Abstract
We previously demonstrated that small-particle (0.5–3.0 µm) aerosol infection of rhesus monkeys (Macaca mulatta) with cowpox virus (CPXV)-Brighton Red (BR) results in fulminant respiratory tract disease characterized by severe lung parenchymal pathology but only limited systemic virus dissemination and limited classic epidermal pox-like lesion development (Johnson et al., 2015). Based on these results, and to further develop CPXV as an improved model of human smallpox, we evaluated a novel large-particle aerosol (7.0–9.0 µm) exposure of rhesus monkeys to CPXV-BR and monitored for respiratory tract disease by serial computed tomography (CT). As expected, the upper respiratory tract and large airways were the major sites of virus-induced pathology following large-particle aerosol exposure. Large-particle aerosol CPXV exposure of rhesus macaques resulted in severe upper airway and large airway pathology with limited systemic dissemination.
Keywords: orthopoxvirus, smallpox, variola virus, nonhuman primate model, aerosol, large-particle aerosol
Introduction
Variola virus (VARV) and its close relative monkeypox virus (MPXV) are considered potential bioterrorism weapons that require biosafety level 4 (VARV) and biosafety level 3 (MPXV) laboratories for study. Direct experimentation with VARV requires World Health Organization approval and can only be conducted in one laboratory in the USA and one laboratory in Russia. These restrictions limit widespread study of their pathogenesis and medical countermeasure development. The future of VARV research is also in question, as debates concerning the destruction of the known VARV stocks continue (Damon et al., 2014; Jahrling & Tomori, 2014; Tucker, 2011). Hence, there is a need to develop safe, accessible, alternative models of human orthopoxvirus infection that meet the United States’ Food and Drug Administration (FDA) ‘Animal Rule’ requirements (Aebersold, 2012). Cowpox virus (CPXV) may provide such an alternative model (Parker et al., 2007a, b; Vorou et al., 2008). CPXV does not require Select Agent permits, as it is a biosafety level (BSL)-2 pathogen, and mouse models are available for further experimentation (Bray & Buller, 2004; Kramski et al., 2010). A naturally occurring infection of CPXV in common marmosets (Callithrix jacchus) at an animal holding facility and subsequent experiments revealed that CPXV infection of non-human primates (NHPs) may provide a suitable orthopoxvirus model (Kramski et al., 2010; Mätz-Rensing et al., 2006).
Previously, we have demonstrated that: (1) intravenous (IV) exposure to CPXV-Brighton Red (BR) in cynomolgus monkeys (Macaca fascicularis) results in a lethal, human haemorrhagic smallpox-like disease (Dixon, 1962; Downie et al., 1969; Fenner, 1988; Johnson et al., 2011b); (2) intrabronchial exposure to CPXV in cynomolgus monkeys results in systemic disease (Smith et al., 2012); and (3) small-particle aerosol exposure of CPXV in rhesus monkeys resulted in a severe, lethal respiratory disease (Johnson et al., 2015). Our work, along with similar work for MPXV, VARV and vaccinia virus (Barnewall et al., 2012; Goff et al., 2011; Hahon, 1961; Johnson et al., 2011a; Nalca et al., 2010; Zaucha et al., 2001) has demonstrated that the viral deposition site is critical to orthopoxviral pathogenesis.
As reviewed in Milton (2012), the natural route of transmission of VARV remains speculation and no previous studies that we are aware of attempted to demonstrate the impact of aerosol particle size on disease progression. However, experiments by Hahon and Wilson with an aerosol particle of <5 µm produced disseminated, moderate disease in macaques (Hahon, 1961). Experiments by Jahrling et al. suggested that lethal disease would develop when small-particle aerosols (1–3 µm) were combined with IV exposure or after IV exposure alone (Jahrling et al., 2004). Speculation about the natural route of VARV transmission in humans suggests that shedding of scabs was not associated with sustained person-to-person transmission (Mitra et al., 1974; Rao et al., 1968), and that respiratory infection is more likely to lead to severe disease (Fenner et al., 1988). The Meschede Germany outbreak of 1970 provided epidemiological evidence of aerosol transmission from the index patient to afflicted individuals in the absence of direct contact (Fenner et al., 1988; Wehrle et al., 1970). Furthermore, Dixon hypothesized that VARV initially establishes infection in macrophages in the upper respiratory tract (Dixon, 1962). After infection, these macrophages disseminate to the peripheral lymphoid organs, establishing smallpox infection in the exposed individual (Fenner, 1980). Based on Dixon’s hypothesis and that small-particle exposure of VARV alone was not sufficient to induce severe or lethal disease in macaques we hypothesized that large-particle aerosol exposure of CPXV-BR would seed the upper respiratory tract resulting in a disease that more accurately mimics human smallpox. To support our hypothesis, Hinds (1999) demonstrated that aerosol-droplet particle size will determine its deposition site. Therefore, changing the particle size of an aerosol-carrying virus will likely alter its deposition site, thus potentially changing disease presentation, progression and outcome.
Results
Experimental design
Four groups of four rhesus monkeys (n=16) were exposed to serial tenfold reductions from 5×107 p.f.u. to 5×104 p.f.u. of CPXV-BR by large-particle aerosol exposure. Large-particle aerosols were generated as described in Bohannon et al. (2015). Aerosol parameters by subject and outcome are shown in Table S1 (available in the online Supplementary Material). Pre- and post-exposure physical exams, computed tomography (CT), and sample collection was performed on study days −10, 3, 6, 9, 12, 15, 18 and 21, and on the day of necropsy. Subjects were considered survivors past day 21. Necropsies were performed between days 22 and 28.
