Abstract
This randomized controlled trial was designed to determine if art therapy in conjunction with Cognitive Processing Therapy (CPT) was more effective for reducing symptoms of combat posttraumatic stress disorder (PTSD) than CPT alone. Veterans (N = 11) were randomized to receive either individual CPT, or individual CPT in conjunction with individual art therapy. PTSD Checklist–Military Version and Beck Depression Inventory–II scores improved with treatment in both groups with no significant difference in improvement between the experimental and control groups. Art therapy in conjunction with CPT was found to improve trauma processing and veterans considered it to be an important part of their treatment as it provided healthy distancing, enhanced trauma recall, and increased access to emotions.
Introduction
Posttraumatic stress disorder (PTSD) affects hundreds of thousands of veterans in the United States. A meta-analysis estimated that 23% of veterans of recent wars in Iraq and Afghanistan suffer from PTSD (Fulton et al., 2015), and 405,915 veterans of these operations were seen in Veterans Affairs facilities as of 2015 (U.S. Department of Veterans Affairs, 2015) and diagnosed with primary, secondary, or provisional PTSD. In addition, an estimated 17% of Vietnam-era veterans (Goldberg et al., 2016; Price, 2016), and an estimated 10% of Gulf War veterans (Kang, Natelson, Mahan, Lee, & Murphy, 2003) have experienced lifetime PTSD.
The Diagnostic and Statistical Manual of Mental Disorders defines posttraumatic stress disorder (PTSD) according to the following diagnostic criteria: exposure to a traumatic event, reexperiencing traumatic material, hyperarousal, negative cognitions and mood, and avoidance of reminders (American Psychiatric Association, 2013). One of the major evidence-based approaches to treating PTSD is Cognitive Processing Therapy (CPT; Forbes et al., 2012; Macdonald, Monson, Doron-Lamarca, Resick, & Palfai, 2011; Nishith, Nixon, & Resick, 2005; Ponniah & Hollon, 2009). However, research has suggested that as many as 30% of patients may be unresponsive to evidence-based treatments (Wisco, Marx, & Keane, 2012), and some experience residual symptoms even after treatment (Riggs & Sermanian, 2012). Evidence also suggests that impairment in verbal memory may be more severe in PTSD caused by combat compared with other sources of trauma (Johnsen & Asbjørnsen, 2008). Therefore, it is critical for new treatment approaches to specifically address the needs of combat veterans.
Art therapy may assist with integration of sensory memories and declarative memory and has been shown to reduce symptoms of PTSD in a number of populations (Harber, 2011; Henderson, Rosen & Mascaro, 2007; Lyshak-Stelzer, Singer, St. John, & Chemtob, 2007; Pifalo, 2007, 2009; Tripp, 2007); however, there are no known randomized controlled trials on the effects of art therapy on combat-related PTSD. In a 2013 Delphi study (Kaiser & Deaver, 2013), a panel of expert art therapy researchers identified randomized controlled trials as the highest priority for the art therapy field, and trauma as the most important psychological construct to address through research. Thus, our study supports these highest priorities of the profession.
Art Therapy and PTSD
Studies have suggested that some traumatic memories are stored nonverbally (Gantt & Tinnin, 2009; Langer, 2011; Talwar, 2007) and may be retrieved through recollections of sensory, affective, visual, olfactory, auditory, and kinesthetic elements (Langer, 2011). Although verbal therapies fail to address nonverbal aspects of trauma experiences, art therapy can access trauma recollections by engaging the senses. Art therapy has been hypothesized to bring order to traumatic experiences by creating links to nonverbal memories so that dissociated memories may be organized and processed in a meaningful way (Gantt & Tinnin, 2009).
Art therapy provides a safe way to approach traumatic memories through the use of symbols, which may facilitate consolidation of experiences by converting an artistic form, representative of emotions and reactions to trauma, into linguistic communication (Gantt & Tinnin, 2007; Morgan & Johnson, 1995). According to Talwar (2007), art making is hypothesized to involve bilateral stimulation, engaging the integrating and planning functions of the prefrontal cortex to sequence narratives using left brain functions. This integration between the left and right hemispheres of the brain allows for complete processing and storage of traumatic experiences in long-term memory.
Art therapy provides externalization and emotional distance through materials and processes that use mediators, such as a paintbrush, between the patient and the image. The controlled distance encourages the patient to depict trauma experiences and to view the finished image at a physical distance (Tinnin, Bills, & Gantt, 2002). According to Tinnin et al., these techniques can be useful when the patient does not consciously remember the sequence of events in visual trauma narratives, and they can help the patient feel safe enough to address unresolved trauma memories.
