Abstract
In poultry several Chlamydia species have been detected, but Chlamydia psittaci and Chlamydia gallinacea appear to be most prevalent and important. Chlamydia psittaci is a well-known zoonosis and is considered to be a pathogen of poultry. Chlamydia gallinacea has been described more recently. Its avian pathogenicity and zoonotic potential have to be further elucidated. Within the Netherlands no data were available on the presence of Chlamydia on poultry farms. As part of a surveillance programme for zoonotic pathogens in farm animals, we investigated pooled faecal samples from 151 randomly selected layer farms. On a voluntary base, 69 farmers, family members or farm workers from these 151 farms submitted a throat swab. All samples were tested with a generic 23S Chlamydiaceae PCR followed by a species specific PCR for C. avium, C. gallinacea and C. psittaci. C. avium and psittaci DNA was not detected at any of the farms. At 71 farms the positive result could be confirmed as C. gallinacea. Variables significantly associated with the presence of C. gallinacea in a final multivariable model were ‘age of hens,’ ‘use of bedding material’ and ‘the presence of horses.’ The presence of C. gallinacea was associated with neither clinical signs, varying from respiratory symptoms, nasal and ocular discharges to diarrhoea, nor with a higher mortality rate the day before the visit. All throat swabs from farmers, family members or farm workers tested negative for Chlamydia DNA, giving no further indication for possible bird-to-human (or human-to-bird) transmission.
Introduction
Chlamydia avium, Chlamydia gallinacea and Chlamydia psittaci belong to the family of Chlamydiaceae, a group of obligate intracellular bacteria. Chlamyia psittaci is widespread and can infect over 465 bird species and several mammalian species, including humans [1]. Pathogenicity in animals depends on host species and C. psittaci strain. Clinical symptoms in birds vary from asymptomatic to acute death. Chlamydia psittaci is a well-known zoonosis and the cause of psittacosis. Transmission from birds to humans occurs via aerosolised respiratory or faecal excretions. In the Netherlands, psittacosis is notifiable in humans and pet birds but not in poultry. In poultry, chickens appeared to be less sensitive to chlamydial infection and a sporadic source of human infection [1–3]. However, in recent publications C. psittaci is regularly detected and chicken-to-human transmission is more frequently described [4–6].
Chlamydia avium and C. gallinacea have been detected in pet birds and poultry since 2009, first being classified as “atypical” and in 2014 added as new members of the genus Chlamydia [7–9]. Chlamydia avium has been found in psittacines and pigeons, C. gallinacea in chickens, guinea fowl and turkeys [10]. Recent studies hypothesised C. gallinacea to be endemic in chickens causing only mild clinical signs such as reduced weight gain in broilers [11]. Its zoonotic potential was suggested, but conclusive evidence has not been presented yet [8].
The impact of transmission of zoonotic pathogens from farm animals to humans was highlighted by the Dutch Q fever outbreak (2007–2010). Due to this outbreak, studies were initiated to assess the public health risks of intensive farming in densely populated areas [12]. One of the findings was a higher incidence of human pneumonia cases in the direct proximity of poultry farms [13, 14]. The cause of this higher incidence was unknown. We therefore hypothesised that C. psittaci or C. gallinacea could play a role. However, no data were available on the presence of C. psittaci and C gallinacea on Dutch poultry farms.
We investigated 755 faecal samples from 151 layer farms for the presence of Chlamydiacea DNA. Per farm a questionnaire was completed to identify possible risk factors. To gather information on possible bird to human transmission, farmers, family members or farm workers were invited to participate on a voluntary basis in throat swab sampling.
