Abstract
Approximately 31% of men in treatment for a substance use disorders (SUD) engage in compulsive sexual behavior (CSB). Shame, a well-documented consequence of CSB, increases the likelihood of relapse following treatment for SUDs. Despite the risk of relapse, prior research has not investigated factors that may attenuate the relation between CSB and shame. Dispositional mindfulness is one such factor known to mitigate shame. However, researchers have yet to examine dispositional mindfulness as a moderator of the relationship between CSB and shame among a sample of men in treatment for SUDs. In an effort to inform intervention efforts, the present study aimed to investigate the hypothesis that CSB would not relate to shame among men with high, as opposed to low, levels of dispositional mindfulness. The present study reviewed medical records of 184 men in residential treatment for SUDs who completed cross-sectional measures of shame, CSB, dispositional mindfulness, and substance use problems. Results demonstrated a significant interaction between CSB and dispositional mindfulness such that CSB positively related to shame at low, but not mean or high, levels of dispositional mindfulness. These results support and extend previous mindfulness and CSB treatment research. Findings suggested that intervention efforts for CSB may benefit from increasing dispositional mindfulness in an effort to reduce shame-related cognitions.
Keywords: compulsive sexual behavior, sexual addiction, shame, mindfulness, substance use
Introduction
Approximately 31% of men seeking treatment for a substance use disorder (SUD) identified as at-risk for compulsive sexual behavior (CSB; Stavro, Rizkallah, Dinh-Williams, Chiasson, & Potvin, 2013). CSB can be defined as compulsive, excessive, or otherwise problematic non-paraphilic sexual behaviors (e.g., excessive or compulsive sexual desire/drive, pornography use, sexual chat/video use, masturbation, sexual intercourse, or engagement in sexual fantasy) that cause distress or impairment in occupation, interpersonal, or social functioning (Kafka, 2010). Such men are at an increased risk of relapse following treatment for SUDs if CSB is not addressed (Carnes, 2001; Schneider & Irons, 2001). It is concerning, then, that only a few studies examined CSB among men in treatment for SUDs, and even fewer explored protective factors needed to inform interventions (e.g., Brem, Shorey, Anderson, & Stuart, in press; Shorey, Elmquist, Gawrysiak, Anderson, & Stuart, 2016). Clinicians and researchers working with this understudied population would benefit from further investigation of risk and protective factors for CSB among individuals in treatment for SUDs.
In contrast to guilt, in which an individual’s behavior is negatively evaluated, shame elicits cognitive patterns such that the entire self is negatively evaluated (Tangney & Dearing, 2002). Shame has been delineated into two subtypes: external shame (i.e., shame associated with the perceived negative evaluations from others), and internal shame (i.e., the internal experience of self-criticism and negative self-evaluations viewed through one’s own eyes; Gilbert, 1998). While researchers have not distinguished these types of shame as they relate to CSB, the limited research in this domain focused on the experience of negative self-evaluations (e.g., self-hostility) in relation to shame among individuals with CSB (Reid, Harper, & Anderson, 2009), thereby supporting the continued investigation of internal shame within this population. Shame was conceptualized as both a cause and consequence of addictive behaviors, including CSB and substance use (Gilliland, South, Carpenter, & Hardy, 2011; Masuma & Patton, 2015; Potter-Efron, 2002). Though many individuals who engaged in CSB harbored pre-existing shame (Gilliland et al., 2011), shame experienced as an adult may be exaggerated by CSB (Hall, 2011). Such shame may be due, in part, to non-conformity to societal norms and religious beliefs (e.g., monogamy, sexual repression, and moral objection to pornography) and failure to prioritize certain domains (e.g., families, partners, work, friends, finances, and health) over sexual behaviors (Hall, 2011).
Theoretical and empirical evidence supported a reciprocal relation between shame and CSB (Reid & Carpenter, 2009; Reid, 2010). That is, the consequences associated with CSB (e.g., sexually transmitted infections, relationship distress, loss of employment, legal problems, and financial loss) contributed to shame-related cognitions (e.g., “I’m defective and unworthy of the love of a partner”); an individual may then (1) attempt to alleviate, or (2) seek to confirm shame-related cognitions through continued engagement in CSB (Derbyshire & Grant, 2015; Reid & Carpenter, 2009). Some researchers posited that the reciprocal relationship between shame and CSB may explain why individuals with CSB were at an increased risk of psychiatric conditions, such as depression, anxiety, and substance use (Gilliland et al., 2011).
