Abstract
Aim:
The aim of this study is to evaluate the prevalence of nasal carriage of coagulase positive methicillin-resistant Staphylococcus aureus (MRSA) among dental students.
Materials and Methods:
Four hundred dental students, divided into two groups – undergraduates (200) and postgraduates (200), were screened using sterile cotton swabs for carriage of MRSA in anterior nares. The samples were inoculated on HiCrome MeReSa Agar Base-with cefoxitin supplement. Further confirmatory tests were done by Gram-staining, Tube coagulase and Cefoxitin disc diffusion test on Mueller–Hinton agar.
Results:
MRSA was positive among 25 (12.50%) undergraduates and 49 (24.50%) postgraduates students. Further confirmatory test also showed the same results. MRSA colonization was significantly more in postgraduate students, who are exposed to more number of patients and have put in more clinical hours as compared to undergraduate students who have just entered clinics and have limited clinical exposure.
Conclusion:
The present study concluded that rate of MRSA colonization was 18.5% in the dental school population. The colonization rate was significantly (P = 0.002%) higher in postgraduate students as compared to undergraduate students emphasizing the need to follow infection control protocols stringently.
Clinical Significance:
Awareness about MRSA among dental doctors is mandatory so as to prevent transmission of MRSA in dental settings.
Keywords: Dental infection control, dental students, methicillin-resistant Staphylococcus aureus, nasal colonization
INTRODUCTION
Staphylococcus aureus is an important bacterial pathogen causing a wide variety of infections ranging from mild local infections of the skin and soft tissue to severe systemic infections such as sepsis and toxic shock syndrome, which may be lethal. Typically, this bacterium lives as a commensal in the nose and/or throat of 20% to 70% of adults. Methicillin-resistant S. aureus (MRSA) which are generally resistant to multiple antibiotics have emerged among people in hospitals, nursing homes and other health-care institutions since the 1960s and are called hospital- or health care-associated MRSA (HA-MRSA). They account for a large part of nosocomial infections worldwide and are associated with longer hospitalization and higher lethality.
In the community setting, several outbreaks of severe infections with MRSA have been reported among people lacking established risk factors for HA-MRSA acquisition. The bacteria are referred to as community-associated MRSA (CA-MRSA) and differ from HA-MRSA in several important aspects. First reported in the 1980s, these CA-MRSA infections seem to have increased in prevalence, affecting children and adult population. CA-MRSA caused predominantly skin and soft-tissue infections but was also associated with severe pulmonary infections including fatal necrotizing pneumonia and empyema.[1]
Staphylococcal infections cause significant morbidity and mortality in both the community and hospital settings. Treatment of infection caused by S. aureus has become more problematic since the development of antimicrobial-resistant S. aureus (MRSA). Since MRSA strain is resistant to all β-lactam antibiotics and the treatment options are limited significantly. The incidence of nosocomial infection caused by MRSA continues to increase worldwide. Infections caused by MRSA strains are associated with longer hospital stay, prolonged antibiotic administration and higher costs than infections caused by methicillin-susceptible S. aureus strains. The presence of S. aureus in the anterior nares of patients may serve as a source of infection to other patients is known to be a significant risk factor. Within the hospital colonized health-care workers act as reservoir for the spread of MRSA.[2]
MRSA is transmitted to nares by contaminated hands and from surfaces where it can survive for months. Nasal carriage of S. aureus acts as endogenous reservoir for clinical infections in the colonized individual but also as a source of cross-colonization for community spread.[3] Hence, the source of MRSA infection in dentistry could be infected or colonized patients, infected or colonized doctors and environmental surfaces such as emergency treatment area, air-and-water syringes, dental chair seat armrest, dental chair push buttons, light handles.[4] Microbial aerosols and splatter containing microbes from oral cavity contaminate the environmental surfaces. MRSA colonization is a risk factor for the development and transmission of MRSA infections in both health care and community settings.[5]
This study was therefore aimed at establishing the carriage rate of MRSA among dental students as they could pose a potential risk factor for nosocomial transmission, and the outcome may be useful for formulating an MRSA infection control protocol in dental hospitals.
MATERIALS AND METHODS
This study was designed to investigate the nasal carriage rate of coagulase positive MRSA among dental students in dental colleges and hospitals of Bengaluru. Anterior nasal cultures were collected from 400 dental student volunteers (200 postgraduates and 200 undergraduates) after obtaining informed consent.
