizing factor. Thus in this model, internalizing and externalizing are cohesive but distinct latent factors (e.g., Rodriguez-Seijas, Stohl, Hasin, & Eaton, 2015). Although this model has been used with various populations (Eaton et al., 2010), it does not address the covariation across internalizing and externalizing factors. In these models there is often a positive correlation observed between the internalizing and externalizing factors (Eaton et al., 2010). In contrast, other statistical models capture the heterogeneity of internalizing and externalizing problems by distinguishing a general factor underlying both internalizing and externalizing problems from specific factors unique to each type of problem. These models, although varying in what the general factor is labeled, all use the same statistical modeling technique (a bifactor model; Gibbons & Hedeker, 1992) and all tap into the same underlying issue: that there is a latent factor underlying the commonly observed comorbidity of internalizing and externalizing problems (Caspi et al., 2014; Keiley, Lofthouse, Bates, Dodge, & Pettit, 2003; Laceulle, Vollebergh, & Ormel, 2015; Lahey et al., 2011, 2012; Olino, Dougherty, Bufferd, Carlson, & Klein, 2014). When comorbidity is explicitly modeled, the positive correlation disappears, and sometimes residual internalizing and externalizing factors show a negative correlation (Caspi et al., 2014; Laceulle et al., 2015). Of note, this latent structure is found among adults using DSM diagnoses (Caspi et al., 2014; Lahey et al., 2012) as well as among children and adolescents using self- or parent-reported questionnaires, such as the Youth Self-Report (YSR; Achenbach, 1991) and the Child Behavior Checklist (Laceulle et al., 2015; Lahey et al., 2011; Olino et al., 2014).
One substantial gap in this emerging literature is the lack of attention paid to minority and high-risk populations. Although early reports using latent variable modeling used nationally representative samples, it is unknown whether the latent structure of internalizing and externalizing problems is the same among groups that are typically underrepresented in such samples. Epidemiological studies often report lower rates of common psychiatric disorders among African Americans compared to White Americans (e.g., Eaton et al., 2013). However, some evidence suggests that African American adults and youth express mental health problems with a symptom profile that is not well captured by common criteria used in national surveys. For example, African Americans show lower rates of DSM-diagnosed major depression than White Americans; however, non-DSM instruments capture lower levels of well-being and higher depressive symptoms and distress among African Americans (Eaton et al., 2013). African American youth also report increased externalizing problems, such as anger and aggression, along with depression compared to youth from other racial groups (Anderson & Mayes, 2010). These findings argue for a potentially unique latent structure of internalizing and externalizing problems among African American youth.
In addition, compared to other racial groups, African American youth disproportionally represent residents living in high-poverty neighborhoods (e.g., Brody et al., 2001; Zenk et al., 2005). Cultural ecological theories have proposed that such conditions inhibit the development of competencies in minority children (Garcı´a Coll et al., 1996) and present multiple risk factors for developmental psychopathology (Grant et al., 2006; Ingram & Price, 2010). Thus, the current study aimed to extend newly emerging latent variable models of specific and comorbid internalizing and externalizing problems to a difficult to reach population; namely, African American youth residing in high-poverty neighborhoods.
In addition to elucidating the structure of psychopathology among an underrepresented population in developmental research, a second aim of the study was to examine several salient risk and protective factors within the latent variable modeling framework. The latent variable modeling approach provides a powerful framework to investigate risk and protective factors for comorbid and specific mental health problems (Krueger & Markon, 2006). Previous studies using latent variable modeling have identified more risk factors that contribute to a comorbid-type factor compared to specific internalizing and externalizing factors (Keiley et al., 2003; Lahey et al., 2012). Specific to this sample, we aimed to examine risk factors that are salient for high-poverty neighborhoods not well captured by prior surveys. Residents in high-poverty neighborhoods experience more stressful life events and higher exposure to violence (Carlson, 2006; Evans & English, 2002). Racial minority youth experience additional adverse events, including racial discrimination (Garcı´a Coll et al., 1996). Although there is evidence to suggest that these stressor types increase risk for internalizing and externalizing problems when examined separately, the bulk of this research has been conducted among White and mixed-race samples of youth; moreover, the issue of comorbidity has rarely been taken into consideration.
In studies that examined internalizing and externalizing problems separately, stressful life events, such as major physical injury, loss of a family member, and transition of a primary caregiver, have been linked with both types of problems among predominantly White youth (e.g., Kim, Conger, Elder, & Lorenz, 2003). Among African American adolescents, stressful life events are associated with internalizing problems (e.g., Gaylord-Harden, Elmore, Campbell, & Wethington, 2011; Sanchez, Lambert, & Cooley-Strickland, 2013), whereas its relation with externalizing problems is far less studied (Lansford et al., 2006).
Similar to stressful life events, research with White and mixed-race samples of youth has established the negative impact of exposure to violence on internalizing and externalizing problems, respectively (for a meta-analysis, see Fowler, Tompsett, Braciszewski, Jacques-Tiura, & Baltes, 2009). However, evidence has been less consistent among African American youth (Mrug & Windle, 2010). Exposure to violence has been associated with externalizing problems among African American adolescents in some studies (e.g., Lambert, Boyd, Cammack, & Ialongo, 2012; Sanchez et al., 2013) but not others (e.g., Cooley-Quille, Boyd, Frantz,&Walsh, 2001; Grant et al., 2005; Sterrett et al., 2014).
Racial discrimination has been associated with a wide range of mental health problems for African Americans (Clark, Anderson, Clark, & Williams, 1999), including but not limited to depression and anxiety (e.g., Banks, Kohn- Wood, & Spencer, 2006; English, Lambert, Evans, & Zonderman, 2014), conduct problems (e.g., Brody et al., 2006, 2011), and other general psychological distress (Brown & Tylka, 2011; Bynum, Burton, & Best, 2007). However, far more studies on racial discrimination have been conducted among African American adults rather than adolescents (e.g., see Williams & Mohammed, 2009). Yet compared to adults, minority adolescents might be especially vulnerable to the negative mental health outcomes of racial discrimination, because adolescents are particularly sensitive to social stressors (e.g., Stroud et al., 2009) but possess less matured ethnic identity and stress regulation capacity (e.g., Gibbons et al., 2007). In addition, prior studies that did focus on African American adolescents tended to examine a few discrete mental health disorders, in particular depression (e.g., Lambert, Robinson,&Ialongo, 2014). The impact of racial discrimination on a wide spectrum of internalizing and externalizing problems has been less examined.
Previous studies have rarely addressed the issue of comorbidity when examining the impact of stressors on internalizing and externalizing problems. Most studies analyzed internalizing and externalizing problems in separate regressions (e.g., Kim et al., 2003; Sanchez et al., 2013), which could not differentiate the effects of stressors on one specific type of problems from the effects on their comorbidity. Some studies analyzed one type of problem while controlling for the other type. For example, stressful life events showed an impact on both internalizing and externalizing problems when their comorbidity was controlled for (King & Chassin, 2008). However, this approach is unable to elucidate the impact of stressful life events on comorbid internalizing and externalizing problems. Two studies have examined relations among stressors and mental health problems via mediation analysis using linear regressions. These studies reported that the effects of stressful life events and racial discrimination on internalizing problems were mediated by comorbid externalizing problems among African American adolescents (Liu et al., 2015) and that the effects of racial discrimination on internalizing and externalizing problems were both mediated by trait anger among African American boys (Nyborg & Curry, 2003). Both of these studies indicated heterogeneity within one type of problem and covariation between internalizing and externalizing problems; however, these mediation analyses were still unable to pinpoint the impact of stressors on the specific and comorbid components underlying internalizing and externalizing problems. In the present study, we sought to further clarify the relations among stressors with internalizing and externalizing problems using a latent variable modeling approach that could statistically tease apart unique and shared variances among internalizing and externalizing problems.
