Abstract
Dobutamine is the inotrope most commonly used in septic shock patients to increase cardiac output and correct hypoperfusion. Although some experimental and clinical studies have shown that dobutamine can improve systemic and regional hemodynamics, other research has found that its effects are heterogenous and unpredictable. In this review, we analyze the pharmacodynamic properties of dobutamine and its physiologic effects. Our goal is to show that the effects of dobutamine might differ between healthy subjects, in experimental and clinical cardiac failure, in animal models and in patients with septic shock. We discuss evidence supporting the claim that dobutamine, in septic shock, frequently behaves as a chronotropic and vasodilatory drug, without evidence of inotropic action. Since the side effects are very common, and the therapeutic benefits are unclear, we suggest that dobutamine should be used cautiously in septic shock. Before a definitive therapeutic decision, the efficacy and tolerance of dobutamine should be assessed during a brief time with close monitoring of its positive and negative side effects.
Keywords: Dobutamine; Sepsis; Shock, septic; Cardiac output; Blood pressure; Microcirculation
Abstract
A dobutamina é o inotrópico mais comumente utilizado em pacientes com choque séptico, com o objetivo de aumentar o débito cardíaco e corrigir a hipoperfusão. Embora alguns ensaios clínicos tenham demonstrado que a dobutamina pode melhorar a hemodinâmica sistêmica e regional, outras pesquisas identificaram que seus efeitos são heterogêneos e imprevisíveis. Nesta revisão, analisamos as propriedades farmacodinâmicas da dobutamina e seus efeitos fisiológicos. Nosso objetivo foi demonstrar que os efeitos da dobutamina podem diferir entre voluntários saudáveis, estudos experimentais e insuficiência cardíaca clínica, em modelos de estudo em animais e em pacientes com choque séptico. Discutimos as evidências que suportam a afirmativa de que a dobutamina utilizada no tratamento do choque séptico frequentemente se comporta como fármaco cronotrópico e vasodilatador, sem evidências de ação inotrópica. Como seus efeitos colaterais são muito comuns e os benefícios terapêuticos não são claros, sugerimos que ela deve ser utilizada com cautela no choque séptico. Antes de uma decisão terapêutica definitiva, a eficácia e a tolerabilidade da dobutamina devem ser avaliadas por um tempo curto com monitoramento estrito de seus efeitos positivos e efeitos colaterais negativos.
Keywords: Dobutamina, Sepse, Choque séptico, Débito cardíaco, Pressão sanguínea, Microcirculação
INTRODUCTION
The main goal of resuscitation in septic shock is the normalization of tissue perfusion through the administration of fluids, vasopressors, and inotropes. Dobutamine is the first-line inotropic drug recommended by the Surviving Sepsis Campaign.(1) According to these guidelines, a trial of dobutamine infusion, up to 20µg/kg/min, should be administered or added to the vasopressor (if in use) in the presence of (a) myocardial dysfunction, as suggested by elevated cardiac filling pressures and low cardiac output, or (b) ongoing signs of hypoperfusion, despite achieving adequate intravascular volume and adequate mean arterial pressure.
Nevertheless, the clinical evidence supporting the beneficial effects of dobutamine on outcomes in septic patients is rather limited. The recommendations are based mainly on the first randomized controlled trial of early goal-directed therapy, in which only 14% of the patients received dobutamine.(2) Moreover, some studies suggest that dobutamine has a low safety profile. A retrospective analysis of 420 patients with septic shock showed that the use of dobutamine was independently associated with increased 90-day mortality, even after adjustment, with a propensity score, for the inotropic treatment.(3) In patients with severe heart failure, a meta-analysis also showed a trend towards worse outcomes with its use.(4) Moreover, some observational studies found that dobutamine might cause variable hemodynamics effects and frequent side effects.(5-7)
Although dobutamine has been used for four decades in the treatment of septic shock,(8) its pharmacodynamics is not well understood. The purpose of this review is to revisit some aspects of its clinical pharmacology. Our goal is to show that the effects of dobutamine are frequently unpredictable, heterogeneous, and dependent on the underlying condition.
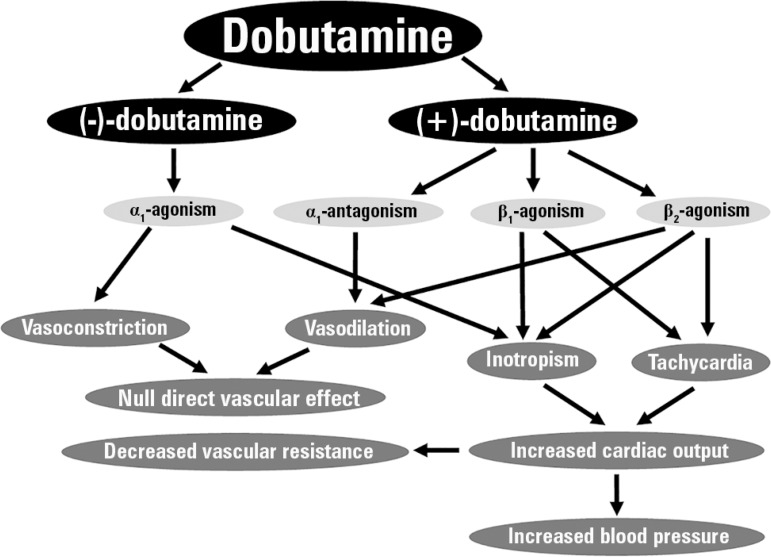
EFFECTS OF DOBUTAMINE IN NORMAL SUBJECTS
Dobutamine is used clinically as a racemic mixture.(9-11) As such, the pharmacodynamic activity of the racemate will result from the interaction of the individual properties of the stereoisomers. (-)-dobutamine is a powerful adrenergic α1 agonist with weak β1 and β2 activity. In contrast, (+)-dobutamine predominantly stimulates β1 and β2 adrenoreceptors and exhibits α1 antagonist activity. Consequently, (±)-dobutamine mainly behaves as an inotrope. Since a significant part of the inotropic effect is related to increased cardiac α1 activity, dobutamine results in less tachycardia than other adrenergic drugs. In addition, there is no direct effect on vascular tone because of the opposing effects of each enantiomer: (-)-dobutamine is a vasoconstrictor, and (+)-dobutamine is a vasodilator. Accordingly, the decreases in vascular tone and peripheral resistance are adaptive adjustments to the simultaneous increases in cardiac output. Figure 1 summarizes the main pharmacodynamic and cardiovascular effects of dobutamine.