Materials and methods
Sampling strategy
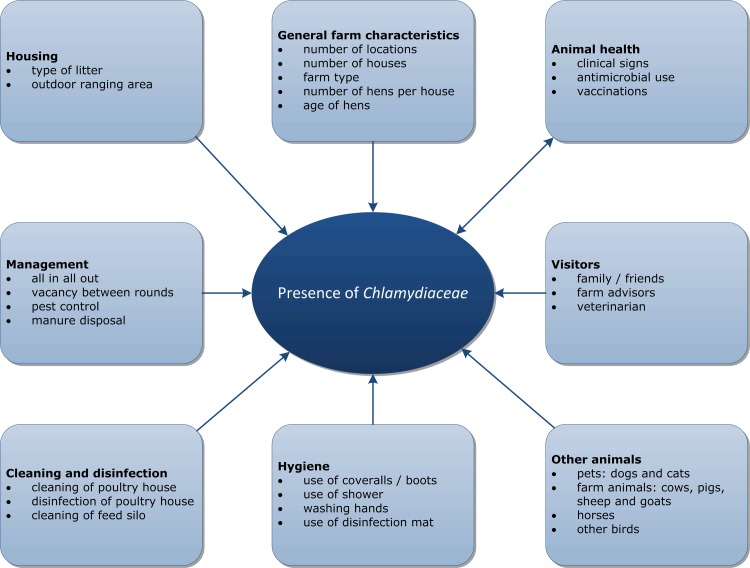
Between March 2015 and January 2016, a cross-sectional study on layer farms was performed as part of a surveillance programme for zoonotic pathogens in farm animals. From the 993 layer farms in the Netherlands, 154 farms were randomly selected stratified on farming system (conventional n = 79, free range n = 34, organic n = 22, enriched cages n = 8, enriched colony n = 6). Finally, 151 farms completed a questionnaire and were included in the analysis. For Chlamydia testing, five pooled faecal samples were collected from one barn per farm, resulting in 755 samples. Each pooled sample contained twelve scoops of fresh faeces. Additional information on farm characteristics, husbandry practices, biosecurity measures, clinical history and antibiotic usage was acquired via a questionnaire (Fig 1). Farmers, family members and farm workers were asked to participate in the poultry-to-human transmission study by submitting two throat swabs (collected through self-sampling) for Chlamydia testing. In total 69 farmers, family members or farm workers from 41 farms participated in the study.
Fig 1. Overview of risk factors.
Overview of possible risk factors for the presence of Chlamydiaceae on which information was gathered via a questionnaire.
Ethics statement
The Medical Ethics Review Committee (Utrecht Medical Centre, Utrecht) stated that the Medical Research Involving Human Subjects Act (WMO) does not apply to this study and therefore no official approval for the study is required under the WMO. All volunteers gave their written consent for participation in the study.
Laboratory tests
DNA isolation of all pooled faecal samples was performed with a NucliSENS® easyMAG® (Biomerieux, Zaltbommel, the Netherlands). In brief, faecal material was taken from each sample with a dry swab, suspended in 1.5 ml Phosphate Buffered Saline (PBS) and thoroughly vortexed. From this suspension, 500 μl was added to 2 ml NucliSENS® lysis buffer for off-board lysis. After at least one hour of incubation at room temperature, the lysis buffer was added to 80 μl of silica and extracted according to manufacturer instructions for specific protocol B. Within this protocol an optimised washing protocol is used with extra and longer washing steps. The final elution volume was 100 μl. DNA isolation of human throat swabs was performed with a MagNA Pure® LC (Roche Diagnostics, Almere, The Netherlands) according to manufacturer instructions for off-board lysis. Of the sample 200 μl was processed to a final elution volume of 50 μl. Chlamydiaceae-DNA was detected using a generic PCR that targeted the 23S rRNA gene with primers and probes according to Ehricht et al [15]. Chlamydia psittaci DNA was detected using a PCR that targeted the ompA gene with primers and probes according to Pantchev et al [16]. For C. avium and C. gallinacea a duplex PCR was used targeting the enoA gene. For C. avium primer and probe sequences were used according to Zocevic et al [9]. For C. gallinacea primer and probe sequences were used according to Laroucau et al [6]. To validate the C. avium and C. gallinacea duplex PCR, 10-fold serial dilutions (single and in a mixture) of C. gallinacea strain 14DC0101 and C. avium strain 10DC97 were tested. The duplex PCR appeared to be as sensitive as the single PCR. No differences in Ct values were observed when C. avium and C. gallinacea were added in a single dilution or as a mixture. The final volume of the reaction mixture was 20 μl, including 5 μl of the DNA template, 10 μl TaqMan® Fast Universal PCR Master Mix (Applied Biosystems, Fisher Scientific, Landsmeer, the Netherlands), 1 μM of each primer, 0.2 μM of the probes, 0.2 μl UDG (5U/μl) and distilled PCR water to reach the final volume. Amplification was carried out in an ABI 7500 Fast Real-Time PCR system (Applied Biosystems, Fisher Scientific, Landsmeer, the Netherlands) using the following cycling parameters: 5 min at 37°C, 20 sec at 95°C, 50 cycles of 95°C for 3 sec and 60°C for 30 sec. As a control for DNA extraction, a known C. psittaci positive faecal swab was used. In each 23S and C. psittaci PCR run a dilution series of three C. psittaci DNA isolates was used as positive controls. In the C. gallinacea and C. avium duplex PCR, DNA from C. gallinacea strain 14DC0101 and C. avium 10DC97 and a mix of both strains were used as positive controls. Each real-time PCR run included a non-template control using 5 μl distilled water as template, and during the extraction per 12 samples a negative sample with 1.5 ml PBS was added. Samples with a Ct value up to 40 were considered positive and samples with a Ct value above 40 were considered negative. Farms were considered positive if at least one of five samples tested positive in the PCR.
