Abstract
Study Design:
This was a retrospective cohort study.
Objective:
To report our 10-year experience of closed reduction using Crutchfield traction followed by anterior cervical discectomy and fusion within 12 h from injury for C-type subaxial cervical fractures (according to the AOSpine classification system).
Methods:
Clinical records and neuroimaging were retrospectively reviewed. Surgical details were provided.
Results:
A total of 22 patients were included in the study. The cervical fracture was diagnosed after whole-body computed tomography scan on admission in all cases. Crutchfield traction was applied within 1–5 h from the diagnosis. Surgery consisting of anterior microdiscectomy and fusion with interbody cage and plating was performed 6–12 h after traction positioning. Most patients (19, 86%) had spinal cord injury: 7 were Frankel A (31%), 3 Frankel B (14%), 6 Frankel C (27%), 3 Frankel D (14%), and 3 Frankel E (14%). No neurologic deterioration was observed after the treatment. In 10 cases (45%), neurological symptoms improved 1 year after the trauma. Two patients (10%) died for complication related to spinal cord transition or other organ damage.
Conclusions:
Early reduction gives the best chance of recovery for patients affected by C-type subaxial cervical fracture. Rapid traction is more often successful and safer than manipulation under anesthesia. After close reduction achieving, anterior microdiscectomy, cage, and plating implant seem to be safe and effective with a low rate of complications.
Keywords: Cervical fracture, cervical traction, Crutchfield traction, spinal trauma
INTRODUCTION
According to the AOSpine subaxial cervical spine injury classification system, C-type fractures include injuries with displacement or translation of one vertebral body in any direction (“translational injury in any axis”).[1] They represent a large group of morphologically complex fracture, typically occurring after high kinetic energy trauma. Even if all the spinal surgeons working in a trauma center experience with this injury, there are still insufficient evidence to recommend treatment standards and guidelines.[2] Options include closed or open reduction, anterior, posterior, or combined arthrodesis. The aim of the study is to describe our 10-year experience of closed reduction using Crutchfield traction followed by anterior cervical discectomy and fusion (ACDF) within 12 h from injury.
METHODS
We conducted a retrospective cohort study including consecutive patients affected by C-type subaxial cervical fractures, operated by one main surgeon from January 2007 to December 2016. Participants were selected after surgical record review. Inclusion criteria were fractures with vertebral body displacement or translation involving cervical segments from C3 to C7. Exclusion criteria were cervical fractures with no displacement (classified as A-or B-type). After patients selection, clinical records and neuroimaging were retrospectively reviewed. We collected data about age, gender, level of fracture, neurological status on admission, the timing of cervical traction, the maximum wedge used to obtain reduction, the surgical operation, perioperative complications, and neurological status 1 year after the trauma. No Institutional Review Board approval was needed to conduct the study.
Surgical technique
The patient is placed on a radiotransparent Stryker frame in the supine position. Close monitoring of cardiac, respiratory, and hemodynamic parameters is mandatory. Crutchfield traction is applied under local anesthesia. The skin is prepped in a sterile fashion and infiltrated with an anesthetic (mepivacaine 20 mg/ml, 5 ml for each side). The pins are applied to the parietal bones, just above the equator of the skull, about 1 cm from the superior temporal line. Direct axial traction is applied with the tongs placed longitudinally in line with the external auditory meatus. The application of weight begins with 1.5 kg per superior injury level. The first X-ray scan is obtained 30-min later. If a good realignment is shown, the patient is conducted to the operative theater. If the realignment is not satisfactory, 2 more kilograms are added and one more X-ray scan is obtained. We use to increase the weight for a maximum of 6 h of traction and 25 kg of weight. If the realignment is obtained, anterior microdiscectomy, cage, and plating implant are performed. If the reduction cannot be achieved and there is no change in position of the dislocated vertebrae with progressive weight application, a magnetic resonance imaging (MRI) scan is obtained, and an open reduction with a combined (posterior and anterior) approach is the treatment of choice.
