Summary
This study investigates whether the rubber hand illusion (RHI) can induce a remission of somatoparaphrenia, a somatic delusion usually following right-hemisphere damage, which typically manifests as a defective sense of ownership of one's contralesional body parts. First, we show that patients with somatoparaphrenia can experience a reliable RHI, exhibiting illusory effects similar to those reported by healthy participants. Moreover, synchronous touches applied to the patients' visible disowned left hand (rather than to the rubber hand), and to their right invisible unimpaired hand, induce an immediate self-attribution of the disowned hand, without affecting other sensorimotor or attentional disorders. The higher-level representation of the body concerned with ownership, deranged as a somatic delusion in patients with somatoparaphrenia, is penetrable, and can be restored by multisensory stimulations.
The sense of body ownership, namely the feeling that one's whole body and body parts belong to oneself,1,2 is related to multisensory integration of bodily signals.3 A useful paradigm for its investigation is the rubber hand illusion4 (i.e., RHI): synchronous touches, applied to a visible rubber hand and to the real hand—hidden from view—produce the sensation that the felt touches originate from the rubber hand, and a feeling of ownership of the artificial hand rapidly develops. The RHI has been widely used to investigate the functional and neural underpinnings of body ownership.3,5 Yet there is no evidence that the RHI may affect the multifarious delusional patterns of body disownership due to damage to the right hemisphere.6,7
Deficient body ownership is the hallmark of somatoparaphrenia: a somatic delusion usually following right-hemisphere lesions, which typically manifests as a defective sense of ownership of one's contralesional body parts.6,7 This condition may occur independently of sensorimotor deficits and right-hemisphere disorders (anosognosia for motor and sensory deficits, spatial hemineglect).7 The delusion is not impenetrable and it may temporarily recover after vestibular stimulation.8
Somatoparaphrenia represents the ideal condition for assessing the chance of manipulating and, possibly, restoring a deranged representation of the body concerned with ownership. Hence, in 2 right-brain-damaged patients with a persistent delusion about the ownership of their left hand, we investigated whether the RHI can rearrange the self-attribution of the disowned hand.
METHODS
Participants