Figure 1.
Schematic of the main pharmacodynamic and cardiovascular effects of dobutamine.
In healthy animals, dobutamine primarily increases stroke volume and cardiac output because of its inotropic effects. There is also a small increase in heart rate that is a minor contribution to the increase in cardiac output. The increased cardiac output induces an elevation in blood pressure and a reflex decrease in systemic vascular resistance.(11,12)
In healthy volunteers, increasing the dose of dobutamine results in elevated cardiac output, which is linearly related to its plasma concentrations.(13) The relationships between heart rate and stroke volume to plasma concentrations, however, are more complex. Heart rate initially remains unchanged and then increases with higher concentrations, while stroke volume only increases at lower concentrations. Thus, cardiac output and blood pressure are linearly related to increasing doses of dobutamine. With 2.5µg/kg/min, both variables increase because of improved stroke volume. Further increases with higher doses only depend on tachycardia.
Beyond its hemodynamic effects, dobutamine produces a marked calorigenic effect, which is the consequence of complex α and β adrenergic metabolic effects. An infusion of 10µg/kg/min induces a rise in energy expenditure of 33% and a decrease in respiratory quotient secondary to increased fat metabolism.(14)
EFFECTS OF DOBUTAMINE IN CARDIAC FAILURE
In some experimental models of cardiogenic shock, the actions of dobutamine are similar to those described in healthy subjects: increased cardiac output and blood pressure. In dogs with reduced cardiac contractility, low cardiac output, and hypotension, dobutamine produces dose-related increases in cardiac contractility and output, restores arterial blood pressure, and reduces total peripheral resistance.(15)
In patients with different forms of cardiac failure, however, the effects are not the same.(16-18) Despite cardiac output improving, blood pressure does not increase. This finding suggests an unexpected primary effect on vascular tone and peripheral resistance not observed in either healthy subjects or models of experimental cardiogenic shock. In these circumstances, the augmentation in cardiac output goes together with elevations in blood pressure.(11-13)
EFFECTS OF DOBUTAMINE IN SEPTIC SHOCK
In septic shock, dobutamine is typically used to increase cardiac output and oxygen transport. Since dobutamine has a thermogenic effect,(14) it has also been used to evaluate the metabolic state of critically ill patients-the so-called dobutamine oxygen flux test. Some clinical studies found that the lack of increase in oxygen consumption in response to dobutamine is associated with worse outcomes, as an indication of a severe underlying cell disorder.(19,20) Unfortunately, the clinical usefulness of this assessment has not been adequately established.
Even though dobutamine is recommended in septic shock to improve cardiac output and correct hypoperfusion,(1) there are controversial reports about its effects in this setting. Several experimental and clinical studies showed beneficial effects on systemic hemodynamics.(21-24) Moreover, increases in splanchnic perfusion and tissue oxygenation have also been found.(25-29) A study performed in patients with septic shock showed that dobutamine increased oxygen transport, together with improvements in intramucosal acidosis and hyperlactatemia.(27) In addition, dobutamine might be useful for the recruitment of microcirculation. In endotoxemic rats, dobutamine prevented the development of arteriolar constriction and maintained villus blood flow.(30) Similar results were described in the hepatic sinusoidal microcirculation.(31) In patients with septic shock, an infusion of 5µg/kg/min for 2 hours improved sublingual microcirculation.(32) Interestingly, the microvascular effects were not correlated with changes in blood pressure or cardiac output.