RESULTS
A total of 47 patients underwent ACDF for subaxial cervical fractures over the selected period. 25 patients were excluded because classified as A- or B-type according to AOSpine classification. A total of 22 patients were definitely enrolled for the study. They were 16 males and 6 females, the mean age was 44. The youngest was a 16-year-old male patient who reported injury after diving into a swimming pool, and the oldest was an 81-year-old male patient as result of a fall down stairs. A part of the two previous cases and a 61–year-old male who fall down stairs, the remaining patients reported injury after road accidents. The most involved levels were C4–C5, C5–C6, and C6–C7, each one in 6 cases (27%), followed by C7–D1 in 3 (14%) and C3–C4 in 1 (5%).
The cervical fracture was diagnosed after whole-body computed tomography (CT) scan on admission in all cases [Figure 1]. Crutchfield traction was applied within 1–5 h from the diagnosis [Figure 2]. X-ray scan was obtained 1 h after traction positioning; if realignment was not observed, 2 more kilograms of wedge was applied and one more X-ray scan was obtained 1 h later. The minimum wedge enough to obtain reduction was 12 kg, and the maximum 26 kg (mean 18). Surgical operation consisting of anterior microdiscectomy and fusion with interbody cage and plating was performed 6–12 h after traction positioning [Figure 3]. In all cases a subintensive or intensive monitoring of vital parameters was obtained. No patient showed symptoms related to vertebral arteries damaging.
Figure 1.
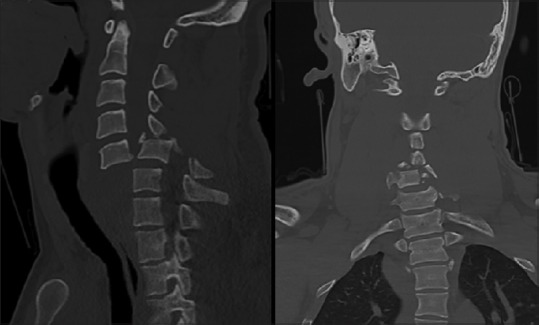
Axial and coronal computed tomography scan reconstruction showing a severe C5–C6 C-type fracture with complete ptosis of C5 vertebral body
Figure 2.

Crutchfield traction
Figure 3.

X-ray scan showing progressive realignment of the C5–C6 dislocation and fixation
Most patients (19, 86%) presented with spinal cord injury, 7 were Frankel A (31%), 3 Frankel B (14%), 6 Frankel C (27%), 3 Frankel D (14%), and 3 Frankel E (14%). No neurologic deterioration was observed after the treatment. In 10 cases (45%), neurological symptoms improved 1 year after the trauma, 2 Frankel grade in 4, and 1 Frankel grade in 4. 2 patients (10%) had died for complications related to spinal cord injury or other organs damages. X-ray scan 1 year after surgery was obtained [Figure 4]; good fusion was observed in all cases with no delayed complication [Figure 5].
Figure 4.

C5–C6–C7 fixation 1 year after surgery X-ray scan in sitting position showing a good realignment and C5–C6 vertebral body fusion
Figure 5.
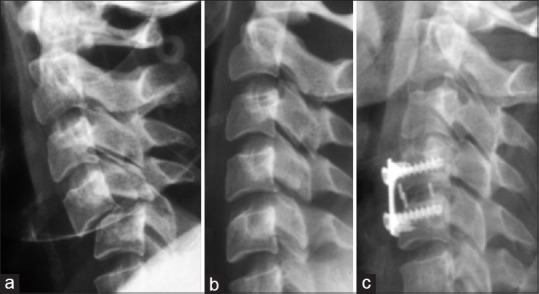
Twenty-eight-year-old female patient reported C4–C5 type C fracture after car accident, Frankel E. (a) X-ray scan before traction, (b) X-ray scan during traction, (c) intraoperative X-ray scan showing C4–C5 microdiscectomy, cage implant, and plating
DISCUSSION
Early reduction gives the best chance of recovery for patients affected by C-type cervical fracture. Rapid traction is more often successful and safer than manipulation under anesthesia.[3] Crutchfield traction, by the name of the author who first used in 1933,[4] can be considered as a part of the early overall medical management, along with close monitoring of cardiac, respiratory, and hemodynamic parameters.[5] The Gardner–Wells tong can be used with the same indication and risks[6,7]
The traction is typically arbitrarily initiated with the application of weight beginning from 1.5 kg per superior injury level. Weight may be added every 10–15–30 min. No upper limit of weight has been described in the literature; anyway, we never used a weight higher than 25 kg. In our experience, we suggest to start with a very little weight in patients under general anesthesia or affected by ankylosing spondylitis, in which 0.5–1 kg per superior injury level may be enough to accomplish reduction.