Two right-brain-damaged patients (P1, P2) and 12 age-matched, neurologically healthy controls (right-handed, mean age = 77 ± 8, 6 female), with no history or evidence of neurologic or psychiatric disorders, were recruited from the inpatient population of the IRCCS Istituto Auxologico Italiano (Milan, Italy). All participants gave their informed consent to participate in the study, which was carried out in accordance with the ethical standards of the Declaration of Helsinki (BMJ 1991;302:1194), and was approved by the local ethical committee.
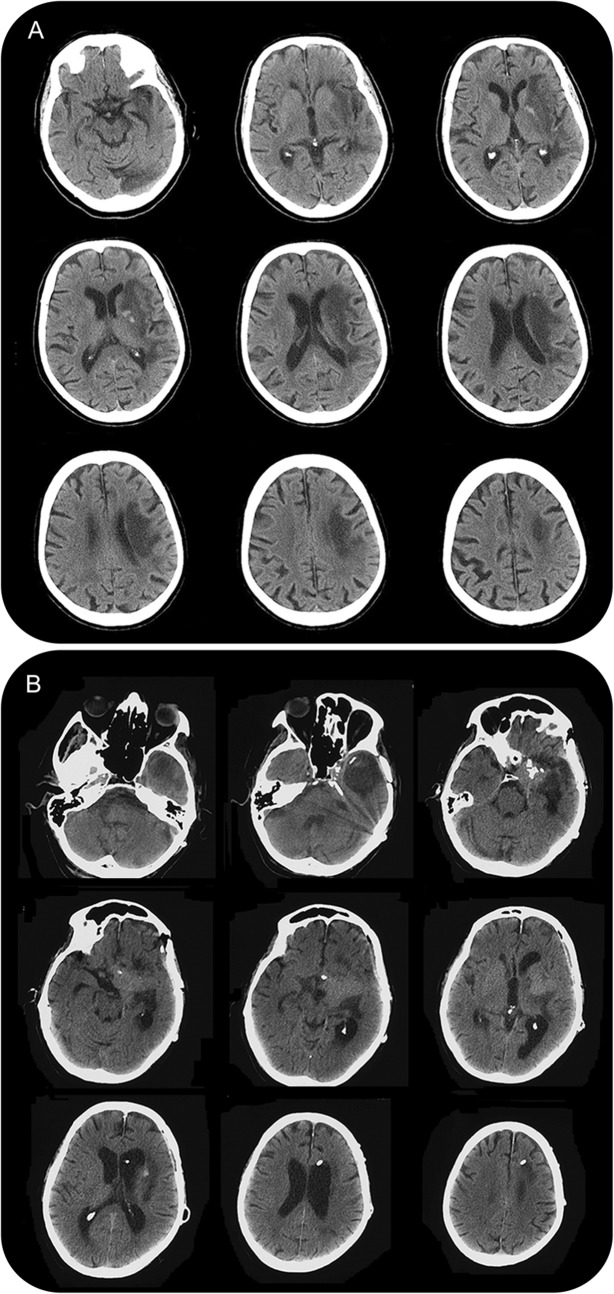
P1 was a 97-year-old right-handed woman with 17 years of education who had worked as a piano music teacher. P1 was largely independent in everyday life, although helped by a caregiver. P1 suddenly presented with a left hemiplegia. CT scan performed 13 days after stroke onset showed an ischemic lesion with a hemorrhagic component in the right hemisphere, involving the fronto-parietal-temporal regions, the underlying white matter, the insular cortex, and the basal ganglia (figure 1A). P1 had no history of neurologic or psychiatric disorders. Fifteen days after stroke onset, P1 was admitted to a neurorehabilitation unit. At that time, P1 was alert, cooperative, and oriented in space, with a mild temporal disorientation. Neurologic examination showed a complete rightward deviation of head and gaze,9 left hemianopia on confrontation testing, left hemiplegia, and hemianesthesia (touch, position sense, and pain). Deep tendon reflexes and muscle tone were increased in the left lower limb and absent in the hypotonic left upper limb. P1 was unaware of her left sensorimotor deficits. The neuropsychological assessment showed left spatial neglect (table 1), with perseveration behavior.10 Personal neglect was mild, as assessed by tasks verbally requiring to reach, with the right hand, the left hand and other left-sided body parts,11,12 and by a task requiring to search targets located on the body,13 when blindfolded. P1, spontaneously and repeatedly, stated that her left hand belonged to her son, obdurately denying it was her own, while ownership of the remaining part of the left upper limb was preserved (table 2A). Occasionally, she showed a delusional belief regarding her left leg, which she did not recognize as a body part but defined as a “metal tube.” Questioned by the examiner about her own left hand, she became silent, or stated that she was unable to account for the fact that her left hand was not available. P1 was not distressed or surprised at being unable to find her left hand; rather, she repeatedly stated that her son's hand was there to help her in the hospital. She never manifested any aggressive behavior toward her left hand, or the left side of her body. Sense of ownership of the right side of the body was consistently preserved.
CT images
Figure 1. (A) P1. (B) P2.
