Abstract
Background
Previous studies have discussed the liver stiffness measurement (LSM) performance on predicting liver-related surgical outcomes for patients of hepatocellular carcinoma (HCC) under hepatic resection, yet there is much variation in reporting and consistency of findings. Therefore, we report a meta-analysis on this issue.
Methods
We comprehensively searched PubMed, Embase, and Web of science to find the eligible cohort studies. The pooled Odds Ratios (OR) and 95% confidence intervals (CIs) were calculated to evaluate effect. The weighted mean LSM value was calculated as the optimal LSM cut-off value among studies.
Results
12 prospective cohort studies and one retrospective cohort study, including a total of 1942 cases were identified. The pooled results showed that preoperative LSM is significantly associated with the occurrence of overall postoperative complications (OR 1.76, 95% CI 1.46–2.11). In addition, a weighted mean LSM value of 14.2 kPa and 11.3KPa were suggested as the optimal LSM cut-off value reference using transient elastoqraphy (TE) for predicting overall postoperative complications in Asia countries and European countries, respectively.
Conclusions
Preoperative LSM should be taken into account cautiously in the management of patients undergoing hepatectomy of HCC. Future studies could focus on setting a prognostic model integrated with LSM in predicting post-hepatectomy outcomes.
Introduction
Hepatic resection is widely accepted as the major curative therapy for hepatocellular carcinoma (HCC), especially in patients with well-compensated cirrhosis[1]. Although advances have been made in perioperative care and surgical techniques, postoperative complications remain the main cause of unsatisfactory outcomes after resection of HCC[2]. Previous studies have identified cirrhosis or liver fibrosis as a negative factor contributing to liver decompensation and mortality after hepatectomy[3]. Hepatic resection may induce postoperative complications due to insufficient liver remnant volume. Therefore, careful preoperative assessment of liver reserve function is important for patient selection or the extent of liver resection to ensure the surgery safety.
The main conventional methods for preoperative assessment of liver function are Child-Pugh score, the model for end-stage liver disease score, and the use of Indocyanine green retention rate at 15 min[4]. Liver biopsy and hepatic venous pressure gradient can provide a more accurate evaluation but are invasive procedures.
Magnetic resonance elastography (MRE) and ultrasound elastography, including transient elastography (TE), shear wave elastography (SWE) and acoustic radio force impulse (ARFI) imaging technology have been reported as a noninvasive and convenient test to measure liver stiffness and distinguish the degree of liver fibrosis and cirrhosis to reflect objectively liver functional reserve[5, 6]. Some prospective cohort studies have indicated that preoperative liver stiffness measurement (LSM) is a valid tool for the prediction of post-hepatectomy liver failure (PHLF), hepatic liver insufficiency, and ascites in patients undergoing hepatic resection for HCC. Recent several meta-analyses had investigated that LSM was used for the assessment of liver fibrosis and cirrhosis degree, as well as the risk factor for liver decompensation, HCC, and death in patients with chronic liver diseases [7, 8]. However, to the best of our knowledge, no other study has examined its utility in surgical judgment. Therefore, we performed this meta-analysis to clarify further prognostic value of LSM for liver-related outcomes of patients after hepatic resection.
Methods
This meta-analysis was conducted following the guidance of Cochrane Handbook[9] and suggestions provided in the study by Singh S[10]. We also followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines[11].
Literature search strategy
We performed a systematic literature search in electronic databases of PubMed (January 1, 1966 through September 1, 2017), Embase (January 1, 1988 through September 1, 2017), and Web of science (January 1, 1993 through September 1, 2017) for articles published. The following key words and their combinations were searched in [Title/Abstract]: “liver,” “hepatic,” “stiffness,” “elastography,” “Fibroscan,” “hepatocellular carcinoma,” “prognosis,” “predict,” “resection,” “hepatectomy,” “operative,” and “surgical treatment.” Then, the major conferences (The Liver Meeting, organized by the American Association for the Study of the Liver; The International Liver Congress, organized by the European Association for the Study of the Liver; Digestive Diseases Week, organized in conjunction with the American Gastroenterological Association; and Congress of the International Hepato- Pancreato-Biliary Association) were searched manually for studies published in abstracts. In addition, the related-articles function was used to identify any potential studies missed by the electronic search. When the same population was described in two studies, the newly published or complete one was included. If necessary, we contacted the corresponding author to get further information. Two authors independently finished the literature search process (Zitong Huang and Jingjing Huang).
Selection criteria
All available prospective or retrospective cohort studies that met the following criteria were included: (1) LSM was performed preoperatively in patients undergoing hepatic resection; (2) correlation of LSM with liver-related surgical outcomes (postoperative complications including PHLF, ascites and hepatic insufficiency) were described; and (3) the studies reported a measure of association—odds ratio (OR), or the sufficient data for their calculation were provided. The included studies were not restricted by language and study size. Specific types of literature such as letters to the editor and review articles comments were excluded.
Quality assessment of studies
The quality assessment was independently preformed by two authors (Zitong Huang and Jingjing Huang), using the Newcastle–Ottawa Scale (NOS). Disagreements were resolved by consensus or by the third investigator (Tianran Zhou). This scale mainly comprises three quality parameters: patient selection, study comparability, and outcome assessment. Studies with NOS scores of ≥7 were regarded as high quality.