GIS map
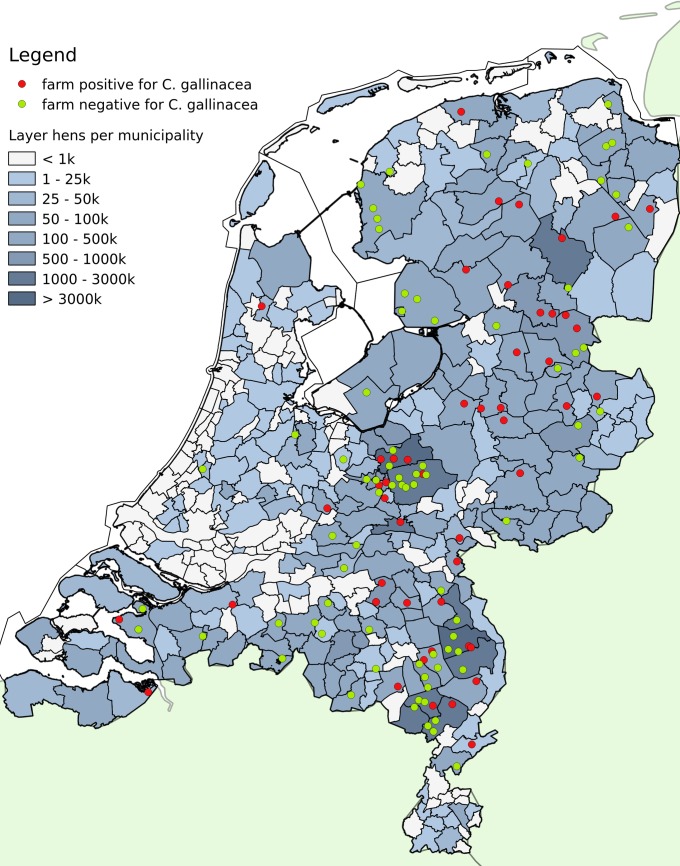
Chlamydia gallinacea positive and negative farms were plotted on a laying hen density map of the Netherlands (Fig 2). Data were extracted from CBS Statline (http://statline.cbs.nl) and imported into QGIS version 2.18.
Fig 2. Map with C. gallinacea positive and negative farms.
Chlamydia gallinacea positive and negative farms plotted on a laying hen density map of the Netherlands.
Statistical analyses
Farm prevalence was determined with an exact (Clopper-Pearson) 95 percent confidence interval (epitools.ausvet.com.au). Data from the questionnaires were collected via a digital form in Epi InfoTM and analysed using IBM SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, N.Y., USA). Overlapping variables or small categories were merged or summarised when possible. Potential risk factors for the presence of C. gallinacea were initially examined with a univariable analysis using a Chi square test or a logistic regression for continuous variables. Variables associated (p ≤ 0.20) with the outcome of interest (presence of C. gallinacea) were considered for inclusion in a stepwise, backward, multiple logistic regression analysis. The selected variables for the multivariable analysis were tested for mutual correlation. A likelihood ratio test was performed to eliminate variables from the multivariable model. Variables had to be significant (p ≤ 0.05) to remain in the final model. The goodness of fit of the final model was tested using the Hosmer and Lemeshow test.
Results
Chlamydiaceae DNA was detected on 74 of the 151 farms and confirmed as C. gallinacea on 71 farms (farm prevalence 47%, 95% CI: 39–55%). Neither C. psittaci DNA nor C. avium DNA was detected in any of the samples from the 151 farms. The distribution of the number of positive samples per farm in the 23S Chlamydiaceae PCR and the C. gallinacea PCR is shown in Table 1. On 31 farms all five samples were positive in both the Chlamydiaceae PCR and C. gallinacea PCR, whereas on 67 farms all five samples were negative in both the Chlamydiaceae PCR and C. gallinacea PCR. At seven farms no Chlamydiaceae DNA was detected, but per farm one or two samples tested positive for C. gallinacea DNA with Ct values above 36. The 71 farms that had one or more positive samples in both the Chlamydiaceae PCR and the C. gallinacea PCR were included in the risk factor analysis.