Table 1 Neuropsychological assessment
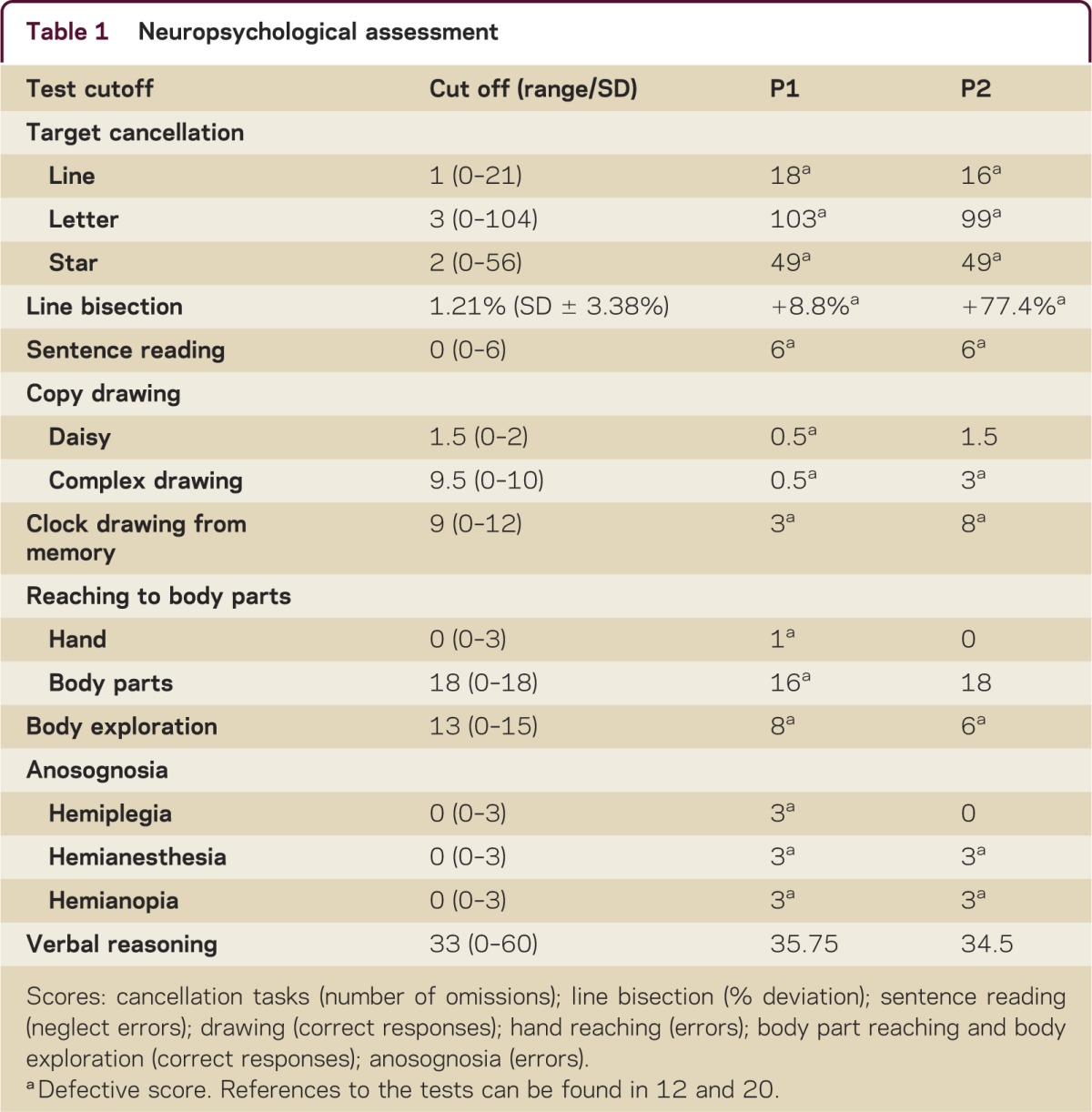
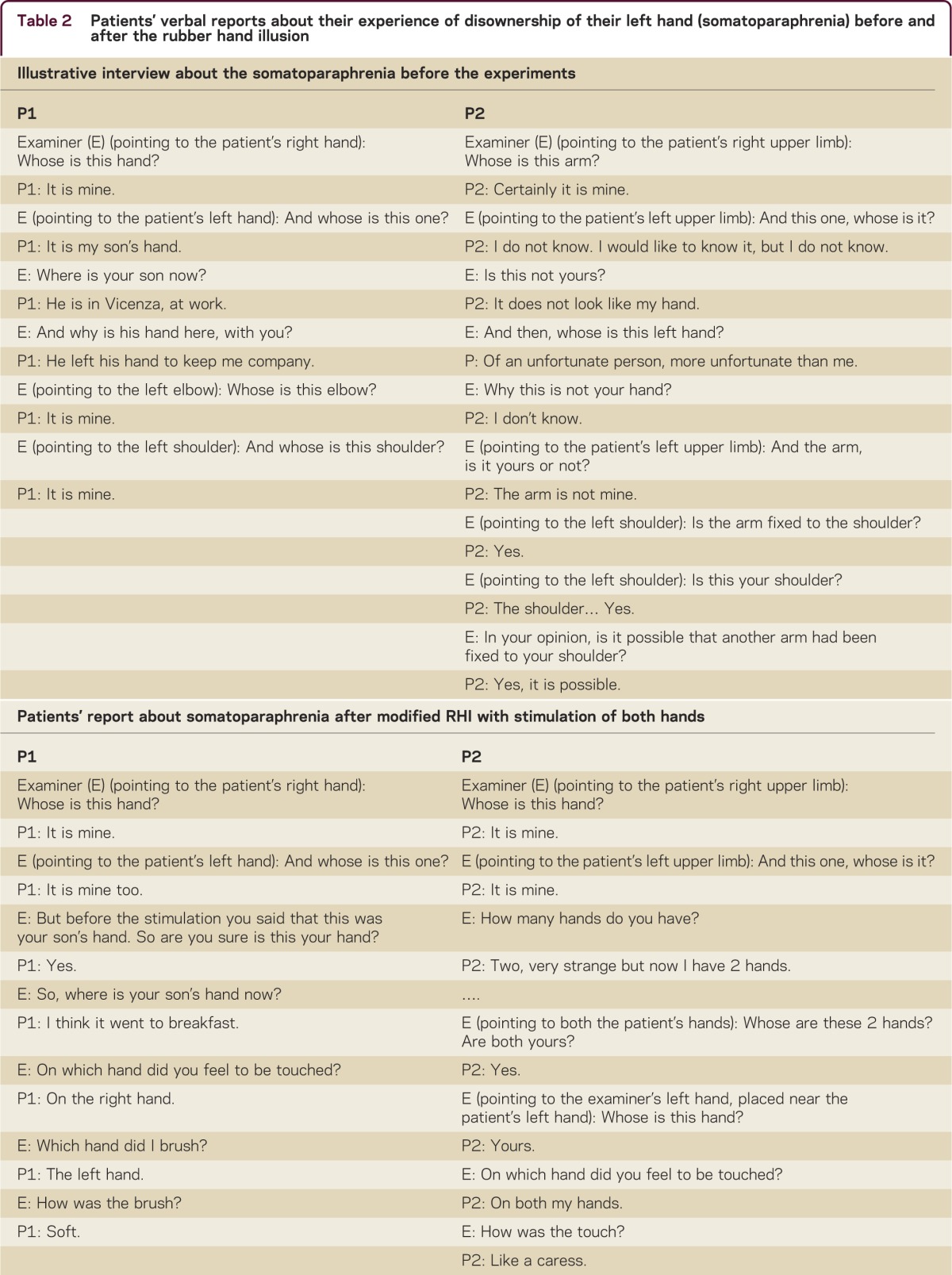
Table 2 Patients' verbal reports about their experience of disownership of their left hand (somatoparaphrenia) before and after the rubber hand illusion
P2 was a 72-year-old right-handed man, a retired technician, with 7 years of education, and no history of neurologic or psychiatric disorders. P2's onset of the disease included left motor and visual-half-field deficits. MRI examination showed a neoplastic lesion in the right parasellar region, for which P2 underwent brain surgery. One month after surgery, CT scan showed a residual lesion in the right parasellar area, extending to the basal ganglia, and a cortical-subcortical hypodense lesion in the right temporal region (figure 1B). Two weeks after surgery, P2 was admitted to a neurorehabilitation hospital. At that time, P2 was alert, cooperative, well oriented in space, poorly oriented in time, and aware of his illness and motor deficits. A neurologic examination showed rightward head and gaze deviation9 and left hemiplegia, with brisk tendon reflexes and increased muscle tone in the left lower limb; in the hypotonic upper limb, tendon reflexes were absent. P2 showed a left hemianesthesia for touch, proprioception, and pain, and left hemianopia on confrontation testing. P2 was unaware of his sensory and visual-half-field deficits. He showed severe left extrapersonal and personal neglect, with no perseveration in cancellation and drawing tasks (table 1). The patient never referred spontaneously to his left hand or, in general, to the left side of his body. Questioned about the ownership of the left upper limb, P2 firmly reported that it did not belong to him, but he did not know exactly whose it was (table 2A). P2 did not attribute the ownership of his left arm to a well-identified person, but the sense of disownership of his left arm was obdurate and continuously reported by him. Sense of ownership of both the left lower limb and of the right limbs was preserved.