Types of Art Therapy for PTSD
The most widely used art therapy practice for PTSD is the creation of a visual trauma narrative (Cross, 2015; Gantt & Tinnin, 2007, 2009; Harber, 2011; Lyshak-Stelzer et al., 2007; Pifalo, 2009; Rankin & Taucher, 2003; Sarid & Huss, 2010; Spiegel, Malchiodi, Backos, & Collie, 2006; Talwar, 2007). The narrative can facilitate new insight, as well as help patients reconstruct their concept of self, others, and the world (Rankin & Taucher, 2003; Spiegel et al., 2006) and is hypothesized to reduce emotional numbing and avoidance (Spiegel et al., 2006; Tinnin et al., 2002). Naff (2014) also has stressed the importance of a visual trauma narrative, after the therapist creates a safe environment to contain the powerful emotional memories and emotions connected with the trauma. According to van der Kolk and Najavits (2013), the first step in trauma therapy is to notice body sensations. In another study, narration of trauma in the first person was associated with greater increases in heart rate and skin conductance responses compared to narrating the trauma in the third person (Wisco et al., 2015).
Results of Prior Studies of Art Therapy for PTSD
In a randomized controlled trial, Henderson et al. (2007) studied two groups of adults with PTSD symptoms; the experimental group depicted trauma-related feelings and emotions within a circle, and the control group drew assigned daily objects such as a cup. At a 1-month follow-up session, the researchers found that participants in the experimental group experienced greater reduction in PTSD symptoms—but not in depression or anxiety symptoms—than control group participants. Creating art also has been found to improve mood significantly more than simply viewing art (Bell & Robbins, 2007). In a randomized controlled trial, Lyshak-Stelzer et al. (2007) found that adolescents with PTSD symptoms who made a narrative book of their life stories demonstrated significant PTSD symptom relief in comparison to control group participants. Furthermore, Gantt and Tinnin (2007) found that when using art therapy for trauma treatment, 89% of participants in their program either fully recovered or met criteria for improvement.
Although there are no prior studies of CPT in conjunction with art therapy (Kaiser et al., 2005), Pifalo (2007) used art therapy in combination with cognitive behavioral therapy and found that art therapy allowed patients to communicate without relying strictly on words, and cognitive behavioral therapy provided clear goals for therapy. The combination of the two methods yielded significant subjective improvement in symptoms of children with PTSD from sexual abuse. An early observational study found that in specialized inpatient PTSD units, out of 15 standard components, art therapy produced the most benefit for combat veterans (Johnson, Lubin, James, & Hale, 1997). In the only known study on art therapy with war veterans, art therapy was associated with reduced depression (Kopytin & Lebedev, 2013).
Based on these prior studies, the goal of our research was to explore whether combining art therapy with Cognitive Processing Therapy would provide greater benefit in processing trauma and reducing symptoms in veterans with combat-related PTSD than CPT alone. A mixed methods design was used with an art therapy protocol devised by Campbell (2014). This was a controlled trial in which participants were randomized by time to receive CPT alone or CPT along with eight sessions of individual art therapy. We hypothesized that participants who received CPT plus art therapy would experience a greater reduction in PTSD symptoms than participants who received only CPT, as measured by the PTSD Checklist–Military Version (PCL-M) and the Beck Depression Inventory–II (BDI-II). We also hypothesized that veterans in the experimental condition might prefer art therapy to CPT, as ascertained through reported satisfaction with treatment. Interviews were conducted to ascertain other benefits of art therapy that participants might have received that were not captured by PCL-M or BDI-II scores.
Method
This was a controlled trial in which participants were randomized to a control group or an experimental group by time of entry into residential treatment. The study received Institutional Review Board approval from the Hampton VA Medical Center and Eastern Virginia Medical School.
Participants
Participants were veterans in treatment for combat-related PTSD in a residential program. All participants received group therapy for PTSD as well as the interventions described herein. Inclusion criteria included a score on the PCL-M higher than 50. There were no restrictions on age, gender, era of combat experience, or branch of service. Exclusion criteria included active substance use disorder, psychosis, and active suicidal or homicidal ideation. Five participants were randomized to receive both art therapy and CPT, all of whom completed treatment, and 10 participants were randomized to receive CPT alone, of whom six completed treatment. Thus, 11 participants completed treatment out of the original sample of 15. Three of five participants in the experimental group who completed treatment were White; the other two were African American. Five of six participants in the control condition who completed treatment were African American and one was White. All participants were male.
Procedures
Veterans who consented to participate in the study were randomized to receive either eight sessions of individual CPT or eight sessions of individual art therapy in addition to eight sessions of individual CPT. Art therapy was delivered by the first author and CPT was delivered by several therapists, including the second author. The BDI-II and PCL-M scales were administered by the clinician delivering CPT or by the second author. The first author conducted semi-structured qualitative interviews with each participant to solicit feedback about the contribution of each therapy to treatment.
Cognitive Processing Therapy
CPT is a manualized, evidence-based treatment for PTSD (Forbes et al., 2012; Macdonald et al., 2011). For this study, CPT consisted of the first eight sessions of the published manual. CPT includes written homework between sessions with worksheets that facilitate separating dysfunctional thoughts and beliefs from emotions generated by the traumatic event (Resick, Monson & Chard, 2008). A written trauma narrative was also completed as homework. Discussion of the written trauma narrative with the CPT therapist and utilization of Socratic questioning to reframe negative thought processes and challenge distorted beliefs is central to CPT.