Data extraction
All data were abstracted by one investigator (Zitong Huang) and verified by another independent investigator (Jingjing Huang). Conflicts were resolved by consensus or by the third investigator (Tianran Zhou). Information taken from each study included primary author, year of publication, country, patient age and sex, study follow-up period, underlying liver diseases, stage of fibrosis, Child-Pugh score, development of liver-surgical outcomes and its definition, the corresponding OR with 95%CI, body mass index, technique of LSM, range of LSM value, cut-off value and its sensitivity and specificity of LSM for predicting outcomes, and methods of data analyses. Study authors were contacted to obtain pertinent data.
Definition
The primary end point was postoperative liver-related complications categorized by the modified Clavien–Dindo classification[12], including PHLF (defined according to the International Study Group of Liver Surgery definition or “50–50” criteria), hepatic ascites and insufficiency. Hepatic insufficiency was defined as persistent hyperbilirubinemia (total bilirubin level>5 mg/dl) for more than 5 days after surgery or postoperative death without other causes[13].
Statistical analysis
The pooled OR with its 95% CI was calculated to estimate the association of LSM and surgical treatment outcomes. The predictive ability of LSM was assessed by the receiver operating characteristic (ROC) curve and corresponding area under the ROC (AUROC) curve. To evaluate the optimal cut-off value of LSM, we used the method performed in the study by Chon YE[7]. Briefly, the cut-off value and sample size of individual study were calculated to make a weighted mean value as the optimal cut-off value of these studies. Heterogeneity among the studies was assessed by the Cochran’s Q statistic and I2 tests. Either P<0.10 or I2 statistic >50% defined significant heterogeneity among the studies. In this case, the random effects model was performed; otherwise, the fixed effects model was implemented. In order to explore potential sources of heterogeneity, subgroup analysis and meta-regression were conducted. We further performed sensitivity analysis by omitting some individual studies or low-quality studies. Stata software version 12.0 (College Station, TX, USA) was used to perform in the meta-analysis.
Results
Study selection
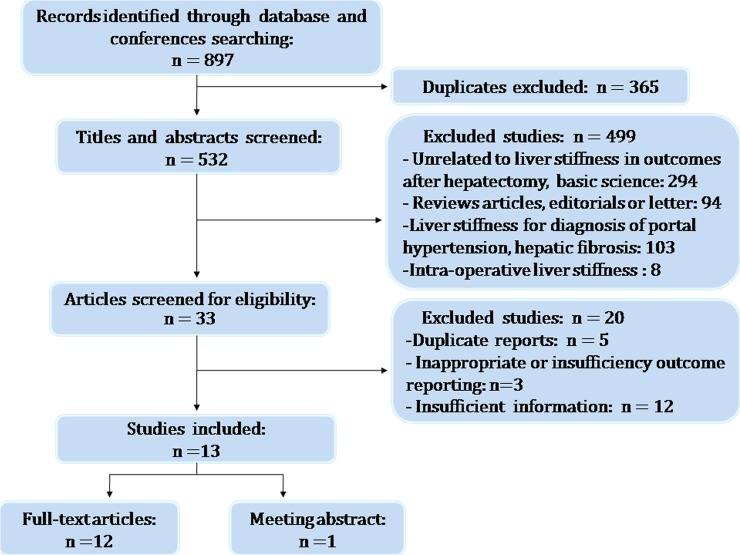
The initial search found a total of 897 articles. Following the exclusion of duplicate publications, 532 records were left. After screening the titles and abstracts, another 499 articles were excluded due to the following reasons: unrelated to liver stiffness in surgical outcome after hepatectomy, basis science(294), reviews articles, editorials or letter(94), LSM for diagnosis of portal hypertension(67) and hepatic fibrosis(36), intra-operative LSM(8). Another 20 articles were eliminated as the reporting outcomes were inappropriate or insufficiency and the data were insufficient or duplicated. Finally, 13 eligible studies were included in the present meta-analysis (Fig 1). The coefficient of agreement between the 2 investigators for study selection (Cohen’s K = 0.89; 95% CI, 0.78–0.99) was very good.
Fig 1. Flow diagram of the study selection process.
Characteristics of the included studies
Among these 13 cohort studies, 10 were in Asia and 3 were in a European country, Italy. 7 studies used TE for measurement of liver stiffness; two used SWE, MRE, and ARFI imaging technology, respectively. The LSM value in patients ranged from 2.5 kPa to 75 kPa. Patients with Child-Pugh C liver function were excluded from the study. The majority of patients included were Child–Pugh class A. All studies, except one, used the receiver operating characteristic (ROC) curve and corresponding area under the ROC (AUROC) curve to assess the predictive ability of LSM; one studies used decision curve analysis. The surgical end point of the 13 studies was postoperative complications. Among these studies, PHLF was specially reported in seven studies, postoperative complications in three studies, ascites in two studies, and hepatic insufficiency in one study. Most of included patients had viral hepatitis, and the others had other chronic liver diseases, including non-alcoholic steatohepatitis and alcohol liver disease. Two Asian studies were performed exclusively in patients with viral hepatitis B. All of the studies included a mix of patient population at varying stages of fibrosis or cirrhosis (defined based on liver biopsy or LSM). The main characteristics of the included studies are summarized in Tables 1 and 2. The coefficient of agreement between two investigators for data extraction (Cohen’s K = 0.86; 95% CI, 0.75–0.96) was excellent.