Moreover, few studies have examined protective factors for comorbid internalizing and externalizing problems, even though both protective and risk factors are essential to understanding the risk and resilience processes in developmental psychopathology (Cicchetti & Rogosch, 2002). Despite the heightened risks related to living in impoverished communities and being a racial minority, most African American adolescents living in disadvantaged neighborhoods do not develop mental health problems. Social support from parents, peers, and community has been documented as one of the important protective processes against adverse developmental outcomes (Cohen & Wills, 1985; Garcı´a Coll et al., 1996; Grant et al., 2006; Lee & Goldstein, 2016). However, social support has typically been examined on an individual or family level rather than on a neighborhood level (e.g., Browning, Gardner, Maimon, & Brooks-Gunn, 2014). The ecological systems theory of human development (Bronfenbrenner, 1986) suggests that individual development is influenced by risk and protective processes on multiple levels, ranging from individual and family, to community and broader contexts. Neighborhood factors are especially relevant to adolescents as they start to engage in more activities outside their own households in the community (Aber, Gephart, Brooks-Gunn, & Connell, 1997; Bhargava & Witherspoon, 2015). The cultural ecological theory (Garcı´a Coll et al., 1996) especially emphasizes neighborhood environments for racial and ethnic minority youth, as a neighborhood can be either inhibiting or promoting the development ofminority youth depending on its characteristics. African Americans, in particular, tend to establish extended interpersonal connectedness and social support networks (Boyd-Franklin, 1989; Choi, 2002; Taylor, Chatters, Woodward, & Brown, 2013); as such, collectively protective processes around neighborhoods may be especially relevant for youth in neighborhoods that are predominantly African American communities. Previous research suggests that a neighborhood with good connections, spontaneous engagement in the community, high levels of mutual trust, and shared values among residents tends to be associated with fewer risks and is believed to promote positive development. These features of a neighborhood are characterized as collective efficacy (Sampson, Raudenbush, & Earls, 1997).
Neighborhoods with high collective efficacy have been found to have lower violence and crime rates (Ahern et al., 2013; Mazerolle, Wickes, & McBroom, 2010; Sampson et al., 1997). Collective efficacy may also buffer the risk effect of neighborhood violence on mental health problems, such as substance use (Fagan, Wright, & Pinchevsky, 2014) and internalizing and externalizing problems (Browning et al., 2014). Beyond violence exposure, evidence for any protective effect of collective efficacy on other outcomes has rarely been studied in youth of any race. To our knowledge there is only one study documenting that collective efficacy buffered the risk of perceived discrimination on depressive symptoms; however, it was conducted with adults of Asian descent residing in Hong Kong (Chou, 2012). There have been no studies testing whether collective efficacy predicts internalizing or externalizing problems among African American youth or whether it may buffer risks associated with racial discrimination or stressful events among residents of high-poverty neighborhoods.
The Present Study
The present study aimed to address several gaps in the literature on understanding comorbidity of internalizing and externalizing problems among an underrepresented population of youth. The first goal of the study was to establish the latent structure of internalizing and externalizing problems among a sample of high-risk youth: African American adolescents residing in high-poverty neighborhoods. We analyzed and compared the internalizing–externalizing two-factor model and comorbid models using a bifactor solution that identify a specific internalizing, specific externalizing, and a comorbid problems factor (see Statistic Analysis Plan section and Figure 1). Based on previous results in other populations, we expected the comorbid models to have substantially better model fit than the internalizing–externalizing two-factor model. In addition, because prior studies found negative correlations between the specific internalizing and externalizing factors (Caspi et al., 2014; Laceulle et al., 2015), we aimed to test whether a similar negative correlation can be found among the present sample.
Figure 1.
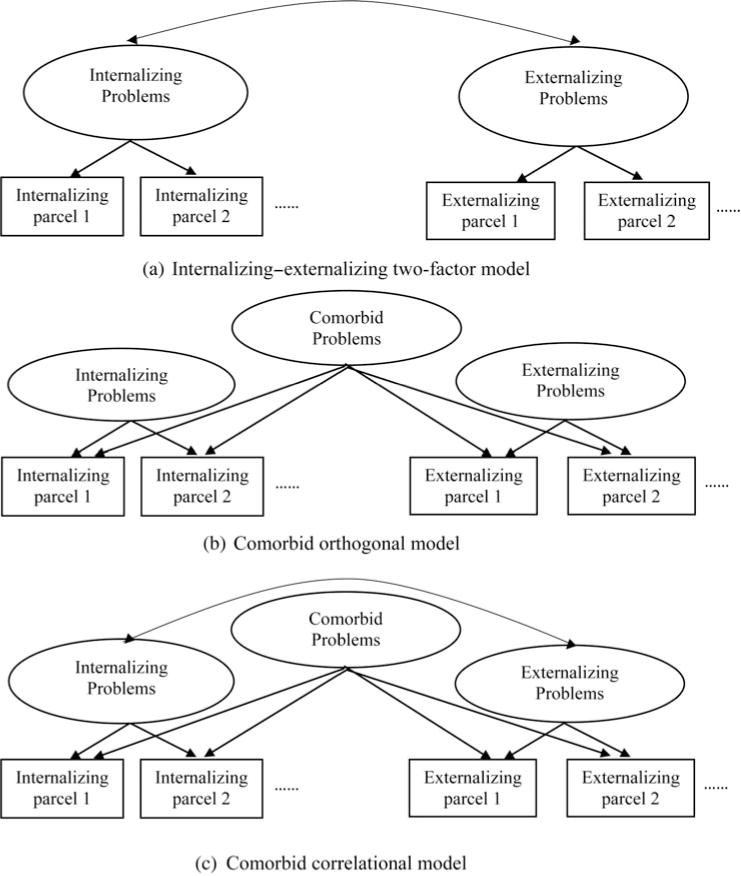
Alternative confirmatory factor analysis models for the latent structure of internalizing and externalizing problems. Youth Self-Report items were grouped into parcels; see Statistical Analysis Plan section for full description.
The second goal was to examine the impact of multiple types of stressors on the latent factors underlying internalizing and externalizing problems. These analyses aim to clarify inconsistent findings between stressors and internalizing/externalizing problems among African American youth in prior studies. Because the three stressors (racial discrimination, stressful life events, and exposure to violence) have been associated with both internalizing and externalizing problems, we hypothesized that all stressors would show significant effects on the comorbid problems factor. Whether these three stressor types would predict the specific internalizing and externalizing factors was less clear a priori, as few studies have utilized the latent model of psychopathology to examine the impact of risk or protective factors. One exception is a study that found an impact of general life stress on a specific externalizing factor across ages 5 to 14 years (Keiley et al., 2003). However, because the study was conducted among predominantly White, middle-class preadolescents and based on maternal report, its results may not necessarily generalize to the present sample.
Finally, we focused on an uncommonly studied but potentially important protective factor: collective efficacy, to advance the understanding of neighborhood impacts on minority adolescents’ mental health. Based on the extensive research of Sampson et al.’s (1997) research in Chicago neighborhoods, we hypothesize that high collective efficacy would mitigate the negative impact of neighborhood violence and other stressors on internalizing and externalizing problems.
Method
Participants
Five hundred and ninety-two African American adolescents (291 male; M age = 15.9 years, SD = 1.43 years, range = 13–19 years) from 439 households were recruited from targeted neighborhoods in the Mobile Metropolitan Statistical Area in Alabama. Because of the hard to reach nature of the sample, any adolescents living in the household within the target age range who agreed to participate were enrolled. All statistical analyses corrected for nonindependent observations within household (see Statistical Analysis Plan section). According to US Census data (2012), 31.5% of African American residents in the Mobile Metropolitan Statistical Area had incomes below the poverty level. Among the present sample, 81.9% lived in a household with less than $20,000 annual income.
Procedure
The present study is part of the Gene, Environment, Neighborhood Initiative. The broad goals of this initiative are to investigate predictors of health outcomes among racialminority adolescents living in high-poverty environments. Families with adolescents between the ages of 13 and 19 years in neighborhoods targeted based on US census data of low household income were reached via flyers and home visits. Interested parents and adolescents were scheduled for an approximately 2-hr survey in a local community center. Some of the families were part of a federal program to relocate from public housing, but analyses of the program found no effects of relocation on internalizing or externalizing outcomes (Byck et al., 2015), so this effect was not incorporated into analyses presented here. Adolescents and their caregivers provided written assent and consent, respectively. Adolescents provided responses to surveys via a combination of audiocomputer assisted self-interview and interviewer-administered questionnaires (along with biomarker data not reported here). Financial compensation was provided after the study.