The timing is really important: Traction should be applied as soon as possible to get the greatest chance of reduction. The goal is to apply traction within 6–12 h from the trauma. Clinical evidence suggest closed reduction is not successful in patients with a fracture dislocation injury >5 days old.[8] As predictable, the best outcome is observed in young patients and in those with preserved neurological function at presentation.[9] After satisfactory realignment, anterior approach is preferred. Anterior microdiscectomy, cage, and plating implant are useful to decompress the spinal cord and stabilize the cervical spine. After closed reduction failure or contraindicated, the posterior approach consisting of open reduction followed by pedicle screw fixation is a good treatment option.[10] The common causes of closed reduction failure include severe pain and spasm, fracture fragments physically preventing reduction, and delay in the time to reduction (with partial soft tissue and bony healing).
In our series, complete reduction was observed in all cases, and no patient had neurological deterioration as a result of reduction. The incidence of neurological deterioration related to Crutchfield traction was historically reported as low, with a permanent neurological complication rate <1%. Therefore, transient neurological deterioration has been reported with an incidence between 2% and 4%.[11,12,13,14]
Contraindications to the cervical traction include an additional rostral injury, cranial fractures,[5] and atlantoaxial dislocations.[15]
Complications related to the application of the cranial tong include perforation the inner table of the skull, pin migration or pullout, and infection. Early pin migration is most likely due to inadequate pin tightening and torque; late failure may occur due to bone resorption as a response to infection or bone necrosis from pressure.[16]
The diagnosis of cervical fracture was made on whole-body CT scan findings. The use of prereduction MRI scan has not been shown to improve the safety or efficacy of closed traction-reduction in awake patients.[17] MRI scan before fracture-dislocation reduction may result in unnecessary delays in accomplishing fracture realignment and decompression of the spinal cord. Prereduction MRI assessment requires the transport of a patient with a potentially unstable cervical spinal fracture/dislocation injury to the MRI suite. Only for patients who cannot be examined because of head injury or intoxication MRI scan before attempted reduction (open or closed) is recommended.
According to the AOSpine subaxial cervical spine injury classification system, C-type includes the most morphologically complex fractures, or rather all the dislocation and luxation, regardless of mechanism of action. The previous classification system[18] included as C-type all the injuries occurred after rotation of the neck, and in it a number of subcategories not very useful to the clinical practice. There was both a simplification and an extension of the group, now including also cervical luxation caused by flexion-extension, previously classified as B-type.
The new classification is more functional in a clinical point of view because it includes as C-type a group of fractures that can be treated in the same way (using traction and ACDF), without renouncing to use descriptive subcategories.