Large-particle CPXV exposure results in a lethal respiratory disease
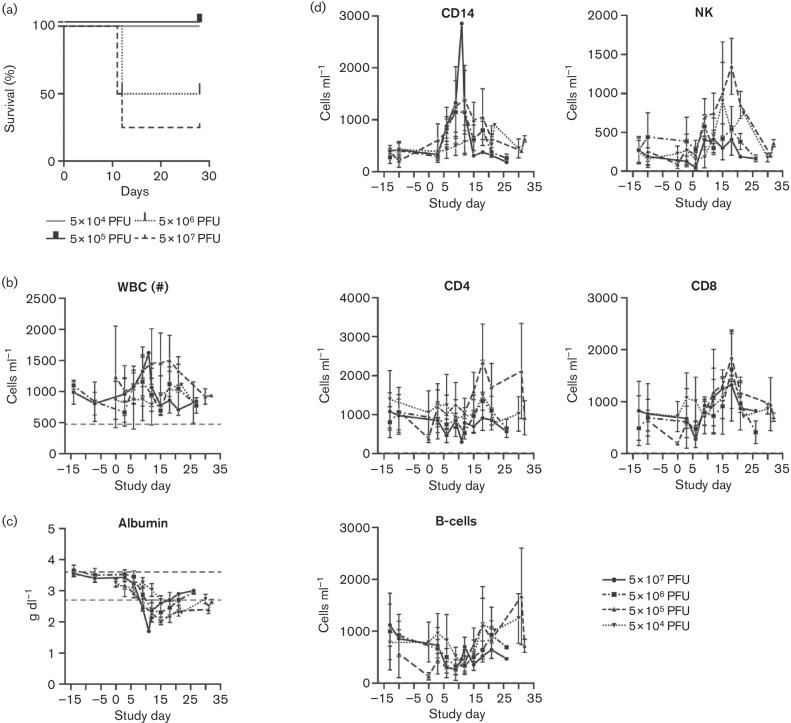
Three of four subjects receiving 5×107 p.f.u. met study endpoint criteria between days 11 and 12 post-exposure. Fifty percent of the monkeys receiving 5×106 p.f.u. met study endpoint criteria on day 12 post-exposure while the remaining survived to study end (day 21 post-exposure) (Fig. 1a). Subjects receiving 5×105 and 5×104 p.f.u. survived to study end but did experience disease. The subjects that succumbed demonstrated laboured breathing and slightly decreased peripheral oxygen saturation (Table S2). Respiratory rate peaks coincided with endpoint criteria for two of the five subjects. The lowest observed peripheral oxygenation coincided with endpoint criteria for one of those five monkeys. Laboured breathing, increased respiratory rate and decreased peripheral oxygen saturation are consistent with the histopathologic findings of severe respiratory tract disease.
Fig. 1.
(a) Kaplan–Meier analysis of the large-particle aerosol exposure of rhesus monkeys. Three out of four (75 %) NHPs receiving 5×107 p.f.u. of CPXV succumbed by day 12 post-exposure, and 50 % of NHPs receiving 5×106 p.f.u. of CPXV succumbed by day 12 post-exposure. Groups receiving 5×105 and 5×104 p.f.u. survived to study end. (b) WBC concentrations during the course of the experiment. Dashed lines indicate normal value ranges. Subjects did not consistently demonstrate leucocytosis. (c) Serum chemistry value of albumin indicates a decrease across all groups, suggesting a response to exposure. (d) The major PBMC populations increased in response to infection. Various PBMC cell populations were assayed periodically by TruCount analysis as described in the Methods.
The hallmark epithelial smallpox lesions were not a common observation in large-particle aerosol CPXV exposed monkeys (Table S2) and were only observed in the lowest doses (5×105 and 5×104) groups. The subjects in the 5×105 p.f.u. group developed few lesions (2–31 at peak of lesions), distributed on the head and limbs, that were first observed at a mean of 8.25 days post-exposure (range: 6–12 days). Other clinical signs included: serous nasal discharge, tussis, inappetence and dyspnea. Clinically, white blood cell (WBC) count increases and albumin decreases were observed and were consistent with disease progression (Fig. 1b, c). PBMCs were analysed by TruCount to evaluate concentrations of circulating leucocytes and were consistent with the total WBC. The 5×104 p.f.u. group demonstrated a lag in expansion of monocytes, NK cells and B-cells when compared to the other groups (Fig. 1d).
In keeping with our previous CPXV experiments, pro-inflammatory cytokines/chemokines were evaluated for changes associated with disease progression and are summarized in Table S3. Vascular endothelial growth factor (VEGF) and sCD40L demonstrated less than twofold changes from baseline for any subject in any group and were excluded from further analysis. Granulocyte-colony stimulating factor (G-CSF) changes were greatest in the 5×107 p.f.u. group with little change observed in the other groups. IFN-γ demonstrated greater than twofold elevations for each group with the peaks occurring between days 6 and 9 for the 5×105 to 5×107 groups. The 5×104 p.f.u. group had a peak of IFN-γ concentration which was consistent with changes in the PBMC population for this group. IL-6 increases were associated with early time points and did not parse with survival within the 5×106 p.f.u. group. IL-12 demonstrated peak mean fold concentration changes that were reciprocal to virus dose.
Gross pathology and histopathology indicate severe upper respiratory tract pathology
Full necropsies were performed on all subjects. Two subjects (nos 13 and 16) from the 5×107 p.f.u. group that met endpoint criteria first (day 11 post-exposure) exhibited subacute, severe, necroulcerative pharyngitis and tracheitis (Fig. 2a) and fibrinosuppurative bronchopneumonia (Fig. 2b). This pneumonia was consolidating in the right middle, caudal part of the left cranial and accessory lung lobes. The remaining subjects that succumbed to CPXV, two from the 5×106 p.f.u. group (subjects 9 and 11) and one from the 5×107p.f.u. dose group (subject 15), exhibited severe, diffuse, necrosuppurative and ulcerative pharyngitis, tracheitis (Fig. 2a), and bronchitis. However, the pulmonary parenchyma from these three subjects exhibited few signs of severe disease. In the two 5×106 p.f.u. dose survivors (subjects 10 and 12), a mild, chronic, multifocal, organizing lymphoplasmacytic bronchopneumonia (Fig. 2c) was seen in alveoli but limited to the alveoli immediately adjacent to the tertiary bronchioles. Two non-survivors, one from the 5×107 p.f.u. dose group (subject 15) and one from the 5×106 p.f.u. dose group (subject 9), also exhibited a severe, necrosuppurative and ulcerative epiglottitis (Fig. 2d). No evidence of pneumonia was seen in the survivor from the 5×107 p.f.u. dose group (subject 14). Histopathologically, the upper airways and bronchi in the three survivors from the higher dose groups exhibited mild chronic, lymphoplasmacytic infiltrates. Together, these data suggest that the upper respiratory tract and major airways were the focal point of disease with only limited dissemination into the alveoli.
Fig. 2.