Art Therapy Protocol
The protocol for art therapy consisted of eight 75-minute sessions. The introductory session included the Art Therapy–Projective Imagery Assessment (Deaver & Bernier, 2014) and an interview with semi-structured interview questions. Session 2 featured psychoeducational material about PTSD, goal setting, and safety, and also addressed and identified symptoms and triggers.
Session 3 focused on creation of a visual trauma narrative, based on work by previous investigators (Gantt & Tinnin, 2007). Each veteran participant was directed to create six images. The first was an image of a time before the trauma when he felt peaceful and safe. The second was an image of the last moment he recalled immediately before the trauma occurred. The third was an image of what happened during the traumatic event. The fourth was an image of the moment immediately after the trauma. The fifth was an image of a time when he was safe from the physical threats of trauma. The last image was of a time when he tried to self-soothe. The participant was then asked to place the images on a wall and narrate the traumatic event from a third-person perspective to enhance healthy distancing from the event. This narrative was then repeated back to the participant by the art therapist. The visual trauma narrative was reviewed three times during the course of treatment.
Session 4 contained two elements: mask making and mind mapping. Mask making was utilized to assist participants in identifying and expressing emotions that were difficult to address verbally, and enable them to explore both their internal feelings and how they present themselves to the world. Mind mapping involved creating a web with the participant’s name in the middle inside of a small circle. From that center circle stemmed the core emotions he was experiencing as identified through the mask making, and any contributors to those emotions were included in order to further explore internal and external triggers. Session 5 began with narrating through the visual trauma narrative for a second time, and then addressed integration of “self before the trauma” with “self in the present.” This included making images about both of these parts of the self, then creating a written dialogue between the two images, using the nondominant hand for the former self, until a compromise could be reached about how these two parts of self can coexist (Gantt & Tinnin, 2007).
In Session 6 participants used art to address grief and loss caused by combat trauma by making an image of something lost during the traumatic event. The image was then torn up and papermaking was used to transform the shredded image into handmade paper on which a new image or list was created to envision how to overcome the loss. Session 7 focused on reconstructing a new worldview and self-concept. The final session consisted of a post-intervention interview, a review of the trauma narrative and all other artwork, and creation of reflective art.
Measures
The PCL-M and BDI-II were administered at the start, midpoint, and end of treatment. The Beck Depression Inventory-II (Beck & Steer, 1984) is a self-report measure of depression. The BDI-II has 21 items rated from 0 to 3, with higher scores indicating worse depression. Scores of 14 to19 indicate mild depression, scores of 20 to 28 indicate moderate depression, and scores above 29 suggest severe depression. The BDI-II demonstrates high internal consistency, with an alpha coefficient of .86 for psychiatric populations (Beck, Steer, & Garbin, 1988).
The PTSD Checklist–Military Version (Weathers, Litz, Herman, Huska & Keane, 1993) is a highly reliable—with Cronbach’s α of .94 (Norris & Hamblen, 2004)—and valid self-report scale with 17 items rated from 1 to 5 that measure the severity of PTSD symptoms. Items on the PCL-M correspond with the definition of PTSD according to criteria in the DSM-IV. A higher score corresponds to more severe PTSD symptoms (Pietrzak, Tsai, Harpaz-Rotem, Whealin, & Southwick, 2012).
Data Analysis
Analysis of variance (ANOVA) with repeated measures was used to analyze results of quantitative rating scales for PTSD and depression symptoms. The dependent variables were the BDI-II and PCL-M scores. The independent variable was assignment to CPT plus art therapy or CPT alone. Statistical results were analyzed using SPSS. Subjective ratings of treatment satisfaction were measured post-treatment with a Likert scale of 1 to 5 (with 5 being the highest) rating the usefulness of art therapy or CPT. Interviews were analyzed using a basic content analysis approach.
Results
PCL-M Scores
ANOVA with repeated measures was used to examine changes in PTSD symptoms. The mean PCL-M score in the experimental group decreased significantly, 73.0, SD = 8.5; 56.0, SD = 12.3.0, as did that of the control group, 62.8, SD = 10.9; 52.0, SD = 7.3. Improvement with treatment was significant for both groups, p < .001, μ2 = 0.80, but there was no between-group effect, p = .54, μ2 = 0.14.
BDI-II Scores
ANOVA with repeated measures was used to examine changes in depression symptoms. The mean BDI-II score improved in the experimental group, 37.0, SD = 11.7; 19.2, SD = 14.4, and the control group, 27.2, SD = 8.1; 17.6, SD = 9.7. The improvement with treatment was statistically significant for both groups with a large effect size, p < 0.001, μ2 = 0.80. There was a nonsignificant trend to a greater improvement for the experimental compared to the control group, with a small effect size, p = 0.06, μ2 = 0.3.
Ratings of Treatment Satisfaction
Control group participants’ average score for satisfaction with treatment was 4.8. Experimental group participants rated CPT at 3.2 and art therapy at 4.6 in terms of treatment satisfaction.