Table 1. The distribution of the number of positive samples per farm in the Chlamydiaceae and C. gallinacea PCR.
| Number of positive samples per farm in C. gallinacea PCR (n = 5 per farm) | ||||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | total | ||
| Number of positive samples per farm in Chlamydiaceae PCR (n = 5 per farm) | 0 | 67 | 6 | 1 | 0 | 0 | 0 | 74 |
| 1 | 2 | 6 | 1 | 1 | 0 | 0 | 10 | |
| 2 | 2 | 3 | 1 | 2 | 2 | 0 | 11 | |
| 3 | 0 | 2 | 1 | 3 | 0 | 1 | 7 | |
| 4 | 0 | 0 | 2 | 1 | 3 | 1 | 6 | |
| 5 | 0 | 0 | 0 | 1 | 3 | 30 | 34 | |
| total | 71 | 17 | 6 | 8 | 8 | 32 | 142* | |
* The results of 142 farms are shown. From seven farms one or more samples showed inhibition. From two farms only four samples could be tested. The results of these nine farms are not shown in the table, but the farm level results were used in the analysis.
The location of the positive and negative farms is shown in Fig 2. Chlamydia gallinacea positive and negative farms appear to be equally distributed in the Netherlands.
General descriptors about farm type and the median farm size are shown in Table 2. Farm type is related to farm size. Farms with enriched cages and colony systems are larger than free range and organic farms. Due to the relation with farm type, farm size was excluded from the analysis. Background and coding information on the variables in the univariable and multivariable analyses are added in the S1 and S2 Files. For the variables ‘age of hens’ and ‘manure disposal’ the smallest categories were merged. From the variable ‘vacancy period’ (period between two flocks, when the barn is empty), outliers with a vacancy period above 90 days were excluded from the analysis.
Table 2. General descriptors of farm type and farm size.
| Farm type | Number of farms | % of participating farms | Median farm size (range) |
|---|---|---|---|
| Conventional (Barn egg) | 79 | 52.3 | 33,696 (1,000–239,000) |
| Free range | 34 | 22.8 | 24,410 (900–117,000) |
| Enriched cages | 8 | 5.3 | 97,693 (648–180,000) |
| Enriched colony system | 6 | 3.9 | 182,600 (66,000–383,000) |
| Organic | 22 | 14.5 | 11850 (500–32,800) |
| Missing information | 2 | 1.3 | n.a. |
| Total | 151 | 100 | 28,750 (500–383,000) |
In the univariable analysis, ten variables met the criteria of p ≤ 0.2, i.e. ‘age of hens’, ‘use of bedding material’, ‘presence of horses’, ‘frequency of manure disposal’, ‘visitors have to shower before entrance’, ‘other birds’, ‘free range’, ‘vaccination against Pasteurella multocida’ or ‘Egg Drop Syndrome’ and ‘vacancy period’ (Table 3). No mutual correlations were found between these ten variables and they were all included in the multivariable analysis. No associations were found between the presence of C. gallinacea and ‘one or more locations’, ‘more than one poultry house’, ‘all in all out at farm level’, ‘fly control’, ‘visitors’, ‘disinfection method’, ‘frequency of cleaning of the feed silo’, ‘washing hands before entrance’ and the ‘presence of other farm animals or pets’. All farms reported that they controlled rats and mice. The variables ‘use of disinfection mat before entrance’ and ‘use of tools in one or more houses’ were not included in the analysis, due to inconsistent answers in the questionnaires.
Table 3. Variables from the univariable analysis with p ≤ 0.2 (ranked by p-value).