Histopathology of CPXV large-particle aerosol-exposed NHPs. (a) Histological evaluation of the upper respiratory tract. Cross-sections of the trachea are shown and demonstrate the severe inflammatory response of the non-survivors when compared to the survivors. Placement of the endotracheal (ET) tube displaced significant intraluminal exudates from subjects 13, 15, 9 and 11 (an ET tube was not placed in subject 16 prior to necropsy). Bars, 1 mm. (b) Severe, consolidating fibrinosuppurative and necrotizing bronchopneumonia for subject 13. Inset: Ulcerated bronchus (note supporting hyaline cartilage at left) with smooth muscle. The bronchial lumen is filled with a necrotic fibrinosuppurative exudate. Bars (including inset), 100 µm. (c) Right caudal lung lobe. The bronchus and surrounding pulmonary parenchyma exhibit mild, locally extensive, peribronchial and peribronchiolar organizing pneumonia. Inset: Focal bronchiolization and squamous metaplasia of affected alveoli. Bars (including inset), 100 µm. (d) Non-survivor epiglottis demonstrating severe necrosuppurative and ulcerative epiglottitis observed in subject 15. The junction of intact epithelium exhibited hydropic degeneration and necrotic epithelium with myriad, intracytoplasmic, intraepithelial inclusion bodies (black arrow). Inset: subgross cross-section of the epiglottis. Bars, 10 µm and 1 mm (inset). (e) Epiglottis from surviving subject (subject 10) which appears normal. Inset: subgross cross-section of the epiglottis. Bars, 100 µm and 1 mm (inset).
Immunohistochemistry and immunofluorescence indicate infection of macrophages and epithelial cells
We evaluated the location of CPXV antigen (Fig. 3a–d) and the cell type infected (Fig. 3e, f) in both the lungs and trachea. As described above, sections of trachea exhibited severe inflammation and necrosis of the lining epithlium, and similar inflammation was present in the underlying submucosal stroma and within submucosal glands (Fig. 3a). Immunohistochemical evaluation of the similar regions showed abundant CPXV antigen staining in these aforementioned regions (Fig. 3b). Similarly, the lung exhibited regions of severe inflammation, fibrin and necrosis (Fig. 3c), which, immunohistochemically, were also consistent with areas of abundant virus antigen staining (Fig. 3d). Furthermore, in both the lung and trachea, virus-antigen-positive cells were morphologically suggestive of macrophage lineage and in order to confirm this, we evaluated the previously described sections with immunofluorescence to determine the identity of the infected cells (Fig. 3e, f). Using a pan-macrophage marker (IBA1) and a CPXV antibody, we found that in both the lungs and the trachea, cells positive for both IBA1 (macrophages) and CPXV antigen co-localized in the previously described regions of severe inflammation and virus antigen deposition (Fig. 3e-iv, f-iv) f-vi. These data suggest that within the areas of severe inflammation and necrosis (trachea and lung), macrophages were the cells targeted for virus infection.
Fig. 3.
(a) Haematoxylin and eosin (H&E)-stained sections of trachea show severe inflammation and necrosis involving the mucosal epithelial cells and the submucosal glands. (b) Immunohistochemistry for CPXV virus shows abundant virus antigen staining (brown) in both attached and free (necrotic) mucosal epithelial cells, and within the subjacent submucosal glands (inset). (c) H&E-stained sections of lung show severe inflammation and necrosis involving bronchioles and the surrounding alveolar interstitium. Alveolar spaces are filled with fibrin, inflammatory cells and karyorrhectic cellular debris (inset). (d) Immunohistochemistry for CPXV shows abundant virus antigen labelling (brown) within sloughed epithelial cells and within the cytoplasm of cells (macrophages) associated with damaged and necrotic alveolar walls. Magnification (a–d), main image ×4; inset ×40. Bars (a–d), 100 µm. (e) Histopathology of CPXV lung infection (i), characterized by severe and necrotizing brochiolitis and alveolitis. Alveolar spaces are filled with fibrin, cellular debris and macrophages. Bright-field immunohistochemistry (BF-IHC) (ii) shows CPXV-antigen-positive cells clustered within alveolar spaces; cells are were often large, round to polygonal with abundant virus-positive cytoplasm. Immunofluorescence images (iii–vi) show the same location with IBA1 (iii; pan-macrophage), CPXV (iv; virus antigen) and DAPI (v; nuclear) immunohistochemical markers, and a merged image (vi) demonstrating CPXV-antigen-positive macrophages (yellow) associated with regions of severe lung damage. (f) Histopathology of CPXV infection of the trachea (i), characterized by severe necrotizing tracheitis and massive cellular infiltration of the submucosal stroma. Bright-field immunohistochemistry (ii) shows CPXV antigen within mucosal epithelial cells; inflammatory cells within the subjacent stroma frequently display cytoplasmic positivity. Immunofluorescence images (iii–vi) show the same location with IBA1 (iii; pan-macrophage), CPXV (iv; virus antigen) and DAPI (v; nuclear) immunohistochemical markers, and a merged image (vi) demonstrating CPXV-antigen-positive macrophages (yellow) associated with regions of severe tracheal damage. Bars (e, f), 100 µm.
CT indicates moderate lung pathology
We evaluated real-time progression of lung disease by CT in all four groups of animals to determine if there was agreement to other parameters and our previous experiments (Fig. 4). CT scans were performed pre-exposure for baseline evaluation, and then every 3 days until study end (day 21 post-exposure) wherein a final necropsy day CT was performed (days 22–28 post-exposure). Day 3 scans performed on two animals from the high dose group had to be excluded due to poor positioning of the endotracheal tube (ET) and concomitant poor aeration of one lung and hyperinflation of the contralateral lung. There were no significant changes noted on day 3 scans in the other two animals from the same group.
Fig. 4.
CT indicates lung pathology and resolution. The selected images are representative of non-survivors or survivors from the two groups in which NHPs met endpoint criteria. The data shown demonstrates the CT image at the observed peak lung pathology for that subject: day 11 for panel (a), day 12 for panel (b), day 12 for panel (c), and day 12 for panel (d). Corresponding CT images from previous or subsequent days were selected for comparison of disease progression and regression within the same anatomical location. Subjects that succumbed or met endpoint criteria demonstrated similar CT findings (a–c). Subjects that survived demonstrated pathology followed by resolution (d). (a) Subject 16, 5×107 p.f.u. group, succumbed at day 11. (b) Subject 15, 5×107 p.f.u. group, euthanized on day 12. (c) Subject 9, 5×106 p.f.u. group, euthanized on day 12. (d) Subject 10, 5×106 p.f.u. group, survivor.