Table 1. The fundamental features of the included studies.
| Study |
Country | Case number |
Mean age (years) |
Gender (M/F) |
Time period |
Etiology | Outcomes |
LSM techniques |
NOS Value |
|---|---|---|---|---|---|---|---|---|---|
| Shen 2017[14] | China | 280 | 56.1 | 240/40 | 2015–2016 | HBV, 100% | PHLF | SWE | 6 |
| Han 2017[15] | China | 77 | 59 | 63/14 | 2014–2015 | HBV,89.6% Others,10.4% |
PHLF | SWE | 7 |
| Chong 2017[16] | China | 255 | 58.6 | 218/37 | 2010–2014 | HBV,81.6% HCV,6.7% Others,11.7% |
PHLF |
TE | 7 |
| Abe 2017[17] | Japan | 175 | 69 | 123/52 | 2014–2016 | HBC,19.4% HCV,23.6% Others,57.1% |
complications | MRE | 8 |
| Nishio 2016[18] | Japan | 177 | 68 | 140/37 | 2011–2014 | HBC,18.6% HCV,37.3% NASH,16.3% EtOH,13.0% Others,14.7% |
PHLF | ARFI | 7 |
| Lee 2016 [19] | China | 144 | 58.9 | 106/38 | 2010–2013 | HBV,80.5% HCV,11.1% EtOH,3.5% NBNC,3.5% Others,1.4% |
PHLF | MRE | 8 |
| Donadon 2016[20] | Italy | 240 | 65 | 225/115 | 2012–2015 | HBV,2% HCV,14% EtOH,9% Others,75% |
complications | TE | 6 |
| Cucchetti 2016[21] | Italy | 202 | 64 | 171/31 | 2008–2014 | HBV,17.8% HCV,63.9% Others,18.3% |
PHLF | TE | 8 |
| Li 2015[22] | China | 75 | 52.15 | 59/16 | 2012–2014 | HBV,100% | PHLF ascites |
TE | 7 |
| Wong 2013[23] | China | 105 | 59 | 82/23 | 2010–2011 | HBV,66.7% HCV,4.8% EtOH,1.9% NBNC,5.7% Others,21% |
complications |
TE | 8 |
| Harada 2012[24] | Japan | 50 | 68 | 36/14 | 2009–2010 | HBV,10% HCV,68% Others,22% |
ascites | ARFI | 8 |
| Cescon 2012[25] | Italy | 90 | 64 | 77/13 | 2008–2011 | HBV,17.8% HCV,65.6% Others,16.6% |
PHLF |
TE | 8 |
| Kim 2008[26] | Korea | 72 | 54.9 | 56/16 | 2006–2007 | HBV,83.3% HCV,12.5% Others,4.2% |
hepatic insufficiency | TE | 7 |
M/F, Male/female; LSM, liver stiffness measurement; PHLF, Post-hepatectomy Liver Failure; HBV, hepatitis B-virus; HCV, hepatitis C-virus; NOS, Newcastle–Ottawa Scale; TE, transient elastography; SWE, shear wave elastography; MRE, magnetic resonance elastography; ARFI, acoustic radio force impulse; ISGLS, International Study Group of Liver Surgery definition; EtOH, alcohol liver disease; NASH, non-alcoholic steatohepatitis; NBNC, non-hepatitis B and non-hepatitis C; NA, data not available.
Table 2. Diagnostic data of each studies evaluating the performance of TE for postoperative complications.
| Study | LSM cut-off value(KPa) |
Sensitivity (%) | Specificity (%) | BMI(Mean) | AUROC |
|---|---|---|---|---|---|
| Chong 2017 | 12 | 83 | 73 | 23.7 | 0.83 |
| Donadon 2016 | 9.7 | 88.9 | 67.3 | 25.1 | 0.728 |
| Li 2015 | 14.3 | 100 | 76.1 | NA | 0.915 |
| Wong 2013 | 12 | 85.7 | 71.8 | 23.2 | 0.79 |
| Cescon 2012 | 15.7 | 96.1 | 68.7 | 24.8 | 0.865 |
| Kim 2008 | 25.6 | 71.4 | 88.6 | 24.0 | 0.824 |
LSM, liver stiffness measurement; PHLF, Post-hepatectomy liver failure; BMI, body mass index; AUROC, area under the receiver operating characteristic curve; KPa, Kilopascal; NA, data not available.
Overall postoperative complications after hepatectomy
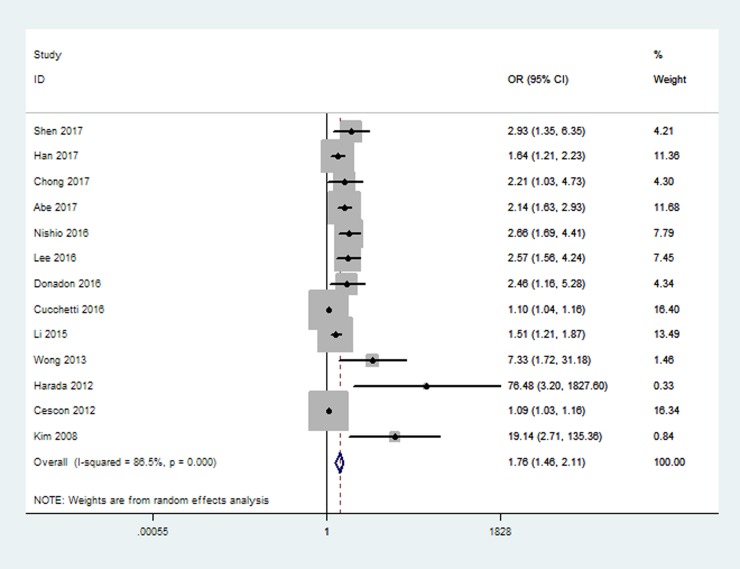
A total of 1942patients were included and analyzed for the prognostic significance of LSM for liver-related surgical outcomes. The relationship LSM and overall postoperative complications after hepatectomy was evaluated in 13 studies. The pooled results of the meta-analysis revealed that preoperative LSM was significantly associated with the development of overall postoperative complications (OR 1.76, 95% CI 1.46–2.11, Fig 2).