Measures
Internalizing and externalizing problems
The YSR (Achenbach, 1991) was used to measure internalizing and externalizing problems. The YSR surveys 112 behavioral and emotional problems in children and adolescents from ages 11 to 18 years. Each item was scored on a 0 (not true) to 2 (very true) scale. Raw scores were used for statistical analyses. We also generated T scores based on established national norm for descriptive purposes only. A T score above 60 indicates an at-risk level of internalizing or externalizing problems (Achenbach, 1991). Internalizing problems were composed of three subscales: anxious/depressed, withdrawn/depressed, and somatic complaints. Externalizing problems were composed of two subscales: aggressive behavior and rule-breaking behavior. Each subscale contained 10 to 15 items. Cronbach a in this sample was 0.86 for internalizing problems and 0.90 for externalizing problems.
Stressful life events
The Stress Index (Attar, Guerra,&Tolan, 1994) was used to measure stressful life events. It contains 16 questions about frequencies of life events during the past 12 months, such as “A close relative or friend died” or “Your family’s property got wrecked or damaged due to fire, burglary, flood, or other disaster.” Frequencies of stressful events were scored on a 0 (none) to 3 (three times or more) scale. Scores on all items were summed to create one summary composite score. The Cronbach α value in this sample was 0.75.
Racial discrimination
The Schedule of Racist Events (Landrine & Klonoff, 1996) was used to assess experiences of racial discrimination within the past 12 months. The original measure developed for use with adults is composed of 18 items, such as “How often have you been accused or suspected of doing something wrong because you are Black?” rated on a 6-point Likert scale (never to almost all of the time). Wording and items were adapted for use with adolescents, resulting in a total of 14 questions of racist events on a 3-point scale (never, sometimes, or a lot). Scores were summed and rescaled to 0–28. The Cronbach a value in this sample was 0.90.
Exposure to violence
A questionnaire version of the Exposure to Violence Interview (Gorman-Smith & Tolan, 1998) was used to assess exposure to violence. Nine specific questions related to victimization and witnessing violence within the last 12 months were asked. Examples of the questions are “Have you seen anyone get shot or stabbed/cut in your neighborhood?” and “Have you been robbed or mugged in your neighborhood?” Answers were coded as 0 (no) or 1 (yes), and scores were summed across all questions. The Cronbach α value in this sample was 0.80.
Collective efficacy
The Collective Efficacy Scale (Sampson et al., 1997) was used. The scale, originally created for use with adults, contains 10 items, such as “How likely is it that your neighbors would get involved or intervene if children were skipping school and hanging out on a street corner?” One item related to city budgets was not included in the adolescent version. The remaining 9 items were scored on a 1 (very unlikely) to 5 (very likely) scale. Scores were averaged to generate a collective efficacy score, with higher scores indicating higher collective efficacy. The Cronbach a value in this sample was 0.77.
Statistical analysis plan
To address the first aim, a latent structure of internalizing and externalizing problems was developed by comparing alternative confirmatory factor analysis (CFA) models previously examined in other demographic groups (Caspi et al., 2014; Keiley et al., 2003; Laceulle et al., 2015). Model A, the internalizing– externalizing two-factor model (Figure 1a), established the internalizing and externalizing factors underlying internalizing and externalizing problems, respectively. The correlation between internalizing and externalizing factors was estimated. We estimated two additional models using a bifactor solution (Gibbons & Hedeker, 1992). Model B, the comorbid orthogonal model (Figure 1b), estimated an additional factor, representing comorbid internalizing and externalizing problems. No correlations between the specific internalizing and externalizing factors or the comorbid factor were allowed. Model C, the comorbid correlated model (Figure 1c), resembled Model B, except the correlation between the specific internalizing and externalizing factors was estimated. These CFA models were estimated based on parcels of the YSR items, as recommended for questionnaires with numerous individual items (Little, Cunningham, Shahar, & Widaman, 2002). Following Little et al.’s (2002) guideline, questionnaire items within each subscale (e.g., anxious/depressed and rule-breaking behavior; see Figure 2) were randomly divided into 2 or 3 parcels, resulting in 12 parcels, each with 5 or 6 items. Participants fromthe same households were clustered to account for nonindependent observations (Byck, Bolland, Dick, Ashbeck, & Mustanski, 2013). Maximum likelihood estimation with robust standard errors and a scaled test statistic (Satorra & Bentler, 1994) was used to account for positively skewed YSR scores and clustered sample. Goodness of fit indices of alternative models were compared based on χ2 to degrees of freedom (df) ratio, comparative fit index (CFI), root mean square errorof approximation (RMSEA), standardized root mean square residual (SRMR), Akaike information criterion, and Bayesian information criterion. A χ2 to df ratio of less than 2, CFI values greater than 0.95, RMSEA scores less than 0.05, and SRMR scores less than 0.06 are considered good fit (Hu & Bentler, 1999). Across alternative models, lower Akaike information criterion and Bayesian information criterion indicate better model fit with parsimonious model parameters.
Figure 2.
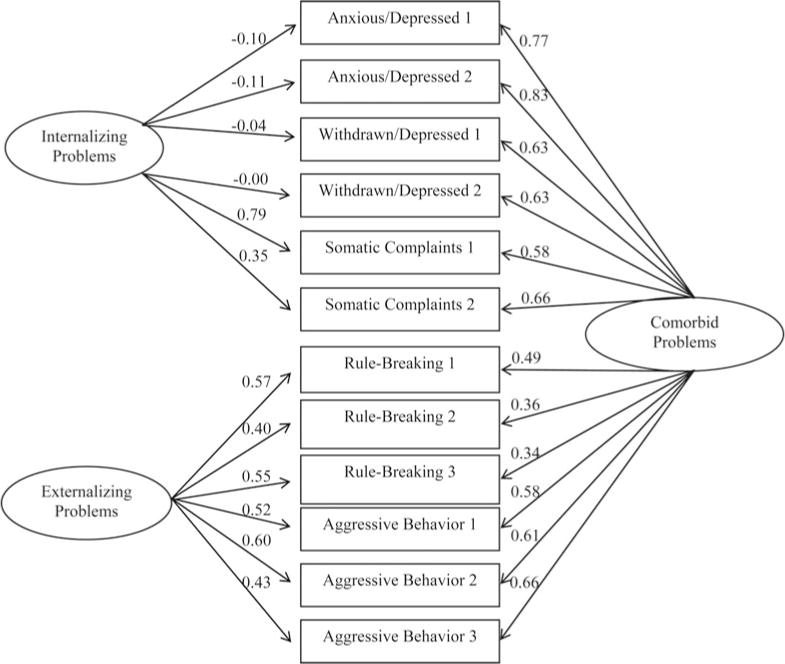
Confirmatory factor analysis of the Youth Self-Report parcels. χ2 = 101.73, df = 42, root mean square error of approximation = 0.05, standardized root mean square residual = 0.03, comparative fit index = 0.98. Standardized factor loadings are shown.
The next set of analyses addressed the second aim of the study to examine risk and protective factors for comorbid and specific internalizing/externalizing problems. The best fitting latent model from the previous step was used to construct a structural equation model (SEM) in which risk and protective factors were included in the model as predictors. Regression paths of stressful life events, racial discrimination, exposure to violence, and collective efficacy on latent factors underlying internalizing and externalizing problems were estimated, controlling for age and gender. To test whether collective efficacy buffers the risk effects of the three stressors, interaction terms between collective efficacy and the three stressor types were computed and entered to the SEM as predictors for the latent factors.
Results
SPSS 22.0 was used to generate descriptive statistics. Mplus version 7.3 (Muthén & Muthén, 2012) was used for confirmatory factor analyses and structural equation modeling. Missing data were at low rates (YSR 2.1%, Stress Index 5.1%, racial discrimination 5.1%, exposure to violence 5.1%, collective efficacy 5.1%) and were treated as missing at random.
Table 1 lists the means, standard deviations, and bivariate correlations of the variables tested. Internalizing and externalizing problems were highly correlated with each other (r = .64, p < .01). All risk and protective factors were significantly correlated with internalizing and externalizing problems (r = −.19 to .38, p < .01). The three stressor types were significantly correlated with each other (r = .26 to .45, p < .01), but not correlated with collective efficacy (r = −.06 to .00, ns).
Table 1.
Means, standard deviations, and correlations among variables tested
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Internalizing problems T score | 48.3 | 10.11 | 1 | |||||
| 2. Externalizing problems T score | 51.6 | 11.43 | .64*** | 1 | ||||
| 3. Stressful life events | 5.7 | 5.21 | .36*** | .38*** | 1 | |||
| 4. Racial discrimination | 2.2 | 3.94 | .23*** | .22*** | .28*** | 1 | ||
| 5. Exposure to violence | 1.7 | 1.89 | .22*** | .29*** | .45*** | .26*** | 1 | |
| 6. Collective efficacy | 3.2 | 0.80 | –.12** | −.19*** | –.04 | −.06 | .00 | 1 |
p < .01.
p < .001.