Qualitatively, subjects from the 5×107 and 5×106 p.f.u. groups started demonstrating CT abnormalities by day 6 and day 9 post-exposure, respectively. For the 5×105 and 5×104 p.f.u. groups, minimal changes were first noticed on days 12 and 15, respectively. As expected, the severity of lung disease was generally proportional to the dose, with the 5×107 p.f.u. and 5×106 p.f.u. groups showing the most significant changes. Those changes were most severe on day 12 post-exposure in seven out of eight animals (one animal from the 5×107 p.f.u. group met endpoint criteria prior to day 12) and included bronchial wall thickening, peribronchovascular infiltrates, patchy ground glass opacities as well as lobar and semilobar lung consolidations in two subjects. Interestingly, on day 12, only one out of three subjects from the 5×107 p.f.u. group developed more severe respiratory disease than the four subjects in the 5×106 p.f.u. group, suggesting a comparable disease burden between these two dose groups (Fig. 4). Changes in the lower dose groups (5×104 and 5×105 p.f.u.) were less marked and included peribronchial thickening/infiltrates, patchy ground glass opacities, with only one monkey (5×105 p.f.u. group) showing consolidative changes in the lower lung fields (data not shown).
For the surviving subjects (one from the 5×107 p.f.u. group, two from the 5×106 p.f.u. group, and all monkeys from the lower dose groups), some lesions did not completely resolve by study end and were evident on CT and histopathologically.
CT abnormalities were quantified by percentage change in lung hyperdensity (PCLH) (Fig. 5). Two of four animals from the 5×107 group had slight increases in PCLH observed at day 6 post-exposure and all four developed changes by day 9. The single survivor in this group demonstrated peak PCLH changes on day 12, which started decreasing on day 15 and almost completely resolved by day 27 (necropsy) (Fig. 2a). Subjects in the 5×106 group demonstrated peak PCLH changes on days 11–12 that subsequently continued to resolve until study end (day 26 necropsy) (Fig. 4d). The 5×105 group demonstrated peak changes in PCLH on day 12 post-exposure that quickly began to resolve and returned to near baseline values by day 21. Only one subject from the 5×104 group demonstrated increased PCLH values that occurred on day 15 and resolved by necropsy on day 28.
Fig. 5.
Quantitative analysis of the CT data indicates progressive and resolving lung pathology that corresponds to dose. CT data was analysed as described in Methods. Individual subjects are shown by group. (a) 5×107 p.f.u., (b) 5×106 p.f.u., (c) 5×105 p.f.u., (d) 5×104 p.f.u. Asterisk indicates that the day 3 data points were dropped due to incorrect placement of the ET tube.
Peripheral oxygen saturation correlated with increased PCLH for the 5×107 (r=−0.8336, R2=0.6949, P=0.0198) and 5×106 (r=0.7848, R2=0.6159, P=0.0122) p.f.u. groups, but no correlation could be found for the lower dose groups. Respiratory rate correlated with PCLH for the 5×107 p.f.u. group only (r=0.9472, R2=0.8970, P=0.0004). Circulating monocyte numbers positively correlated with PCLH for the 5×107 (r=0.9580, R2=0.9178, P<0.0001) and 5×105 (r=0.7121, R2=0.5071, P=0.0209) groups.
Virology supports viraemia and limited dissemination
Quantitative PCR (qPCR) was used to determine viral genomic load in peripheral blood and swabs (nasal and oral, Table S4). Using a Tukey’s multiple comparisons test from Graphpad Prism 6.0, comparison of peak viral load in the nasal swabs indicated statistically significant (P<0.05) differences were observed between the 5×106 and 5×105 groups and the 5×106 and 5×104 groups. Due to wide variation in the 5×107 p.f.u. group, no statistically significant difference was observed. A similar comparison for the oral swabs indicated no statistically significant differences between the groups. Viral genomic DNA could not be detected in peripheral blood from subjects in the 5×104 and 5×105 p.f.u. groups. Viraemia could be detected by day 9 in three of five non-survivors from the higher dose groups which was consistent with the gross and histopathology data. Viraemia was not detected in the single survivor from the 5×107 p.f.u. group, but was detected in the two surviving 5×106 p.f.u. group subjects. We were unable to collect a sample to determine the peak viral load from the subject that succumbed from the 5×107 p.f.u. group. At necropsy of non-survivors, virus was readily detected from the lungs and from the tracheobronchial lymph node, however a wide variation in the titres from each subject resulted in no statistically significant difference between the lethal doses (data not shown). Other evaluated tissues including adrenal gland (n=1; 4500 p.f.u. mg−1), kidney (n=1; 750 p.f.u. mg−1) and heart (n=2; 5600 p.f.u. mg−1) contained infectious virus at concentrations that would be consistent with blood contamination of the tissue. Livers were also evaluated by plaque assay and no infectious virus could be detected.
Discussion
We sought to determine if large-particle aerosol exposure of rhesus macaques with CPXV would provide an improved model of human smallpox. We demonstrated that increasing the aerosol particle size changed the anatomic location of virus deposition from the pulmonary parenchyma to the large conducting airways and, consequently, altered disease presentation. CPXV was chosen because it is a more accessible model of human smallpox than MPXV and VARV, is a BSL-2 pathogen that does not require Select Agent permits, and mouse models are available. Recently, we demonstrated that small-particle aerosol (0.5–3.0 µm) exposure of rhesus monkeys with 5×105 p.f.u. CPXV resulted in a severe, uniformly lethal, respiratory disease characterized by: (1) lung consolidation and pathology; (2) viraemia at endpoint only; (3) decreases in peripheral oxygen saturation; and (4) monocytosis. In this study, we observed: (1) an increased mean day to endpoint criteria (day 9 for small-particle aerosol, day 12 for large-particle); (2) viraemia prior to endpoint; and (3) severe pathology of the upper respiratory tract. A comparison of large-particle CPXV aerosol exposure to small-particle CPXV exposure can be found in Table 1. However, we did not observe uniformly lethal disease at any of the doses evaluated in this experiment. This may be due to the differing microanatomy of the upper respiratory tract where the large-particles deposit when compared with the lower respiratory tract where the small-particles deposit.