Sample collection
Sterile disposable culture swab moistened with saline was used for sample collection. Each swab was rotated against the inside of each nostril for 3 times with slight finger pressure on the outside of the nose to assure good contact between the swab and the inside of the nose. Using the same swab, procedure was carefully repeated for the second nostril without contaminating the swab. Samples were carried in transport media and inoculated within 4 h of collection.
Sample processing
MRSA screening using chrome agar method: the swabs were inoculated onto HiChrome MeReSa Agar, Base-with cefoxitin supplement (HiChrome MRSA Agar Base: MRSA Chromogenic Agar from HiMedia Laboratory Pvt. Ltd, Mumbai, India) to screen MRSA. The test was performed as per the manufacturer. After incubation at 37°C for 48 h, samples showing the presence of bluish-green colored colonies were reported as MRSA positive [Figure 1].
Figure 1.
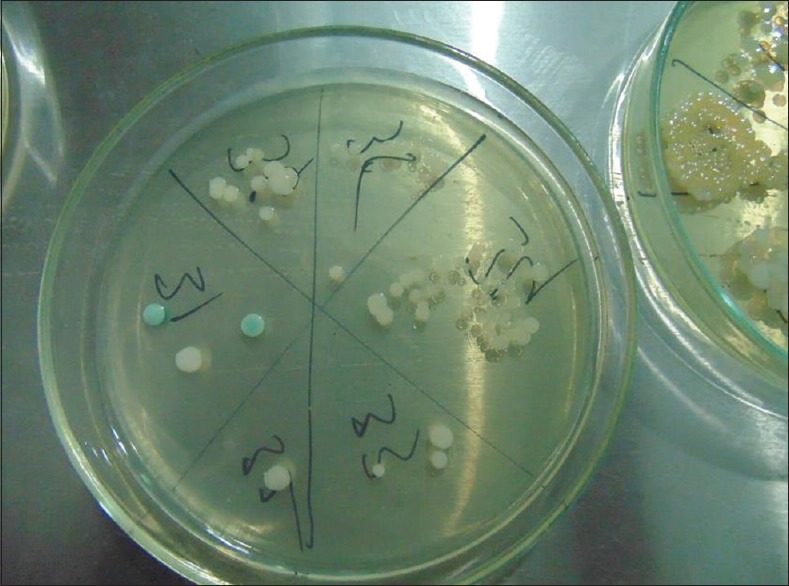
Colonies of methicillin-resistant Staphylococcus aureus (blue-green colonies) on HiChrome MeReSAgar, Base-with cefoxitin supplement
Further testing of positive samples was done by Gram staining, tube coagulase and cefoxitin disc diffusion test on Mueller–Hinton agar, to confirm MRSA-positive cases [Figures 2–4].
Figure 2.

Gram-staining
Figure 4.
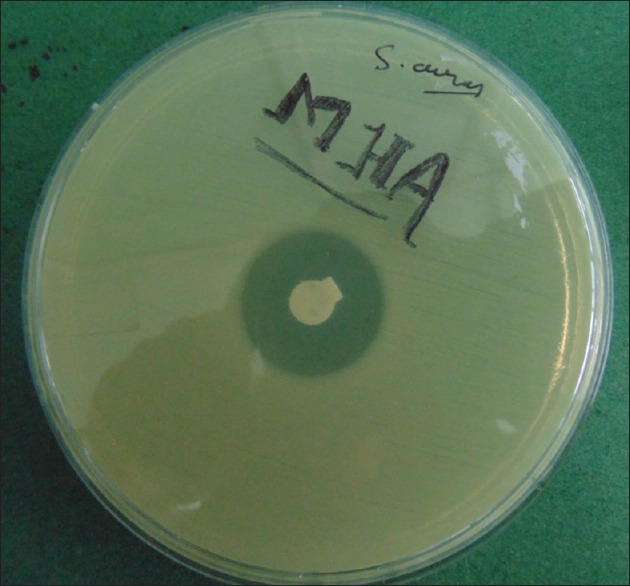
Inhibition zone on Cefoxitin disc diffusion test on Mueller–Hinton agar
Figure 3.
