Abstract
Background:
We are a tertiary care cancer center and have approximately 1000–1500 emergency visits by cancer patients undergoing treatment under the adult medical oncology unit each month. However, due to the lack of a systematic audit, we are unable to plan steps toward the improvement in quality of emergency services, and hence the audit was planned.
Methods:
All emergency visits under the adult medical oncology department in the month of July 2015 were audited. The cause of visit, the demographic details, cancer details, and chemotherapy status were obtained from the electronic medical records. The emergency visits were classified as avoidable or unavoidable. Descriptive statistics were performed. Reasons for avoidable emergency visits were sought.
Results:
Out of 1199 visits, 1168 visits were classifiable. Six hundred and ninety-six visits were classified as unavoidable (59.6%, 95% CI: 56.7–62.4), 386 visits were classified as probably avoidable visit (33.0%, 95% CI: 30.4–35.8) whereas the remaining 86 (7.4%, 95% CI: 6.0–9.01) were classified as absolutely avoidable. Two hundred and ninety-seven visits happened on weekends (25.6%) and 138 visits converted into an inpatient admission (11.9%). The factors associated with avoidable visits were curative intention of treatment (odds ratio - 2.49), discontinued chemotherapy status (risk ratio [RR] - 8.28), and private category file status (RR – 1.89).
Conclusion:
A proportion of visits to emergency services can be curtailed. Approximately one-fourth of patients are seen on weekends, and only about one-tenth of patients get admitted.
Keywords: Avoidable, emergency visit, medical, oncology, unavoidable
Introduction
Emergency visits by cancer patients are a source of considerable financial, physical, and psychological burden to both the patients and the health-care delivery system.[1,2,3,4] The administration of chemotherapy is associated with medical emergencies such as febrile neutropenia, tumor lysis syndrome, and electrolyte imbalances.[5] Timely interventions for these conditions are required for satisfactory outcomes.[5,6,7] Emergency visits are considered appropriate for assessing and managing such acute onset problems. However, they may also reflect on issues, not adequately addressed or managed during routine outpatient care. For example, visits to the emergency department occurring near the end of life are considered as an indicator of poor quality care for such patients.[8,9]
Nearly 25%–50% of emergency visits in Western countries are considered as avoidable.[4,10] We are a tertiary care cancer center and have nearly 1000–1500 emergency visits by cancer patients under the adult medical oncology unit each month. Systematic audit is important to plan steps toward resource allocation, triaging, and improvement in quality of emergency services. Hence, this audit was done to understand the pattern of presentation of patients visiting the emergency services. The primary objective of this analysis was to estimate the proportion of patients having absolutely avoidable visits. The secondary objectives were to identify the causes of same, to quantify the proportion of emergency visits seen on weekends, and getting indoor admission.
Methods
Study planning
This study was a retrospective cross-sectional analysis of emergency visits done under the department of adult medical oncology. The protocol for the study was approved by the Institutional Ethics Committee (IEC-III), and in view of the retrospective nature of the study, the Ethics Committee approved the investigator's request for waiver of consent. The IEC capped the study after an audit of 1300 patient records for this study.
Selection of patients
All emergency visits registered under the adult medical oncology department (age ≥15 years) were audited in a randomly selected month.
Data collection
The data regarding the cause of visit, the demographic details (age, gender, and category), cancer details (type and intention of treatment), palliative care referral (yes or no), and chemotherapy status (ongoing or stopped) were obtained from the electronic medical records.