The three alternative CFA models (see Figure 1) were tested and compared by model fit indices. The internalizing–externalizing two-factor model (Model A) showed substantially worse model fit compared to the two comorbid models that use a bi-factor solution (Models B and C, see Table 2). The latter two models showed similar model fit indices, with the comorbid orthogonal model (Model B) showing slightly better model fit than the comorbid correlated model (Model C). Moreover, correlation between the specific internalizing and externalizing factors in Model C was not significant (r = .00, ns). Therefore, the comorbid orthogonal model (Model B, Figure 1b) was chosen as the best fitting model for the latent structure of internalizing and externalizing problems. Subsequent SEM was based on the comorbid orthogonal model.
Table 2.
Model fit comparisons for alternative latent comorbidity models
| χ2 | df | CFI | AIC | BIC | RMSEA | SRMR | |
|---|---|---|---|---|---|---|---|
| 1. Internalizing–externalizing two factor | 241.50 | 53 | 0.92 | 1383.68 | 1545.05 | 0.08 | 0.05 |
| 2. Comorbid orthogonal | 101.73 | 42 | 0.98 | 1210.91 | 1420.25 | 0.05 | 0.03 |
| 3. Comorbid correlated | 103.58 | 41 | 0.97 | 1212.90 | 1426.60 | 0.05 | 0.03 |
Note: CFI, Comparative fit index; AIC, Akaike information criterion; BIC, Bayesian information criterion; RMSEA, root mean square error of approximation; SRMR, standardized root mean square residual.
Figure 2 shows the latent structure and factor loadings of internalizing and externalizing problems in the comorbid orthogonal model. Parcels from internalizing subscales loaded onto a specific internalizing factor, and parcels from externalizing subscales loaded onto a specific externalizing factor. In addition, both internalizing and externalizing parcels loaded onto a comorbid factor. Parcels from two of the internalizing subscales, anxious/depressed and withdrawn/depressed, had very low, nonsignificant factor loadings on the specific internalizing factor; only somatic complaints loaded above 0.35 on the specific internalizing factor. Therefore, the specific internalizing factor should be interpreted as reflecting the component of internalizing problems manifest as somatic symptoms. In contrast, all the internalizing parcels had consistently high loadings (0.58–0.83) on the comorbid factor. Externalizing parcels had moderate to high (0.34–0.66) loadings on both the specific externalizing factor and the comorbid factor.
The structural equation model estimated the effects of risk and protective factors on the latent factors, controlling for age and gender (Figure 3). The comorbid factor was significantly associated with higher stressful life events and racial discrimination (βs = 0.20 and 0.19, p < 01), and was inversely related to neighborhood collective efficacy (β = −0.09, p < 05). The specific externalizing factor was significantly associated with higher stressful life events and exposure to violence (βs = 0.23 and 0.16, p < 05) and was also inversely related to neighborhood collective efficacy (β = −0.16, p <.05). The specific internalizing (somatic) factor was not associated with any of the risk or protective factors assessed in this study.
Figure 3.
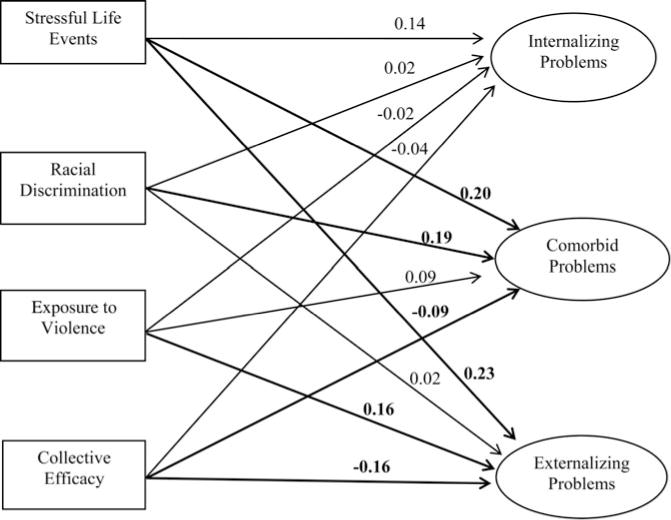
Effects of stressors and collective efficacy on latent factors of psychopathology. Regression coefficients were standardized. Regression paths and coefficients in bold were significant at p < .05. χ2 = 256.13, df = 96, root mean square error of approximation = 0.06, standardized root mean square residual = 0.03, comparative fit index = 0.94.
Next, the interactions between collective efficacy and the three stressor types on the latent factors were tested (as per the analysis model shown in Figure 4). The effects of stressful life events and racial discrimination on the comorbid factor were significantly moderated by collective efficacy (βs = −0.11 and−0.12, p < .05). To interpret these two interactions, we followed Aiken and West’s (1991) guideline on plotting interactions between continuous variables. Estimated comorbid problem scores were calculated based on the regression coefficients obtained from the final structural equation model. Figure 5 demonstrated that when neighborhood collective efficacy level was higher (shown as 1 SD above mean), the association between stressful life events/racial discrimination and comorbid problems was weakened compared to when neighborhood collective efficacy level was lower (1 SD below mean). This suggests that high neighborhood collective efficacy buffered the risk effects of stressful life events and racial discrimination on comorbid problems.
Figure 4.
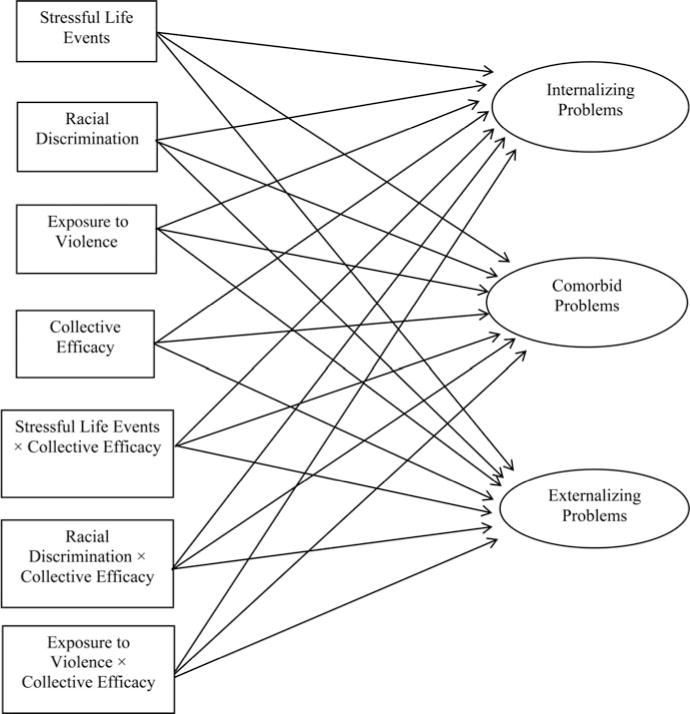
Structural equal model testing the interactions between collective efficacy and the three stressors on the latent factors. Main effect variables were Z transformed to avoid multicollinearity.
Figure 5.
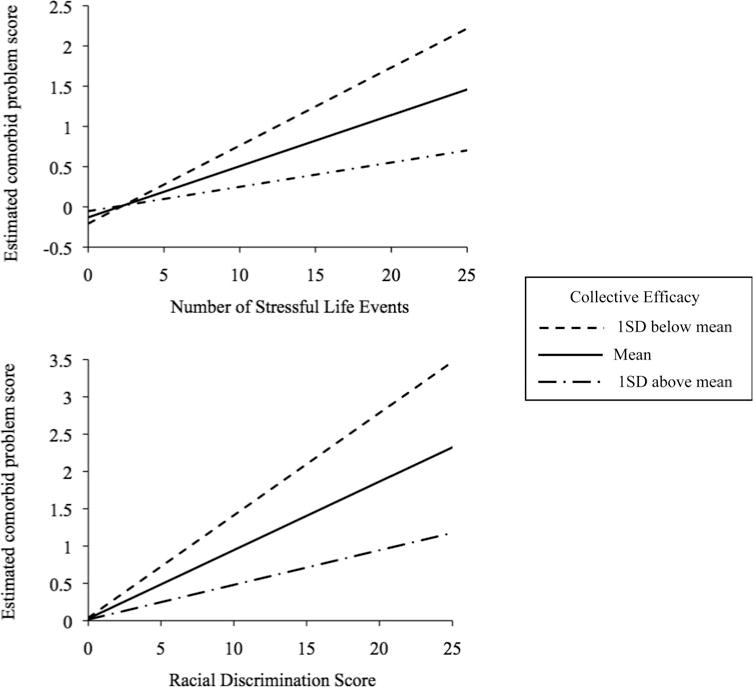
Associations between racial discrimination/stressful life events and comorbid problems at different levels of neighborhood collective efficacy.