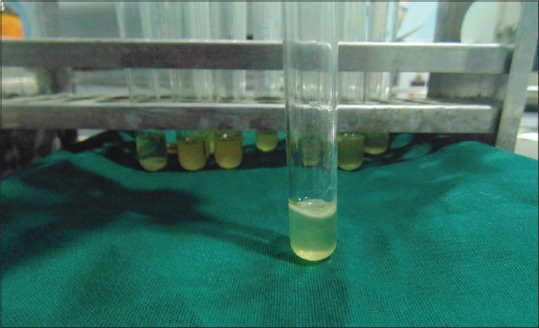
Coagulation in Tube coagulase test
RESULTS
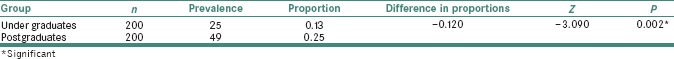
Out of the 400 specimens, 74 (18%) students were positive for coagulase positive MRSA (CoPS MRSA). Out of 74 positive isolates, 49 (66.3%) were postgraduate and 25 (33.6%) were undergraduates students. The data were subjected to statistical analysis using Z-test for the difference in two proportions. Nasal carriage for coagulase positive MRSA among the postgraduate students was found to be significantly higher (P = 0.002) than the undergraduate students [Graph 1 and Table 1].
Graph 1.
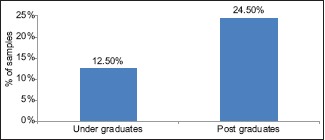
Nasal colonization of methicillin-resistant Staphylococcus aureus in undergraduates and postgraduates
Table 1.
Comparison of the prevalence of methicillin-resistant Staphylococcus aureus between the two groups (z-test for proportions)
DISCUSSION
MRSA infections account for a large part of nosocomial infections worldwide and add to the total economic burden as they are associated with high treatment cost, longer hospitalizations and limited treatment options due to multiple drug resistance.[6,7]
The Centers for Disease Control – National Nasocomial Infection Surveillance system reported that methicillin resistance among S. aureus in US hospitals increased from 2.4% in 1975 to 29% in 1991, with a higher degree of resistance in intensive care units. More recent data from 1990 through 1997 identified that the MRSA incidence rate increased 260% in hospitals.[8]
In dental health-care setting, MRSA can be transmitted from patients to doctors, patients to patients and from doctors to patients.[9]
The source of MRSA infection in dentistry could be infected or colonized patients, infected or colonized doctors and environmental surfaces such as emergency treatment area, air-and-water syringes, dental chair seat armrest, dental chair push buttons and light handles.[10] Microbial aerosols and splatter containing microbes from oral cavity contaminate the environmental surfaces. S. aureus may colonize any part of the body, including the throat, groin, armpits and perineum, anterior nares has the highest sensitivity of any single site for determining MRSA colonization, and that the greater the numbers of MRSA isolated from the nose, the higher the chance of finding colonization at other body sites as well. It has the ability to survive for up to 12 days on abiotic surfaces.[11] Risk of MRSA infection transmission is not just limited to the medical hospitals; rather it is a serious public health problem.[12]
In this study, the prevalence of MRSA nasal carriage among dental students in Bengaluru city was found to be 18.5% out of which 24.5% were postgraduate students.[13]
Goud et al. studied Community prevalence of MRSA in and around Bengaluru and found MRSA nasal carriage rate of 9.9% among individuals between 20 and 40 years of age and 22% among doctors which is similar to our study.[14]
Robert et al. who found 21% nasal carriage rate of MRSA among dental students with greater prevalence in the final year students as compared to 1st years.[13]
The prevalence of MRSA nasal carriage in health-care workers (HCWs), in USA[14] (2008) was around 12%, whereas in India, according to a study by Malini et al. it is 8%, among HCWs in a hospital in Bengaluru.[15]
MRSA cannot be eradicated; it can only be prevented. Various preventive measures carriers to prevent transmission of drug-resistant strains of Staphylococci from the community to the hospital settings and hospital settings to community include following standard infection control precautions strictly, stopping antibiotic abuse, using decolonizing agents such as mupirocin and most importantly Screening high-risk patients to identify asymptomatic carriers and placing them under contact precautions should be mandatory, as in some countries.
CONCLUSION
Risk of MRSA infection transmission is not just limited to the medical hospitals; rather it is a serious public health problem.