Data interpretation
The data of cause of visit in light of the clinical records was reviewed for classification of emergency visits under the below-mentioned types. The visits were classified by a group of four medical oncologists who are teaching faculty and have an experience of more than 5 years. The cause of visits were classified as below
Oncological emergency
-
Nononcological emergency
- Blood transfusion with congestive cardiac failure
- Platelet transfusion
- Allergic reactions
-
Medical emergency
- Uncontrolled comorbidity
- Infections
- Adverse events (vomiting and nausea)
Visits for symptom management (these are ongoing symptoms which have worsened or have newly appeared or have not resolved)
Visits of emergency patients seen in outpatient department for admissions (the institute has limited inpatient beds; hence frequently patients with emergencies seen in outpatient departments who are advised admission visit the emergency services if inpatient beds were not available)
Visits for showing investigations when emergency is suspected from outpatient department
Visits for transfusions excluding details mentioned in point 2
Visits for showing investigations when emergency is not suspected from outpatient department
Visits for prescriptions
Visits of new patients not registered in hospital without any oncological emergency
Visits of patients for admissions without oncological or nononcological emergencies (these are patients who are advised admissions for indoor chemotherapy; however, they visit emergency to inform that beds were not available for admission).
These visits were classified as avoidable or unavoidable according to the cause of the visit.
Unavoidable: Causes 1–2
-
Avoidable
- Probably avoidable: Causes 3–5
- Absolutely avoidable: Causes 6–10.
Decision rule
Hypothesis for this study was that more than 80% of emergency visits would be for unavoidable causes. If the rate unavoidable visits were below 80%, then corrective steps are required toward controlling patients with avoidable causes visiting the emergency services. The primary endpoint of this study was to estimate the proportion of patients having unavoidable visits. In July 2015 (randomly selected month), 1199 patients were seen in adult medical oncology casualty. Assuming unavoidable visit rate to be around 80%, the present sample size had the ability to calculate the unavoidable proportion rate with 95% confidence interval (CI) limit of ±4.7%.
Decision rule - If the lower limit of 95% CI of proportion of patients having unavoidable visits was below 80%, then appropriate corrective measures were warranted.
Statistical analysis
Descriptive statistics were performed. 95% CI for proportions was calculated. The factors leading to avoidable visits were identified using binary logistic regression analysis. P ≤ 0.05 was considered as statistically significant.
Results
Baseline characteristics
The median age of patients was 46 years (range 16–87 years). The site of malignancy was central nervous system in 4 (0.3%), head and neck in 138 (11.6%), thoracic in 158 (13.3%), breast in 134 (11.3%), gastrointestinal in 212 (17.9%), genitourinary in 81 (6.8%), gynecological in 88 (7.3%), bone and soft tissue in 72 (6.0%), and hematological in 299 patients (25.1%). The data regarding the site of primary were missing in five patients (0.4%). The baseline details of these visits are shown in Table 1.
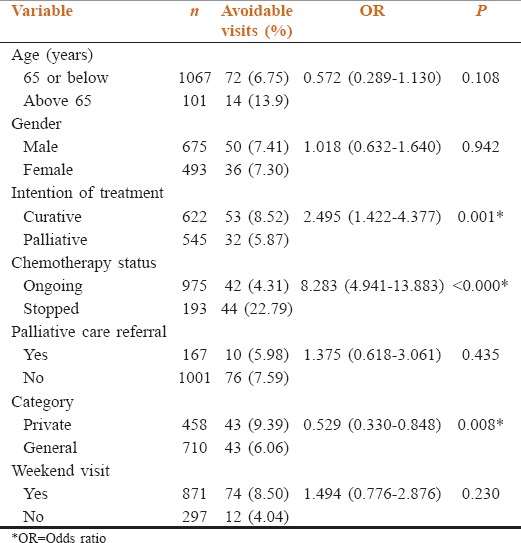
Table 1.