Discussion
The present study explored the latent structure of specific and comorbid internalizing and externalizing problems in a sample of economically disadvantaged African American adolescents and investigated the impact of stressful life events, exposure to violence, racial discrimination, and neighborhood collective efficacy in the latent variable model. Our results showed a high level of comorbidity of internalizing and externalizing problems. This was evident initially via bivariate correlation among the measured variables. Relevant for latent variable modeling, parcels from both internalizing and externalizing items showed high factor loadings on the latent co-morbid factor, suggesting that a substantial portion of variation across internalizing and externalizing problems was attributed to a shared underlying factor. This result is consistent with the growing body of evidence suggesting high factor loadings of internalizing and externalizing problems on a common factor (Caspi et al., 2014; Keiley et al., 2003; Laceulle et al., 2015; Lahey et al., 2011, 2012; Olino et al., 2014). Previous studies differed substantially from each other and from the present study, in terms of participant race (predominantly White versus African American), age range (from 3 to 38 years), and measures of psychopathology (ranging from clinically diagnosed DSM disorders to quantitative measures using self-report), yet all studies found a common factor underlying a broad spectrum of internalizing and externalizing problems with high factor loadings. Collectively, these studies demonstrate the robustness of this finding across a variety of populations.
Where the present results diverge from prior reports was the observation in this study of low factor loadings of anxious/depressed and withdrawn/depressed on the specific internalizing factor. Laceulle et al. (2015) measured a comparable set of anxious/depressed and withdrawn/depressed problems among Dutch adolescents and found similarly low factor loading (0.39 and 0.14) on a specific internalizing factor. However, they also measured other DSM internalizing symptoms, such as general anxiety disorder, social anxiety, and panic disorder, and found relatively higher loadings (0.21–0.59) on the internalizing factor. Other studies that have used the bifactor model have not specifically analyzed the anxious/depressed and withdrawn/depressed subscales; therefore, results were not directly comparable to the present study. However, regardless of whether data were obtained via diagnostic interview or questionnaire measures among adolescents or adults, internalizing problems in general seem to show lower factor loadings on its specific factor compared to externalizing problems (Caspi et al., 2014; Kim & Eaton, 2015; Laceulle et al., 2015; Lahey et al., 2012). One exception is a report that described comparably moderate factor loadings for internalizing and externalizing problems on their respective specific factors (Keiley et al., 2003). However, that study was based on maternal and teacher report among children 5 to 14 years. The observed structure of internalizing and externalizing problems may vary by informant (Youngstrom, Findling, & Calabrese, 2003) or by developmental changes prior and subsequent to the transition to adolescence.
Even among prior studies reporting relatively low factor loadings of internalizing problems on a specific internalizing factor, none reported factor loadings of anxious/depressed and withdrawn/depressed as low as those found in the present study. There are several possible explanations for this difference. First, compared to White and Hispanic Americans, African American youth are less likely to co-endorse somatic symptoms along with affective symptoms of depression; instead, somatic symptoms among African Americans are a relatively distinct component of health problems (Choi & Park, 2006). Consistent with this notion, in the present study, somatic complaints loaded primarily onto the specific internalizing factor whereas anxious/depressed and withdrawn/depressed both had only very low factor loadings on that same factor that were not statistically significant. Second, African American youth show distinct symptom expressions of internalizing problems compared to other racial and ethnic groups. Anderson and Mayes (2010) reported that compared to White youth, African American youth are more likely to express depression as anger, aggression, and irritability, which may outwardly manifest as externalizing problems. This may explain why symptoms of anxious/depressed and withdrawn/depressed in the present sample showed high co-morbidity with observed externalizing problems but retained very little unique variance. Third, the present sample was drawn from high-poverty inner-city neighborhoods. Poverty is a documented risk factor for both internalizing and externalizing problems (Yoshikawa, Aber, & Beardslee, 2012). Thus, it is also possible that chronic exposure to poverty and its related risk factors could more commonly precipitate the development of comorbid problems rather than a specific type of problem (Compas & Andreotti, 2013).
African American youth are less likely to co-endorse somatic symptoms along with affective symptoms of depression; instead, somatic symptoms among African Americans are a relatively distinct component of health problems (Choi & Park, 2006). Consistent with this notion, in the present study, somatic complaints loaded primarily onto the specific internalizing factor whereas anxious/depressed and withdrawn/depressed both had only very low factor loadings on that same factor that were not statistically significant. Second, African American youth show distinct symptom expressions of internalizing problems compared to other racial and ethnic groups. Anderson and Mayes (2010) reported that compared to White youth, African American youth are more likely to express depression as anger, aggression, and irritability, which may outwardly manifest as externalizing problems. This may explain why symptoms of anxious/depressed and withdrawn/depressed in the present sample showed high co-morbidity with observed externalizing problems but retained very little unique variance. Third, the present sample was drawn from high-poverty inner-city neighborhoods. Poverty is a documented risk factor for both internalizing and externalizing problems (Yoshikawa, Aber, & Beardslee, 2012). Thus, it is also possible that chronic exposure to poverty and its related risk factors could more commonly precipitate the development of comorbid problems rather than a specific type of problem (Compas & Andreotti, 2013).
This study also found no correlation between the specific internalizing and externalizing factors, which differs from the negative correlation sometimes reported in studies using a bi-factor model structure (Caspi et al., 2014; Laceulle et al., 2015). This finding may be due to differences in how symptoms loaded onto the specific and comorbid factors in the population we targeted compared to other studies. It has been suggested that inhibition, which may be characteristic of individuals high in withdrawn/depressed or anxious/depressed symptoms, is “protective” against externalizing problems (e.g., Schwartz, Snidman, & Kagan, 1996). In that view, once the comorbidity of internalizing and externalizing is modeled, the residual specific factors would show a negative correlation (Caspi et al., 2014; Laceulle et al., 2015). This would not be expected in populations where the specific internalizing factor mainly represents somatic symptoms, whereas withdrawn/depressed and anxious/depressed are largely loading onto a comorbid factor along with externalizing problems. This is precisely what was observed in our sample of African American youth from high-poverty, high-violence neighborhoods. By teasing apart the comorbid component underlying internalizing and externalizing problems from their specific components, the latent comorbid model clarifies the often perplexing relations observed between internalizing and externalizing symptoms.
In brief, the latent structure of internalizing and externalizing problems in the present sample demonstrated acomorbid factor as a core feature of psychopathology, a model that is gaining traction in developmental psychopathology. At the same time, the unique findings in the present study with respect to how internalizing and externalizing items loaded onto specific and comorbid factors highlight the importance of applying the latent modeling approach to a diverse set of populations, including those from difficult to reach communities. By separating the comorbid factor from the specific factors underlying internalizing and externalizing problems, our results show distinct impacts of several environmental stressors and the protective effect of collective efficacy on internalizing and externalizing problems via various underlying components.
With respect to racial discrimination, this stressor has previously been shown to negatively impact both internalizing and externalizing problems (e.g., Clark et al., 1999; Williams & Mohammed, 2009). The present study incorporated racial discrimination as a predictor in the bifactor model representing specific and comorbid problems. In so doing, our results demonstrated that among African American youth from disadvantaged neighborhoods, the impact of racial discrimination on internalizing and externalizing problems may be fully attributed to their shared component, as racial discrimination did not show an effect on either the specific internalizing (somatic) or externalizing factor. These findings suggest that studies using a traditional regression approach, regardless of whether comorbidity was not assessed or statistically controlled for, may have overlooked the effects on comorbidity between internalizing and externalizing problems. These findings demonstrate the importance of representing both comorbid and specific components underlying psychopathology.