Nevertheless, some data suggest that the effects of dobutamine in septic shock are not so predictable. The inotropic effect could be blunted in sepsis. An experimental study showed that the inotropic, but not the chronotropic, effect was reduced after an endotoxin challenge.(21)
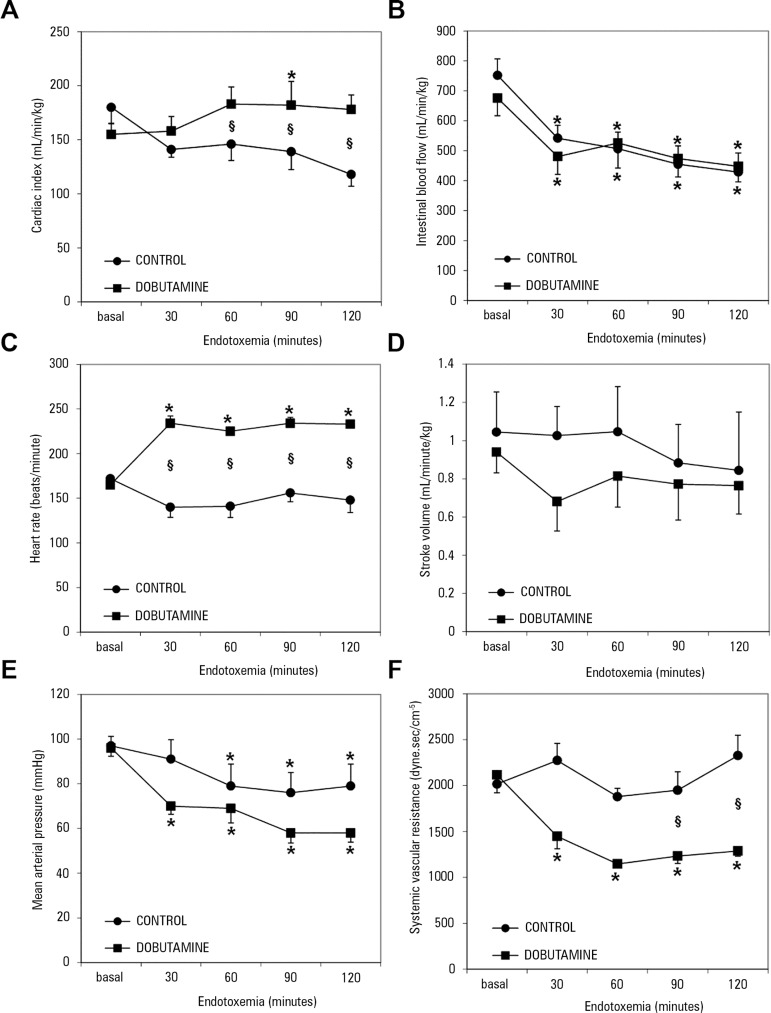
A study performed in sheep endotoxemia showed that dobutamine increased cardiac output but decreased the fraction of blood flow directed to the gut.(33) Moreover, the effect on cardiac output was completely explained by tachycardia, since the stroke volume was unchanged. In addition, there were decreases in blood pressure and systemic vascular resistance. The reduction in blood pressure and systemic vascular resistance, along with preserved cardiac output, imply that dobutamine primarily caused vasodilation (Figure 2). In this study, dobutamine induced vasodilation and tachycardia but did not show evidence of an inotropic effect. Furthermore, there was no improvement in gut perfusion. Similarly, in an experimental model of partial superior mesenteric artery occlusion, dobutamine, without fluid resuscitation, increased cardiac output but decreased the fraction of blood flow directed to the superior mesenteric artery and worsened intramucosal pH and the portal venous-arterial lactate gradient.(34)
Figure 2.
Behavior of hemodynamic variables in control and dobutamine-treated endotoxemic sheep. (A) Cardiac index; (B) superior mesenteric artery blood flow; (C) heart rate; (D) stroke volume; (E) Mean arterial pressure; (F) systemic vascular resistance.
Source: Modified from: Dubin A, Murias G, Sottile JP, Pozo MO, Barán M, Edul VS, et al. Effects of levosimendan and dobutamine in experimental acute endotoxemia: a preliminary controlled study. Intensive Care Med. 2007;33(3):485-94.(33)
In patients with septic shock, dobutamine might produce severe vasodilation. This phenomenon was evident in a randomized controlled trial in which 5 - 200µg/kg/min of dobutamine were used to reach supranormal values of oxygen transport. This therapeutic approach not only increased mortality, but larger doses of norepinephrine were also required in patients assigned to the dobutamine arm compared to the control group.(35) Accordingly, maximal doses of norepinephrine were 1.20 versus 0.23µg/kg/min, respectively. In three large, randomized controlled trials in which dobutamine was used as part of the EGDT, no side effects related to dobutamine were reported.(36-38) Nevertheless, the higher requirements for vasopressors in the EGDT group compared to the control group might reflect dobutamine-induced vasodilation.