Baseline characteristics and their impact on avoidable emergency visit are shown
Type of visits
Out of 1186 visits, 1168 visits were classifiable. Six hundred and ninety-six visits were classified as unavoidable (59.6%, 95% CI: 56.7–62.4), 386 visits were classified as probably avoidable visit (33.0%, 95% CI: 30.4–35.8), whereas the remaining 86 (7.4%, 95% CI: 6.0–9.01) were classified as absolutely avoidable. Two hundred and ninety-seven visits happened on weekends (25.6%) and 138 visits converted into an inpatient admission (11.9%). In radically treated patients, out of 622 visits, 53 were classified as absolutely avoidable (8.5%), 155 as probably avoidable visits (24.9%), and 414 were classified as unavoidable (66.6%). In patients treated with palliative intent, 32 visits (5.9%) were classified as absolutely avoidable, 231 (42.4%) were classified as probably avoidable visit, and 282 (51.7%) as unavoidable visits. Figure 1 explains the classification of visits. The most common reason for absolutely avoidable visits was visited for showing investigations when no emergency was suspected (57 out of 86 visits), whereas the most common one for probably avoidable visit was visited for symptomology (301 out of 386 visits). Pain (242 out of 301) was the most common symptom leading to an avoidable visit in both radically and palliative intent treated patients.
Figure 1.
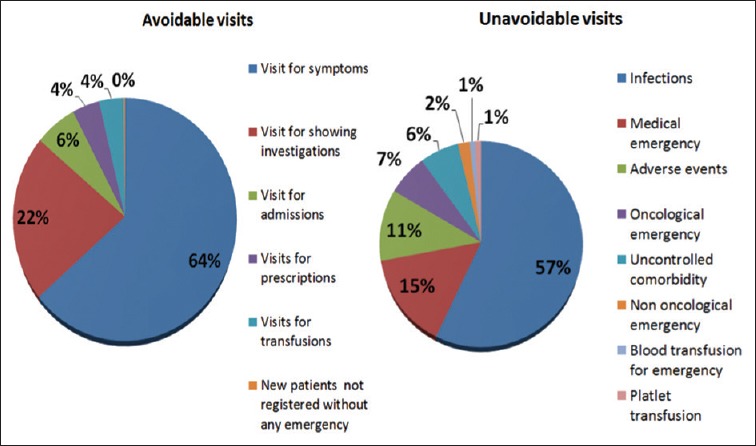
Cause of all visits
Factors leading to absolutely avoidable visits
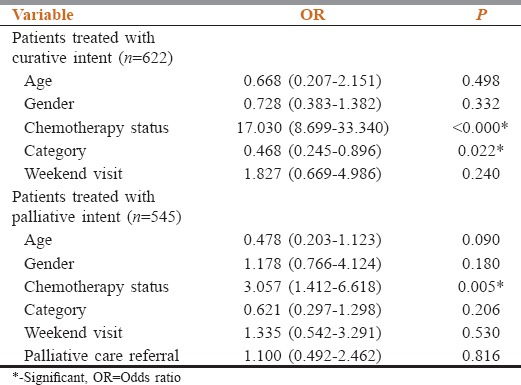
The details of factors and its relation with avoidable visits are shown in Table 1. The factors associated with absolutely avoidable visits were the curative intention of treatment (odds ratio - 2.49), discontinued chemotherapy status (risk ratio [RR] - 8.28), and private category file status (RR - 1.89). The factors contributing toward avoidable visits in curative and palliative intent patients are shown in Table 2. The factors associated with avoidable visits in radically treated patients were discontinued chemotherapy status and private file status whereas the factors in palliatively treated patients were discontinued chemotherapy status.
Table 2.
Impact of factors on avoidable emergency visit in accordance with the intention of treatment
Discussion
Evaluation and maintenance of quality of medical care require timely audits for identification of lacunae and remedial steps to correct them with potentially, further audits to identify the impact of these steps.[11] Quality check is a continuous procedure. Emergency management is an important aspect of medical oncology practice, and hence this audit was carried out by us. The goals of this audit were to obtain information which would help us inappropriate resource allocation, identify lacunae, and to suggest evidence-based remedial action if required.