Interview Analysis
Content analysis of comments made by participants during pre-treatment and post-treatment interviews revealed the value of art therapy in helping participants work through avoidance and barriers to overcoming trauma. Another theme was that art therapy provided a positive form of expression, especially for painful emotions. One participant stated that art therapy “breaks through the ice and gets to heavier matters.” Two veterans had similar observations of the benefits of trauma exploration through art therapy: “It is easier for me to draw than write. It’s hard for me to put what I’m thinking into words,” and, “It helped me visualize trauma and emotions and connect it at the same time.”
Participants stated that art therapy assisted with understanding traumatic experiences: “I feel I learned a lot and was able to do a lot of soul searching.” A review of one participant’s artwork helped him “see differences in my perceptions before and after treatment.” One participant commented that art therapy helped with avoidance, and another stated, “I think I’ve made the greatest leaps forward here in my treatment with art therapy than with any of the other stuff.” Participants identified both the therapeutic relationship and the process as being helpful, and indicated that art therapy felt safe. Most veterans stated they would have liked to continue receiving art therapy.
Artwork
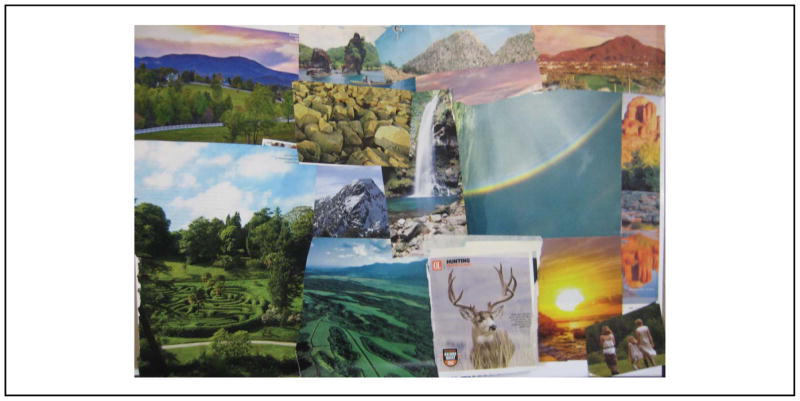
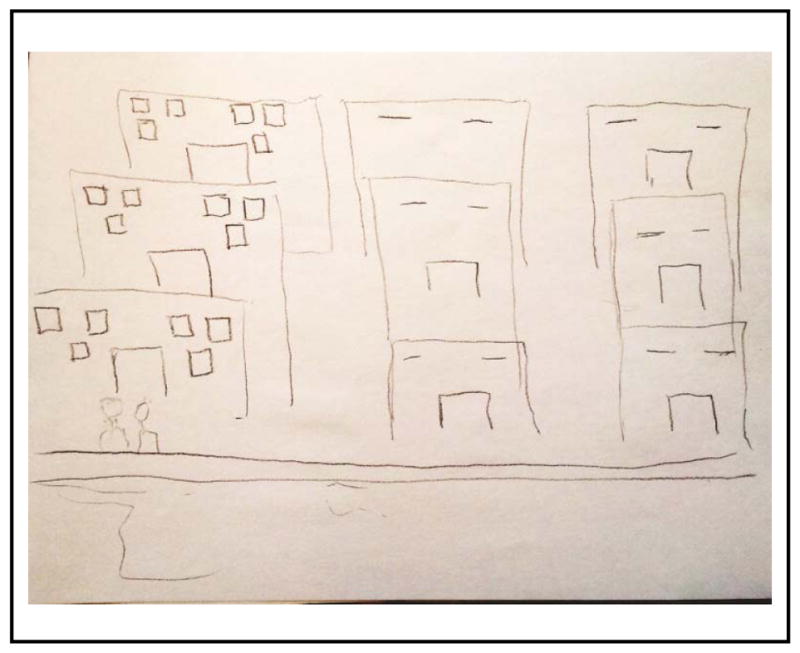
Some trends between participants’ artwork before and after treatment were noted. Pre-treatment artwork manifested sketchy line quality, avoidance, regression in response to anxiety, lack of identity, and encapsulation in images about the reason for being in treatment. The collage of safety incorporated themes of nature, religious symbols, cool colors, arc shapes, and, for some, isolation—as shown in the image in Figure 1. Participants were asked to depict six specific moments before, during, and after the traumatic event. The trauma narrative depicted in Figure 2 was created by a participant who added post-it notes with feelings labeled for each of the moments: the first reads “tranquility,” the second, “confusion,” the third “duty (anger),” the fourth “shock (disgust),” the fifth “content,” to which the participant later added “scared s…less,” and the last “numb.” Most participants’ trauma narratives manifested anxiety and deflection, and several did not include themselves in the images. Brown and black were common color choices. Most participants showed regression in their drawings of the trauma or the aftermath, as shown in the image in Figure 2. Containment was suggested in the drawing of physical safety after the trauma, where most participants used square shapes or circles, as seen in Figures 3 and 4. The image in Figure 3 is an example of a theme that was present in several participants’ artwork: containment using rectangular shapes or boxes to encapsulate sensitive material or provide compartmentalization for overwhelming emotions. It depicts a town in which the participant found physical safety after the trauma that includes rectangular buildings and two human outlines, with no other details. Another method of containment several participants used (Figure 4) was to encircle traumatic events or emotions. This image depicts the participant controlling suicidal ideation by encircling the image of suicide by firearm with a red circle that is crossed through, and which he stated represents his goal “not to commit suicide.” Most participants had difficulty speaking in the third person while narrating the trauma narrative. Mask creation required 2 hours to complete instead of the planned hour. Participants created complex masks with multicolored exteriors and colored interiors with a simpler palette.