| Variable | No. of infected farms n = 71* (%) | No. of non-infected farms n = 80 (%) | Odds Ratio (CI 95%) | p-value (Chi square) |
|---|---|---|---|---|
| Age of hens# | < 0.01 | |||
| till 40 weeks | 15/70 (21.4) | 32/77 (41.6) | Ref | Ref |
| 40–60 weeks | 28/70 (40.0) | 13/77 (16.9) | 4.6 (1.87–11.29) | < 0.01 |
| older than 60 weeks | 27/70 (38.6) | 32/77 (41.6) | 1.80 (0.81–4.00) | 0.15 |
| Use of bedding material | 64/69 (92.8) | 60/80 (75.0) | 4.27 (1.51–12.09) | <0.01 |
| Horses present | 26/71 (36.6) | 14/80 (17.5) | 2.72 (1.28–5.78) | <0.01 |
| Manure disposal# | 0.08 | |||
| once or less than once a week | 6/70 (8.6) | 18/77 (23.4) | Ref | Ref |
| once every two weeks | 21/70 (29.6) | 14/77 (18.3) | 4.50 (1.43–14.14) | 0.10 |
| once a month | 17/70 (23.9) | 18/77 (23.4) | 2.83 (0.91–8.83) | 0.07 |
| less than once a month | 26/70 (38.0) | 27/77 (35.1) | 8.89 (0.99–8.4) | 0.05 |
| Use of shower before entrance (visitors) | 6/71 (8.5) | 14/80 (17.5) | 0.44 (0.16–1.16) | 0.10 |
| Other birds presenti | 5/71 (7.0) | 1/80 (1.3) | 5.99 (0.68–52.5) | 0.10 |
| Vaccination against Pasteurella multocidai | 8/71 (11.3) | 3/80 (3.8) | 3.26 (0.83–12.80) | 0.12 |
| Vacancy periodii | / | 0.14 | ||
| Vaccination against Egg Drop Syndrome | 41/71 (57.7) | 37/80 (46.3) | 1.59 (0.83–3.02) | 0.16 |
| Free range sampled house | 39/69 (42.0) | 25/80 (31.3) | 1.60 (0.81–3.12) | 0.17 |
*Due to missing values, the number of farms per variable can differ
#p-value was calculated with logistic regression
iFisher exact p-value was used (cells with counts n<5)
iicontinuous variable
In the multivariable analysis, three variables were significantly associated with the presence of C. gallinacea as shown in Table 4: ‘age of hens’, ‘use of bedding material’ and ‘presence of horses’. The final model met the criteria of the Hosmer-Lemeshow goodness of fit test.
Table 4. Results of multivariable analysis (ranked by p-value).
| Variable | Odds Ratio (CI 95%) | p-value |
|---|---|---|
| Age of hens | < 0.01 | |
| till 40 weeks | ref | ref |
| 40–60 weeks | 5.41 (2. 02–14.53) | < 0.01 |
| older than 60 weeks | 2.28 (0.94–5.53) | 0.07 |
| Use of bedding material | 4.22 (1.40–12.75) | 0.01 |
| Horses present | 2.67 (1.16–6.12) | 0.02 |
For the multivariable analysis 139 farms were selected, 12 had missing values for one or more of the selected variables.
No associations between the presence of C. gallinacea DNA and clinical signs, varying from respiratory symptoms and nasal and ocular discharges to diarrhoea, were found. The number of farms reporting clinical signs was low (n = 11). Also no association was found between the mortality rate the day before the visit and the presence of C. gallinacea. A total of 83 farms reported a mortality rate per day of < 0.01%, 58 a mortality rate between 0.01% and 0.05%, and 7 farms a mortality rate > 0.05% (3 farms did not report the mortality rate the day before the visit).
The 69 human throat swabs all tested negative in the Chlamydiaceae PCR. A total of 26 human samples were collected from farmers, family members or workers from 17 C. gallinacea DNA positive farms and 42 samples from 24 C. gallinacea DNA negative farms. One human sample could not be related to a sampled farm.
In summary, C. gallinacea DNA is highly prevalent on Dutch layer farms (farm prevalence 47%, 95% CI 39–55%), while neither C. psittaci DNA nor C. avium DNA were detected in any of the samples from the 151 farms. In the multivariable model, the presence of C. gallinacea appears to be associated with the ‘ age of hens’, ‘presence of horses’ and ‘use of bedding material’. No association was found with clinical signs or mortality rate the day before the visit. All of the 69 human throat swabs collected from farmers, family members or workers tested negative for Chlamydiaceae DNA.
Discussion
Our cross-sectional study shows that C. gallinacea DNA is present on 47% (95% CI 39–55%) of layer farms in the Netherlands. The high prevalence of C. gallinacea DNA is in agreement with publications that postulate C. gallinacea to be the most important Chlamydia spp in chickens [11, 17]. In 2012, Zocevic et al. detected mainly DNA of atypical Chlamydias (later redefined as C. gallinacea) in 95 of 283 samples from different poultry flocks from France, Greece, Slovenia, Croatia and China [9]. Guo et al. detected C. gallinacea DNA in about 20% (359/1791) of oral and cloacal swabs of chickens from different provinces in China [11]. Hulin et al. reported a predominance of C. gallinacea in a poultry slaughterhouse where mainly chickens were slaughtered; in 52 / 129 flocks one or more samples were PCR positive for C. gallinacea.