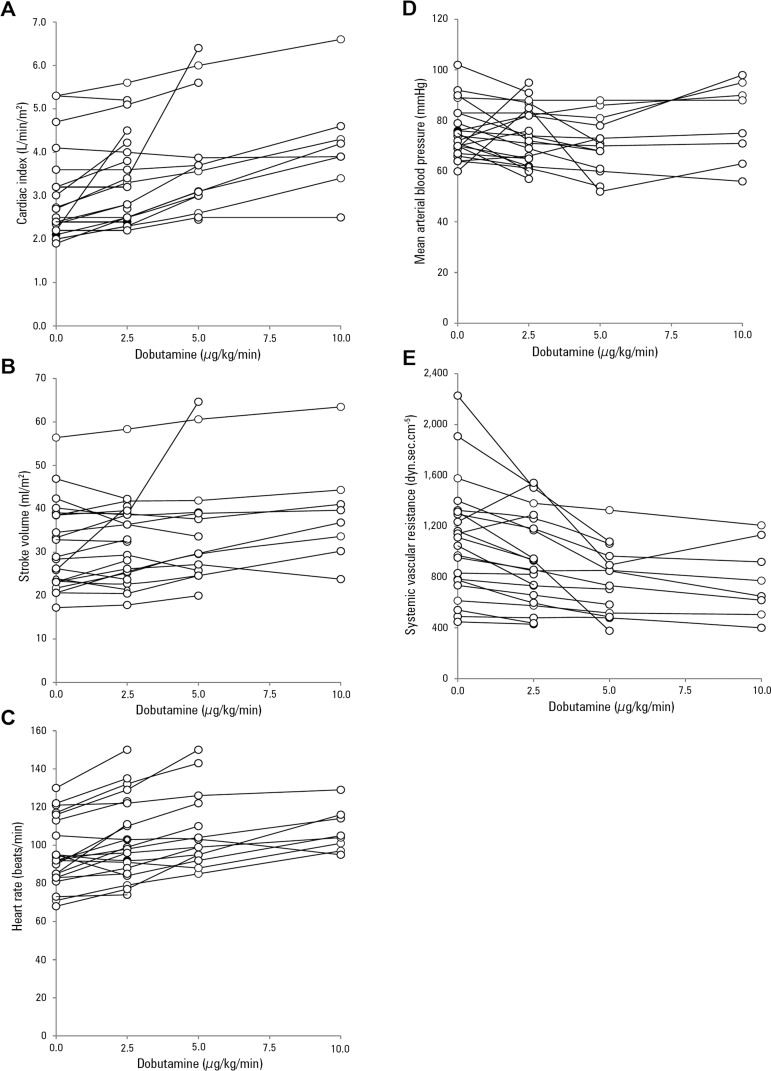
Few clinical studies attempted to identify heterogeneous cardiovascular responses, taking into account individual responses. In these observational studies, the use of dobutamine was associated with erratic responses and frequent side effects.(5-7) In one of these studies, 19 trials of increasing doses of dobutamine were carried out in 12 patients.(5) In 12 cases, dobutamine was suspended because of hypotension or tachycardia. Most of the patients did not have increased stroke volume. Another study also showed unpredictable cardiovascular effects.(6) Again, in most of the patients, dobutamine produced tachycardia and vasodilation without inotropic effects.
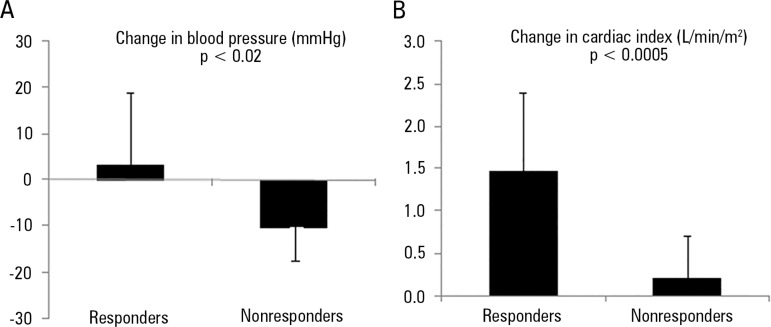
The third study assessed the effects of increasing doses of dobutamine in 23 patients with septic shock.(7) The responses of hemodynamic variables to dobutamine were dichotomized according to changes greater than or less than 10% from baseline to the maximal dose. The maximal dosage of 10µg/kg/min was only reached in 8 patients. In most of the patients, the study could not be completed because of the occurrence of side effects, mainly decreases in blood pressure and increases in heart rate. Dobutamine increased cardiac output in 70% of the patients. There were opposite effects on mean arterial blood pressure: it decreased in 43% of the patients and increased in 22% of them. Stroke volume only improved in half of the patients. In most of the patients, the heart rate increased, and systemic vascular resistance decreased (Figure 3). There were no differences in baseline hemodynamics between patients with increased stroke volume in response to dobutamine and non-responders. Stroke volume responders, however, had lower left ventricle ejection fraction and more frequently showed systolic dysfunction and severe systolic dysfunction than non-responders did. Accordingly, the stroke volume changes in response to dobutamine correlated with baseline left ventricle ejection fraction. Stroke volume responders had a large increase in cardiac index and a trend toward increased blood pressure. In non-responders, cardiac output remained almost unchanged and blood pressure fell. These findings indicate that dobutamine behaved as an inotrope in responders, while it was only a vasodilator without inotropic effects in non-responders (Figure 4).
Figure 3.
Individual behavior of hemodynamic variables in patients with septic shock treated with increasing doses of dobutamine. (A) Cardiac index; (B) stroke volume; (C) heart rate; (D) mean arterial pressure; (E) systemic vascular resistance.
Source: Modified from: Enrico C, Kanoore Edul VS, Vazquez AR, Pein MC, Pérez de la Hoz RA, Ince C, et al. Systemic and microcirculatory effects of dobutamine in patients with septic shock. J Crit Care. 2012;27(6):630-8.(7)
Figure 4.
Difference in hemodynamic behavior of stroke volume-responder and non-responder patients with septic shock at the maximal dosage of dobutamine. In responders, dobutamine behaved as an inotrope, increasing blood pressure and cardiac index. In non-responders, dobutamine mainly acted as a vasodilator, since blood pressure decreased, and cardiac index marginally increased. (A) Change in mean arterial pressure; (B) change in cardiac index.