In both patients, somatoparaphrenia and the left-sided somatosensory deficit were not affected by the position of the left hand with respect to body midline.14
Experimental procedure
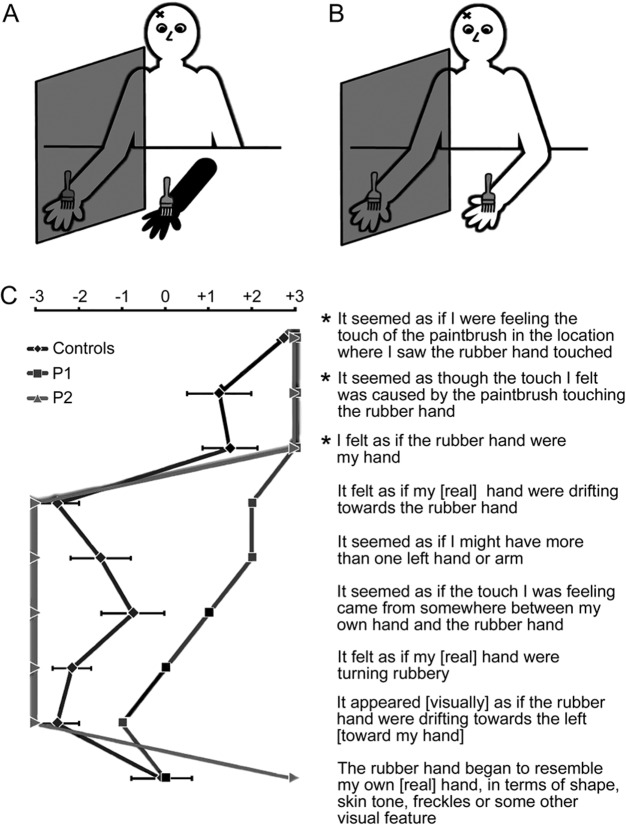
In the first experiment, RHI was induced through tactile stimulation of the right hand (ipsilesional hand for right-brain-damaged patients) and simultaneous visual stimulation of a rubber right hand, following the original paradigm4 (figure 2A). Patients were seated with their right forearm resting upon a table, with a standing screen positioned beside the right arm, to hide it from view; they wore a black smock to occlude their upper right and left arms, and a life-sized rubber right hand and arm was placed in front of them, near the body midline. Patients were instructed to look at and pay attention to the rubber hand, while the experimenter stroked, with 2 small paintbrushes, the right rubber hand for 10 minutes (visual stimulation), and the patient's hidden right-ipsilesional hand (tactile stimulation), synchronizing the timing of the 2 brushings as closely as possible. The experimenter checked that the patient looked at the rubber hand throughout its stimulation, recalling his or her attention if necessary. After stimulation, participants completed a questionnaire4 asking them to affirm or deny the occurrence of 9 perceptual effects (figure 2C), marking their response on a vertically arranged 7-step visual analogue scale, ranging from “agree strongly” (+3) to “disagree strongly” (−3).
Setups for the RHI and for the multisensory stimulation of the left disowned hand
Figure 2. (A) Rubber hand illusion (RHI). (B) Multisensory stimulation of the left disowned hand. (C) Questionnaire results: The questionnaire included the 9 statements shown. Asterisks = statements featuring the RHI. Error bars = SE for controls.
In the second experiment, P1 and P2 were then submitted to a modified version of RHI, during which their visible left disowned hand, near the body midline, and the hidden right hand, in a symmetrical position, were simultaneously stroked for 10 minutes (figure 2B). Throughout the stimulation, the experimenter took care to control that patients looked at the left hand, recalling their attention whenever necessary. Before and after stimulation, for 6 times the experimenter pointed to the patient's left hand, asking: “Whose is this hand?” The procedure was repeated for the right hand, immediately recognized as their own hand by the patients. These questions were asked in random order, while involving the patient in a general conversation, to avoid stereotyped verbal responses.