Conclusions
Closed reduction of C-type subaxial cervical fractures by Crutchfield traction followed by ACDF seems to be safe and effective with a low rate of complication, even for severe dislocation and luxation, if used within 5 days from trauma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, et al. AOSpine subaxial cervical spine injury classification system. Eur Spine J. 2016;25:2173–84. doi: 10.1007/s00586-015-3831-3. [DOI] [PubMed] [Google Scholar]
- 2.Gelb DE, Aarabi B, Dhall SS, Hurlbert RJ, Rozzelle CJ, Ryken TC, et al. Treatment of subaxial cervical spinal injuries. Neurosurgery. 2013;72(Suppl 2):187–94. doi: 10.1227/NEU.0b013e318276f637. [DOI] [PubMed] [Google Scholar]
- 3.Lee AS, MacLean JC, Newton DA. Rapid traction for reduction of cervical spine dislocations. J Bone Joint Surg Br. 1994;76:352–6. [PubMed] [Google Scholar]
- 4.Crutchfield WG. Skeletal traction in treatment of injuries to the cervical spine. J Am Med Assoc. 1954;155:29–32. doi: 10.1001/jama.1954.03690190035010. [DOI] [PubMed] [Google Scholar]
- 5.Hadley MN, Fitzpatrick BC, Sonntag VK, Browner CM. Facet fracture-dislocation injuries of the cervical spine. Neurosurgery. 1992;30:661–6. [PubMed] [Google Scholar]
- 6.Gardner WJ. The principle of spring-loaded points for cervical traction. Technical note. J Neurosurg. 1973;39:543–4. doi: 10.3171/jns.1973.39.4.0543. [DOI] [PubMed] [Google Scholar]
- 7.Uche EO, Nwankwo OE, Okorie E, Muobike A. Skull traction for cervical spinal injury in Enugu: A 5-year retrospective multicenter analysis of the clinical outcomes of patients treated with two common devices. Niger J Clin Pract. 2016;19:580–4. doi: 10.4103/1119-3077.188713. [DOI] [PubMed] [Google Scholar]
- 8.O’Connor PA, McCormack O, Noël J, McCormack D, O’Byrne J. Anterior displacement correlates with neurological impairment in cervical facet dislocations. Int Orthop. 2003;27:190–3. doi: 10.1007/s00264-003-0449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greg Anderson D, Voets C, Ropiak R, Betcher J, Silber JS, Daffner S, et al. Analysis of patient variables affecting neurologic outcome after traumatic cervical facet dislocation. Spine J. 2004;4:506–12. doi: 10.1016/j.spinee.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Park JH, Roh SW, Rhim SC. A single-stage posterior approach with open reduction and pedicle screw fixation in subaxial cervical facet dislocations. J Neurosurg Spine. 2015;23:35–41. doi: 10.3171/2014.11.SPINE14805. [DOI] [PubMed] [Google Scholar]
- 11.Burke DC, Berryman D. The place of closed manipulation in the management of flexion-rotation dislocations of the cervical spine. J Bone Joint Surg Br. 1971;53:165–82. [PubMed] [Google Scholar]
- 12.Cloward RB. Reduction of traumatic dislocation of the cervical spine with locked facets. Technical note. J Neurosurg. 1973;38:527–31. doi: 10.3171/jns.1973.38.4.0527. [DOI] [PubMed] [Google Scholar]
- 13.Sabiston CP, Wing PC, Schweigel JF, Van Peteghem PK, Yu W. Closed reduction of dislocations of the lower cervical spine. J Trauma. 1988;28:832–5. doi: 10.1097/00005373-198806000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Farmer J, Vaccaro A, Albert TJ, Malone S, Balderston RA, Cotler JM, et al. Neurologic deterioration after cervical spinal cord injury. J Spinal Disord. 1998;11:192–6. [PubMed] [Google Scholar]
- 15.Maserati MB, Stephens B, Zohny Z, Lee JY, Kanter AS, Spiro RM, et al. Occipital condyle fractures: Clinical decision rule and surgical management. J Neurosurg Spine. 2009;11:388–95. doi: 10.3171/2009.5.SPINE08866. [DOI] [PubMed] [Google Scholar]
- 16.Krag MH, Monsey RD, Fenwick JW. Cranial morphometry related to placement of tongs in the temporoparietal area for cervical traction. J Spinal Disord. 1988;1:301–5. doi: 10.1097/00002517-198800140-00004. [DOI] [PubMed] [Google Scholar]
- 17.Vaccaro AR, Falatyn SP, Flanders AE, Balderston RA, Northrup BE, Cotler JM, et al. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine (Phila Pa 1976) 1999;24:1210–7. doi: 10.1097/00007632-199906150-00007. [DOI] [PubMed] [Google Scholar]
- 18.Blauth MK, Mair G, Schmid R, Reinhold M, Rieger M. Classification of injuries of the subaxial cervical spine. In: Aebi MA, Webb JK, editors. AO Spine Manual: Clinical Applications. Stuttgart: Thieme; 2017. pp. 21–38. [Google Scholar]