Figure 1.
A Participant’s Collage Made to Depict the Concept of Safety
Figure 2.
Example of a Trauma Narrative
Figure 3.
Example of Containment Using Rectangular Shapes or Boxes to Encapsulate Sensitive Material or Provide Compartmentalization for Overwhelming Emotions
Figure 4.
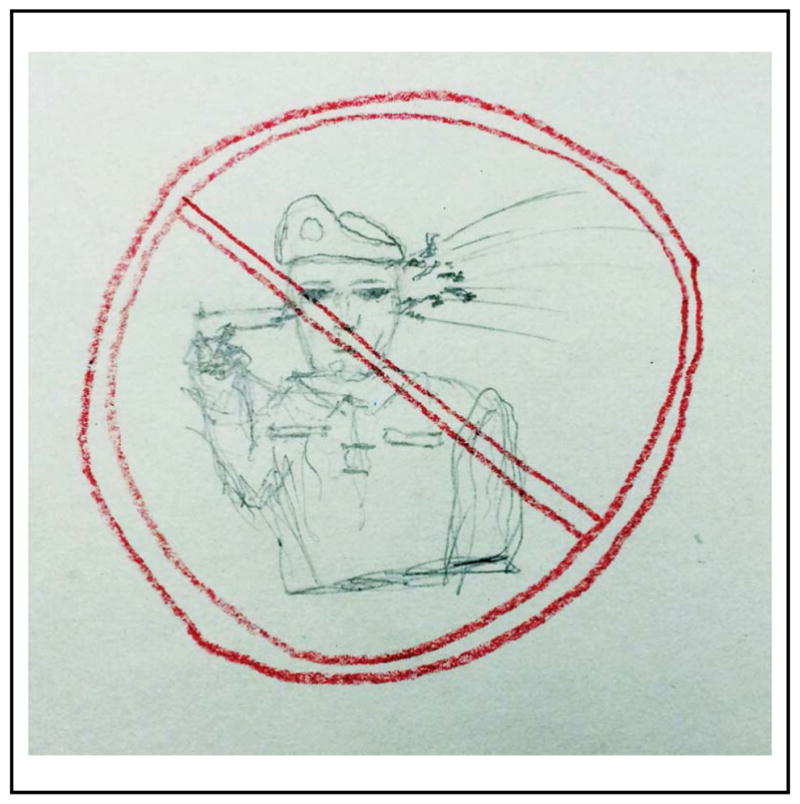
Another Method of Containment: Encircling Traumatic Events or Emotions
During the integration session, participants demonstrated a common theme of emptiness regarding the depiction of the self with PTSD, and none were able to complete a dialogue between the prior self and current self. There were no common themes in the session on grief and loss. Participants drew trauma-free worldviews that focused on childhood. All reported feeling stuck on trauma in their worldview. During the review of all artwork created during treatment, participants demonstrated an openness and honesty about what to leave behind.
Discussion
PTSD and Depression Scores
Two of the highest priorities for the field of art therapy were recently identified as randomized controlled trials of art therapy and researching the use of art therapy for treatment of trauma (Kaiser & Deaver, 2013). The current study addressed both these priorities. The hypothesis of our study was that art therapy provided with CPT would result in a greater reduction of PTSD symptoms in participants who received both treatments, compared with participants who received individual CPT alone. Both groups achieved clinically significant gains as defined by Weathers et al. (2013). However, there was no statistically significant difference between the experimental and control groups. It is possible that the lack of significant difference between groups was due to the small sample size (N = 11).
Another hypothesis was that participants receiving art therapy might experience greater reduction in depression symptoms than participants receiving only CPT. Both groups’ depression symptoms were reduced and both final mean scores were in the range of mild depression. Although not significantly different statistically, a trend toward greater reduction in depression symptoms for the experimental group compared to the control was noted.
Treatment Engagement and Satisfaction
An unexpected finding was that none of the participants in the experimental group dropped out of treatment, whereas 40% of those randomized to CPT alone left treatment prematurely. The dropout rate of the control group is consistent with a recent meta-analysis that showed a dropout rate for PTSD psychotherapies of 36% overall (Goetter et al., 2015). Although this study had a small sample size, our results suggest that art therapy may enhance engagement, which would be an important improvement in the treatment of PTSD.