Preliminarily, the effect of the mere view of the tactile stimulation of the rubber hand, and of the left hand, without the concurrent tactile stimulation of the right hand, was assessed: in both cases, the patients did not report any sense of ownership concerning either the rubber hand (a delusional belief) or the left hand.
Statistical analysis and results
RHI
The participants' scores on the RHI questionnaire were submitted to a repeated-measure analysis of variance, with the between-subject factor group (controls vs patients) and the within-subject factor statement. Only a main effect of statement was found (F8,96 = 9.16, p < 0.00001, pη2 = 0.5); the main effect of group (F1,12 = 1.08, p = 0.319, pη2 = 0.08) and the group by statement interaction (F8,96 = 0.41, p = 0.92, pη2 = 0.03) were not significant. The patients' scores on each item of the questionnaire did not differ from those of controls (all ps > 0.07), as further assessed by t tests for single case analysis.15
In the second experiment, the sign test was used to verify the reliability of the self-attribution of the contralesional, disowned hand, before and after the stimulation. Before the stimulation, both P1 and P2 stated that the left hand did not belong to them (0/6, p = 1). Instead, after stimulation, both patients reported that the left hand was their own left hand (6 out 6 trials, sign test, p = 0.0313). The regained sense of ownership was further confirmed through additional questions such as “Are you sure that it is yours?” or “How many hands do you have now?” as reported in table 2B.
After 10 minutes, P1 again denied ownership of the left hand (0/6, p = 1). However, P2 still recognized his left hand as his own 2 hours and 1 day after the experiment (6/6, p = 0.0313), as also reported at the interviews. P2, who remembered the previous delusional belief, was strongly convinced that his hand had “returned,” and he thanked the examiners who “gave it back” to him.
Neurologic and cognitive disorders
After the second experiment, no change of the neurologic deficits was observed in P1, except for the remission of somatoparaphrenia: P1 continued to show a rightward deviation of eyes and head during the interview; the impairment in orienting the attention toward the left hemispace was still evident. A formal reassessment of spatial, body, and sensorimotor disorders could not be performed during the short-lasting (10 minutes) remission of somatoparaphrenia. The following day, before discharge from the hospital, P1's neurologic and neuropsychological deficits were unchanged as compared to the first evaluation.
P2's left, complete, hemiplegia hemianopia hemianesthesia and the rightward deviation of the head and eyes did not change during remission of the somatic delusion. On the Star cancellation task,16 P2 crossed out only 8 right-sided targets, similar to the first assessment. Overall, the preadmission evaluation shows no change as compared to the first neurologic/neuropsychological assessment.
DISCUSSION
The present study shows that multisensory body-related signals provided through the RHI affect hand ownership and self-attribution in 2 right-brain-damaged patients with somatoparaphrenia. Both patients show a reliable RHI comparable to that of healthy participants, as assessed with the questionnaire. The main aspects of the patients' reports include the illusory tactile experience of feeling the viewed, rather than the hidden, brush, as if the rubber hand sensed the touch; and the feeling that the rubber hand was their own hand (figure 2C). The sense of body ownership may be based on the integration and processing of congruent multisensory signals from the person's own body.3 In the RHI, the combination of tactile stimulation (stroking) and visual input (the rubber hand) may allow patients to project their own body representation onto the rubber hand. This, in turn, may give leeway for encoding the rubber hand as a part of the patients' own body schema, including feeling of ownership of it. Therefore, at least in some patients with somatic delusions, multisensory mechanisms supporting the sense of body part ownership are not completely lost,17 notwithstanding their pathologic delusion of body disownership.