MRSA infection transmission is a serious public dental health issue and a cause for concern among dental health-care professionals and a cause for concern among dental health-care professionals and patients. The present study provides an epidemiological data so as to guide preventive measures to stop transmission of MRSA infection in dental setup. According to the results of this study, MRSA nasal carriage rate among dental students in Bengaluru city is 18.5%. This advocates the need of greater awareness about MRSA among dental doctors. The rate of colonization was found to be significantly (P = 0.002) more in postgraduate students (66.3%) as compared to undergraduate students (33.66%) emphasizing the need to follow infection control protocols stringently.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zimmerli M, Widmer AF, Dangel M, Filippi A, Frei R, Meyer J, et al. Methicillin-resistant Staphylococcus aureus (MRSA) among dental patients: A problem for infection control in dentistry? Clin Oral Investig. 2009;13:369–73. doi: 10.1007/s00784-008-0244-2. [DOI] [PubMed] [Google Scholar]
- 2.Kumar P, Shukla I, Varshney S. Nasal screening of healthcare workers for nasal carriage of coagulase positive MRSA and prevalence of nasal colonization with Staphylococcus aureus. Biol Med. 2011;3:182–6. [Google Scholar]
- 3.Pathak A, Marothi Y, Iyer RV, Singh B, Sharma M, Eriksson B, et al. Nasal carriage and antimicrobial susceptibility of Staphylococcus aureus in healthy preschool children in Ujjain, India. BMC Pediatr. 2010;10:100. doi: 10.1186/1471-2431-10-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurita H, Kurashina K, Honda T. Nosocomial transmission of methicillin-resistant Staphylococcus aureus via the surfaces of the dental operatory. Br Dent J. 2006;201:297–300. doi: 10.1038/sj.bdj.4813974. [DOI] [PubMed] [Google Scholar]
- 5.Smith AJ, Jackson MS, Bagg J. The ecology of staphylococcus species in the oral cavity. J Med Microbiol. 2001;50:940–6. doi: 10.1099/0022-1317-50-11-940. [DOI] [PubMed] [Google Scholar]
- 6.National Nosocomial Infections Surveillance System. National nosocomial infections surveillance (NNIS) system report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32:470–85. doi: 10.1016/S0196655304005425. [DOI] [PubMed] [Google Scholar]
- 7.Graffunder EM, Venezia RA. Risk factors associated with nosocomial methicillin-resistant Staphylococcus aureus (MRSA) infection including previous use of antimicrobials. J Antimicrob Chemother. 2002;49:999–1005. doi: 10.1093/jac/dkf009. [DOI] [PubMed] [Google Scholar]
- 8.Staat RH, Van Stewart A, Stewart JF. MRSA: An important consideration for geriatric dentistry practitioners. Spec Care Dentist. 1991;11:197–9. doi: 10.1111/j.1754-4505.1991.tb01730.x. [DOI] [PubMed] [Google Scholar]
- 9.Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: Epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev. 1997;10:505–20. doi: 10.1128/cmr.10.3.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang R, Mehta S, Weed D, Price CS. Methicillin-resistant Staphylococcus aureus survival on hospital fomites. Infect Control Hosp Epidemiol. 2006;27:1267–9. doi: 10.1086/507965. [DOI] [PubMed] [Google Scholar]
- 11.Petti S, Polimeni A. Risk of methicillin-resistant Staphylococcus aureus transmission in the dental healthcare setting: A narrative review. Infect Control Hosp Epidemiol. 2011;32:1109–15. doi: 10.1086/662184. [DOI] [PubMed] [Google Scholar]
- 12.Goud R, Gupta S, Neogi U, Agarwal D, Naidu K, Chalannavar R, et al. Community prevalence of methicillin and vancomycin resistant Staphylococcus aureus in and around Bangalore, Southern India. Rev Soc Bras Med Trop. 2011;44:309–12. doi: 10.1590/s0037-86822011005000035. [DOI] [PubMed] [Google Scholar]
- 13.Roberts MC, Soge OO, Horst JA, Ly KA, Milgrom P. Methicillin-resistant Staphylococcus aureus from dental school clinic surfaces and students. Am J Infect Control. 2011;39:628–32. doi: 10.1016/j.ajic.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 14.Ibarra M, Flatt T, Van Maele D, Ahmed A, Fergie J, Purcell K, et al. Prevalence of methicillin-resistant Staphylococcus aureus nasal carriage in healthcare workers. Pediatr Infect Dis J. 2008;27:1109–11. doi: 10.1097/inf.0b013e31817eeefa. [DOI] [PubMed] [Google Scholar]
- 15.Malini J, Shruti A, Harle Padmavathy M, Umapathy BL, Navaneeth BV, Keerthi Mannan J, et al. Methecillin-resistant Staphylococcus aureus carriage among the health Care workers in a tertiary care hospital. J Clin Diagn Res. 2012;6:791–3. [Google Scholar]