Source: Based on the publication data: Enrico C, Kanoore Edul VS, Vazquez AR, Pein MC, Pérez de la Hoz RA, Ince C, et al. Systemic and microcirculatory effects of dobutamine in patients with septic shock. J Crit Care. 2012;27(6):630-8.(7)
This study also evaluated the effects of dobutamine on sublingual microcirculation. In the group as a whole, there were no significant changes in microcirculatory variables. Nevertheless, there were variable individual responses. The behavior of the microcirculation was independent of systemic hemodynamics. The changes in perfused capillary density were not correlated with changes in either cardiac output or blood pressure. In contrast, changes were dependent on the basal state of the microcirculation. Therefore, patients with a compromised microcirculation at baseline had a positive response to dobutamine. On the other hand, a controlled crossover trial in patients with septic shock found detrimental effects of dobutamine on muscle and hepatic perfusion, a lack of improvement in peripheral perfusion, and a nonsignificant trend toward an increase in the proportion of perfused sublingual capillaries.(39)
The explanations for the heterogeneous responses to dobutamine in septic shock remain unclear. A putative reason is the inconstant pathophysiologic pattern of septic shock. The hemodynamic profile of septic shock results from interactions among variable components of hypovolemia, alterations in vascular tone, and myocardial dysfunction. After fluid resuscitation, most of the patients show hypotension, tachycardia, and normal or high cardiac output. Despite preserved systemic oxygen transport, septic shock patients frequently die from multiple organ failure or cardiovascular collapse. Typically, death from septic shock is related to the persistence of a hyperdynamic state with progressive and refractory vasodilation.(40) Septic patients die from the inability to regulate peripheral circulation, not from low cardiac output. In this context, myocardial dysfunction may be a contributor to the hemodynamic instability but not the main cause. In addition, cardiac alterations in septic shock comprise systolic and diastolic dysfunction,(41) dynamic left intraventricular obstruction,(42) and acute stress cardiomyopathy.(43) Diastolic dysfunction is common in septic patients (48%) and is related to increased mortality. In contrast, systolic dysfunction is less frequent (30%) and does not influence outcomes.(41) Dynamic left intraventricular obstruction is found in 22% of patients with septic shock and is associated with poorer outcome.(42) Only systolic dysfunction can be improved with the use of dobutamine; diastolic dysfunction, dynamic left intraventricular obstruction, and acute stress cardiomyopathy might be worsened. Therefore, dobutamine will not be useful for most of the cardiac alterations in septic shock. As supported by the results of an observational study,(7) only patients with systolic dysfunction have positive responses in stroke volume. This observation might be an explanation for the heterogeneous responses to dobutamine.
Nevertheless, several other factors might contribute to the variability in responses. Sepsis is characterized by alterations in the adrenergic receptors, which subsequently may modify the response to catecholamines.(44-46) Genetic polymorphisms might also be involved in the hemodynamic response. In healthy individuals, resting heart rate responses to 6µg/kg/min of dobutamine were 4.7-fold larger in Arg389Arg than in Gly389Gly homozygotes.(47) Another study showed that dobutamine resulted in larger heart rate and contractility increases and diastolic blood pressure decreases in Arg389- versus Gly389-beta1AR subjects.(48) On the other hand, it has been reported that polymorphisms do not substantially influence the magnitude of hemodynamic response to dobutamine during dobutamine stress echocardiography.(49) In addition, a blunted inotropic, but preserved or increased chronotropic, response to dobutamine, has been associated with the aging process.(50,51) The age-related decreases in contractile function in response to dobutamine might be explained by an inability to increase myocardial glucose utilization.(51) An assessment, by means of cardiac magnetic resonance imaging, showed that dobutamine markedly decreased the passive left atrial emptying function and correspondingly increased the active emptying function in older adults (60 - 70 years) but not in young (20 - 30 years) healthy subjects.(52) Accordingly, older adults had lower cardiac output during dobutamine stress. Finally, women might have an increased chronotropic response,(53) but the data are inconclusive.(54)
CONCLUSIONS
Patients with septic shock commonly display varying responses to dobutamine. Frequently, vasodilation and tachycardia are the most prominent effects without evidence of improved cardiac performance. These findings suggest a low profile of efficacy and safety. In addition, the effects on regional and microcirculatory perfusion are also unpredictable. The presence of echocardiographic systolic dysfunction and severe microvascular disorders could help in the identification of patients who would benefit from the use of dobutamine. Before a definitive therapeutic decision, efficacy of and tolerance to dobutamine should be evaluated during a brief time with close monitoring of its positive and negative effects.
Footnotes
Conflicts of interest: None.