C. psittaci and C. avium DNA were not detected at any of the 151 farms (95% CI 0–2%). These results are in line with the findings of Guo et al., where 41 of 1791 (2.3%) chicken samples were PCR positive for C. psittaci [11], and with the study of Hulin et al. where only one of the 129 flocks (bird species not specified) from the chicken slaughterhouse was PCR positive [17]. In contrast, Lagae et al. PCR detected and cultured C. psittaci from individual pharynx swabs from 7/7 broiler, 5/5 layer and 6/7 broiler breeder farms in Belgium. Differences in sampling methods might play a role. It has been shown that pharyngeal swabs are a more sensitive sampling method than cloacal swabs or faecal samples for the detection of C. psittaci [18]. Culturing, however has proven to be a less sensitive detection method than PCR, so this might not fully explain the large difference in prevalence [19]. The prevalence of C. psittaci might differ between countries. The absence of C. avium was expected. So far, this bacterium has only been found in psittacines and pigeons and not in poultry [7].
In the risk factor analysis ‘ age of hens’, ‘use of bedding material’ and ‘presence of horses’ were associated with the presence of C. gallinacea. The age related risk for the presence of C. gallinacea peaks between 40 and 60 weeks (OR 5.41, p < 0.01). Factors that might influence this risk are the moment of introduction, the duration of C. gallinacea infections and the acquisition of immunity. However, this information is currently not available for C. gallinacea infections. Studies with a more longitudinal approach are therefore needed. The association with the ‘use of bedding material’ might be explained by the introduction of the bacterium via bedding material or the effect of this material on the persistence of the bacterium in the environment. It has been reported that the elementary bodies of other Chlamydiaceae can survive in litter for several months [20]. There is no obvious explanation for the association with the ‘presence of horses’. Several Chlamydia species have been detected in horses, but the presence of C. gallinacea has not been described [21]. However, C. gallinacea has been detected in vaginal swabs from cattle in China suggesting it might not be restricted to poultry [22]. There might be other associated factors as well, such as frequent movement of trailers, which explains the association with horses. More detailed studies are needed to confirm the relation between the risk factors in the final model and the presence of C. gallinacea DNA.
We did not observe an association between the presence of C. gallinacea and ‘clinical signs’, based on the results of the questionnaire. It should be noted that only 11 farms reported overt clinical problems, which varied from respiratory symptoms and nasal and ocular discharges to diarrhoea. Also no association was found with the mortality rate the day before the visit. An association with increased mortality cannot be excluded, because the mortality rate might have increased earlier in the infection and subsequently returned to a normal level. To study this we should have analysed for a period longer than 1 day before the visit. Furthermore, a possible clinical outcome of a C. gallinacea infection could be more subtle or subclinical. For example Guo et al. did not report any clinical signs, but did find a reduction in growth of broiler chicks [11]. Reinhold et al. discussed the role of Chlamydiaceae in cattle and suggested subclinical and chronic chlamydial infections might be economically more important than a clinical outbreak [20]. Further studies should also take into account subclinical or more economically important parameters, such as egg production during the entire production round.
All human samples collected tested negative for Chlamydiacea DNA. Participants were not selected for clinical signs and 26 were working or living at a C. gallinacea positive farm. A positive sample would have given an indication of possible bird-to-human (or human-to-bird) transmission. To date C. gallinacea has only been suggested as a cause of human pneumonia [8], but in our study we could not confirm this. Sputum or bronchoalveolar lavage fluid (BAL) from patients with community acquired pneumonia (CAP) should be examined to further investigate whether C. gallinacea could be a cause of human pneumonia.
Our study adds to the hypothesis that C. gallinacea is the endemic Chlamydia of chickens. However, many questions still need to be answered. The most important of these is to elucidate the zoonotic potential of C. gallinacea and to investigate the pathogenesis of a C. gallinacea infection, as these could be of economic significance for the poultry sector.
Supporting information
This file holds data on the variables used in the univariable and multivariable analysis.
(XLSX)
This file holds information on the coding of the variables.