A growing body of research emphasized the need to address shame-related cognitions among those who engage in CSB to prevent continued CSB and, potentially, other maladaptive coping strategies (e.g., substance use; Gilliland et al., 2011; Reid, 2010). Although shame hindered the treatment of CSB and SUDs individually (Gilliland et al., 2011; Luoma et al., 2007), the complex relations between CSB and SUDs further complicated treatment for men with both CSB and SUDs (Carnes, 1991). For instance, clinical and theoretical evidence suggested that men who display CSB may use substances to cope with CSB-related shame (Carnes, 1991). Furthermore, substance use may exacerbate both shame (Dearing, Stuewig, & Tangney, 2005) and engagement in risky sexual activity (Tull, Weiss, Adams, & Gratz, 2012) which may perpetuate the CSB-shame cycle for individuals with CSB and SUD. For men who engage in both CSB and substance use, reducing shame may interfere with continued CSB, thereby reducing the likelihood of relapse for individuals in treatment for SUDs (Schneider & Irons, 2001). However, researchers have yet to examine moderators of the CSB-shame link among men seeking treatment for SUDs.
Conceptualized as a propensity to purposefully and non-judgmentally attend to present-moment internal and external events, dispositional mindfulness is one such construct linked to lower levels of shame (Baer, 2003; Woods & Proeve, 2014). Individuals higher in dispositional mindfulness were better able to separate cognitions and emotions from the self thereby reducing over-engagement with emotions (Bowlin & Baer, 2012; Hayes & Feldman, 2004). Furthermore, such individuals may approach distressing cognitions, emotions, or physiological experiences with curiosity and acceptance as opposed to avoidance, the latter of which contributed to maladaptive coping strategies (Bishop et al., 2004). Recent evidence suggested that approaching experiences with acceptance facilitated self-compassion (i.e., being touched by or open to one’s suffering as opposed to avoiding or disconnecting from it; Neff, 2003). That self-compassion negatively related to shame implies that mindfulness may reduce shame through increases in self-compassion (Woods & Proeve, 2014).
Given the protective utility of dispositional mindfulness from shame, it is plausible that increases in dispositional mindfulness might interfere with the development of shame-related beliefs among men who engage in CSB. However, researchers have only recently begun to examine dispositional mindfulness as it relates to CSB, and no past research addressed the role of shame. Dispositional mindfulness negatively related to CSB among a sample of men in residential treatment for SUDs (Shorey et al., 2016). Similarly, Reid, Bramen, Anderson, and Cohen (2014) found an inverse relationship between men’s dispositional mindfulness and CSB. Using a single-subject design, van Gordon, Shonin, and Griffiths (2016) found that CSB and CSB-related negative self-thoughts decreased following a mindfulness-based meditation training that incorporated acceptance, awareness, and self-compassion. Furthermore, because research supported the efficacy of mindfulness-based interventions in treating SUDs (Chiesa & Serretti, 2014), it follows that such interventions may be applied to the treatment of CSB among men with SUDs in an effort to reduce both substance use and shame. However, researchers have yet to examine the role of dispositional mindfulness in the relation between CSB and shame.
In sum, existing research has not examined factors that may reduce the likelihood of shame among men with CSB. Dispositional mindfulness is one such factor which may curtail shame among individuals with CSB. Thus, the purpose of the present study was to investigate dispositional mindfulness as a moderator of the relationship between CSB and shame within a treatment sample. Based on existing research and theory, we hypothesized that CSB would positively relate to shame for men with low, but not high, levels of dispositional mindfulness.