Fig 2. Forest plot on the associations between LSM and overall postoperative complications.
Optimal cut-off value of LSM using TE for overall postoperative complications
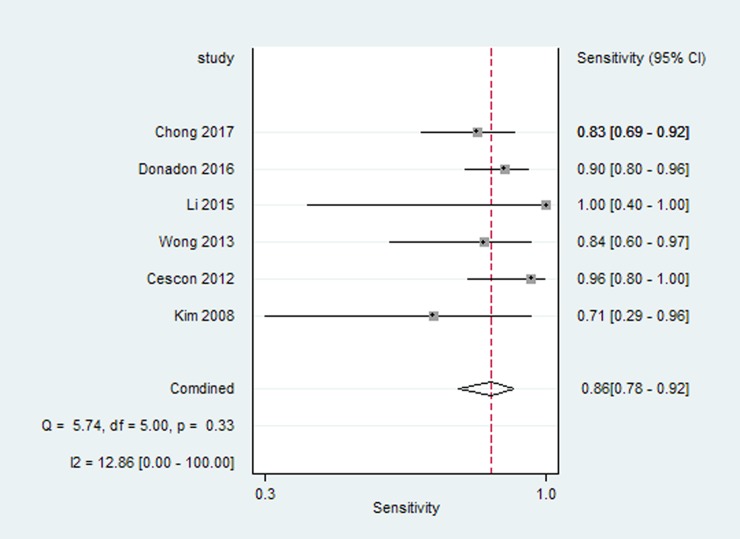
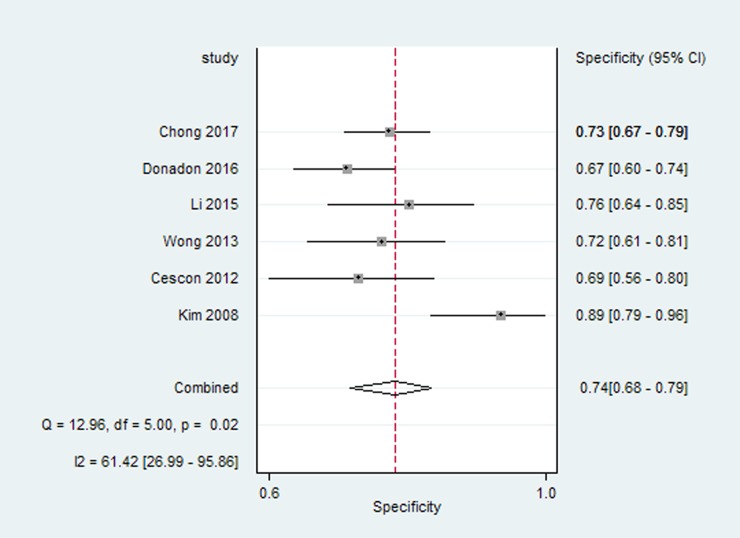
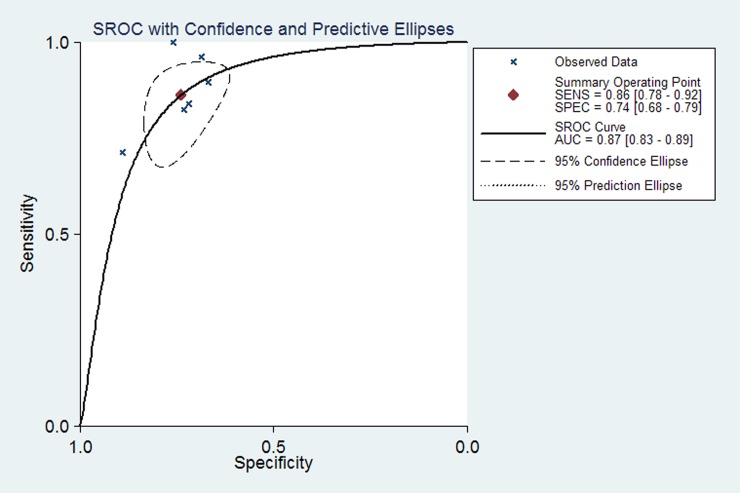
Six studies reported the preoperative LSM cut-off value using TE and diagnostic accuracy parameters (sensitivity, specificity and AUROC) for overall postoperative complications after hepatectomy. For the diagnosis of postoperative complications by TE, the pooled estimate for sensitivity was 86% (95% CI 78%, 92%) (Fig 3), and the pooled estimate for specificity was 74% (95% CI 68%, 79%) (Fig 4). The AUC of the live stiffness measured by TE to predict the overall postoperative complications was 0.87(95% CI 0.83, 0.89) (Fig 5). The LSM cut-off value using TE for postoperative complications varied from 9.7kPa to 25.6kPa. To ascertain the optimal LSM cut-off value, we made a weighted mean LSM value of these studies. The results showed that the weighted mean value of 14.2kPa and 11.3kPa as the optimal LSM cut-off value using TE for predicting postoperative complications in Asian and European countries, respectively (Table 3).
Fig 3. Forest plot meta-analyses of studies evaluating the sensitivity of live stiffness measured by TE to predict the overall postoperative complications.
Fig 4. Forest plot meta-analyses of studies evaluating the specificity of live stiffness measured by TE to predict the overall postoperative complications.
Fig 5. SROC curves for 6 studies of live stiffness measured by TE to predict the overall postoperative complications.