Responsible editor: Gilberto Friedman
REFERENCES
- 1.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med. 2017;5(3):486–552. doi: 10.1097/CCM.0000000000002255. [DOI] [PubMed] [Google Scholar]
- 2.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 3.Wilkman E, Kaukonen KM, Pettilä V, Kuitunen A, Varpula M. Association between inotrope treatment and 90-day mortality in patients with septic shock. Acta Anaesthesiol Scand. 2013;57(4):431–442. doi: 10.1111/aas.12056. [DOI] [PubMed] [Google Scholar]
- 4.Tacon CL, McCaffrey J, Delaney A. Dobutamine for patients with severe heart failure: a systematic review and meta-analysis of randomised controlled trials. Intensive Care Med. 2012;38(3):359–367. doi: 10.1007/s00134-011-2435-6. [DOI] [PubMed] [Google Scholar]
- 5.Jellema WT, Groeneveld AB, Wesseling KH, Thijs LG, Westerhof N, van Lieshout JJ. Heterogeneity and prediction of hemodynamic responses to dobutamine in patients with septic shock. Crit Care Med. 2006;34(9):2392–2398. doi: 10.1097/01.CCM.0000233871.52553.CD. [DOI] [PubMed] [Google Scholar]
- 6.Kumar A, Schupp E, Bunnell E, Ali A, Milcarek B, Parrillo JE. Cardiovascular response to dobutamine stress predicts outcome in severe sepsis and septic shock. Crit Care. 2008;12(2):R35–R35. doi: 10.1186/cc6814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Enrico C, Kanoore Edul VS, Vazquez AR, Pein MC, Pérez de la Hoz RA, Ince C, et al. Systemic and microcirculatory effects of dobutamine in patients with septic shock. J Crit Care. 2012;27(6):630–638. doi: 10.1016/j.jcrc.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Dupeyron JP, Pottecher T, Haberer JP, Gauthier-Lafaye JP. Use of dobutamine in the treatment of septic shock. Anesth Analg (Paris) 1977;34(5):917–927. French. [PubMed] [Google Scholar]
- 9.Ruffolo RR Jr, Spradlin TA, Pollock GD, Waddell JE, Murphy PJ. Alpha and beta adrenergic effects of the stereoisomers of dobutamine. J Pharmacol Exp Ther. 1981;219(2):447–452. [PubMed] [Google Scholar]
- 10.Ruffolo RR Jr, Yaden EL. Vascular effects of the stereoisomers of dobutamine. J Pharmacol Exp Ther. 1983;224(1):46–50. [PubMed] [Google Scholar]
- 11.Ruffolo RR Jr, Messick K. Systemic hemodynamic effects of dopamine, (+/-)-dobutamine and the (+)-and (-)- enantiomers of dobutamine in anesthetized normotensive rats. Eur J Pharmacol. 1985;109(2):173–181. doi: 10.1016/0014-2999(85)90418-2. [DOI] [PubMed] [Google Scholar]
- 12.Robie NW, Nutter DO, Moody C, McNay JL. In vivo analysis of adrenergic receptor activity of dobutamine. Circ Res. 1974;34(5):663–671. doi: 10.1161/01.res.34.5.663. [DOI] [PubMed] [Google Scholar]
- 13.Ahonen J, Aranko K, Iivanainen A, Maunuksela EL, Paloheimo M, Olkkola KT. Pharmacokinetic-pharmacodynamic relationship of dobutamine and heart rate, stroke volume and cardiac output in healthy volunteers. Clin Drug Investig. 2008;28(2):121–127. doi: 10.2165/00044011-200828020-00006. [DOI] [PubMed] [Google Scholar]
- 14.Green CJ, Frazer RS, Underhill S, Maycock P, Fairhurst JA, Campbell IT. Metabolic effects of dobutamine in normal man. Clin Sci (Lond) 1992;82(1):77–83. doi: 10.1042/cs0820077. [DOI] [PubMed] [Google Scholar]
- 15.Tuttle RR, Mills J. Dobutamine: development of a new catecholamine to selectively increase cardiac contractility. Circ Res. 1975;36(1):185–196. doi: 10.1161/01.res.36.1.185. [DOI] [PubMed] [Google Scholar]
- 16.Beregovich J, Bianchi C, D'Angelo R, Diaz R, Rubler S. Haemodynamic effects of a new inotropic agent (dobutamine) in chronic cardiac failure. Br Heart J. 1975;37(6):629–634. doi: 10.1136/hrt.37.6.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stoner 3rd JD, Bolen JL, Harrison DC. Comparison of dobutamine and dopamine in treatment of severe heart failure. Br Heart J. 1977;39(5):536–539. doi: 10.1136/hrt.39.5.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fowler MB, Timmis AD, Crick JP, Vincent R, Chamberlain DA. Comparison of haemodynamic responses to dobutamine and salbutamol in cardiogenic shock after acute myocardial infarction. Br Med J (Clin Res Ed) 1982;284(6309):73–76. doi: 10.1136/bmj.284.6309.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vallet B, Chopin C, Curtis SE, Dupuis BA, Fourrier F, Mehdaoui H, et al. Prognostic value of the dobutamine test in patients with sepsis syndrome and normal lactate values: a prospective, multicenter study. Crit Care Med. 1993;21(12):1868–1875. doi: 10.1097/00003246-199312000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Rhodes A, Lamb FJ, Malagon I, Newman PJ, Grounds RM, Bennett ED. A prospective study of the use of a dobutamine stress test to identify outcome in patients with sepsis, severe sepsis, or septic shock. Crit Care Med. 1999;27(11):2361–2366. doi: 10.1097/00003246-199911000-00007. [DOI] [PubMed] [Google Scholar]