Participants were highly satisfied with art therapy. Interventions that addressed insight, safety, containment, nonverbal symbolic access to emotions, and visual trauma processing can be considered unique elements of art therapy that increased participant satisfaction. Some participants also expressed that they had not expected the art to be such a useful source of healing.
Art therapy helped access traumas and overwhelming emotions in a safe way as evidenced by veterans’ interviews. The need for containment was seen in participants’ artwork through the use of circles or boxes to encapsulate sensitive material or provide compartmentalization for overwhelming feelings. Not only did the artwork indicate this need, it helped facilitate the fulfillment of it.
Trauma Processing
All participants who received art therapy stated that they either recovered previously blocked memories or gained insights and realizations crucial to their healing processes through art therapy. This is consistent with prior hypotheses that sensory methods of accessing and processing traumatic memories facilitate integration of those memories, and that some portion of traumatic memory is stored nonverbally (Gantt & Tinnin, 2009; Langer, 2011; Talwar, 2007). It has been hypothesized that trauma processing may be enhanced using sensory modalities to activate areas of the brain that have been affected and create pathways between declarative and nonverbal memories (Gantt & Tinnin, 2009).
Improved trauma processing was one of the most significant contributions of the art therapy intervention. Through externalization of trauma and emotions, artwork acted as an external reflection of the internal self for each participant during treatment. Some participants stated that the most significant gains occurred while hearing their experiences recited back to them as they viewed the visual trauma narrative. Repetition of auditory, verbal, and visual processing also appeared to be important. Each review of the visual trauma narrative built on the last, filled more gaps in memory, and reduced anxiety. It also may have been that the sensory modalities involved in art therapy represented an alternate, nonverbal way of deconditioning the threat response.
This study was limited by the small number of participants and by the lack of long-term follow-up. Another limitation was that there were multiple CPT therapists but only one art therapist, so experimenter effects may have affected validity. Participants were a subpopulation of veterans with severe symptoms and no women were available to participate in this study, which limits the study’s generalizability, even to other veterans. There were many areas of positive growth post-treatment that were not measured. Finally, both the PCL-M and BDI-II are self-rating scales, so participants may have exaggerated or underreported their symptoms.
In this study, both depression and PTSD symptoms were reduced in veterans with combat-related PTSD. The results suggest that art therapy is a useful addition to treatment of PTSD using Cognitive Processing Therapy. Future studies should include larger numbers of participants, more art therapist researchers to eliminate experimenter bias, and perhaps also focus on the contribution of art therapy alone for treatment of PTSD. Finally, other measures are needed to elucidate the mechanism of art therapy’s contribution to trauma symptom reduction.
Footnotes
Portions of this study were completed as a master’s art therapy thesis by the first author at Eastern Virginia Medical School.
Color versions of one or more of the figures in this article can be found online at www.tandfonline.com/uart.
Contributor Information
Melissa Campbell, Art therapist at the University Neuro-psychiatric Institute, University of Utah, Salt Lake City.
Kathleen P. Decker, Staff psychiatrist at the Hampton VA Medical Center, Hampton, VA, and faculty member in the Department of Psychiatry at Eastern Virginia Medical School, Norfolk
Kerry Kruk, Community faculty.
Sarah P. Deaver, Professor in the Graduate Art Therapy and Counseling Professions Program, Eastern Virginia Medical School
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory. Journal of Clinical Psychology. 1984;40(6):1365–1367. doi: 10.1002/1097-4679(198411)40:6<1365::AID-JCLP2270400615>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- Bell CE, Robbins SE. Effect of art production on negative mood: A randomized, controlled trial. Art Therapy: Journal of the American Art Therapy Association. 2007;24(2):71–75. doi: 10.1016/j.aip.2011.06.002. [DOI] [Google Scholar]
- Campbell M. Unpublished master’s thesis. Eastern Virginia Medical School; Norfolk, VA: 2014. Art therapy and cognitive processing therapy for combat PTSD: A randomized, controlled trial. [Google Scholar]
- Cross K. Unpublished master’s thesis. Eastern Virginia Medical School; Norfolk, VA: 2015. Interviews with trauma informed art therapists: A qualitative study. [Google Scholar]
- Deaver S, Bernier M. The Art Therapy–Projective Imagery Assessment. In: Handler L, Thomas A, editors. Drawings in assessment and psychotherapy: Research and application. New York, NY: Routledge; 2014. pp. 131–147. [Google Scholar]
- Forbes D, Lloyd D, Nixon RDV, Elliott P, Varker T, Perry D, … Creamer M. A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. Journal of Anxiety Disorders. 2012;26:442–452. doi: 10.1016/j.janxdis.2012.01.006. [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, … Beckham JC. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans: A meta-analysis. Journal of Anxiety Disorders. 2015;31:98–107. doi: 10.1016/j.janxdis.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Gantt L, Tinnin LW. Intensive trauma therapy of PTSD and dissociation: An outcome study. The Arts in Psychotherapy. 2007;34:69–80. doi: 10.1016/j.aip.2006.09.007. [DOI] [Google Scholar]