Table 1. Comparison of large-particle CPXV exposure to small-particle CPXV exposure.
| Parameter | Large-particle aerosol | Small-particle aerosol |
|---|---|---|
| Dose (p.f.u.) | 5×107 | 5×105 |
| Lethality (%) | 75 | 100 |
| Skin lesion count | None | <50 |
| Mean day to lesion onset | n/a | 9 |
| Disease | Severe tracheitis and epiglotitis | Severe bronchopneumonia |
| Peak viraemia (gene copies log10 p.f.u. ml−1) | 5 | 6 |
| Tissue distribution | Lung, tracheobronchial lymph node, kidney, heart, adrenal gland | Lung, kidney, liver |
| Cytokine response | Mixed | Pro-inflammatory |
| Monocytosis | Yes | Yes |
| Decrease in peripheral oxygenation | No | Yes |
| Mean day to endpoint | 12 | 9 |
Further comparison of large-particle exposure of CPXV to rhesus monkeys to other NHP models of human smallpox, and smallpox itself suggests some similarities and notable differences as summarized in Fig. 6 (Fenner, 1988; Huggins et al., 2009; Jahrling et al., 2004; Johnson et al., 2011a, 2011b, 2015; Kramski et al., 2010; Nalca et al., 2010; Reynolds et al., 2006). Most notably, CPXV-infected macaques develop few skin lesions when compared with MPXV-infected macaques and VARV-infected humans. The incubation period (time from exposure to development of clinical signs) of the intranasal CPXV marmoset model more closely matches smallpox than the other models. However, reagent availability, subject availability and subject size limit the utility of the common marmoset model. The MPXV IV exposure models result in rapid disease with onset of clinical signs between days 4 and 6 and IV exposure is not a natural route of transmission, which impacts the utility of the model in terms of the FDA’s ‘Animal Rule’. Airway exposure models are more variable, but provide the best avenue for development of an NHP model of smallpox due to increased incubation periods, and more accurately reflect a natural exposure route than IV exposure.
Fig. 6.
Comparison of NHP models of smallpox to human smallpox. The different NHP models are aligned against human smallpox. Incubation period, rash onset and staging, and lymphadenopathy and development of other clinical signs are noted for cross-model comparison. IB, Intrabronchial; IN, intranasal.
Large-particle aerosol of CPXV resulted in a predictable distribution of lesions within the upper respiratory tract and major airways resulting in severe pharyngitis, tracheitis and bronchitis/bronchiolitis. Consolidating pulmonary parenchymal or alveolar lesions were seen in only two subjects in the high dose group. The pulmonary parenchymal lesions seen in the remainder of the subjects extended only a short distance from the tertiary bronchioles and were not as severe as those observed following small-particle aerosol exposure. Additionally, we showed that within these areas of severe lung and tracheal pathology, macrophages were commonly CPXV-antigen-positive, suggestive of direct infection. Independent of dose, lung pathology observed by CT in monkeys that met endpoint criteria was similar and corresponded with gross pathology and histopathology. The CT changes included peribronchial thickening/infiltrates, patchy foci of ground glass (alveolar) opacification, with occasional consolidations mainly seen in the high dose group subjects. No pleural effusions were seen. Quantification of disease severity using PCLH significantly correlated with various clinical parameters including peripheral oxygen saturation, respiratory rate and circulating monocyte numbers, especially for the 5×107p.f.u. group. This suggests reliable assessment of disease severity using CT, and the potential to use imaging as surrogate endpoint of disease progression/treatment in future therapeutic intervention studies. Unfortunately, quantitative evaluation of the pharynx, epiglottis and proximal trachea using CT is limited, and was obscured by the presence of the ET tube in these anaesthetized monkeys.
Characterization of the immune response to large-particle exposure demonstrated many differences when compared with small-particle aerosol exposure to CPXV. Most notably, a dominant pro-inflammatory systemic cytokine response was not observed. This is in contrast to the systemic inflammatory response as has been suggested after IV CPXV, MPXV and small-particle aerosol exposures (Jahrling et al., 2004; Johnson et al., 2011a, b, 2015). Changes in the PBMCs were consistent with the dosing, for example, monocytes increased substantially and more rapidly for the 5×107 and 5×106 p.f.u. group subjects than for the 5×105 and 5×104 p.f.u. groups. NK cells increased the most for the 5×105 and 5×104 p.f.u. group, underscoring their importance for resolution of poxvirus-induced disease (Americo et al., 2010; Bai et al., 2005; Born et al., 2000; Earl et al., 2012; Harris et al., 1995). Predictably, T- cells and immature B-cells increased in surviving subjects independent of dose. The specific function of these cells and cytokines in response to CPXV infection is beyond the scope of this work, but establishing the dynamics of these cell populations and cytokines provides many opportunities for future hypothesis-driven research. The current experiment was designed to establish the large-particle infection model. Future experiments would include a more detailed investigation of the tissue-specific response to infection. Such experiments would include serial euthanasia to directly compare CT and pathology during disease development. Since bronchoalveolar lavage can induce an inflammatory response that can be observed by CT (Haley et al., 1989; Von Essen et al., 1991), such procedures would be best performed as terminal procedures with control groups to provide an accurate basis of comparison.
A model that accurately mimics human smallpox should result in systemic disease. In this study, viraemia was detected 3 days prior to euthanasia for three of five subjects with a peak of 5.23 log10 genome copies ml−1. Viral load in the tissue as measured by plaque assay indicates that many tissues were positive, but at levels that indicate blood contamination of the tissue rather than production of infectious virus in those tissues. However, viral load in the lung (6.9 log10 p.f.u. mg−1) and tracheobronchial lymph node (6.23 log10 p.f.u. mg−1) indicates that these tissues were actively infected and that the observed tissue damage is virus-induced. Regrettably, we did not collect trachea for evaluation of viral load, however, myriads of intraepithelial, eosinophilic, intracytoplasmic inclusion bodies consistent with orthopoxvirus were seen in the tracheal epithelium by histopathology.
The current study demonstrates that aerosol particle size impacts virus deposition within the respiratory tract and drives disease presentation and pathogenesis, and that systemic virus dissemination following large-particle aerosol exposure is possible. However, the observed severe respiratory disease may progress too quickly to allow for the development of secondary viraemia and systemic disease as described for smallpox. This may be overcome by large-particle aerosol exposure with other poxviruses such as MPXV or VARV as neither is as pathogenic as CPXV in Macaca species (Goff et al., 2011; Jahrling et al., 2004; Johnson et al., 2011a, b, 2015). In addition, CPXV strains other than Brighton Red, that possess differences in pathogenicity, may provide a model with greater fidelity to human smallpox.
Methods
Virus and cells.
CPXV-BR was propagated as described previously (Johnson et al., 2015). Briefly, B-SC-1 cells (ATCC) were infected at a low multiplicity of infection until cytopathic effect reached 80 % (roughly 2 days). B-SC-1 cells were maintained in modified Eagle’s medium (MEM) (HyClone) supplemented with 2 % FBS (Sigma) and 1 % penicillin/streptomycin at 37 °C with 5 % CO2. Virus was prepared for exposure by rapid thaw of the virus stock and sonication.
Exposure and monitoring of NHPs.