Method
Participants
Medical records for 184 men aged 18 and older in residential treatment for SUDs were included in the present study. The primary diagnoses for this sample were alcohol dependence (56.1%), opioid dependence (17.6%), polysubstance dependence (12.8%), alcohol abuse (5.3%), cannabis dependence (3.2%), amphetamine dependence (1.6%), sedative, hypnotic, or anxiolytic dependence (1.6%), cocaine dependence (0.5%), cannabis abuse (0.5%), and opioid abuse (0.5%). The racial/ethnic composition of the sample was as follows: White (89.3%), Black (7.0%), Hispanic (3.2%), and Native American/American Indian (0.5%). Patients’ mean age was 40.82 (SD = 9.88). The majority of the sample reported that they were married (40.1%), followed by never married (24.1%), divorced (19.8%), separated (7.5%), engaged (2.7%), other (2.1%), remarried (1.6%), widowed (1.1%), and none reported (1.1%). The mean number of years of education of the present sample was 13.69 years (SD = 1.94).
Procedure
We reviewed patients’ medical records from a private, residential treatment facility for individuals with SUDs located in the Southeastern United States. Admission dates on records reviewed ranged from February 2013 to April 2014. Admission into the 28–30 day program required that participants be at least 18 years old and have a primary SUD diagnosis. Following admission to the program and after medical detoxification (if necessary), patients completed a series of self-report measures. Treatment thereafter was largely based on the 12-step model of recovery. Diagnoses were based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition – Text Revision (DSM-IV-TR; American Psychiatric Association, 2000) and were determined through consultation of the treatment team, which included a licensed psychologist, psychiatrist, general physician, and chemical dependency counselor. Patients provided consent to have their de-identified medical records used for research purposes. Patient medical records included total scores of each measure only; thus reliability statistics could not be calculated. All procedures were approved by the Institutional Review Board of the first author.
Measures
Dispositional Mindfulness
The treatment facility utilized a 14-item version of the Mindful Attention Awareness Scale (MAAS; Brown & Ryan, 2003), which does not contain the item “I drive places on ‘automatic pilot’ and then wonder why I went there,” to assess self-reported dispositional mindfulness. The treatment facility used the 14-item version of the measure because patients cannot drive while in treatment; the treatment facility wanted to be able to eventually measure pre-post treatment changes in dispositional mindfulness. Participants indicated the extent to which they experience 14 statements (e.g., “I find myself preoccupied with the future or the past”) with responses ranging from 1 (almost always) to 6 (almost never). Scores are summed then divided by 14 to result in a mean MAAS score with possible scores ranging from 1 to 6. Higher scores correspond to higher levels of dispositional mindfulness. Existing literature supports the psychometric properties and use of the MAAS in assessing dispositional mindfulness within treatment-seeking populations (Brown & Ryan, 2003; Dakwar, Mariani, & Levin, 2011).
Compulsive Sexual Behavior
The 20-item Core scale of the Sexual Addiction Screening Test-Revised (SAST-R; Carnes, Green, & Carnes, 2010) was used by the treatment facility to assess core components of CSB, including preoccupation (i.e., obsessive thinking about sexual behavior, opportunities, and fantasies), loss of control (i.e., inability to stop behavior despite commitments to self and others and despite problems caused by the behavior), affective disturbance (i.e., significant depression, despair, or anxiety over sexual behavior), and relationship disturbance (i.e., sexual behavior has created significant relationship problems). Items (e.g., Have you made efforts to quit a type of sexual activity and failed?) are presented in a forced-choice (Yes/No) format with possible scores ranging from 0–20. Higher scores represent higher levels of CSB. The SAST-R demonstrated adequate psychometric properties in clinical and non-clinical samples of adults, and across sexual orientations (Carnes et al., 2010).
Shame
The Young Schema Questionnaire – Long Form, Third Edition’s (YSQ-L3; Young & Brown, 2003) Defectiveness/Shame subscale was used by the treatment facility to assess self-reported internal shame, defined as the belief that one is inherently flawed, defective, and unlovable. The 15 items (e.g., “If others found out about my basic defects I could not face them”) that comprise the defectiveness/shame subscale are answered on a six-point Likert scale ranging from 1 (completely untrue of me) to 6 (describes me perfectly). Items rated by the individual as a 4, 5, or 6 are considered particularly relevant for that individual and are summed such that higher scores are indicative of higher subjective feelings of shame. Items rated by the individual as a 1, 2, or 3 are recoded into “0.” The YSQ’s defectiveness/shame scale associated with a number of psychiatric symptoms, including depression, anxiety, posttraumatic stress disorder, and social phobia to support the convergent validity of the defectiveness/shame scale (Cockram, Drummond & Lee, 2010; Hawke & Provencher, 2011; Pinto-Gouveia, Castilho, Galhardo & Cunha, 2006; Schmidt, Joiner, Young, & Telch, 1995). The YSQ’s defectiveness/shame scale demonstrated good psychometric properties across various populations (Oei & Baranoff, 2007) and has been used with individuals in residential treatment for substance use disorders (Shorey, Elmquist, Anderson, & Stuart, 2015).