Table 3. Results of optimal LSM cut-off value using TE in predicting postoperative complications.
| Country | Studies | Patients(n) | Weighted Mean LSM value(KPa) | Range(KPa) |
|---|---|---|---|---|
| Asia countries | 4 | 507 | 14.2 | 12–25.6 |
| European countries | 2 | 330 | 11.3 | 9.7–15.7 |
| overall | 6 | 837 | 13.1 | 9.7–25.6 |
LSM, liver stiffness measurement; TE, transient elastography; KPa, Kilopascal.
Subgroup analyses and meta-regression analyses
Considerable heterogeneity was observed in the overall analysis (I2 = 86.5%, P = 0.000) and the random effects model was adopted. There was significant inconsistency in the magnitude of effects and not in the direction of effect. Subgroup analyses and multivariable meta-regression were performed to explore sources of heterogeneity. Subgroup analysis (Table 4) indicated that the technique of LSM used, etiology of CLD and overall postoperative complications might result in the clinical heterogeneity. Further meta-regression analysis suggested that location of countries might be a potential source of heterogeneity (P = 0.033). Subgroup analysis and meta-regression indicated that percentage of patients with advanced fibrosis could not explain the heterogeneity. Summarized ORs of 2 studies using MRE (OR 2.24, 95% CI 1.74–2.89) and 2 studies using SWE (OR 1.98, 95% CI 1.60–3.30) was higher as compared with seven studies using TE (OR 1.30, 95% CI 1.11–1.52). The pooled ORs of ARFI subgroup demonstrated that LSM using ARFI had no significant effect on overall complications (OR 9.74, 95% CI 0.39–240.25). Additionally, the pooled ORs of ascites subgroup were 7.70 (95% CI 0.17–341.88), which had no significant association with LSM.
Table 4. Subgroup analyses for association between LSM and overall postoperative complications.
| Group factors | Subgroup | studies | Combined OR | 95%CI | Heterogeneity | P value |
|---|---|---|---|---|---|---|
| I2 | ||||||
| Regions | Asia | 10 | 2.30 | 1.75, 3.04 | 63.2% | 0.004 |
| Europe | 3 | 1.12 | 1.00, 1.26 | 78.5% | 0.010 | |
| Technique of LSM | MRE | 2 | 2.24 | 1.74, 2.89 | 0.0% | 0.536 |
| TE | 7 | 1.30 | 1.11,1.52 | 48.3% | 0.085 | |
| SWE | 2 | 1.98 | 1.16, 3.30 | 46.1% | 0.173 | |
| ARFI | 2 | 9.74 | 0.39, 240.25 | 76.2% | 0.040 | |
| Outcome | Composite complications | 3 | 2.87 | 1.65, 5.00 | 47.3% | 0.150 |
| PHLF | 7 | 1.46 | 1.23, 1.74 | 84.7% | 0.000 | |
| ascites | 2 | 7.70 | 0.17, 341.88 | 82.9% | 0.000 | |
| Hepatic insufficiency | 1 | 19.14 | 2.71, 135.27 | NA | NA | |
| Etiology of CLD | Mixed | 11 | 1.74 | 1.42, 2.13 | 87.0% | 0.000 |
| Viral hepatitis | 2 | 1.89 | 1.02, 3.49 | 62.0% | 0.105 | |
| Stage of fibrosis | The percentage of patients with fibrosis grade F4≥50% | 7 | 1.32 | 1.11, 1.57 | 80.4% | 0.000 |
| The percentage of patients with fibrosis grade F4<50% | 6 | 2.20 | 1.60, 3.01 | 64.2% | 0.016 |
LSM, liver stiffness measurement; TE, transient elastography; SWE, shear wave elastography; MRE, magnetic resonance elastography; ARFI, acoustic radio force impulse; CLD, chronic liver diseases.
Sensitivity analysis
All studies were sequentially removed to evaluate the effect of individual study on the pooled ORs (Table 5). The pooled ORs of sensitivity analyses varied from 1.67(95%CI, 1.39–2.00) to 2.20(95%CI, 1.62–3.00) for the prognostic value of liver stiffness measurement for overall postoperative complications, suggesting that the pooled ORs were not significantly affected by individual study.
Table 5. Effect of individual studies on the pooled ORs of the prognostic value of liver stiffness measurement for overall postoperative complications.
| Study omitted | OR | LCI | HCI |
|---|---|---|---|
| Shen 2017 | 1.71 | 1.42 | 2.05 |
| Han 2017 | 1.77 | 1.46 | 2.14 |
| Chong 2017 | 1.73 | 1.44 | 2.09 |
| Abe 2017 | 1.67 | 1.39 | 2.00 |
| Nishio 2016 | 1.67 | 1.39 | 2.00 |
| Lee 2016 | 1.68 | 1.40 | 2.02 |
| Donadon 2016 | 1.72 | 1.43 | 2.07 |
| Cucchetti 2016 | 2.20 | 1.62 | 3.00 |
| Li 2015 | 1.80 | 1.48 | 2.20 |
| Wong 2013 | 1.71 | 1.42 | 2.04 |
| Harada 2012 | 1.72 | 1.44 | 2.06 |
| Cescon 2012 | 2.20 | 1.62 | 3.00 |
| Kim 2008 | 1.70 | 1.43 | 2.04 |
Discussion
This meta-analysis of 13 cohort studies on 1942 patients showed that LSM can significantly predict the occurrence of overall postoperative complications, which include PHLF, hepatic insufficiency, and ascites for patients with HCC undergoing hepatic resection. The result showed that preoperative LSM was significantly higher in patients who developed postoperative complications than in those who did not. Regardless of the varied baseline of LSM, a positive correlation was observed with the development of different grades of postoperative complications. Patients with a higher LSM will have a higher chance of getting high-grade complications.