All animal procedures were approved by the National Institute of Allergy and Infectious Diseases (NIAID) Division of Clinical Research Animal Care and Use Committee, and adhered to National Institutes of Health (NIH) policies. The experiments were carried out at the NIAID Integrated Research Facility, an AAALAC and AALAS accredited facility. Experiments followed the guidelines and basic principles of the United States Public Health Service Policy on Human Care and Use of Laboratory Animals and the Guide for the Care and Use of Laboratory Animals. Procedures were carried out under anaesthesia using ketamine and/or isoflurane by trained veterinary personnel. Subjects were housed in individual caging that allowed for social interactions in a temperature- and humidity-controlled environment. Food and water were available ad libitum and enrichment was provided twice daily. Endpoint criteria, as approved by the Division of Clinical Research, Animal Care and Use Committee (DCR ACUC), were used to determine when animals met humane endpoint criteria. At that time, they were euthanized under deep anaesthesia.
Sixteen rhesus monkeys (Macaca mulatta), that were pan-orthopox-negative and negative for simian retrovirus, simian T-lymphotrophic virus, and ranged in weight from 4.16 to 13.12 kg were included in this study. The groups consisted of 13 males and 3 females and ranged in age from to 3 to 8 years. Groups received a target dose of 5×107 p.f.u. – 5×104 p.f.u. in decreasing serial tenfold increments. Prior to and post-aerosol exposure, CT and physical exams, including temperature, weight and lesion counts, were performed, and blood draws and swabs from oral and nasal cavities were taken on physical exam days and necropsy. Subjects were maintained on inhalational isoflurane during CT procedures. Study subjects were monitored at least twice daily and euthanized when they met pre-established criteria; these criteria included: (1) overall clinical appearance, (2) laboured breathing, (3) activity and behaviour, (4) responsiveness, and (5) core body temperatures as evaluated by veterinary staff. At the time of necropsy, NHPs were humanely euthanized and additional blood, oral and nasal swabs, and select tissues were collected for further evaluation.
Large-particle aerosol exposure.
Rhesus monkeys (n=16) were exposed to CPXV-BR using a 16 l, head only, aerosol exposure chamber and an aerosol management platform (AeroMP; Biaera Technologies) within a Class III biosafety cabinet (BSC) (Germfree). Characterization studies ensuring viral stability and viability were conducted prior to NHP aerosol exposures. Virus dilutions were prepared in Eagle’s minimum essential medium (Lonza) in 10 % glycerol (v/v) (Sigma Aldrich). The subjects were anaesthetized with ketamine and received a time-calculated aerosol exposure based on NHP minute ventilation. Aerosol particles were generated by the Centered Flow Tangential Aerosol Generator (CenTAG; CH Technologies). A stainless steel filter sampler (In-Tox Products) using a gelatin membrane filter (Sartorius) operating at a continuous flow rate of 2 LPM was used to determine the aerosol concentration within the chamber. An air wash period of 5 min between exposures allowed the particles to decay. The exposure chamber (−0.1’ WC) and Class III BSC (−1.0’ WC) both maintained negative airflow throughout the challenge. Prior to an exposure, subject-specific minute volume values were obtained using plethysmography acquisition equipment (Buxco-DSI). An averaged respiratory minute volume (l min−1) for a 3 min collection period was obtained and used to calculate the presented dose. A presented dose was calculated using the simplified formula D=R×Ca×T, where D is the presented or estimated inhaled dose (p.f.u.), R is the respiratory minute volume (l min−1), Ca is the aerosol concentration (p.f.u. l−1), and T is the duration of the exposure (min) (Hartings & Roy, 2004).
Computed tomography (CT) and image analysis.
CT was acquired as previously described (Johnson et al., 2015). PCLH was determined as described previously (Solomon et al., May 2014). The quantitative analysis was compared with a blinded, qualitative evaluation of CT lung pathology over time, performed by a radiologist (D. A. H.).
Haematology and serology.
Samples for complete blood cell differential count (CBC/diff) were collected in EDTA-coated blood tubes and analysed using a Sysmex XT2000V (Sysmex America). Blood samples for serum chemistries evaluation were drawn using a serum separation tube and analysed on a COBAS INTEGRA 400Plus (Roche Diagnostics).
PBMC dynamics were evaluated as previously described in Johnson et al. (2011b). Briefly, EDTA whole blood samples were collected from NHPs and analysed using TruCount tubes (BD Biosciences) using a commercial antibody cocktail containing markers for CD45, CD3, CD4, CD8, CD14, CD16, CD20 (BD Biosciences), and CD159 (NKG2a) (Beckman Coulter). Samples were analysed on the BD Fortessa flow cytometer. Data were analysed using BD FACSDiva software v6.1.3 (BD Biosciences). Cells were first gated on CD45, then CD3+ and CD3− populations were selected against CD45. CD3+ populations were then gated against CD4 and CD8 subpopulations. CD3− populations were gated against CD14, NKG2a and CD20 subpopulations.
Quantification of viraemia by quantitative PCR and tissue viral load by plaque assay.
Swabs and whole blood samples were extracted with Trizol and evaluated for CPXV genomes using the HA gene assay (Sofi Ibrahim et al., 2003) on an ABI 7900HT. Plaque assays were performed as previously described (Johnson et al., 2015). Viral load in lungs were the mean titres of samples from the six lobes for each NHP. Liver titres were the mean of left, right, medial and caudal liver lobe titres. Sections of the right kidney and right adrenal gland for each non-surviving subject were excised and titres determined.
Cytokine and chemokine analysis.
The concentrations of the cytokines and chemokines MCP-1, IL-6, IL-8, IFN-γ, sCD40L, G-CSF, IL-12 and VEGF in plasma samples were analysed using the Millipore NHP Cytokine Panel (Millipore) following manufacturer's recommendations and were assayed on the FlexMap 3D System (Luminex).
Histopathology, immunohistochemistry and immunofluor- escence.
Forty-one tissues from all major organ systems were collected and fixed in 10 % neutral buffered formalin. Samples were embedded in paraffin, sectioned at 4 µm, and stained with haematoxylin and eosin (H&E) according to established protocols. H&E sections were examined by light microscopy by a veterinary pathologist (D. L. P.). For immunohistochemical (IHC) and immunofluorescence (IF) analyses, lung sections were baked at 60 °C for 1 h then deparaffinized with xylene and rehydrated with alcohol-gradated washes. Sections were microwaved with Antigen Unmasking Solution (Vector Laboratories). After exposure to protein block (Dako) for 30 m, rabbit anti-Vaccinia virus antibody was added at a dilution of 1 : 800 (IHC) or 1 : 1000 (IF), followed by biotinylated goat anti-rabbit immunoglobulin G (IgG; Vector Laboratories) at a dilution of 1 : 200 (IHC) or AlexaFluor 594 (Vaccinia) and AlexaFluor 488 (IBA1; Macrophage at a dilution of 1 : 100) (IF). Sections were incubated for 30 m with Vectastain ABC reagent (Vector Laboratories) and for 25 min with 3′3′ diaminobenzidine (DAB) were counterstained with haematoxylin (IHC) or DAPI (IF) and evaluated by a veterinary pathologist (I. N. M.).