The number of recent stressful life events was significantly associated with higher comorbid and specific externalizing problems but not specific internalizing problems. The results of this study clarify prior research on the association of stressful life events in this population. Using traditional measured variables of internalizing and externalizing problems, the effect of stressful life events on internalizing problems was previously reported as partially mediated by externalizing problems (Liu et al., 2016). However, the latent structure revealed in the best fitting latent variable model demonstrated that the bulk of the variation in internalizing problems in this population was largely accounted for by a comorbid factor, with anxious/depressed and withdrawn/depressed symptoms loading almost exclusively on this factor. Stressful life events predicted the comorbid factor but not the specific internalizing factor, the latter of which reflected only somatic symptoms in this population of African American youth from economically disadvantaged neighborhoods. For externalizing problems, the present results were consistent with and expanded upon prior findings. Among White and mixed-race samples, stressful life events have previously been shown to predict externalizing problems (Grant, Compas, Thurm, McMahon, & Gipson, 2004). The present findings expand upon these findings in demonstrating that among high-risk African American adolescents, stressful life events was associated with externalizing problems, and that it did so via effects on a latent externalizing factor as well as a comorbid factor.
For exposure to violence, this risk factor has been associated with externalizing problems in some studies of African American adolescents (e.g., Lambert et al., 2012; Sanchez et al., 2013) but not others (e.g., Cooley-Quille et al., 2001; Grant et al., 2005). By isolating the comorbid factor from the specific factor underlying externalizing problems, our results indicated that exposure to violence impacted externalizing problems exclusively via the specific component but not the comorbid component. These findings enabled a clearer understanding that exposure to violence predicts externalizing problems specifically and further illustrates the advantages of employing a bifactor solution incorporating both specific and comorbid components to understanding risks for developmental psychopathology.
Higher neighborhood collective efficacy was associated with lower comorbid problems and specific externalizing problems but not specific internalizing problems. Moreover, the results showed that collective efficacy buffered the risk effects of stressful life events and racial discrimination on co-morbid problems. These results supported the protective effect of collective efficacy on internalizing and externalizing problems both directly and by mitigating the effects of other risk factors.
Neighborhood collective efficacy appeared to be a distinct predictor of internalizing/externalizing problems, as it was not correlated with any of the three stressor types assessed in this study. Of note, this stands in contrast to some prior research documenting an association of higher collective efficacy with lower violence in Chicago neighborhoods (Morenoff, Sampson, & Raudenbush, 2001; Sampson et al., 1997). However, the studies conducted in Chicago neighborhoods drew from a wide range of socioeconomic and racial backgrounds, whereas the present study specifically targeted high-poverty neighborhoods. Previous research suggests that economically disadvantaged neighborhoods often show lower collective efficacy (Kilewer, 2013; Sampson et al., 1997). The average reported collective efficacy in the present study (M = 2.8) seemed to be lower than reported in previous studies (e.g., M = 3.9; Morenoff et al., 2001). Nevertheless, the present study is the first to report that higher collective efficacy buffers the risks of stressful life events and racial discrimination on a shared component underlying both internalizing and externalizing problems.
Interpretations of this data should be made in light of some limitations. First, we specifically targeted African American youth from extremely disadvantaged neighborhoods; thus, the results may differ compared to other racial or economic groups. Nevertheless, the successful recruitment of a population of youth who are traditionally underrepresented in research and difficult to reach is a strength of the study. More-over, focusing on disadvantaged neighborhoods may have increased the internal validity of the findings, as we eliminated potentially unmeasured confounding effects of socioeconomic status, which is often the case in studies of populations with heterogeneous socioeconomic backgrounds (for a discussion, see Umlauf, Bolland, & Lian, 2011). Second, environmental stressors and mental health problems often show reciprocal influences over time (e.g., Grant et al., 2004; Kim et al., 2003). The present study demonstrated that environmental stressors were associated with comorbid and specific externalizing problems, but due to the cross-sectional nature of the study, we were unable to examine whether the specific and co-morbid components of psychopathology predict future incidences of stressful events. The latent bifactor model should be applied to existing and novel longitudinal studies to elucidate the developmental trajectories of specific and comorbid components underlying internalizing and externalizing problems. Third, reports of collective efficacy in the present study were based on participants’ reported characteristics of the neighborhoods. Comparisons of self-report to other objective neighborhood measures (e.g., presence of neighborhood watch groups) would be important to address in future research. Fourth, future studies incorporating genetic risk factors into latent variable models are also needed. One twin study examining heritability of the latent components underlying DSM disorders found that a latent factor common to internalizing and externalizing problems can be largely attributed to shared genetic risk factors (Lahey et al., 2011). With the latent structure of internalizing and externalizing problems established, genetic factors and gene–environment interactions can be easily adapted to the latent modeling framework.
Acknowledgments
This project was supported by a grant from the National Institute on Drug Abuse (RO1DA025039). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
References
- Aber JL, Gephait MA, Brooks-Gunn J, Cornell JP. Development in context: Implications for studying neighborhood effects. Neighborhood Poverty: Context and Consequences for Children. 1997;7:44–61. [Google Scholar]
- Achenbach TM. Manualforthe YouthSelf-Reportformand 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Ahern J, Cerda M, Lippnnan SA, Tardiff KJ, Vlahov D, Galea S. Navigating non-positivity in neighbourhood studies: An analysis of collective efficacy and violence. Journal of Epidemiology and Community Health. 2013;67:159–165. doi: 10.1136/jech-2012-201317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Anderson ER, Mayes LC. Race/ethnicity and internalizing disorders in youth: A review. Clinical Psychology Review. 2010;30:338–348. doi: 10.1016/j.cpr.2009.12.008. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. doi: 10.1017/S0021963098003448. [DOI] [PubMed] [Google Scholar]
- Attar BK, Guerra NG, Tolan PH. Neighborhood disadvantage, stressful life events and adjustments in urban elementary-school children. Journal of Clinical Child Psychology. 1994;23:391–400. [Google Scholar]
- Banks KH, Kohn-Wood LP, Spencer M. An examination of the African American experience of everyday discrimination and symptoms of psychological distress. Community Mental Health Journal. 2006;42:555–570. doi: 10.1007/s10597-006-9052-9. [DOI] [PubMed] [Google Scholar]
- Beyers JM, Loeber R. Untangling developmental relations between depressedmood and delinquency in male adolescents. Journal of Abnormal Child Psychology. 2003;31:247–266. doi: 10.1023/a:1023225428957. 101023/A:1023225428957. [DOI] [PubMed] [Google Scholar]
- Bhargava S, Witherspoon DP. Parental involvement across middle and high school: Exploring contributions of individual and neighborhood characteristics. Journal of Youth and Adolescence. 2015;44:1702–1719. doi: 10.1007/sl0964-015-0334-9. [DOI] [PubMed] [Google Scholar]
- Boyd-Franklin N. Five key factors in the treatment of Black families. Journal of Psychotherapy and the Family. 1989;6:53–69. doi: 10.1300/J287v06n01_04. [DOI] [Google Scholar]
- Boyle MH, Offord DR, Racine Y, Szatmari P, Fleming JE, San-ford M. Identifying thresholds for classifying childhood psychiatric disorder: Issues and prospects. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:1440–1448. doi: 10.1097/00004583-199611000-00012. [DOI] [PubMed] [Google Scholar]
- Brody GH, Beach SH, Chen Y, Obasi E, Philibert RA, Kogan SM, Simons RL. Perceived discrimination, serotonin transporter linked polymorphic region status, and the development of conduct problems. Development and Psychopathology. 2011;23:617–627. doi: 10.1017/S0954579411000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Chen YF, Murry VM, Ge X, Simons RL, Gibbons FX, Cutrona CE. Perceived discrimination and the adjustment of African American youths: A five-year longitudinal analysis with contextual moderation effects. Child Development. 2006;77:1170–1189. doi: 10.1111/j.1467-8624.2006.00927.x. [DOI] [PubMed] [Google Scholar]