- 21.McCaig D, Parratt JR. A comparison of the cardiovascular effects of dobutamine and a new dopamine derivative (D4975) during shock induced by E. coli endotoxin. Br J Pharmacol. 1980;69(4):651–656. doi: 10.1111/j.1476-5381.1980.tb07917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vincent JL, Van der Linden P, Domb M, Blecic S, Azimi G, Bernard A. Dopamine compared with dobutamine in experimental septic shock: relevance to fluid administration. Anesth Analg. 1987;66(6):565–571. [PubMed] [Google Scholar]
- 23.Regnier B, Safran D, Carlet J, Teisseire B. Comparative haemodynamic effects of dopamine and dobutamine in septic shock. Intensive Care Med. 1979;5(3):115–120. doi: 10.1007/BF01683192. [DOI] [PubMed] [Google Scholar]
- 24.Jardin F, Sportiche M, Bazin M, Bourokba A, Margairaz A. Dobutamine: a hemodynamic evaluation in human septic shock. Crit Care Med. 1981;9(4):329–332. [PubMed] [Google Scholar]
- 25.Nevière R, Chagnon JL, Vallet B, Lebleu N, Marechal X, Mathieu D, et al. Dobutamine improves gastrointestinal mucosal blood flow in a porcine model of endotoxic shock. Crit Care Med. 1997;25(8):1371–1377. doi: 10.1097/00003246-199708000-00026. [DOI] [PubMed] [Google Scholar]
- 26.Nevière R, Mathieu D, Chagnon JL, Lebleu N, Wattel F. The contrasting effects of dobutamine and dopamine on gastric mucosal perfusion in septic patients. Pt 1Am J Respir Crit Care Med. 1996;154(6):1684–1688. doi: 10.1164/ajrccm.154.6.8970355. [DOI] [PubMed] [Google Scholar]
- 27.Gutierrez G, Clark C, Brown SD, Price K, Ortiz L, Nelson C. Effect of dobutamine on oxygen consumption and gastric mucosal pH in septic patients. Am J Respir Crit Care Med. 1994;150(2):324–329. doi: 10.1164/ajrccm.150.2.8049810. [DOI] [PubMed] [Google Scholar]
- 28.Levy B, Nace L, Bollaert PE, Dousset B, Mallie JP, Larcan A. Comparison of systemic and regional effects of dobutamine and dopexamine in norepinephrine-treated septic shock. Intensive Care Med. 1999;25(9):942–948. doi: 10.1007/s001340050986. [DOI] [PubMed] [Google Scholar]
- 29.Joly LM, Monchi M, Cariou A, Chiche JD, Bellenfant F, Brunet F, et al. Effects of dobutamine on gastric mucosal perfusion and hepatic metabolism in patients with septic shock. Am J Respir Crit Care Med. 1999;160(6):1983–1986. doi: 10.1164/ajrccm.160.6.9708113. [DOI] [PubMed] [Google Scholar]
- 30.Secchi A, Wellmann R, Martin E, Schmidt H. Dobutamine maintains intestinal villus blood flow during normotensive endotoxemia: an intravital microscopic study in the rat. J Crit Care. 1997;12(3):137–141. doi: 10.1016/s0883-9441(97)90043-5. [DOI] [PubMed] [Google Scholar]
- 31.Secchi A, Ortanderl JM, Schmidt W, Walther A, Gebhard MM, Martin E, et al. Effects of dobutamine and dopexamine on hepatic micro- and macrocirculation during experimental endotoxemia: an intravital microscopic study in the rat. Crit Care Med. 2001;29(3):597–600. doi: 10.1097/00003246-200103000-00023. [DOI] [PubMed] [Google Scholar]
- 32.De Backer D, Creteur J, Dubois MJ, Sakr Y, Koch M, Verdant C, et al. The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit Care Med. 2006;34(2):403–408. doi: 10.1097/01.ccm.0000198107.61493.5a. [DOI] [PubMed] [Google Scholar]
- 33.Dubin A, Murias G, Sottile JP, Pozo MO, Barán M, Edul VS, et al. Effects of levosimendan and dobutamine in experimental acute endotoxemia: a preliminary controlled study. Intensive Care Med. 2007;33(3):485–494. doi: 10.1007/s00134-006-0519-5. [DOI] [PubMed] [Google Scholar]
- 34.Heino A, Hartikainen J, Merasto ME, Koski EM, Tenhunen J, Alhava E, et al. Effects of dobutamine on splanchnic tissue perfusion during partial superior mesenteric artery occlusion. Crit Care Med. 2000;28(10):3484–3490. doi: 10.1097/00003246-200010000-00020. [DOI] [PubMed] [Google Scholar]
- 35.Hayes MA, Timmins AC, Yau EH, Palazzo M, Hinds CJ, Watson D. Elevation of systemic oxygen delivery in the treatment of critically ill patients. N Engl J Med. 1994;330(24):1717–1722. doi: 10.1056/NEJM199406163302404. [DOI] [PubMed] [Google Scholar]
- 36.ARISE Investigators. ANZICS Clinical Trials Group. Peake SL, Delaney A, Bailey M, Bellomo R, Cameron PA, Cooper DJ, et al. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014;371(16):1496–1506. doi: 10.1056/NEJMoa1404380. [DOI] [PubMed] [Google Scholar]
- 37.ProCESS Investigators. Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370(18):1683–1693. doi: 10.1056/NEJMoa1401602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, Jahan R, Harvey SE, Bell D, Bion JF, Coats TJ, Singer M, Young JD, Rowan KM, ProMISe Trial Investigators Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015;372(14):1301–1311. doi: 10.1056/NEJMoa1500896. [DOI] [PubMed] [Google Scholar]