Acknowledgements
This work was supported by the US National Institute of Allergy and Infectious Diseases (NIAID) Division of Intramural Research. We are grateful to Marisa St. Claire (Integrated Research Facility, Division of Clinical Research, NIAID), Russell Byrum (Integrated Research Facility, Division of Clinical Research NIAID), Dan Ragland (Integrated Research Facility, Division of Clinical Research, NIAID), and the entire EVPS and IRF team for their contributions to these studies. We thank Jiro Wada for his contribution to the preparation of this manuscript. The content of this publication does not necessarily reflect the views or policies of the US Department of Health and Human Services (DHHS) or of the institutions and companies affiliated with the authors. This work was funded in part through Battelle Memorial Institute’s prime contract with the NIAID under contract no. HHSN272200700016I. K. B. J. and K. J. B. performed this work as employees of Battelle Memorial Institute. Subcontractors to Battelle Memorial Institute who performed this work are: C. J., an employee of Tunnell Government Services, Inc.; D. L. P. and K. C., employees of Charles River Laboratories; K. R. H. an employee of MRI Global; and P. J. S. an employee of MedRelief. This project has been funded in whole or in part with federal funds from the National Cancer Institute, National Institutes of Health, under contract no. HHSN261200800001E. The content of this publication does not necessarily reflect the views or policies of the DHHS, nor does mention of trade names, commercial products, or organization imply endorsement by the US Government.
Supplementary Data
Supplementary File 1
References
- Aebersold P.(2012). FDA experience with medical countermeasures under the Animal Rule. Adv Prev Med 2012507571. 10.1155/2012/507571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Americo J. L., Moss B., Earl P. L.(2010). Identification of wild-derived inbred mouse strains highly susceptible to monkeypox virus infection for use as small animal models. J Virol 848172–8180. 10.1128/JVI.00621-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai H., Buller R. M., Chen N., Green M., Nuara A. A.(2005). Biosynthesis of the IFN-gamma binding protein of ectromelia virus, the causative agent of mousepox. Virology 33441–50. 10.1016/j.virol.2005.01.015 [DOI] [PubMed] [Google Scholar]
- Barnewall R. E., Fisher D. A., Robertson A. B., Vales P. A., Knostman K. A., Bigger J. E.(2012). Inhalational monkeypox virus infection in cynomolgus macaques. Front Cell Infect Microbiol 2117. 10.3389/fcimb.2012.00117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohannon J. K., Lackemeyer M. G., Kuhn J. H., Wada J., Bollinger L., Jahrling P. B., Johnson R. F.(2015). Generation and characterization of large-particle aerosols using a center flow tangential aerosol generator with a non-human-primate, head-only aerosol chamber. Inhal Toxicol 27247–253. 10.3109/08958378.2015.1033570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Born T. L., Morrison L. A., Esteban D. J., VandenBos T., Thebeau L. G., Chen N., Spriggs M. K., Sims J. E., Buller R. M.(2000). A poxvirus protein that binds to and inactivates IL-18, and inhibits NK cell response. J Immunol 1643246–3254. 10.4049/jimmunol.164.6.3246 [DOI] [PubMed] [Google Scholar]
- Bray M., Buller M.(2004). Looking back at smallpox. Clin Infect Dis 38882–889. 10.1086/381976 [DOI] [PubMed] [Google Scholar]
- Damon I. K., Damaso C. R., McFadden G.(2014). Are we there yet? The smallpox research agenda using variola virus. PLoS Pathog 10e1004108. 10.1371/journal.ppat.1004108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon C. W.(1962). Smallpox. London: Churchill. [Google Scholar]
- Downie A. W., Fedson D. S., Saint Vincent L., Rao A. R., Kempe C. H.(1969). Haemorrhagic smallpox. J Hyg 67619–629. 10.1017/S0022172400042078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earl P. L., Americo J. L., Moss B.(2012). Lethal monkeypox virus infection of CAST/EiJ mice is associated with a deficient gamma interferon response. J Virol 869105–9112. 10.1128/JVI.00162-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenner F.(1980). Smallpox and its eradication. Aust Nz J Med 10459. [Google Scholar]
- Fenner F.(1988). The clinical features of smallpox. Smallpox and Its Eradication. Edited by Fenner F., Henderson D. A., Arita I., Jezek Z., Ladnyi I. D.Geneva, Switzerland: World Health Organization. [Google Scholar]
- Fenner F., Henderson D. A., Arita I., Jezek J., Ladnyi I. D.(1988). Smallpox and Its Eradication. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Goff A. J., Chapman J., Foster C., Wlazlowski C., Shamblin J., Lin K., Kreiselmeier N., Mucker E., Paragas J., et al. (2011). A novel respiratory model of infection with monkeypox virus in cynomolgus macaques. J Virol 854898–4909. 10.1128/JVI.02525-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahon N.(1961). Smallpox and related poxvirus infections in the simian host. Bacteriol Rev 25459–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley P. J., Muggenburg B. A., Rebar A. H., Shopp G. M., Bice D. E.(1989). Bronchoalveolar lavage cytology in cynomolgus monkeys and identification of cytologic alterations following sequential saline lavage. Vet Pathol 26265–273. 10.1177/030098588902600312 [DOI] [PubMed] [Google Scholar]
- Harris N., Buller R. M., Karupiah G.(1995). Gamma interferon-induced, nitric oxide-mediated inhibition of vaccinia virus replication. J Virol 69910–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartings J. M., Roy C. J.(2004). The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J Pharmacol Toxicol Methods 4939–55. 10.1016/j.vascn.2003.07.001 [DOI] [PubMed] [Google Scholar]
- Hinds W. C.(1999). Respiratory Deposition, Aerosol Technology. Properties, Behavior and Measurement of Aerosol Particles. New York: John Wiley & Sons. [Google Scholar]