- Brody GH, Ge X, Conger R, Gibbons FX, Murry VM, Gerrard M, Simons RL. The influence of neighborhood disadvantage, collective socialization, and parenting on African American children’s affiliation with deviant peers. Child Development. 2001;72:1231–1246. doi: 10.1111/1467-8624.00344. Retrieved from http://www.jstor.org/stable/1132439. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22 ITS-HAl. [Google Scholar]
- Brown DL, Tylka TL. Racial discrimination and resilience in African American young adults: Examining racial socialization as a moderator. Journal of Black Psychology. 2011;37:259–285. doi: 10.1177/0095798410390689. [DOI] [Google Scholar]
- Browning CR, Gardner M, Maimon D, Brooks-Gunn J. Collective efficacy and the contingent consequences of exposure to life-threatening violence. Developmental Psychology. 2014;50:1878–1890. doi: 10.1037/a0036767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byck GR, Bolland J, Dick D, Ashbeck AW, Mustanski BS. Prevalence of mental health disorders among low-income African American adolescents. Social Psychiatry and Psychiatric Epidemiology. 2013;48:1555–1567. doi: 10.1007/s00127-013-0657-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byck GR, Bolland J, Dick D, Swann G, Henry D, Mustanski B. Effect of housing relocation and neighborhood environment on adolescent mental and behavioral health. Journal of Child Psychology and Psychiatry. 2015 doi: 10.1111/jcpp.l2386. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bynum MS, Burton ET, Best C. Racism experiences and psychological functioning in African American college freshmen: Is racial socialization a buffer? Cultural Diversity and Ethnic Minority Psychology. 2007;13:64–11. doi: 10.1037/1099-9809.13.1.64. [DOI] [PubMed] [Google Scholar]
- Carlson KT. Poverty and youth violence exposure: Experiences in rural communities. Children and Schools. 2006;28:87–96. doi: 10.1093/cs/28.2.87. [DOI] [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry. 1991;32:1063–1080. doi: 10.1111/j.1469-7610.199l.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SI, Harrington H, Israel S, Moffitt TE. The p factor: One general psychopath ology factor in the structure of psychiatric disorders? Clinical Psychological Science. 2014;2:119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda M, Sagdeo A, Galea S. Comorbid forms of psychopa-thology: Key patterns and future research directions. Epidemiologic Reviews. 2008;30:155–177. doi: 10.1093/epirev/mxn003. [DOI] [PubMed] [Google Scholar]
- Choi H. Understanding adolescent depression in ethnocultural context. Advances in Nursing Science. 2002;25:71–85. doi: 10.1097/00012272-200212000-00006. [DOI] [PubMed] [Google Scholar]
- Choi H, Park CG. Understanding adolescent depression in ethnocultural context: Updated with empirical findings. Advances in Nursing Science. 2006;29:E1–E12. doi: 10.1097/00012272-200610000-00009. Retrieved from http://journals.lww.com/advancesinnursingscience/toc/2006/10000. [DOI] [PubMed] [Google Scholar]
- Chou K. Perceived discrimination and depression among new migrants to Hong Kong: The moderating role of social support and neighborhood collective efficacy. Journal of Affective Disorders. 2012;138:63–70. doi: 10.1016/j.jad.2011.12.029. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology. 2002;70:6–20. doi: 10.1037//0022-006x.70.1.6. [DOI] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- Compas BE, Andreotti C. Risk and resilience in child and adolescent psychopathology. In: Beauchaine TP, Hinshaw SP, editors. Child and adolescent psychopathology. Hoboken, NJ: Wiley; 2013. pp. 143–170. [Google Scholar]
- Cooley-Quille M, Boyd RC, Frantz E, Walsh J. Emotional and behavioral impact of exposure to community violence in inner-city adolescents. Journal of Clinical Child Psychology. 2001;30:199–206. doi: 10.1207/S15374424JCCP3002_7. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RE, Noordhof A, Skodol AE, Mar-kon KE, Hasin DS. Ethnicity and psychiatric comorbidity in a national sample: Evidence for latent comorbidity factor invariance and connections with disorder prevalence. Social Psychiatry and Psychiatric Epidemiology. 2013;48:701–710. doi: 10.1007/s00127-012-0595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Rodriguez-Seijas C, Carragher N, Krueger RF. Transdiagnostic factors of psychopathology and substance use disorders: A review. Social Psychiatry and Psychiatric Epidemiology. 2015;50:171–182. doi: 10.1007/s00127-014-1001-2. [DOI] [PubMed] [Google Scholar]
- Eaton NR, South SC, Krueger RF. The meaning of comorbidity among common mental disorders. In: Millon T, Krueger R, Simonsen E, editors. Contemporary directions in psychopathology: Scientific foundations of the DSM-V and ICD-11. 2nd. New York: Guilford Press; 2010. pp. 223–241. [Google Scholar]
- English D, Lambert SF, Evans MK, Zonderman AB. Neighborhood racial composition, racial discrimination, and depressive symptoms in African Americans. American Journal of Community Psychology. 2014;54:219–228. doi: 10.1007/sl0464-014-9666-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, English K. The environment of poverty: Multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Development. 2002;73:1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- Fagan AA, Wright EM, Pinchevsky GM. The protective effects of neighborhood collective efficacy on adolescent substance use and violence following exposure to violence. Journal of Youth and Adolescence. 2014;43:1498–1512. doi: 10.1007/sl0964-013-0049-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler PJ, Tompsett CJ, Braciszewski JM, Jacques-Tiura A, Baltes BB. Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Development and Psychopathology. 2009;21:227–259. doi: 10.1017/S0954579409000145. [DOI] [PubMed] [Google Scholar]
- Garcia Coll C, Crnic K, Lamberty G, Wasik BH, Jenkins R, Garcia HV, McAdoo HP. An integrative model for the study of developmental competencies in minority children. Child Development. 1996;67:1891–1914. doi: 10.1111/j.1467-8624.1996.tb01834.x. [DOI] [PubMed] [Google Scholar]
- Gaylord-Harden NK, Elmore CA, Campbell CL, Wethington A. An examination of the tripartite model of depressive and anxiety symptoms in African American youth: Stressors and coping strategies as common and specific correlates. Journal of Clinical Child and Adolescent Psychology. 2011;40:360–374. doi: 10.1080/15374416.2011.563467. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hedeker DR. Full-information item bi-factor analysis. Psychometrika. 1992;57:423–436. doi: 10.1007/BF02295430. [DOI] [Google Scholar]
- Gibbons FX, Yen H, Gerrard M, Cleveland MJ, Cutrona C, Simons RL, Brody GH. Early experience with racial discrimination and conduct disorder as predictors of subsequent drug use: A critical period hypothesis. Drug and Alcohol Dependence. 2007;88:27–37. doi: 10.1016/j.drugalcdep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman-Smith D, Tolan P. The role of exposure to community violence and developmental problems among inner-city youth. Development and Psychopathology. 1998;10:101–116. doi: 10.1017/s0954579498001539. [DOI] [PubMed] [Google Scholar]
- Grant KE, Compas BE, Thurm AE, McMahon SD, Gipson PY. Stressors and child and adolescent psychopathology: Measurement issues and prospective effects. Journal of Clinical Child and Adolescent Psychology. 2004;33:412–425. doi: 10.1207/s15374424jccp3302_23. [DOI] [PubMed] [Google Scholar]
- Grant KE, Compas BE, Thurm AE, McMahon SD, Gipson PY, Campbell AJ, Westerholm RI. Stressors and child and adolescent psychopathology: Evidence of moderating and mediating effects. Clinical Psychology Review. 2006;26:257–283. doi: 10.1016/j.cpr.2005.06.011. [DOI] [PubMed] [Google Scholar]
- Grant KE, McCormick A, Poindexter L, Simpkins T, Janda CM, Thomas KJ, Taylor J. Exposure to violence and parenting as mediators between poverty and psychological symptoms in urban African American adolescents. Journal of Adolescence. 2005;28:507–521. doi: 10.1016/j.adolescence.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Ha C, Balderas JC, Zanarini MC, Oldham J, Sharp C. Psychiatric comorbidity in hospitalized adolescents with borderline personality disorder. Journal of Clinical Psychiatry. 2014;75:e457–e464. doi: 10.4088/JCP13m08696. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Ingram RE, Price JM. Vulnerability to psychopathology: Risk across the lifespan. 2nd. New York: Guilford Press; 2010. [Google Scholar]