The daily visits in emergency services under medical oncology were approximately forty patients per day after outpatient hours. At present, two medical oncology physicians cater to them. Unfortunately, the data regarding time to assessment and intervention postreporting to the emergency by patients was not captured in this study. This information would have enabled us to identify the time lag between patients’ presentation to the emergency and start of treatment and would have helped in resource allocation. At present, approximately forty visits are seen in 12 h; 3.33 visits per hour, as two physicians cater to them, the ratio comes to 1.67 visits per physician per hour. The American Academy of Emergency Medicine suggests a physician staffing ratio which should be ≤2.5 patients per physician per hour.[12] Hence, the workforce resource allocated for the emergency management seems adequate.
This audit identified a low rate of avoidable visits (7.4% of visits) in the emergency department. A further decrease in these visits can lead to better doctor–patient ratio in the emergency services and better utilization of workforce in patient management. The most common reasons for such avoidable visits were visits for showing investigations, for getting prescriptions, and for routine (nonemergency) blood product transfusions. Such visits can easily be curtailed further.
Our audit identified high rates of probably avoidable visits. Patients undergoing cancer treatment, especially palliative chemotherapy are likely to have symptoms, the grade and type of which would change as the natural history of the disease evolves. Inadequate symptom relief might occur due to either unaddressed symptom (or a symptom for which symptomatic care was not provided) or development of a new symptom. Inadequate symptom relief due to the prior reason would be resolved with better communication and proactive management of symptoms in the outpatient clinic. In case of new symptoms, patients could have been educated about these symptoms, and a liaison could have been arranged with the community practitioners for the management of these complaints. However, with a doctor–patient ratio of nearly 40–50 patients per medical oncologist in the outpatient department, such detailed prolonged communication is a challenge. Surprisingly, patients treated with radical intent had a high avoidable visit rate postcompletion of chemotherapy. This might reflect posttreatment anxiety related to the development of a new symptom or treatment-related side effect. This again suggests patient educational needs regarding cancer treatment side effects.
The corrective measures suggested by us are
-
Outpatient department
- Improvement of doctor–patient ratio in outpatient departments
- Preconsultation enquiry about common symptoms by a volunteer or paramedical staff and the suggestion of a remedial action till optimal doctor–patient ratio is achieved
- Group counseling of common symptoms, its management along with the disease status, and treatment counseling
- Reinforcement on counseling of acute and chronic toxicity in patients who have completed treatment with chemotherapy
- Development of post of clinician assistant or staff nurse for dedicated symptom evaluation and counseling
-
Referrals
- Liaison with community practitioners so that certain complaints can be managed by them
-
Emergency services
-
b.Developments of an emergency call service were triage can be done, and remedial actions can be suggested.
-
b.
Another important observation noted in the audit was the rate of admissions; only 11.9% of patients visiting the emergency could get admitted. This rate is very low in comparison with figures from other Western centers of 48%–63%.[13,14] This seems to be due to the unfavorable patient–bed ratio. Adult medical oncology department in the studied center has only 29 inpatient beds on general side for all purposes (inclusive for hemato-oncology and solid tumor medical oncology). With a daily outpatient load of 500–700 patients with 200–250 day-care chemotherapies have been delivered daily, these beds are grossly inadequate. Assuming conservatively that 1% of patients postchemotherapy required admission, we would have 20–25 patients daily for admissions. At present, patients requiring admissions, who are unable to get admitted are managed in emergency itself. The option of indoor admissions at centers around the hospital is provided. However, these patients do congest the emergency services hampers its effective functioning. There is evidence suggesting that such congestions lead to an increase in the emergency and inpatient mortality rate.[15,16] The steps suggested by the investigators to decrease suggestions congestions were
To increase the inpatient beds
Liaison with community practitioners and hospitals so that patients requiring inpatient care can be provided the same.