- Huggins J., Goff A., Hensley L., Mucker E., Shamblin J., Wlazlowski C., Johnson W., Chapman J., Larsen T., et al. (2009). Nonhuman primates are protected from smallpox virus or monkeypox virus challenges by the antiviral drug ST-246. Antimicrob Agents Chemother 532620–2625. 10.1128/AAC.00021-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrling P. B., Hensley L. E., Martinez M. J., LeDuc J. W., Rubins K. H., Relman D. A., Huggins J. W.(2004). Exploring the potential of variola virus infection of cynomolgus macaques as a model for human smallpox. Proc Natl Acad Sci U S A 10115196–15200. 10.1073/pnas.0405954101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrling P. B., Tomori O.(2014). Variola virus archives: a new century, a new approach. The Lancet 3831525–1526. 10.1016/S0140-6736(14)60693-0 [DOI] [PubMed] [Google Scholar]
- Johnson R. F., Dyall J., Ragland D. R., Huzella L., Byrum R., Jett C., St Claire M., Smith A. L., Paragas J., et al. (2011a). Comparative analysis of monkeypox virus infection of cynomolgus macaques by the intravenous or intrabronchial inoculation route. J Virol 852112–2125. 10.1128/JVI.01931-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R. F., Yellayi S., Cann J. A., Johnson A., Smith A. L., Paragas J., Jahrling P. B., Blaney J. E.(2011b). Cowpox virus infection of cynomolgus macaques as a model of hemorrhagic smallpox. Virology 418102–112. 10.1016/j.virol.2011.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R. F., Hammoud D. A., Lackemeyer M. G., Yellayi S., Solomon J., Bohannon J. K., Janosko K. B., Jett C., Cooper K., et al. (2015). Small particle aerosol inoculation of cowpox Brighton Red in rhesus monkeys results in a severe respiratory disease. Virology 481124–135. 10.1016/j.virol.2015.02.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramski M., Mätz-Rensing K., Stahl-Hennig C., Kaup F. J., Nitsche A., Pauli G., Ellerbrok H.(2010). A novel highly reproducible and lethal nonhuman primate model for orthopox virus infection. PLoS One 5e10412. 10.1371/journal.pone.0010412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mätz-Rensing K., Ellerbrok H., Ehlers B., Pauli G., Floto A., Alex M., Czerny C. P., Kaup F. J.(2006). Fatal poxvirus outbreak in a colony of New World monkeys. Vet Pathol 43212–218. 10.1354/vp.43-2-212 [DOI] [PubMed] [Google Scholar]
- Milton D. K.(2012). What was the primary mode of smallpox transmission? Implications for biodefense. Front Cell Infect Microbiol 2. 10.3389/fcimb.2012.00150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra A. C., Sarkar J. K., Mukherjee M. K.(1974). Virus content of smallpox scabs. Bull World Health Organ 51106–107. [PMC free article] [PubMed] [Google Scholar]
- Nalca A., Livingston V. A., Garza N. L., Zumbrun E. E., Frick O. M., Chapman J. L., Hartings J. M.(2010). Experimental infection of cynomolgus macaques (Macaca fascicularis) with aerosolized monkeypox virus. PLoS One 5e12880. 10.1371/journal.pone.0012880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker A. K., Parker S., Yokoyama W. M., Corbett J. A., Buller R. M. L.(2007a). Induction of natural killer cell responses by ectromelia virus controls infection. J Virol 814070–4079. 10.1128/JVI.02061-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker S., Nuara A., Buller R. M. L., Schultz D. A.(2007b). Human monkeypox: an emerging zoonotic disease. Future Microbiol 217–34. 10.2217/17460913.2.1.17 [DOI] [PubMed] [Google Scholar]
- Rao A. R., Jacob E. S., Kamalakshi S., Appaswamy S., Bradbury(1968). Epidemiological studies in smallpox. A study of intrafamilial transmission in a series of 254 infected families. Indian J Med Res 561826–1854. [PubMed] [Google Scholar]
- Reynolds M. G., Yorita K. L., Kuehnert M. J., Davidson W. B., Huhn G. D., Holman R. C., Damon I. K.(2006). Clinical manifestations of human monkeypox influenced by route of infection. J Infect Dis 194773–780. 10.1086/505880 [DOI] [PubMed] [Google Scholar]
- Smith A. L., St Claire M., Yellayi S., Bollinger L., Jahrling P. B., Paragas J., Blaney J. E., Johnson R. F.(2012). Intrabronchial inoculation of cynomolgus macaques with cowpox virus. J Gen Virol 93159–164. 10.1099/vir.0.036905-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofi Ibrahim M., Kulesh D. A., Saleh S. S., Damon I. K., Esposito J. J., Schmaljohn A. L., Jahrling P. B.(2003). Real-time PCR assay to detect smallpox virus. J Clin Microbiol 413835–3839. 10.1128/JCM.41.8.3835-3839.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon J., Johnson R., Douglas D., Hammoud D.(2014). New image analysis technique for quantitative longitudinal assessment of lung pathology on CT in infected rhesus macaques. IEEE Computer-Based Medical Systems , p. 169 Edited by O'Conner L.New York: IEEE Computer Society. [Google Scholar]
- Tucker J. B.(2011). Breaking the deadlock over destruction of the smallpox virus stocks. Biosecur Bioterror 955–67. 10.1089/bsp.2010.0065 [DOI] [PubMed] [Google Scholar]
- Von Essen S. G., Robbins R. A., Spurzem J. R., Thompson A. B., McGranaghan S. S., Rennard S. I.(1991). Bronchoscopy with bronchoalveolar lavage causes neutrophil recruitment to the lower respiratory tract. Am Rev Respir Dis 144848–854. 10.1164/ajrccm/144.4.848 [DOI] [PubMed] [Google Scholar]
- Vorou R. M., Papavassiliou V. G., Pierroutsakos I. N.(2008). Cowpox virus infection: an emerging health threat. Curr Opin Infect Dis 21153–156. 10.1097/QCO.0b013e3282f44c74 [DOI] [PubMed] [Google Scholar]
- Wehrle P. F., Posch J., Richter K. H., Henderson D. A.(1970). An airborne outbreak of smallpox in a German hospital and its significance with respect to other recent outbreaks in Europe. Bull World Health Organ 43669–679. [PMC free article] [PubMed] [Google Scholar]
- Zaucha G. M., Jahrling P. B., Geisbert T. W., Swearengen J. R., Hensley L.(2001). The pathology of experimental aerosolized monkeypox virus infection in cynomolgus monkeys (Macaca fascicularis). Lab Invest 811581–1600. 10.1038/labinvest.3780373 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary File 1