Alcohol Use and Problems
The Alcohol Use Disorders Identification Test (AUDIT; Saunders, Asaland, Babor, de la Fuente, & Grant, 1993) was used by the treatment facility to assess the patient’s self-reported alcohol use and problems in the year prior to treatment admission. Ten items examined the intensity and frequency of alcohol use, symptoms of alcohol tolerance and dependence, and negative consequences of alcohol use. Scores are summed such that higher scores are indicative of greater levels of alcohol use and problems. Possible scores range from 0 to 40. The AUDIT demonstrated excellent reliability and validity across multiple populations (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001).
Drug Use and Problems
The Drug Use Disorders Identification Test (DUDIT; Stuart, Moore, Ramsey, & Kahler, 2003; Stuart, Moore, Kahler, & Ramsey, 2003) was used by the treatment facility to assess patients’ drug use (i.e., cannabis, cocaine, hallucinogens, stimulants, sedatives/hypnotics/anxiolytics, opiates, and other substances [e.g., inhalants]) and problems in the year prior to treatment admission. Like the AUDIT, the DUDIT’s 14 items examined the intensity and frequency of drug use, symptoms of drug tolerance and dependence, and negative consequences of drug use. Possible scores range from 0–40. The DUDIT evidenced good psychometric properties (Stuart et al., 2003a, b).
Data Analysis
We conducted a hierarchical multiple regression using Hayes’ (2012) PROCESS macro to test the interaction between CSB and dispositional mindfulness predicting shame while controlling for problems related to alcohol and drug use. Shame scores were entered as the criterion variable, CSB scores as the focal predictor, and dispositional mindfulness as the moderating variable. AUDIT and DUDIT scores were entered as covariates given the relation between these constructs and shame (Luoma et al., 2007). AUDIT and DUDIT scores were entered into the first step, SAST-R Core subscale total scores and MAAS total scores were entered into the second step, and the interaction term (i.e., SAST-R Core subscale total scores multiplied by MAAS total scores) was entered in the third step. All variables were mean centered to reduce multicollinearity (Cohen, Cohen, West, & Aiken, 2003). To explicate the interaction, we tested the relationship between CSB and shame at high (+1 SD), mean, and low (−1 SD) levels of dispositional mindfulness (Aiken & West, 1991).
Results
Means, standard deviations, and correlations between the variables are displayed in Table 1. Bivariate correlations revealed that CSB positively correlated with problems related to alcohol use, and shame. CSB negatively correlated with dispositional mindfulness and did not significantly correlate with problems related to drug use. Dispositional mindfulness negatively correlated with problems related to alcohol and drug use, and shame. Shame positively correlated with problems related to drug and alcohol use.
Table 1.
Means, standard deviations, and correlations among variables.
| Variables | M | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| 1. CSB | 1.34 | 2.64 | --- | ||||
| 2. Dispositional Mindfulness | 3.95 | 1.00 | −.28*** | --- | |||
| 3. Shame | 8.80 | 17.37 | .31*** | −.49*** | --- | ||
| 4. Drug Use and Problems | 10.27 | 12.35 | .04 | −.28*** | .13* | --- | |
| 5. Alcohol Use and Problems | 15.39 | 11.20 | .24** | −.23** | .22** | −.31*** | --- |
Note. CSB = Compulsive sexual behavior.
p < .05,
p <.01,
p < .001.