- 39.Hernandez G, Bruhn A, Luengo C, Regueira T, Kattan E, Fuentealba A, et al. Effects of dobutamine on systemic, regional and microcirculatory perfusion parameters in septic shock: a randomized, placebo-controlled, double-blind, crossover study. Intensive Care Med. 2013;39(8):1435–1443. doi: 10.1007/s00134-013-2982-0. [DOI] [PubMed] [Google Scholar]
- 40.Parker MM, Shelhamer JH, Natanson C, Alling DW, Parrillo JE. Serial cardiovascular variables in survivors and nonsurvivors of human septic shock: heart rate as an early predictor of prognosis. Crit Care Med. 1987;15(10):923–929. doi: 10.1097/00003246-198710000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Mosley 2nd WJ, Manuchehry A, McEvoy C, Rigolin V. Takotsubo cardiomyopathy induced by dobutamine infusion: a new phenomenon or an old disease with a new name. Echocardiography. 2010;27(3):E30–E33. doi: 10.1111/j.1540-8175.2009.01089.x. [DOI] [PubMed] [Google Scholar]
- 42.Sanfilippo F, Corredor C, Fletcher N, Landesberg G, Benedetto U, Foex P, et al. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis. Intensive Care Med. 2015;41(6):1004–1013. doi: 10.1007/s00134-015-3748-7. Erratum in Intensive Care Med. 2015;41(6):1178-9. [DOI] [PubMed] [Google Scholar]
- 43.Chauvet JL, El-Dash S, Delastre O, Bouffandeau B, Jusserand D, Michot JB, et al. Early dynamic left intraventricular obstruction is associated with hypovolemia and high mortality in septic shock patients. Crit Care. 2015;19:262–262. doi: 10.1186/s13054-015-0980-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bucher M, Kees F, Taeger K, Kurtz A. Cytokines down-regulate alpha1-adrenergic receptor expression during endotoxemia. Crit Care Med. 2003;31(2):566–571. doi: 10.1097/01.CCM.0000048621.36569.69. [DOI] [PubMed] [Google Scholar]
- 45.Weiss M, Arendt P, Hassna R. Effect of disease states on a1 -adrenoceptor binding and signal transduction parameters in isolated perfused heart: quantification by pharmacokinetic-pharmacodynamic modelling. J Pharm Pharmacol. 2014;66(5):668–676. doi: 10.1111/jphp.12184. [DOI] [PubMed] [Google Scholar]
- 46.Tang C, Yang J, Wu LL, Dong LW, Liu MS. Phosphorylation of beta-adrenergic receptor leads to its redistribution in rat heart during sepsis. Pt 2Am J Physiol. 1998;274(4):R1078–R1086. doi: 10.1152/ajpregu.1998.274.4.R1078. [DOI] [PubMed] [Google Scholar]
- 47.Yogev D, Basheer M, Blotnick S, Caraco Y, Muszkat M. Effects of sex and the common ADRB1 389 genetic polymorphism on the hemodynamic response to dobutamine. Pharmacogenet Genomics. 2015;25(11):555–563. doi: 10.1097/FPC.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 48.Bruck H, Leineweber K, Temme T, Weber M, Heusch G, Philipp T, et al. The Arg389Gly beta1-adrenoceptor polymorphism and catecholamine effects on plasma-renin activity. J Am Coll Cardiol. 2005;46(11):2111–2115. doi: 10.1016/j.jacc.2005.08.041. [DOI] [PubMed] [Google Scholar]
- 49.Aquilante CL, Yarandi HN, Cavallari LH, Andrisin TE, Terra SG, Lewis JF, et al. Beta-adrenergic receptor gene polymorphisms and hemodynamic response to dobutamine during dobutamine stress echocardiography. Pharmacogenomics J. 2008;8(6):408–415. doi: 10.1038/sj.tpj.6500490. [DOI] [PubMed] [Google Scholar]
- 50.Hees PS, Fleg JL, Mirza ZA, Ahmed S, Siu CO, Shapiro EP. Effects of normal aging on left ventricular lusitropic, inotropic, and chronotropic responses to dobutamine. J Am Coll Cardiol. 2006;47(7):1440–1447. doi: 10.1016/j.jacc.2005.11.052. [DOI] [PubMed] [Google Scholar]
- 51.Soto PF, Herrero P, Kates AM, Dence CS, Ehsani AA, Dávila-Román V, et al. Impact of aging on myocardial metabolic response to dobutamine. Am J Physiol Heart Circ Physiol. 2003;285(5):H2158–H2164. doi: 10.1152/ajpheart.00086.2003. [DOI] [PubMed] [Google Scholar]
- 52.Ahtarovski KA, Iversen KK, Lønborg JT, Madsen PL, Engstrøm T, Vejlstrup N. Left atrial and ventricular function during dobutamine and glycopyrrolate stress in healthy young and elderly as evaluated by cardiac magnetic resonance. Am J Physiol Heart Circ Physiol. 2012;303(12):H1469–H1473. doi: 10.1152/ajpheart.00365.2012. [DOI] [PubMed] [Google Scholar]
- 53.Tsutsui JM, Falcão SN, Dourado PM, Lima MF, Alves AA, Guerra VC, et al. Gender differences in chronotropic and hemodynamic responses during dobutamine-atropine stress echocardiography. Echocardiography. 2007;24(8):843–850. doi: 10.1111/j.1540-8175.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- 54.Aquilante CL, Humma LM, Yarandi HN, Andrisin TE, Lewis JF, Hamilton KK, et al. Influence of gender and race on hemodynamic response to dobutamine during dobutamine stress echocardiography. Am J Cardiol. 2004;94(4):535–538. doi: 10.1016/j.amjcard.2004.04.076. [DOI] [PubMed] [Google Scholar]