(HTM)
Acknowledgments
The authors thank Christiane Schnee from the FLI in Jena, Germany for providing strains of C. avium (12DC97) and C. gallinacea (14DC0101 and 08DC00063). The authors acknowledge Herma Buys and Evelien Kern-van Nes of the WBVR diagnostic lab for their assistance in the DNA isolation of the faecal samples from the layers and Pieter Overduin from the National Institute for Public Health and the Environment for the DNA isolation of the human throat swabs.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was partly financed by the Food and Consumer Product Safety Authority (NVWA) and partly as a public-private-partnership: “1H4F-Chlamydia and respiratory problems in poultry” (TKI-AF-14212, http://www.1health4food.nl/nl/show/Chlamydia-en-respiratoire-problemen-in-pluimvee-.htm).
References
- 1.Kaleta EF, Taday EM. Avian host range of Chlamydophila spp. based on isolation, antigen detection and serology. Avian pathology: journal of the WVPA. 2003;32(5):435–61. Epub 2003/10/03. doi: 10.1080/03079450310001593613 . [DOI] [PubMed] [Google Scholar]
- 2.Suwa T, Ando S, Hashimoto N, Itakura C. Pathology of experimental chlamydiosis in chicks. Nihon juigaku zasshi The Japanese journal of veterinary science. 1990;52(2):275–83. Epub 1990/04/01. . [DOI] [PubMed] [Google Scholar]
- 3.Salisch H VMK, Ryll M, Hinz K-H. Chlamydial infections of poultry and human health. World's Poultry Science Journal. 1996;52(3):279–308. https://doi.org/10.1079/WPS19960021. [Google Scholar]
- 4.Lagae S, Kalmar I, Laroucau K, Vorimore F, Vanrompay D. Emerging Chlamydia psittaci infections in chickens and examination of transmission to humans. Journal of medical microbiology. 2014;63(Pt 3):399–407. Epub 2013/12/11. doi: 10.1099/jmm.0.064675-0 . [DOI] [PubMed] [Google Scholar]
- 5.Yin L, Kalmar ID, Lagae S, Vandendriessche S, Vanderhaeghen W, Butaye P, et al. Emerging Chlamydia psittaci infections in the chicken industry and pathology of Chlamydia psittaci genotype B and D strains in specific pathogen free chickens. Veterinary microbiology. 2013;162(2–4):740–9. Epub 2012/10/27. doi: 10.1016/j.vetmic.2012.09.026 . [DOI] [PubMed] [Google Scholar]
- 6.Laroucau K, Aaziz R, Meurice L, Servas V, Chossat I, Royer H, et al. Outbreak of psittacosis in a group of women exposed to Chlamydia psittaci-infected chickens. Euro surveillance: bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin. 2015;20(24). Epub 2015/06/26. . [DOI] [PubMed] [Google Scholar]
- 7.Sachse K, Laroucau K, Riege K, Wehner S, Dilcher M, Creasy HH, et al. Evidence for the existence of two new members of the family Chlamydiaceae and proposal of Chlamydia avium sp. nov. and Chlamydia gallinacea sp. nov. Systematic and applied microbiology. 2014;37(2):79–88. Epub 2014/01/28. doi: 10.1016/j.syapm.2013.12.004 . [DOI] [PubMed] [Google Scholar]
- 8.Laroucau K, Vorimore F, Aaziz R, Berndt A, Schubert E, Sachse K. Isolation of a new chlamydial agent from infected domestic poultry coincided with cases of atypical pneumonia among slaughterhouse workers in France. Infection, genetics and evolution: journal of molecular epidemiology and evolutionary genetics in infectious diseases. 2009;9(6):1240–7. Epub 2009/09/01. doi: 10.1016/j.meegid.2009.08.005 . [DOI] [PubMed] [Google Scholar]
- 9.Zocevic A, Vorimore F, Vicari N, Gasparini J, Jacquin L, Sachse K, et al. A real-time PCR assay for the detection of atypical strains of Chlamydiaceae from pigeons. PloS one. 2013;8(3):e58741 Epub 2013/03/22. doi: 10.1371/journal.pone.0058741 ; PubMed Central PMCID: PMC3597529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sachse K, Laroucau K, Vanrompay D. Avian Chlamydiosis. Current Clinical Microbiology Reports. 2015;2(1):10–21. doi: 10.1007/s40588-014-0010-y [Google Scholar]