Prediction on patients with high risk of poor surgical outcomes before hepatectomy allows surgeons to select appropriate candidates and improve chances for cure. Liver stiffness is closely related to liver function and reflects the possible volume of remnant liver after hepatectomy, which determine the risk of postoperative complications[27]. Additionally, Llop E et al. reported that TE can predict the occurrence of portal hypertension (hepatic venous pressure gradient≥ 10 mm Hg) in about 50% of patients, particularly in patients with LSM>21kPa[28]. Portal hypertension has been proven as a risk factor for postoperative complications[29]. Accordingly, the LSM prognostic value can also account for the presence of portal hypertension in some patients.
The optimal LSM cut-off value varied between the included studies. Firstly, this variation can be explained by the different definitions of postoperative complications in studies that range from hepatic insufficiency to fulminant hepatic failure with high mortality. In the study by Hong Han et al., the LSM cut-off value at 6.9 kPa was used to identify PHLF grade A/B; whereas in the study by Seung Up Kim et al., the outcomes were hepatic insufficiency, which was defined as persistent hyperbilirubinemia for more than 5 days after surgery or postoperative death without other identifiable cause. As a result, a high LSM cut-off value at 25.7kPa was detected because it caused a high risk of irreversible PHLF. Secondly, LSM varied in patient groups with different backgrounds, such as nonalcoholic fatty liver disease and viral hepatitis[30]. Thirdly, in comparison with the European population, the body mass index was smaller in the Asian cohort. A higher prevalence of hepatitis C infection was also observed in European countries, whereas hepatitis B infection in Asian countries. If the major cause of liver diseases was the hepatitis B virus infection, the liver tends to become macronodular and the total amount of fibrotic material maybe lower than that in the hepatitis C virus infection or other causes[31]. Moreover, Wong et al. and Chong et al. recommended LSM >12kPa as a predictor for the development of major complications after hepatectomy for various pathologies. In this meta-analysis, we calculated weighted mean LSM value of TE separately in European and Asian countries. The cut-off value can be >14.2kPa in Asian patients and >11.3kPa in European patients of HCC, in reference to predict overall postoperative complications.
Predicting the high risk postoperative complications before surgery is significant because its prevention is more important than treatment. Appropriate choice of preoperative technique to reduce the risk of complications and excellent management for high risk patients are essential to optimize surgical outcomes. The cutoff value of LSM at 14.2kPa in Asian patients and 11.3kPa in European patients can be used to stratify patients who need extra peri-operative care. Before hepatectomy, techniques like portal vein embolization should be considered to improve the functional liver remnant and minimize intra-operative hepatocyte injury that would be caused by the abrupt increase in portal venous pressure at the time of resection[32]. In order to preserve more liver parenchyma, precise hepatectomy should be performed. At the time of surgery, factors associated with increased risk should be avoid and included massive operative blood loss, blood transfusions, vascular resection and extended operative time[33]. The time of portal occlusion must be strictly assessed and half hepatic blood flow occlusion is recommended. After operation, close postoperative monitoring and early supportive treatment to save the function of remnant liver are critical for survivals. Supporting care of failing systems, infusion of albumin, blood transfusion and nutritional supplementation are the main treatments of postoperative complications[34].
Significant heterogeneities were found among studies when we investigated the associations between LSM with composite postoperative complications, which included PHLF, hepatic insufficiency, and ascites. The random-effects model was used in the pooling of data to achieve relatively narrow CIs. This method might reduce the effect of heterogeneity but not abolish it. The heterogeneities were seen mainly in the strength of the association between LSM and surgical outcomes but not in the direction of association. To explore the sources of heterogeneities, both the subgroup analyses and meta-regression were performed. The result showed that technique of LSM used, location of countries, and overall postoperative complications might contribute to the heterogeneities. TE, SWE, and ARFI imaging technology are three noninvasive methods of ultrasound elastography. TE and SWE are all shear wave-based elastography, which uses a mechanical vibrator to apply shear stress to the target tissue[35]. Numerous investigations have extensively validated that these elastography methods had similar diagnostic performances for predicting cirrhosis and liver fibrosis in patients with CLD[36]. Moreover, liver stiffness can be measured with MRE in patients who are obese or have ascites, whereas the shear waves used with ultrasound elastography are limited for these problems[37, 38]. In this study, the results showed that these elastography techniques have similar positive effect as predictors for postoperative complications.
Several potential limitations must be taken into account in this study. The study by Altman DG had shown the intrinsic limitations of meta-analysis of prognostic studies, mainly owing to the quality of the primary studies and the possibility of publication bias on non-significant reports[39]. Clinical heterogeneity of patients and poor assessing methodological quality of prognostic studies have been found, as well as influence in treatment on follow-up evaluation. In this regard, several heterogeneities remain unexplained. The limited number of the included studies is also a limiting factor. Thus, insufficient data to perform all the preplanned subgroup analyses was found. Statistical tests were not performed for funnel plot asymmetry because of the number of studies and the considerable heterogeneity.
In summary, these data converged into a conclusion that LSM is a useful preoperative predictor of the development of postoperative complications in patients with HCC undergoing hepatectomy. Future studies can focus on setting a prognostic model integrated with LSM in predicting post-hepatectomy outcomes.
Supporting information
(DOC)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was funded by National Natural Science Foundation of China (no. 81573715), Natural Science Foundation of Guangdong Province, China (no. 2015A030313348), and Science and Technology Program of Guangzhou, China (no. 201510010257). The funders had significant role in study design, data analysis and preparation of the manuscript.