- Gantt L, Tinnin L. Support for a neurobiological view of trauma with implications for art therapy. The Arts in Psychotherapy. 2009;36:148–153. doi: 10.1016/j.aip.2008.12.005. [DOI] [Google Scholar]
- Goetter EM, Bui E, Ojserkis RA, Zakarian RJ, Brendel RW, Simon NM. A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. Journal of Traumatic Stress. 2015;28:401–409. doi: 10.1002/jts.22038. [DOI] [PubMed] [Google Scholar]
- Goldberg J, Magruder KM, Forsberg CW, Friedman MJ, Litz BT, Vaccarino V, … Smith NL. Prevalence of post-traumatic stress disorder in aging Vietnam-era veterans: Veterans Administration Cooperative Study 569: Course and consequences of post-traumatic stress disorder in Vietnam-era veteran twins. American Journal of Geriatric Psychiatry. 2016;24(3):181–91. doi: 10.1016/j.jagp.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harber K. Creating a framework: Art therapy elicits the narrative. Art Therapy: Journal of the American Art Therapy Association. 2011;28(1):19–25. doi: 10.1080/07421656.2011.557766. [DOI] [Google Scholar]
- Henderson P, Rosen D, Mascaro N. Empirical study on the healing nature of mandalas. Psychology of Aesthetics, Creativity, and the Arts. 2007;1(3):148–154. doi: 10.1037/1931-3896.1.3.148. [DOI] [Google Scholar]
- Johnsen GE, Asbjørnsen AE. Consistent impaired verbal memory in PTSD: A meta-analysis. Journal of Affective Disorders. 2008;111:74–82. doi: 10.1016/j.jad.2008.02.007. [DOI] [PubMed] [Google Scholar]
- Johnson DR, Lubin H, James M, Hale K. Single session effects of treatment components within a specialized inpatient posttraumatic stress disorder program. Journal of Traumatic Stress. 1997;10(3):377–390. doi: 10.1023/A:1024833119339. [DOI] [PubMed] [Google Scholar]
- Kaiser D, Deaver S. Establishing a research agenda for art therapy: A Delphi study. Art Therapy: Journal of the American Art Therapy Association. 2013;30(3):114–121. doi: 10.1080/07421656.2013.819281. [DOI] [Google Scholar]
- Kaiser D, Dunne M, Malchiodi C, Feen H, Howie P, Cutcher D, Ault R. Call for art therapy research on treatment of PTSD. Alexandria, VA: American Art Therapy Association; 2005. Retrieved from http://www.americanarttherapyassociation.org/upload/callforresearchptsd.pdf. [Google Scholar]
- Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: A population-based survey of 30,000 veterans. American Journal of Epidemiology. 2003;157(2):141–148. doi: 10.1093/aje/kwf187. [DOI] [PubMed] [Google Scholar]
- Kopytin A, Lebedev A. Humor, self-attitude, emotions, and cognitions in group art therapy with war veterans. Art Therapy: Journal of the American Art Therapy Association. 2013;30(1):20–29. doi: 10.1080/07421656.2013.757758. [DOI] [Google Scholar]
- Langer R. Combat trauma, memory and the World War II veteran. War, Literature, and the Arts: An International Journal of the Humanities. 2011;23(1):50–58. [Google Scholar]
- Lyshak-Stelzer F, Singer P, St John P, Chemtob CM. Art therapy for adolescents with posttraumatic stress disorder symptoms: A pilot study. Art Therapy: Journal of the American Art Therapy Association. 2007;24(4):163–169. doi: 10.1080/07421656.2007.10129474. [DOI] [Google Scholar]
- Macdonald A, Monson CM, Doron-Lamarca S, Resick PA, Palfai TP. Identifying patterns of symptom change during a randomized controlled trial of cognitive processing therapy for military-related posttraumatic stress disorder. Journal of Traumatic Stress. 2011;24(3):268–276. doi: 10.1002/jts.20642. [DOI] [PubMed] [Google Scholar]
- Morgan CA, Johnson DR. Use of a drawing task in the treatment of nightmares in combat-related post-traumatic stress disorder. Art Therapy: Journal of the American Art Therapy Association. 1995;12:244–247. [Google Scholar]
- Naff K. A framework for treating cumulative trauma with art therapy. Art Therapy: Journal of the American Art Therapy Association. 2014;31(2):79–86. doi: 10.1080/07421656.2014.903824. [DOI] [Google Scholar]
- Nishith P, Nixon RDV, Resick PA. Resolution of trauma-related guilt following treatment of PTSD in female rape victims: A result of cognitive processing therapy targeting comorbid depression? Journal of Affective Disorders. 2005;86:259–265. doi: 10.1016/j.jad.2005.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, Hamblen JL. Standardized self-report measures of civilian trauma and PTSD. In: Wilson JP, Keane TM, Martin T, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 2004. pp. 63–102. [Google Scholar]
- Pietrzak RH, Tsai J, Harpaz-Rotem I, Whealin JM, Southwick SM. Support for a novel five-factor model of posttraumatic stress symptoms in three independent samples of Iraq/Afghanistan veterans: A confirmatory factor analytic study. Journal of Psychiatric Research. 2012;46(3):317–22. doi: 10.1016/j.jpsychires.2011.11.013. [DOI] [PubMed] [Google Scholar]
- Pifalo T. Jogging the cogs: Trauma-focused art therapy and cognitive behavioral therapy with sexually abused children. Journal of the American Art Therapy Association. 2007;24(4):170–175. doi: 10.1080/07421656.2007.10129471. [DOI] [Google Scholar]
- Pifalo T. Mapping the maze: An art therapy intervention following disclosure of sexual abuse. Art Therapy: Journal of the American Art Therapy Association. 2009;26(1):12–18. doi: 10.1080/07421656.2009.10129313. [DOI] [Google Scholar]
- Ponniah K, Hollon SD. Empirically supported psychological treatments for adult acute stress disorder and post-traumatic stress disorder: A review. Depression and Anxiety. 2009;26:1086–1109. doi: 10.1002/da.20635. [DOI] [PubMed] [Google Scholar]
- Price JL. Findings from the National Vietnam Veterans’ Readjustment Study. 2016 Retrieved from National Center for PTSD website: http://www.ptsd.va.gov/professional/research-bio/research/vietnam-vets-study.asp.