Can multisensory bodily signals induce a remission of delusional beliefs concerning the somatoparaphrenic hand? This issue was addressed by stroking the patients' visible left (disowned) hand and invisible right hand. Notably, patients could not report the feeling of being touched during the stroking of their left hand, due to the left hemianesthesia. Before stimulation, the patients' delusional belief was stable, as repeatedly assessed daily for a week. The manipulation induced an immediate self-attribution of the left hand: both patients reported that the left hand was their own left hand; they were convinced about that, as shown by their reports during the poststimulation interview (see table 2B). Notably, the mere view of the left hand being stroked, without the concomitant tactile stimulation of the right hand, did not affect somatoparaphrenia; therefore, the RHI is necessary for the self-attribution of the disowned hand. After 10 minutes, P1 again denied ownership of the left hand. This is in line with evidence showing that other forms of crossmodal stimulation (i.e., vestibular stimulation,8 mirror therapy18) may temporarily relieve somatoparaphrenic symptoms. Instead, P2 still reported that his left hand was his own hand after 24 hours; during repeated sessions, P2 continued to report the firm conviction of ownership of both hands, and the feeling of relief because his left hand had been “returned” to him. Therefore, the visuo-tactile stimulation of both hands (i.e., visual stimulation of the disowned hand, tactile stimulation of the right hand) can even induce a stable remission of somatoparaphrenia. Future studies may clarify which clinical features are associated with the enduring modulation of the delusional belief.
Remarkably, the patients' delusional belief concerning their left hand was the only symptom affected by the experimental manipulation, while other deficits related to their right-hemisphere damage did not change. Indeed, left spatial neglect was stable after the stimulation, as clinically observed in P1 and P2, and assessed by tests in P2. Neither the motor, somatosensory, nor visual-half-field deficits (and the related anosognosia) were affected by the experimental procedure (based on P2's data). Therefore, remission of somatoparaphrenia can be ascribed neither to effects involving the patient's representation of extrapersonal space nor to a mere shift of spatial attention on the left hand.19
This evidence shows that a delusional experience of body disownership, caused by a unilateral brain lesion, can be selectively modified by a brief exposure to a cross-modal illusion. Although unisensory processing in the visual and somatosensory modalities may be disrupted by unilateral hemispheric lesions, multisensory integration may still work efficiently.17 The combination of tactile stimulation (stroking the right hand) and visual input (the left somatoparaphrenic hand) provided by the RHI promotes a projection of the patients' sensations from the unimpaired hand onto the disowned hand. In this way, patients may regain the sense of ownership of their left hand. The higher-level damaged representation of the body concerned with ownership, deranged as a somatic delusion in somatoparaphrenia,6,7 is penetrable and may be restored by multisensory bodily signals, which affect sense of body ownership in an unimpaired state.
STUDY FUNDING
Supported by F.A.R. Grant 2013 (University of Milano-Bicocca) to N.B. and G.V.
DISCLOSURES
N. Bolognini serves as an Associate Editor for BMC Neuroscience. R. Ronchi, C. Casati, P. Fortis, and G. Vallar report no disclosures. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
Correspondence to: giuseppe.vallar@unimib.it
Funding information and disclosures are provided at the end of the article. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
Footnotes
Correspondence to: giuseppe.vallar@unimib.it
REFERENCES
- 1.Feinberg TE. Some interesting perturbations of the self in neurology. Semin Neurol. 1997;17:129–135. doi: 10.1055/s-2008-1040922. [DOI] [PubMed] [Google Scholar]
- 2.Gallagher I. Philosophical conceptions of the self: implications for cognitive science. Trends Cogn Sci. 2000;4:14–21. doi: 10.1016/s1364-6613(99)01417-5. [DOI] [PubMed] [Google Scholar]
- 3.Ehrsson HH. The concept of body ownership and its relation to multisensory integration. In: Stein BE, ed. The New Handbook of Multisensory Processes. Cambridge, MA: MIT Press; 2011:775–792.