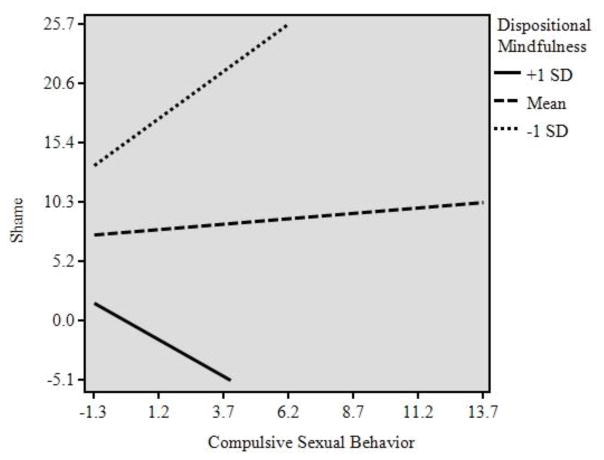
Table 2 displays results of the regression analysis. Our hypothesis was supported. Controlling for problems related to alcohol and drug use, results of a two-way interaction between CSB and dispositional mindfulness revealed the addition of the interaction term contributed to a significant increase in R2 suggesting that the inclusion of the interaction term predicted additional variance in shame scores. The relationship between CSB and shame differed based on the level of dispositional mindfulness reported. Explication of this interaction evidenced a positive association between CSB and shame for men who endorsed low (B = 1.64, p < .001), but not mean (B = .18, p = .73) or high (B = −1.27, p = .16), levels of dispositional mindfulness. Figure 1 displays a visual depiction of the interaction.
Table 2.
Hierarchical regression analyses predicting shame (n = 184)
| Predictor | R2 | ΔR2 | B | β | F |
|---|---|---|---|---|---|
| Step 1 | .09 | 9.15*** | |||
|
| |||||
| Alcohol Use and Problems | .44*** | .29*** | |||
| Drug Use and Problems | .31** | .22** | |||
|
| |||||
| Step 2 | .28 | .19 | 17.67*** | ||
|
| |||||
| Alcohol Use and Problems | .05 | .09 | |||
| Drug Use and Problems | .14 | .04 | |||
| CSB | 1.10* | .17* | |||
| Dispositional Mindfulness | −.48*** | −.42*** | |||
|
| |||||
| Step 3 | .32 | .04 | 16.65*** | ||
|
| |||||
| Alcohol Use and Problems | .11 | .07 | |||
| Drug Use and Problems | .03 | .02 | |||
| CSB | 5.96** | .91** | |||
| Dispositional Mindfulness | −.39*** | −.34*** | |||
| CSB x Dispositional Mindfulness | −.10** | −.74** | |||
Note. All continuous variables are centered. CSB = Compulsive sexual behavior.
p < .05,
p < .01,
p < .001.
Figure 1.
Men’s compulsive sexual behavior positively relates to shame at low, but not mean or high, levels of dispositional mindfulness.
Discussion
The present study examined dispositional mindfulness as a moderator of the relation between CSB and shame among men in residential treatment for SUDs in an effort to extend prior research and inform directions for intervention. Consistent with our hypothesis, men who engaged in CSB were more likely to experience shame when such men also endorsed low levels of dispositional mindfulness. For men with average and high levels of dispositional mindfulness, CSB was not related to shame. Our results provided preliminary support for the relevance of dispositional mindfulness to populations afflicted by CSB, more specifically, men in residential treatment for SUDs.
These findings were consistent with, and extended, previous mindfulness research documenting an inverse association between mindfulness and shame-based cognitions (Woods & Proeve, 2014). Specifically, results from the present study suggested that individuals with low levels of dispositional mindfulness may be more likely to negatively evaluate themselves due, in part, to their engagement in CSB. It is plausible, then, that increases in mindfulness would facilitate acceptance, self-compassion, and non-judgment such that shame diminishes (Woods & Proeve, 2014), even among individuals who engaged in behaviors that are more prone to judgment and non-acceptance (e.g., CSB and substance use). Future research is needed to evaluate this supposition.
Tangney and Dearing (2002) suggested that replacing shame (i.e., the entire self is negatively evaluated) with guilt (i.e., the behavior is negatively evaluated) evokes an empathic, reparative response that deters the development of additional maladaptive coping strategies. Indeed, guilt, not shame, positively predicted motivation to change among a sample of individuals seeking treatment for problematic pornography use (Gilliland et al., 2011). That dispositional mindfulness prevented over-identification with evaluative statements (Bowlin & Baer, 2012) suggests that increasing dispositional mindfulness might promote guilt as a response to CSB as opposed to shame, thereby promoting adaptive behavioral changes. This supposition remains speculative pending additional empirical investigation. It should be noted that no studies have examined the efficacy of a mindfulness-based intervention for CSB. Given the results of the current and prior research (Van Gordon et al., 2016; Reid et al., 2014; Shorey et al., 2016), and the supported efficacy for mindfulness-based interventions for SUDs (Chiesa & Serretti, 2014), future research should investigate the extent to which mindfulness-based interventions for SUDs demonstrate efficacy in reducing CSB and shame among substance-dependent populations.