- Rankin AB, Taucher LC. A task-oriented approach to art therapy in trauma treatment. Art Therapy: Journal of the American Art Therapy Association. 2003;20(3):138–147. doi: 10.1080/07421656.2003.10129570. [DOI] [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive Processing Therapy: Veteran/military version manual. Washington, DC: Department of Veterans Affairs; 2008. [Google Scholar]
- Riggs DS, Sermanian D. Prevention and care of combat-related PTSD: Directions for future explorations. Military Medicine. 2012;177(8):14–20. doi: 10.7205/MILMED-D-12-00140. [DOI] [PubMed] [Google Scholar]
- Sarid O, Huss E. Trauma and acute stress disorder: A comparison between cognitive behavioral intervention and art therapy. The Arts in Psychotherapy. 2010;37:8–12. doi: 10.1016/j.aip.2009.11.004. [DOI] [Google Scholar]
- Spiegel D, Malchiodi C, Backos A, Collie K. Art therapy for combat-related PTSD: Recommendations for research and practice. Art Therapy: Journal of the American Art Therapy Association. 2006;23(4):157–164. doi: 10.1080/07421656.2006.10129335. [DOI] [Google Scholar]
- Talwar S. Accessing traumatic memory through art making: An art therapy trauma protocol (ATTP) The Arts in Psychotherapy. 2007;34:22–25. doi: 10.1016/j.aip.2006.09.001. [DOI] [Google Scholar]
- Tinnin LW, Bills L, Gantt LM. Short-term treatment of simple and complex PTSD. In: Williams MB, Sommer JF Jr, editors. Simple and complex post-traumatic stress disorder: Strategies for comprehensive treatment in clinical practice. New York, NY: The Haworth Press; 2002. pp. 99–118. [Google Scholar]
- Tripp T. A short term therapy approach to processing trauma: Art therapy and bilateral stimulation. Journal of the American Art Therapy Association. 2007;24(4):176–183. doi: 10.1080/07421656.2007.10129476. [DOI] [Google Scholar]
- U.S. Department of Veterans Affairs. Report on VA Facility Specific Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) Veterans Diagnosed with Potential or Provisional PTSD. 2015 Retrieved from: http://www.publichealth.va.gov/docs/epidemiology/ptsd-report-fy2015-qtr2.pdf.
- van der Kolk BA, Najavits LM. Interview: What is PTSD really? Surprises, twists of history, and the politics of diagnosis and treatment. Journal of Clinical Psychology. 2013;69(5):516–22. doi: 10.1002/jclp.21992. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman D, Huska J, Keane T. The PTSD Checklist: Reliability, validity and diagnostic utility. Paper presented at the Annual Meeting of the International Society of Traumatic Stress Studies; San Antonio, TX. 1993. Oct, [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD checklist for DSM-5 (PCL-5) 2013 Retrieved from National Center for PTSD website: http://www.ptsd.va.gov/professional/pages/assessments/ptsd-checklist.asp.
- Wisco BE, Marx BP, Keane TM. Screening, diagnosis, and treatment of post-traumatic stress disorder. Military Medicine. 2012;177(8):7–13. doi: 10.7205/MILMED-D-12-00111. [DOI] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, Sloan DM, Gorman KR, Kulish AL, Pineles SL. Self-distancing from trauma memories reduces physiological but not subjective emotional reactivity among veterans with posttraumatic stress disorder. Clinical Psychological Science. 2015;3(6):956–963. doi: 10.1177/2167702614560745. [DOI] [PMC free article] [PubMed] [Google Scholar]