- 4.Botvinick M, Cohen J. Rubber hands “feel” touch that eyes see. Nature. 1998;391:756. doi: 10.1038/35784. [DOI] [PubMed] [Google Scholar]
- 5.Tsakiris M. My body in the brain: a neurocognitive model of body-ownership. Neuropsychologia. 2010;48:703–712. doi: 10.1016/j.neuropsychologia.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 6.Feinberg TE, Venneri A, Simone AM, Fan Y, Northoff G. The neuroanatomy of asomatognosia and somatoparaphrenia. J Neurol Neurosurg Psychiatry. 2010;81:276–281. doi: 10.1136/jnnp.2009.188946. [DOI] [PubMed] [Google Scholar]
- 7.Vallar G, Ronchi R. Somatoparaphrenia: a body delusion: a review of the neuropsychological literature. Exp Brain Res. 2009;192:533–551. doi: 10.1007/s00221-008-1562-y. [DOI] [PubMed] [Google Scholar]
- 8.Bisiach E, Rusconi ML, Vallar G. Remission of somatoparaphrenic delusion through vestibular stimulation. Neuropsychologia. 1991;29:1029–1031. doi: 10.1016/0028-3932(91)90066-h. [DOI] [PubMed] [Google Scholar]
- 9.De Renzi E, Colombo A, Faglioni P, Gibertoni M. Conjugate gaze paresis in stroke patients with unilateral damage: an unexpected instance of hemispheric asymmetry. Arch Neurol. 1982;39:482–486. doi: 10.1001/archneur.1982.00510200024004. [DOI] [PubMed] [Google Scholar]
- 10.Ronchi R, Posteraro L, Fortis P, Bricolo E, Vallar G. Perseveration in left spatial neglect: drawing and cancellation tasks. Cortex. 2009;45:300–312. doi: 10.1016/j.cortex.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 11.Bisiach E, Perani D, Vallar G, Berti A. Unilateral neglect: personal and extra-personal. Neuropsychologia. 1986;24:759–767. doi: 10.1016/0028-3932(86)90075-8. [DOI] [PubMed] [Google Scholar]
- 12.Fortis P, Maravita A, Gallucci M. Rehabilitating patients with left spatial neglect by prism exposure during a visuomotor activity. Neuropsychology. 2010;24:681–697. doi: 10.1037/a0019476. [DOI] [PubMed] [Google Scholar]
- 13.Cocchini G, Beschin N, Jehkonen M. The Fluff Test: a simple task to assess body representation neglect. Neuropsychological Rehabil. 2001;11:17–31. [Google Scholar]
- 14.Moro V, Zampini M, Aglioti SM. Changes in spatial position of hands modify tactile extinction but not disownership of contralesional hand in two right brain-damaged patients. Neurocase. 2004;10:437–443. doi: 10.1080/13554790490894020. [DOI] [PubMed] [Google Scholar]
- 15.Crawford JR, Garthwaite PH. Testing for suspected impairments and dissociations in single-case studies in neuropsychology: evaluation of alternatives using Monte Carlo simulations and revised tests for dissociations. Neuropsychology. 2005;19:318–331. doi: 10.1037/0894-4105.19.3.318. [DOI] [PubMed] [Google Scholar]
- 16.Wilson B, Cockburn J, Halligan PW. Behavioural Inattention Test. Titchfield, UK: Thames Valley Test; 1987.
- 17.Bolognini N, Convento S, Rossetti A, Merabet LB. Multisensory processing after a brain damage: clues on post-injury crossmodal plasticity from neuropsychology. Neurosci Biobehav Rev. 2013;37:269–278. doi: 10.1016/j.neubiorev.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Fotopoulou A, Jenkinson PM, Tsakiris M, Haggard P, Rudd A, Kopelman MD. Mirror-view reverses somatoparaphrenia: dissociation between first- and third-person perspectives on body ownership. Neuropsychologia. 2011;49:3946–3955. doi: 10.1016/j.neuropsychologia.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 19.Kitadono K, Humphreys GW. Short-term effects of the “rubber hand” illusion on aspects of visual neglect. Neurocase. 2007;13:260–271. doi: 10.1080/13554790701625815. [DOI] [PubMed] [Google Scholar]
- 20.Bolognini N, Casanova D, Maravita A, Vallar G. Bisecting real and fake body parts: effects of prism adaptation after right brain damage. Front Hum Neurosci. 2012;6:154. doi: 10.3389/fnhum.2012.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]