Results of the present study also provide direction for future research to determine whether increases in dispositional mindfulness deter against shame as well as subsequent substance use and relapse following engagement in CSB. This area of research may be especially instrumental for men with SUDs who engage in CSB given the treatment-hindering properties of shame regarding these behaviors (Gilliland et al., 2011; Luoma et al., 2007). Specifically, mindfulness-based interventions may act as secondary intervention strategies to prevent continued dysfunction (e.g., shame, continued CSB, continued substance use, or other psychiatric symptoms) among treatment-seeking men. Additional research is needed to determine the extent to which dispositional mindfulness reduces shame, CSB, and substance use among treatment-seeking men.
Limitations
Although the present study provided important directions for future research, there are a number of limitations that should be noted. First, our sample was comprised of primarily educated, married, White men. Future research using a more diverse sample is needed to ascertain the generalizability of the present findings to different populations (e.g., women, and individuals of varying racial/ethnic identities and educational backgrounds). We could not determine the percentage of men in the present sample who were involved in same-sex relationships. Therefore, results from the present study may have limited generalizability to men in same-sex relationships. Second, the cross-sectional nature of our data precluded causal conclusions and directionality of study variables. Although research suggested that CSB contributed to shame (Reid, 2010), it is plausible that men in our sample harbored pre-existing shame from early life experiences and used CSB and substances to cope with these experiences (Hall, 2011). Future research should consider examining the proximal relations between CSB-specific shame and engagement in CSB (e.g., via daily diary research methods) to elucidate directionality of study variables. Third, the present study did not assess both internal and external shame (Gilbert, 1998), thereby hindering the generalization of the present findings to instances of external shame. Future research should further explicate the differences in internal and external shame as it relates to CSB. Fourth, our study did not include structured diagnostic interviews for SUDs. Additional research using structured interviews and more robust, multifaceted, well-validated measures of SUDs and shame (e.g., both internal and external shame) would provide a more approximate assessment of the relations among the study variables. Finally, because only total scores were available for each measure, reliability statistics could not be calculated.
Acknowledgments
Funding: This work was supported, in part, by grant K24AA019707 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) awarded to the last author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAAA or the National Institutes of Health.
Footnotes
Conflict of interest: Gregory Stuart started conducting psychoeducational treatment groups for patients at Cornerstone of Recovery for a maximum of 4 hours per week. None of this research project pertains to any of the psychoeducational groups. Dr. Stuart does not ever do any study recruitment, is not informed which patients do or do not participate in research, and does not mention anything about research to the patients attending groups. Ryan Shorey started working as a research consultant at Cornerstone. There is no restriction on what Ryan can publish and his research consultation does not influence the study results in any way. Ryan does not interact with Cornerstone patients. Ryan has reported all of his consultation activities to Ohio University and no concern about financial conflict of interest has been raised. Scott Anderson is employed as the Chief Clinical Officer/Clinical Director at Cornerstone of Recovery. His positions do not influence the study results in any way. Meagan Brem declares no conflict of interest.