- 11.Guo W, Li J, Kaltenboeck B, Gong J, Fan W, Wang C. Chlamydia gallinacea, not C. psittaci, is the endemic chlamydial species in chicken (Gallus gallus). Scientific reports. 2016;6:19638 Epub 2016/01/19. doi: 10.1038/srep19638 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roest HI, Tilburg JJ, van der Hoek W, Vellema P, van Zijderveld FG, Klaassen CH, et al. The Q fever epidemic in The Netherlands: history, onset, response and reflection. Epidemiology and infection. 2011;139(1):1–12. Epub 2010/10/06. doi: 10.1017/S0950268810002268 . [DOI] [PubMed] [Google Scholar]
- 13.Smit LA, van der Sman-de Beer F, Opstal-van Winden AW, Hooiveld M, Beekhuizen J, Wouters IM, et al. Q fever and pneumonia in an area with a high livestock density: a large population-based study. PloS one. 2012;7(6):e38843 Epub 2012/06/12. doi: 10.1371/journal.pone.0038843 ; PubMed Central PMCID: PMC3369851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freidl GS, Spruijt IT, Borlee F, Smit LA, van Gageldonk-Lafeber AB, Heederik DJ, et al. Livestock-associated risk factors for pneumonia in an area of intensive animal farming in the Netherlands. PloS one. 2017;12(3):e0174796 Epub 2017/04/01. doi: 10.1371/journal.pone.0174796 ; PubMed Central PMCID: PMC5376295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ehricht R, Slickers P, Goellner S, Hotzel H, Sachse K. Optimized DNA microarray assay allows detection and genotyping of single PCR-amplifiable target copies. Molecular and cellular probes. 2006;20(1):60–3. Epub 2005/12/07. doi: 10.1016/j.mcp.2005.09.003 . [DOI] [PubMed] [Google Scholar]
- 16.Pantchev A, Sting R, Bauerfeind R, Tyczka J, Sachse K. New real-time PCR tests for species-specific detection of Chlamydophila psittaci and Chlamydophila abortus from tissue samples. Veterinary journal. 2009;181(2):145–50. Epub 2008/04/17. doi: 10.1016/j.tvjl.2008.02.025 . [DOI] [PubMed] [Google Scholar]
- 17.Hulin V, Oger S, Vorimore F, Aaziz R, de Barbeyrac B, Berruchon J, et al. Host preference and zoonotic potential of Chlamydia psittaci and C. gallinacea in poultry. Pathogens and disease. 2015;73(1):1–11. Epub 2015/02/11. doi: 10.1093/femspd/ftv005 . [DOI] [PubMed] [Google Scholar]
- 18.Andersen AA. Comparison of pharyngeal, fecal, and cloacal samples for the isolation of Chlamydia psittaci from experimentally infected cockatiels and turkeys. Journal of veterinary diagnostic investigation: official publication of the American Association of Veterinary Laboratory Diagnosticians, Inc. 1996;8(4):448–50. Epub 1996/10/01. doi: 10.1177/104063879600800407 . [DOI] [PubMed] [Google Scholar]
- 19.Hewinson RG, Griffiths PC, Bevan BJ, Kirwan SE, Field ME, Woodward MJ, et al. Detection of Chlamydia psittaci DNA in avian clinical samples by polymerase chain reaction. Veterinary microbiology. 1997;54(2):155–66. Epub 1997/02/01. . [DOI] [PubMed] [Google Scholar]
- 20.Reinhold P, Sachse K, Kaltenboeck B. Chlamydiaceae in cattle: commensals, trigger organisms, or pathogens? Veterinary journal. 2011;189(3):257–67. Epub 2010/10/29. doi: 10.1016/j.tvjl.2010.09.003 . [DOI] [PubMed] [Google Scholar]
- 21.Pantchev A, Sting R, Bauerfeind R, Tyczka J, Sachse K. Detection of all Chlamydophila and Chlamydia spp. of veterinary interest using species-specific real-time PCR assays. Comparative immunology, microbiology and infectious diseases. 2010;33(6):473–84. Epub 2009/09/08. doi: 10.1016/j.cimid.2009.08.002 . [DOI] [PubMed] [Google Scholar]
- 22.Li J, Guo W, Kaltenboeck B, Sachse K, Yang Y, Lu G, et al. Chlamydia pecorum is the endemic intestinal species in cattle while C. gallinacea, C. psittaci and C. pneumoniae associate with sporadic systemic infection. Veterinary microbiology. 2016;193:93–9. Epub 2016/09/08. doi: 10.1016/j.vetmic.2016.08.008 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This file holds data on the variables used in the univariable and multivariable analysis.
(XLSX)
This file holds information on the coding of the variables.
(HTM)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.