- Keiley MK, Lofthouse N, Bates JE, Dodge KA, Pettit GS. Differential risks of covarying and pure components in mother and teacher reports of externalizing and internalizing behavior across ages 5 to 14. Journal of Abnormal Child Psychology. 2003;31:267–283. doi: 10.1023/A:1023277413027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler LA, Berglund P, Green JG, McLaughlin KA, Fayyad J, Zaslavsky AM. The effects of temporally secondary co-morbid mental disorders on the associations of DSM-IV ADHD with adverse outcomes in the US national comorbidity survey replication adolescent supplement (NCS-A) Psychological Medicine. 2014;44:1779–1792. doi: 10.1017/S0033291713002419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Dernier O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Esh-leman S, Kendler KS. Lifetime and 12-month prevalence of DSM-m—R psychiatric disorders in the United States: Results from the national comorbidity study. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.l994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kilewer W. The role of neighborhood collective efficacy and fear of crime in socialization of coping with violence in low-income communities. Journal of Community Psychology. 2013;41:920–930. doi: 10.1002/jcop.21573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KJ, Conger RD, Elder GHJ, Lorenz FO. Reciprocal influences between stressful life events and adolescent internalizing and externalizing problems. Child Development. 2003;74:127–143. doi: 10.1111/1467-8624.00525. [DOI] [PubMed] [Google Scholar]
- Kim H, Eaton NR. The hierarchical structure of common mental disorders: Connecting multiple levels of comorbidity, bifactor models, and predictive validity. Journal of Abnormal Psychology. 2015;124:1064. doi: 10.1037/abn0000113. [DOI] [PubMed] [Google Scholar]
- King KM, Chassin L. Adolescent stressors, psychopathology, and young adult substance dependence: A prospective study. Journal of Studies on Alcohol and Drugs. 2008;69:629–638. doi: 10.15288/jsad.2008.69.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laceulle OM, Vollebergh WAM, Ormel J. The structure of psychopathology in adolescence: Replication of a general psychopathology factor in the TRAILS study. Clinical Psychological Science. 2015 doi: 10.1177/2167702614560750. Advance online publication. [DOI] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Ra-thouz PJ. Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology. 2012;121:971–977. doi: 10.1037/a0028355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, VanHulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68:181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert SF, Boyd RC, Cammack NL, Ialongo NS. Relationship proximity to victims of witnessed community violence: Associations with adolescent internalizing and externalizing behaviors. American Journal of Orthopsychiatry. 2012;82:1–9. doi: 10.1111/j.1939-0025.2011.01135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert SF, Robinson WL, Ialongo NS. The role of socially prescribed perfectionism in the link between perceived racial dissimulation and African American adolescents’ depressive symptoms. Journal of Abnormal Child Psychology. 2014;42:577–587. doi: 10.1007/sl0802-013-9814-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrine H, Klonoff EA. The schedule of racist events: A measure of racial discrimination and a study of its negative physical and mental health consequences. Journal of Black Psychology. 1996;22:144–168. doi: 10.1177/00957984960222002. [DOI] [Google Scholar]
- Lansford JE, Malone PS, Stevens KI, Dodge KA, Bates JE, Pettit GS. Developmental trajectories of externalizing and internalizing behaviors: Factors underlying resilience in physically abused children. Development and Psychopathology. 2006;18:35–55. doi: 10.1017/S0954579406060032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CS, Goldstein SE. Loneliness, stress, and social support in young adulthood: Does the source of support matter? Journal of Youth and Adolescence. 2016;45:568–580. doi: 10.1007/sl0964-015-0395-9. [DOI] [PubMed] [Google Scholar]
- Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling. 2002;9:151–173. [Google Scholar]
- Liu J, Borland J, Dick D, Mustanski B, Kertes DA. Effect of environmental risk and externalizing comorbidity on internalizing problems among economically disadvantaged African American youth. Journal of Research on Adolescence. 2016;26:552–566. doi: 10.1111/jora.12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazerolle L, Wickes R, McBroom J. Community variations in violence: The role of social ties and collective efficacy in comparative context. Journal of Research in Crime and Delinquency. 2010;47:3–30. doi: 10.1177/0022427809348898. [DOI] [Google Scholar]
- Morenoff JD, Sampson RJ, Raudenbush SW. Neighborhood inequality, collective efficacy, and the spatial dynamics of urban violence. Criminology. 2001;39:517–559. [Google Scholar]
- Mrug S, Windle M. Prospective effects of violence exposure across multiple contexts on early adolescents internalizing and externalizing problems. Journal of Child Psychology and Psychiatry. 2010;51:953–961. doi: 10.1111/j.l469-7610.2010.02222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user’s guide. 7th. Los Angeles: Author; 2012. [Google Scholar]
- Nyborg VM, Curry JF. The impact of perceived racism: Psychological symptoms among African American boys. Journal of Clinical Child and Adolescent Psychology. 2003;32:258–266. doi: 10.1207/S15374424JCCP3202_11. [DOI] [PubMed] [Google Scholar]
- Olino TM, Dougherty LR, Bufferd SJ, Carlson GA, Klein DN. Testing models of psychopathology in preschool-aged children using a structured interview-based assessment. Journal of Abnormal Child Psychology. 2014;42:1201–1211. doi: 10.1007/sl0802-014-9865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plomin R, Haworth CMA, Davis OSP. Common disorders are quantitative traits. Nature Reviews Genetics. 2009;10:872–878. doi: 10.1038/nrg2670. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Stohl M, Hasin DS, Eaton NR. Trans-diagnostic factors and mediation of the relationship between perceived racial discrimination and mental disorders. JAMA Psychiatry. 2015;72:706–713. doi: 10.1001/jamapsychiatry.2015.0148. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sanchez YM, Lambert SF, Cooley-Strickland M. Adverse life events, coping and internalizing and externalizing behaviors in urban African American youth. Journal of Child and Family Studies. 2013;22:38–47. [Google Scholar]
- Schwartz CE, Snidman N, Kagan J. Early childhood temperament as a determinant of externalizing behavior in adolescence. Development and Psychopathology. 1996;8:527–537. doi: 10.1017/S0954579400007252. [DOI] [Google Scholar]
- Satorra A, Bentler PM. Corrections to test statistics and standard errors in covariance structure analysis. In: von Eye A, Clogg CC, editors. Latent variables analysis: Applications for developmental research. Thousand Oaks, CA: Sage; 1994. pp. 399–419. [Google Scholar]
- Sentse M, Ormel J, Veenstra R, Verhulst FC, Oldehinkel AJ. Child temperament moderates the impact of parental separation on adolescent mental health: The TRAILS study. Journal of Family Psychology. 2011;25:97–106. doi: 10.1037/a0022446. 10.1037Va0022446. [DOI] [PubMed] [Google Scholar]
- Sterrett EM, Dymnicki AB, Henry D, Byck G, Borland J, Mustanski B. Predictors of co-occurring risk behavior trajectories among economically disadvantaged African American youth: Contextual and individual factors. Journal of Adolescent Health. 2014;55:380–387. doi: 10.1016/j.jadohealth.2014.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud LR, Foster E, Papandonatos GD, Handwerger K, Granger DA, Kivlighan KT, Niaura R. Stress response and the adolescent transition: Performance versus peer rejection stressors. Development and Psychopathology. 2009;21:47–68. doi: 10.1017/S0954579409000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Woodward AT, Brown E. Racial and ethnic differences in extended family, friendship, fictive kin, and congregational informal support networks. Family Relations. 2013;62:609–624. doi: 10.1111/fare.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmermans M, van Lier PAC, Koot HM. The role of stressful events in the development of behavioural and emotional problems from early childhood to late adolescence. Psychological Medicine. 2010;40:1659–1668. doi: 10.1017/S0033291709992091. [DOI] [PubMed] [Google Scholar]
- Umlauf M, Borland J, Lian B. Sleep disturbance and risk behaviors among inner-city African-American adolescents. Journal of Urban Health. 2011;88:1130–1142. doi: 10.1007/sl1524-011-9591-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widiger TA, Samuel DB. Diagnostic categories or dimensions? A question for the Diagnostic and Statistical Manual of Mental Disorders—Fifth edition. Journal of Abnormal Psychology. 2005;114:494–504. doi: 10.1037/0021-843X.114.4.494. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshikawa H, Aber JL, Beardslee WR. The effects of poverty on the mental, emotional, and behavioral health of children and youth: Implications for prevention. American Psychologist. 2012;67:272–284. doi: 10.1037/a0028015. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Findling RL, Calabrese JR. Who are the comorbid adolescents? Agreement between psychiatric diagnosis, youth, parent, and teacher report. Journal of Abnormal Child Psychology. 2003;31:231–245. doi: 10.1023/A:1023244512119. [DOI] [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. American Journal of Public Health. 2005;95:660–667. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]