Compliance with Ethical Standards
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Author contributions: First author: formulated the hypothesis, analyzed the data, and wrote the manuscript. Second author: collaborated with the analyses, writing, and editing of the manuscript. Third author: collaborated with the writing and editing of the manuscript. Fourth author: collaborated with the writing and editing of the manuscript.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park: Sage; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guideline for use in primary care. 2. Geneva: World Health Organization; 2001. [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10(2):125–143. doi: 10.1093/clipsy.bpg015. [DOI] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Walsh E, Duggan D, Williams JMG. Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal ZV, Abbey S, Speca M, Velting D, Devins G. Mindfulness: A Proposed Operational Definition. Clinical Psychology: Science and Practice. 2004;11(3):230–241. doi: 10.1093/clipsy.bph077. [DOI] [Google Scholar]
- Bowlin SL, Baer RA. Relationships between mindfulness, self-control, and psychological functioning. Personality and Individual Differences. 2012;52(3):411. [Google Scholar]
- Brem MJ, Shorey RC, Anderson S, Stuart GL. Depression, anxiety, and compulsive sexual behavior among men in residential treatment for substance use disorders: The role of experiential avoidance. Journal of Clinical Psychology and Psychotherapy. doi: 10.1002/cpp.2085. in press. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Carnes P. Don’t call it love. New York: Bantam Books; 1991. [Google Scholar]
- Carnes P. Out of the shadows: Understanding sexual addiction. Center City, MN: Hazelden Publishing; 2001. [Google Scholar]
- Carnes P, Green B, Carnes S. The same yet different: Refocusing the Sexual Addiction Screening Test (SAST) to reflect orientation and gender, sexual addiction and compulsivity. The Journal of Treatment and Prevention. 2010;17(1):7–30. [Google Scholar]
- Chiesa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use and Misuse. 2014;49(5):492–512. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Cockram DM, Drummond PD, Lee CW. Role and treatment of early maladaptive schemas in Vietnam veterans with PTSD. Clinical Psychology & Psychotherapy. 2010;17(3):165–182. doi: 10.1002/cpp.690. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Dakwar E, Mariani JP, Levin FR. Mindfulness impairments in individuals seeking treatment for substance use disorders. The American Journal of Drug and Alcohol Abuse. 2011;37(3):165–169. doi: 10.3109/00952990.2011.553978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearing RL, Stuewig J, Tangney JP. On the importance of distinguishing shame from guilt: Relations to problematic alcohol and drug use. Addictive Behaviors. 2005;30(7):1392–1404. doi: 10.1016/j.addbeh.2005.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derbyshire KL, Grant JE. Compulsive sexual behavior: A review of the literature. Journal of Behavioral Addictions. 2015;4(2):37–43. doi: 10.1556/2006.4.2015.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P. What is shame? Some core issues and controversies. In: Gilbert P, Andrews B, editors. Shame: Interpersonal behavior, psychopathology and culture. New York: Oxford University Press; 1998. pp. 3–36. [Google Scholar]
- Gilliland R, South M, Carpenter BN, Hardy SA. The roles of shame and guilt in hypersexual behavior. Sexual Addiction and Compulsivity: The Journal of Treatment & Prevention. 2011;18(1):12–29. doi: 10.1080/10720162.2011.551182. [DOI] [Google Scholar]
- Hall PA. A biopsychosocial view of sex addiction. Sexual and Relationship Therapy. 2011;26(3):217–228. [Google Scholar]
- Hawke LD, Provencher MD. Schema theory and schema therapy in mood and anxiety disorders: A review. Journal of Cognitive Psychotherapy. 2011;25(4):257–276. doi: 10.1891/0889-8391.27.4.359. [DOI] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White Paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Hayes AM, Feldman G. Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology: Science and Practice. 2004;11(3):255–262. doi: 10.1093/clipsy.bph080. [DOI] [Google Scholar]
- Kafka MP. Hypersexual disorder: A proposed diagnosis for DSM-V. Archives of Sexual Behavior. 2010;39:377–400. doi: 10.1007/s10508-009-9574-7. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Twohig MP, Waltz T, Hayes SC, Roget N, Padilla M, Fisher G. An investigation of stigma in individuals receiving treatment for substance abuse. Addictive Behaviors. 2007;32(7):1331–1346. doi: 10.1016/j.addbeh.2006.09.008. [DOI] [PubMed] [Google Scholar]