Conclusion
The current study identified potentially correctable lacunae in our emergency services. A proportion of visits to emergency services can be curtailed. There is a need to address patients who require inpatient admission.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shemesh E, Keshavarz R, Leichtling NK, Weinberg E, Mousavi A, Sadow K, et al. Pediatric emergency department assessment of psychological trauma and posttraumatic stress. Psychiatr Serv. 2003;54:1277–81. doi: 10.1176/appi.ps.54.9.1277. [DOI] [PubMed] [Google Scholar]
- 2.Fortner BV, Okon TA, Portenoy RK. A survey of pain-related hospitalizations, emergency department visits, and physician office visits reported by cancer patients with and without history of breakthrough pain. J Pain. 2002;3:38–44. doi: 10.1054/jpai.2002.27136. [DOI] [PubMed] [Google Scholar]
- 3.Henson LA, Gao W, Higginson IJ, Smith M, Davies JM, Ellis-Smith C, et al. Emergency department attendance by patients with cancer in their last month of life: A systematic review and meta-analysis. J Clin Oncol. 2015;33:370–6. doi: 10.1200/JCO.2014.57.3568. [DOI] [PubMed] [Google Scholar]
- 4.Delgado-Guay MO, Kim YJ, Shin SH, Chisholm G, Williams J, Allo J, et al. Avoidable and unavoidable visits to the emergency department among patients with advanced cancer receiving outpatient palliative care. J Pain Symptom Manage. 2015;49:497–504. doi: 10.1016/j.jpainsymman.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Lewis MA, Hendrickson AW, Moynihan TJ. Oncologic emergencies: Pathophysiology, presentation, diagnosis, and treatment. CA Cancer J Clin. 2011;61:287–314. doi: 10.3322/caac.20124. [DOI] [PubMed] [Google Scholar]
- 6.Pi J, Kang Y, Smith M, Earl M, Norigian Z, McBride A. A review in the treatment of oncologic emergencies. J Oncol Pharm Pract. 2016;22:625–38. doi: 10.1177/1078155215605661. [DOI] [PubMed] [Google Scholar]
- 7.Nirenberg A, Mulhearn L, Lin S, Larson E. Emergency department waiting times for patients with cancer with febrile neutropenia: A pilot study. Oncol Nurs Forum. 2004;31:711–5. doi: 10.1188/04.ONF.711-715. [DOI] [PubMed] [Google Scholar]
- 8.Earle CC, Park ER, Lai B, Weeks JC, Ayanian JZ, Block S. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol. 2003;21:1133–8. doi: 10.1200/JCO.2003.03.059. [DOI] [PubMed] [Google Scholar]
- 9.Barbera L, Paszat L, Chartier C. Indicators of poor quality end-of-life cancer care in Ontario. J Palliat Care. 2006;22:12–7. [PubMed] [Google Scholar]
- 10.Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30:253–6. doi: 10.1177/1049909112447285. [DOI] [PubMed] [Google Scholar]
- 11.Tapela NM, Mpunga T, Karema N, Nzayisenga I, Fadelu T, Uwizeye FR, et al. Implementation science for global oncology: The imperative to evaluate the safety and efficacy of cancer care delivery. J Clin Oncol. 2016;34:43–52. doi: 10.1200/JCO.2015.61.7738. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Emergency Medicine. American Academy of Emergency Medicine. [Last cited on 2016 Sep 13]. Available from: http://www.aaem.org/em-resources/position-statements/workforce/physician-to-patient .
- 13.Wong HJ, Morra D, Caesar M, Carter MW, Abrams H. Understanding hospital and emergency department congestion: An examination of inpatient admission trends and bed resources. CJEM. 2010;12:18–26. doi: 10.1017/s1481803500011970. [DOI] [PubMed] [Google Scholar]
- 14.Mayer DK, Travers D, Wyss A, Leak A, Waller A. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina? J Clin Oncol. 2011;29:2683–8. doi: 10.1200/JCO.2010.34.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun BC, Hsia RY, Weiss RE, Zingmond D, Liang LJ, Han W, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61:605–11.e6. doi: 10.1016/j.annemergmed.2012.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goh SL. Emergency department overcrowding and mortality after the introduction of the 4-hour rule in Western Australia. Med J Aust. 2012;197:148. doi: 10.5694/mja12.10828. [DOI] [PubMed] [Google Scholar]