References
- 1.Poon RT, Fan ST. Hepatectomy for hepatocellular carcinoma: patient selection and postoperative outcome. Liver Transpl. 2004;10(2 Suppl 1):S39–45. [DOI] [PubMed] [Google Scholar]
- 2.Nakayama H, Takayama T. Role of surgical resection for hepatocellular carcinoma based on Japanese clinical guidelines for hepatocellular carcinoma. World J Hepatol. 2015;7(2):261–9. doi: 10.4254/wjh.v7.i2.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ishikawa M, Yogita S, Miyake H, Fukuda Y, Harada M, Wada D, et al. Clarification of risk factors for hepatectomy in patientswith hepatocellular carcinoma. Hepato-Gastroenterology. 2001;49:1625–31. [PubMed] [Google Scholar]
- 4.Fung J, Poon RT, Yu WC, Chan SC, Chan AC, Chok KS, et al. Use of liver stiffness measurement for liver resection surgery: correlation with indocyanine green clearance testing and post-operative outcome. PLoS One. 2013;8(8):e72306 doi: 10.1371/journal.pone.0072306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frulio N, Trillaud H. Ultrasound elastography in liver. Diagn Interv Imaging. 2013;94(5):515–34. doi: 10.1016/j.diii.2013.02.005 [DOI] [PubMed] [Google Scholar]
- 6.Kim SU, Kim BK, Han KH. Clinical application of liver stiffness measurement using transient elastography: a surgical perspective. Digestion. 2013;88(4):258–65. doi: 10.1159/000355948 [DOI] [PubMed] [Google Scholar]
- 7.Chon YE, Choi EH, Song KJ, Park JY, Kim DY, Han KH, et al. Performance of transient elastography for the staging of liver fibrosis in patients with chronic hepatitis B: a meta-analysis. PLoS One. 2012;7(9):e44930 doi: 10.1371/journal.pone.0044930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh S, Fujii LL, Murad MH, Wang Z, Asrani SK, Ehman RL, et al. Liver stiffness is associated with risk of decompensation, liver cancer, and death in patients with chronic liver diseases: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013;11(12):1573–84 e1-2; quiz e88-9. doi: 10.1016/j.cgh.2013.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of interventions. Version 5.1.0. The Cochrane Collaboration; 2011. Retrieved from: http://handbook.cochrane.org/. [Google Scholar]
- 10.Singh S. How to Conduct and Interpret Systematic Reviews and Meta-Analyses. Clin Transl Gastroenterol. 2017;8(5):e93 doi: 10.1038/ctg.2017.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Plos Med. 2009;6:e1000097 doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96. doi: 10.1097/SLA.0b013e3181b13ca2 [DOI] [PubMed] [Google Scholar]
- 13.Nanashima A, Yamaguchi H, Kenji Tanaka SS, Takashi Tsuji NI, Hidaka S, Sawai T, et al. Preoperative serum hyaluronic acid level as a goodpredictor of posthepatectomy complications. Surgery Today. 2004;34:913–9. doi: 10.1007/s00595-004-2845-y [DOI] [PubMed] [Google Scholar]
- 14.Shen Y, Zhou C, Zhu G, Shi G, Zhu X, Huang C, et al. Liver Stiffness Assessed by Shear Wave Elastography Predicts Postoperative Liver Failure in Patients with Hepatocellular Carcinoma. J Gastrointest Surg. 2017. [DOI] [PubMed] [Google Scholar]
- 15.Han H, Hu H, Xu YD, Wang WP, Ding H, Lu Q. Liver failure after hepatectomy: A risk assessment using the pre-hepatectomy shear wave elastography technique. Eur J Radiol. 2017;86:234–40. doi: 10.1016/j.ejrad.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 16.Chong CC, Wong GL, Chan AW, Wong VW, Fong AK, Cheung YS, et al. Liver stiffness measurement predicts high-grade post-hepatectomy liver failure: A prospective cohort study. J Gastroenterol Hepatol. 2017;32(2):506–14. doi: 10.1111/jgh.13503 [DOI] [PubMed] [Google Scholar]
- 17.Abe H, Midorikawa Y, Mitsuka Y, Aramaki O, Higaki T, Matsumoto N, et al. Predicting postoperative outcomes of liver resection by magnetic resonance elastography. Surgery. 2017;162(2):248–55. doi: 10.1016/j.surg.2017.02.014 [DOI] [PubMed] [Google Scholar]
- 18.Nishio T, Taura K, Koyama Y, Tanabe K, Yamamoto G, Okuda Y, et al. Prediction of posthepatectomy liver failure based on liver stiffness measurement in patients with hepatocellular carcinoma. Surgery. 2016;159(2):399–408. doi: 10.1016/j.surg.2015.06.024 [DOI] [PubMed] [Google Scholar]
- 19.Lee DH, Lee JM, Yi NJ, Lee KW, Suh KS, Lee JH, et al. Hepatic stiffness measurement by using MR elastographyprognostic values after hepatic resection for hepatocellularcarcinoma. Eur J Radiol. 2016;27:1713–21. [DOI] [PubMed] [Google Scholar]
- 20.Donadon M, Gatti A, Costa G, Palmisano A, Fontana A, Torzilli G. Prediction of postoperative complications after hepatectomy using the fibroscan. Hpb. 2016;18:e11. [Google Scholar]
- 21.Cucchetti A, Cescon M, Colecchia A, Neri F, Cappelli A, Ravaioli M, et al. Adding Liver Stiffness Measurement to the Routine Evaluation of Hepatocellular Carcinoma Resectability Can Optimize Clinical Outcome. Ultraschall Med. 2016. [DOI] [PubMed] [Google Scholar]