- Masuma R, Patton R. The association between shame and substance use in young people: A systematic review. PeerJ. 2015;3:e737. doi: 10.7717/peerj.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff K. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity. 2003;2(2):85–101. [Google Scholar]
- Oei TPS, Baranoff J. Young schema questionnaire: review of psychometric and measurement issues. Australian Journal of Psychology. 2007;59:78–86. [Google Scholar]
- Pinto-Gouveia J, Castilho P, Galhardo A, Cunha M. Early maladaptive schemas and social phobia. Cognitive Therapy and Research. 2006;30(5):571–584. [Google Scholar]
- Potter-Efron RT. Shame, guilt, and alcoholism: treatment in clinical practice. NY: Haworth Press; 2002. [Google Scholar]
- Reid RC. Differentiating emotions in a sample of men in treatment for hypersexual behavior. Journal of Social Work Practice in the Addictions. 2010;10(2):197–213. doi: 10.1080/15332561003769369. [DOI] [Google Scholar]
- Reid RC, Bramen JE, Anderson A, Cohen MS. Mindfulness, emotion dysregulation, impulsivity, and stress proneness among hypersexual patients. Journal of Clinical Psychology. 2014;70(4):313–321. doi: 10.1002/jclp.22027. [DOI] [PubMed] [Google Scholar]
- Reid RC, Carpenter BN. Exploring relationships of psychopathology in hypersexual patients using the MMPI–2. Journal of Sex and Marital Therapy. 2009;35:294–310. doi: 10.1080/00926230902851298. [DOI] [PubMed] [Google Scholar]
- Reid RC, Harper JM, Anderson EH. Coping strategies used by hypersexual patients to defend against the painful effects of shame. Clinical Psychology & Psychotherapy. 2009;16:125–138. doi: 10.1002/cpp.609. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Jr, Joiner TE, Young JE, Telch MJ. The schema questionnaire: Investigation of psychometric properties and the hierarchical structure of a measure of maladaptive schemas. Cognitive Therapy and Research. 1995;19(3):295–321. [Google Scholar]
- Schneider JP, Irons RR. Assessment and treatment of addictive sexual disorders: Relevance for chemical dependency relapse. Substance Use & Misuse. 2001;36(13):1795–1820. doi: 10.1081/JA-100108428. [DOI] [PubMed] [Google Scholar]
- Shorey RC, Elmquist J, Anderson S, Stuart GL. The relationship between early maladaptive schemas, depression, and generalized anxiety among adults seeking residential treatment for substance use disorders. Journal of Psychoactive Drugs. 2015;47(3):230–238. doi: 10.1080/02791072.2015.1050133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, Elmquist J, Gawrysiak MJ, Anderson S, Stuart GL. The relationship between mindfulness and compulsive sexual behavior in a sample of men in treatment for substance use disorders. Mindfulness. 2016;7:866–873. doi: 10.1007/s12671-016-0525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stavro K, Rizkallah E, Dinh-Williams L, Chiasson J, Potvin S. Hypersexuality among a substance use disorder population. Sexual Addiction and Compulsivity. 2013;20(3):210–216. [Google Scholar]
- Stuart GL, Moore TM, Kahler CW, Ramsey SE. Substance abuse and relationship violence among men court-referred to batterers’ intervention programs. Substance Abuse. 2003a;24(2):107–122. doi: 10.1080/08897070309511539. [DOI] [PubMed] [Google Scholar]
- Stuart GL, Moore TM, Ramsey SE, Kahler CW. Relationship aggression and substance use among women court-referred to domestic violence intervention programs. Addictive Behaviors. 2003b;28(9):1603–1610. doi: 10.1016/j.addbeh.2003.08.038. [DOI] [PubMed] [Google Scholar]
- Tangney JP, Dearing RL. Shame and guilt. NY: Guilford Press; 2002. [Google Scholar]
- Tull MT, Weiss NH, Adams CE, Gratz KL. The contribution of emotion regulation difficulties to risky sexual behavior within a sample of patients in residential substance abuse treatment. Addictive Behaviors. 2012;37(10):1084–1092. doi: 10.1016/j.addbeh.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gordon W, Shonin E, Griffiths MD. Meditation awareness training for the treatment of sex addiction: A case study. Journal of Behavioral Addictions. 2016;5(2):363–372. doi: 10.1556/2006.5.2016.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods H, Proeve M. Relationships of mindfulness, self-compassion, and meditation experience with shame-proneness. Journal of Cognitive Psychotherapy: An International Quarterly. 2014;28(1):20–33. doi: 10.1891/0889-8391.28.1.20. [DOI] [PubMed] [Google Scholar]
- Young JE, Brown G. Young schema questionnaire. NY: Cognitive Therapy Center of New York; 2003. [Google Scholar]