- 22.Li C, Zhang JY, Zhang XY, Wen TF, Yan LN. FibroScan predicts ascites after liver resection for hepatitis B virus-related hepatocellular carcinoma: A prospective cohort study. Int J Surg. 2015;20:21–5. doi: 10.1016/j.ijsu.2015.05.047 [DOI] [PubMed] [Google Scholar]
- 23.Wong JS, Wong GL, Chan AW, Wong VW, Cheung YS, Chong CN, et al. Liver stiffness measurement by transient elastography as a predictor on posthepatectomy outcomes. Ann Surg. 2013;257(5):922–8. doi: 10.1097/SLA.0b013e318269d2ec [DOI] [PubMed] [Google Scholar]
- 24.Harada N, Shirabe K, Ijichi H, Matono R, Uchiyama H, Yoshizumi T, et al. Acoustic radiation force impulse imaging predicts postoperative ascites resulting from curative hepatic resection for hepatocellular carcinoma. Surgery. 2012;151(6):837–43. doi: 10.1016/j.surg.2011.12.035 [DOI] [PubMed] [Google Scholar]
- 25.Cescon M, Colecchia A, Cucchetti A, Peri E, Montrone L, Ercolani G, et al. Value of transient elastography measured with FibroScan in predicting the outcome of hepatic resection for hepatocellular carcinoma. Ann Surg. 2012;256(5):706–12; discussion 12–3. doi: 10.1097/SLA.0b013e3182724ce8 [DOI] [PubMed] [Google Scholar]
- 26.Kim SU, Ahn SH, Park JY, Kim DY, Chon CY, Choi JS, et al. Prediction of postoperative hepatic insufficiency by liver stiffness measurement (FibroScan((R))) before curative resection of hepatocellular carcinoma: a pilot study. Hepatol Int. 2008;2(4):471–7. doi: 10.1007/s12072-008-9091-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Milgrom DP, Maluccio MA, Koniaris LG. Management of Hepatocellular Carcinoma (HCC). Current Surgery Reports. 2016;4(6). doi: 10.1007/s40137-016-0140-7 [Google Scholar]
- 28.Llop E, Berzigotti A, Reig M, Erice E, Reverter E, Seijo S, et al. Assessment of portal hypertension by transient elastography in patients with compensated cirrhosis and potentially resectable liver tumors. J Hepatol. 2012;56(1):103–8. doi: 10.1016/j.jhep.2011.06.027 [DOI] [PubMed] [Google Scholar]
- 29.Choi SB, Kim HJ, Song TJ, Ahn HS, Choi SY. Influence of clinically significant portal hypertension on surgical outcomes and survival following hepatectomy for hepatocellular carcinoma: a systematic review and meta-analysis. Journal of Hepato-Biliary-Pancreatic Sciences. 2014;21(9):639–47. doi: 10.1002/jhbp.124 [DOI] [PubMed] [Google Scholar]
- 30.Wong G, Wong V, Chim A. Factors associated with unreliable liver stiffness measurement and its failure with transient elasto. J Gastroenterol Hepatol. 2011;26:300–5. doi: 10.1111/j.1440-1746.2010.06510.x [DOI] [PubMed] [Google Scholar]
- 31.Castera L, Forns X, Alberti A. Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol. 2008;48(5):835–47. doi: 10.1016/j.jhep.2008.02.008 [DOI] [PubMed] [Google Scholar]
- 32.Thakrar PD, Madoff DC. Preoperative portal vein embolization: an approach to improve the safety of major hepatic resection. Semin Roentgenol. 2011;46(2):142–53. doi: 10.1053/j.ro.2010.08.003 [DOI] [PubMed] [Google Scholar]
- 33.Jin S, Fu Q, Wuyun G, Wuyun T. Management of post-hepatectomy complications. World J Gastroenterol. 2013;19(44):7983–91. doi: 10.3748/wjg.v19.i44.7983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kauffmann R, Fong Y. Post-hepatectomy liver failure. Hepatobiliary Surg Nutr. 2014;3(5):238–46. doi: 10.3978/j.issn.2304-3881.2014.09.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jeong WK, Lim HK, Lee HK, Jo JM, Kim Y. Principles and clinical application of ultrasound elastography for diffuse liver disease. Ultrasonography. 2014;33(3):149–60. doi: 10.14366/usg.14003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park CC, Nguyen P, Hernandez C, Bettencourt R, Ramirez K, Fortney L, et al. Magnetic Resonance Elastography vs Transient Elastography in Detection of Fibrosis and Noninvasive Measurement of Steatosis in Patients With Biopsy-Proven Nonalcoholic Fatty Liver Disease. Gastroenterology. 2017;152(3):598–607 e2. doi: 10.1053/j.gastro.2016.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tang A, Tan J, Sun M, Hamilton G, Bydder M, Wolfson T, et al. Nonalcoholic Fatty Liver Disease: MR Imaging of Liver Proton Density Fat Fraction to Assess Hepatic Steatosis. Radiology. 2013;267:422–31. doi: 10.1148/radiol.12120896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huwart L, Sempoux C, Vicaut E, Salameh N, Annet L, Danse E, et al. Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology. 2008;135(1):32–40. doi: 10.1053/j.gastro.2008.03.076 [DOI] [PubMed] [Google Scholar]
- 39.Altman DG. Systematic reviews of evaluations of prognostic variables. BMJ. 2001;323:224–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.